Potential risks include kidney injury1-3, liver injury2-5, cardiovascular toxicity5,6, pulmonary toxicity6,7, and mutagenicity, carcinogenicity, teratogenicity, embryotoxicity, and the creation of dangerous variants8-14. Favipiravir may impair clotting15. Variants may be less susceptible to favipiravir16.
Favipiravir was adopted
in 21 countries.
Recent:Ülger Ozhan Siripongboonsitti Siby.
Feb 23 |
Favipiravir for COVID-19: real-time meta-analysis of 75 studies (Version 88) | |
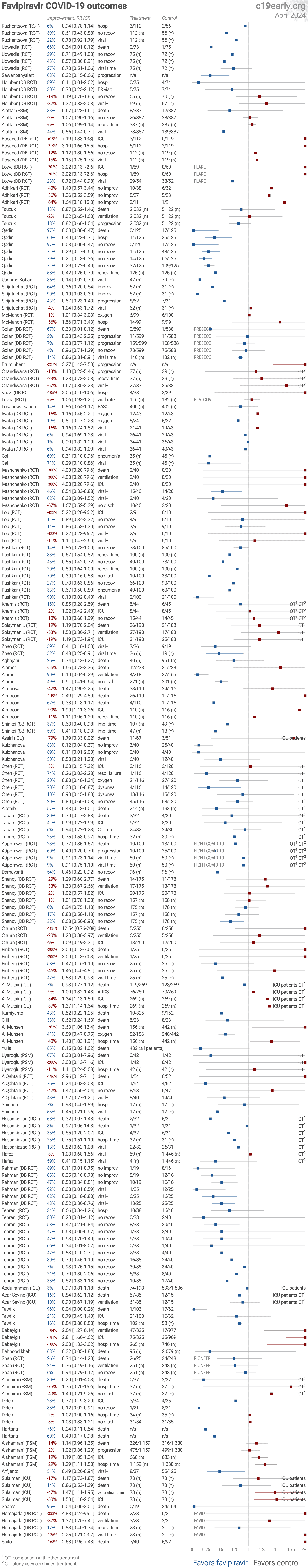
| Significantly lower risk is seen for recovery and viral clearance. 32 studies from 32 independent teams in 16 countries show significant benefit. Meta-analysis using the most serious outcome reported shows 10% [2‑18%] lower ris.. | ||
Jan 14 |
et al., Journal of Infection and Public Health, doi:10.1016/j.jiph.2026.103150 | Post-Exposure Prophylaxis with Favipiravir among Household Close Contacts to Confirmed COVID-19 Cases: A Cluster-Randomized Trial (PEPfavi) |
| 50% fewer symptomatic cases (p=0.37) and 36% fewer cases (p=0.46). RCT 168 household close contacts showing no significant difference in SARS-CoV-2 infection with favipiravir post-exposure prophylaxis. The primary endpoint of laboratory-confirmed infection by day 14 occurred in 7.3% of the favipiravir gr.. | ||
Jan 14 |
et al., Scientific Reports, doi:10.1038/s41598-025-31048-4 | Evaluation of the cardiopulmonary effects of repurposed COVID-19 therapeutics in healthy rats |
| Animal study analyzing potential cardiopulmonary harm with molnupiravir (MOL), favipiravir (FAVI), hydroxychloroquine (HCQL), and dexamethasone (DEX) in healthy Wistar albino rats. In summary: Data suggests molnupiravir may have the highe.. | ||
Jan 11 |
et al., Open Forum Infectious Diseases, doi:10.1093/ofid/ofaf695.1825 | Temporal Trends in Serious Adverse Events Associated with Oral Antivirals During the COVID-19 Pandemic: Insights from the FAERS Database (2020–2023) |
| Retrospective 11,547 serious adverse event reports from the FDA database (2020-2023) showing significant safety signals with oral COVID-19 antivirals. Paxlovid showed the strongest signals for drug-drug interactions (ROR: 4.83) and liver .. | ||
Jul 31 2025 |
et al., Phytomedicine Plus, doi:10.1016/j.phyplu.2025.100858 | Andrographis paniculata or Favipiravir in Mild COVID-19: A Randomized Control Trial |
| RCT 184 mild COVID-19 patients in Thailand showing no difference in pneumonia incidence or viral clearance between Andrographis paniculata and favipiravir. | ||
Jun 26 2025 |
et al., Pharmaceutics, doi:10.3390/pharmaceutics17070832 | Carboxylesterase Factors Influencing the Therapeutic Activity of Common Antiviral Medications Used for SARS-CoV-2 Infection |
| Review of how carboxylesterase (CES) enzymes influence the activity of certain COVID-19 antivirals, focusing on remdesivir, molnupiravir, nirmatrelvir, and favipiravir. Authors highlight that remdesivir requires activation by CES1, while .. | ||
Jun 24 2025 |
et al., Antimicrobial Agents and Chemotherapy, doi:10.1128/aac.00054-25 | Clinical effectiveness, safety, and viral mutagenicity of oral favipiravir for COVID-19: results from a community-based, open-label, randomized Phase III trial |
| 34% lower hospitalization (p=0.68), 21% improved 7-point scale results (p=0.61), 3% improved recovery (p=0.82), and 12% improved viral clearance (p=0.68). RCT 302 outpatients with mild COVID-19 showing no significant difference in outcomes with favipiravir treatment. The study population was relatively young and had few comorbidities, resulting in a low incidence of severe disease. Favipira.. | ||
Jun 23 2025 |
et al., Journal of the Medical Association of Thailand, doi:10.35755/jmedassocthai.2025.6.431-439-01780 | Favipiravir Exposure in the Second and Third Trimesters of Pregnancy with COVID-19: Risk of Adverse Perinatal Outcomes: A Retrospective Cohort Study |
| Retrospective 214 pregnant women with COVID-19 showing increased risk of small for gestational age (SGA) infants with favipiravir exposure during the second and third trimesters. | ||
Jun 9 2025 |
et al., medRxiv, doi:10.1101/2025.06.09.25329141 | Optimal dose and safety of intravenous favipiravir in hospitalised patients with SARS-CoV-2 infection: a Phase Ib, open-label, dose-escalating, randomised controlled study |
| RCT 24 hospitalized COVID-19 patients (16 treatment, 8 standard of care) evaluating safety and pharmacokinetics of intravenous favipiravir at escalating doses. The study found that IV favipiravir was safe and well-tolerated up to 2400mg t.. | ||
Jun 4 2025 |
et al., PLOS One, doi:10.1371/journal.pone.0324903 | In-hospital mortality outcomes of favipiravir in patients with moderate to severe COVID-19 infection: An emulated target trial using real-world data from the largest field hospital in Thailand |
| 4% improved survival (p=0.004). Retrospective 3,193 moderate to severe COVID-19 patients in Thailand showing modest survival benefits with favipiravir. This emulated target trial found that favipiravir alone increased restricted mean survival time by 1.32 days (p=0.042).. | ||
Apr 29 2025 |
et al., Food and Chemical Toxicology, doi:10.1016/j.fct.2025.115472 | Experimental evaluation of favipiravir (T-705)-induced liver and kidney toxicity in rats |
| Rat study showing dose-dependent liver and kidney toxicity with favipiravir. Authors note that lesions worsened at medium and high-dose levels and propose that co-administration of antioxidant or anti-inflammatory treatments might mitigat.. | ||
Apr 6 2025 |
et al., Talanta, doi:10.1016/j.talanta.2025.128084 | Does Favipiravir interact with DNA? Design of electrochemical DNA nanobiosensor to investigate the interaction between DNA and Favipiravir used in the treatment of COVID-19 |
| Favipiravir exhibits a direct interaction with DNA, as detected by a novel electrochemical nanobiosensor. Authors observed a decrease in guanine oxidation signals that suggests favipiravir may bind to or alter DNA structure, raising conce.. | ||
Feb 12 2025 |
et al., Viruses, doi:10.3390/v17020252 | Inhaled Dry Powder of Antiviral Agents: A Promising Approach to Treating Respiratory Viral Pathogens |
| Review of inhaled dry powder antiviral formulations for treating respiratory viral infections, focusing on COVID-19. Authors explain that traditional antiviral tablets face limitations including systemic side effects and delayed onset of .. | ||
Jan 11 2025 |
et al., Food and Chemical Toxicology, doi:10.1016/j.fct.2025.115235 | Evaluation of the effects of favipiravir (T-705) on the lung tissue of healty rats: An experimental study |
| Animal study showing dose-dependent lung inflammation and fibrosis with favipiravir. | ||
Jan 1 2025 |
et al., Mansoura Medical Journal, doi:10.58775/2735-3990.1433 | Clinical Features and Prognosis of Acute Kidney Injury in Hospital-Admitted Patients with COVID-19 in Egypt: A Single-Center Experience |
| 149% worse results (p=0.03). Retrospective 236 hospitalized COVID-19 patients showing favipiravir use associated with increased risk of acute kidney injury (AKI). AKI was associated with higher mortality. | ||
Dec 12 2024 |
et al., Journal of Virus Eradication, doi:10.1016/j.jve.2024.100576 | Assessing Favipiravir's Impact on SARS-CoV-2 Transmission within Households: Insights from a Multi-center Study (FaviPrev) |
| 25% lower transmission (p=0.05). Retrospective 976 mild to moderate COVID-19 outpatients in Thailand showing significantly lower household transmission with favipiravir treatment of index cases. | ||
Nov 7 2024 |
et al., Pharmacology Research & Perspectives, doi:10.1002/prp2.1233 | Favipiravir pharmacokinetics in Thai adults with mild COVID‐19: A sub‐study of interpatient variability and ethnic differences in exposure |
| Pharmacokinetic study of 8 Thai adults with mild COVID-19 showing higher favipiravir plasma concentrations compared to studies in other populations, suggesting regional/ethnic differences in pharmacokinetics. 7 of 8 adults achieved plasma.. | ||
Sep 14 2024 |
et al., Respiratory infections and bronchiectasis, doi:10.1183/13993003.congress-2024.PA1507 | Influence of demographics and dosing on COVID-19 outcomes and Favipiravir efficacy |
| Analysis of the Pioneer trial for favipiravir suggesting benefit in women and patients achieving target plasma concentrations. Only 17% of patients reached target plasma concentrations, with this subgroup showing trends toward improved ou.. | ||
Aug 31 2024 |
et al., Journal of Infection, doi:10.1016/j.jinf.2024.106248 | Favipiravir for COVID-19 in adults in the community in PRINCIPLE, an open-label, randomised, controlled, adaptive platform trial of short- and longer-term outcomes |
| 86% lower mortality (p=0.11), 1% lower combined mortality/hospitalization (p=0.51), and 17% improved recovery (p=0.003). RCT 3,622 (concurrent and eligible) COVID-19 outpatients in the UK showing significantly faster recovery with favipiravir, and significantly greater full recovery at 3, 6, and 12 months. Authors note: "From 16 Dec 2021, a minority of extr.. | ||
Aug 24 2024 |
et al., Journal of Clinical Medicine, doi:10.3390/jcm13175013 | Prevalence and Risk Factors of Headache Associated with COVID-19 |
| 70% higher long COVID (p=0.24) and 45% worse results (p=0.14). Retrospective 295 hospitalized COVID-19 patients in Slovakia showing 35% prevalence of headache, of which 41% of patients had persistent headache 12-15 months after infection. Authors' analysis of long COVID headache is only for the subgr.. | ||
Jul 30 2024 |
, C., The University of Hong Kong, PhD Thesis | An investigational study into the drug-associated mutational signature in SARS-CoV-2 viruses |
| In vitro and hamster study of drug associated SARS-CoV-2 mutations with several drugs including molnupiravir and favipiravir. Next-generation sequencing was used to identify de novo mutational spectra and single base substitution mutation.. | ||
Jul 26 2024 |
et al., Heliyon, doi:10.1016/j.heliyon.2024.e35331 | Convenient screening of the reproductive toxicity of favipiravir and antiviral drugs in Caenorhabditis elegans |
| Reproductive toxicity analysis of antiviral drugs in C. elegans, showing increased incidence of arrested embryos with molnupiravir, favipiravir, ribavirin, acyclovir, ganciclovir, zidovudine, and thalidomide compared to controls. Authors .. | ||
Jun 24 2024 |
et al., Current Clinical Microbiology Reports, doi:10.1007/s40588-024-00229-6 | SARS-CoV-2 Resistance to Small Molecule Inhibitors |
| Review of resistance mutations in SARS-CoV-2 3CLpro and nsp12 that could reduce efficacy of antiviral therapies including nirmatrelvir, ensitrelvir, remdesivir, and favipiravir. Authors identify 39 single mutations across 17 critical resi.. | ||
Jan 28 2024 |
et al., Infection Prevention in Practice, doi:10.1016/j.infpip.2024.100341 | Predictors of in-hospital mortality in elderly unvaccinated patients during SARS-CoV-2 Alpha variants epidemic |
| 168% higher mortality (p=0.06). Retrospective 132 hospitalized COVID-19 patients over age 65 in Japan during the Alpha variant surge, showing higher mortality with favipiravir in unadjusted results, without statistical significance. | ||
Jan 8 2024 |
et al., Infectious Diseases in Clinical Practice, doi:10.1097/IPC.0000000000001336 | Consequence of Antivirals Versus Standard Care on Clinical Situation in Patients With COVID-19 |
| 87% higher mortality (p=0.26). RCT 156 COVID-19 patients showing higher mortality with favipiravir and remdesivir overall. Favipiravir and remdesivir were more effective when started earlier, however note that Table 10 compares earlier favipiravir/remdesivir+standard c.. | ||
Jan 4 2024 |
et al., Virus Evolution, doi:10.1093/ve/veae001 | Genetic consequences of effective and suboptimal dosing with mutagenic drugs in a hamster model of SARS-CoV-2 infection |
| Syrian hamster study showing that short-term treatment with the mutagenic antiviral drugs favipiravir and molnupiravir led to increased genetic variation in SARS-CoV-2 viral populations. Treatment with effective antiviral doses resulted i.. | ||
Dec 29 2023 |
et al., Journal of Thai Traditional & Alternative Medicine, 21:3 | Randomized-Controlled Trial to Compare the Efficacy of Andrographis paniculata Powder and Favipiravir for the Treatment of Mild COVID-19 |
| RCT 231 mild COVID-19 outpatients in Thailand comparing Andrographis paniculata (AP) extract in two forms versus favipiravir, showing no significant differences between groups. Patients were randomized to either aerial parts AP extract (n.. | ||
Dec 6 2023 |
et al., Frontiers in Medicine, doi:10.3389/fmed.2023.1287542 | Unveiling patenting strategies of therapeutics and vaccines: evergreening in the context of COVID-19 pandemic |
| Review of the patenting activity and evergreening approaches for three major COVID-19 antiviral medications - remdesivir, molnupiravir, and favipiravir. Authors found extensive primary and secondary patent filing, with 29 applications cov.. | ||
Dec 1 2023 |
et al., Journal of Advanced Veterinary Research, 13:10 | Experimental Studies on Some Drugs Used in Covid-19 Treatment (Favipiravir and Dexamethasone) in Albino Rats |
| Animal study showing organ toxicity induced by favipiravir in rats. Histopathological and clinical results showed that favipiravir caused lesions in the liver, kidney and lung as well as increased liver enzymes, kidney function markers, o.. | ||
Nov 9 2023 |
et al., Journal of Biochemical and Molecular Toxicology, doi:10.1002/jbt.23536 | Assessment of toxicological effects of favipiravir (T‐705) on the lung tissue of rats: An experimental study |
| Analysis of the toxicological effects of favipiravir on healthy lung tissue in rats. Authors found that favipiravir treatment increased oxidative stress, apoptosis, and inflammation in the lung tissue as evidenced by changes in antioxidan.. | ||
Oct 12 2023 |
et al., Journal of Infection and Chemotherapy, doi:10.1016/j.jiac.2023.10.010 | Findings from a discontinued clinical trial of favipiravir in high-risk patients with early-onset COVID-19 |
| 16% higher need for oxygen therapy (p=0.73) and 16% worse viral clearance (p=0.66). Early terminated RCT 84 patients in Japan, showing no significant difference in outcomes with favipiravir treatment. There was a trend for improved efficacy for patients enrolled within 48 hours of symptom onset. | ||
Oct 7 2023 |
, M., Master's Thesis | COVID-19 hastalarında yüksek frekans odyometrisi sonuçlarının incelenmesi |
| High frequency audiometry in 40 individuals who had COVID-19, 21 treated with favipiravir, showing worse high frequency hearing for favipiravir patients, with statistical significance for right 14 kHz and left 12.5 kHz measurements, sugge.. | ||
Aug 24 2023 |
et al., Pneumonia, doi:10.1186/s41479-023-00124-6 (date from preprint) | Safety and efficacy of favipiravir in COVID-19 patients with pneumonia. A randomized, double-blind, placebo-controlled study (FAVID) |
| 383% higher mortality (p=0.49), 37% higher ventilation (p=1), no change in improvement (p=0.45), and 17% improved recovery (p=0.64). Underpowered RCT with 44 hospitalized patients in Spain, showing no significant difference with favipiravir treatment in the primary outcome of time to clinical improvement, or in the secondary efficacy outcomes. Adverse events were more .. | ||
Jul 17 2023 |
et al., Canadian Journal of Infectious Diseases and Medical Microbiology, doi:10.1155/2023/5205188 | Survival and Mortality in Hospitalized Children with COVID-19: A Referral Center Experience in Yazd, Iran |
| 96% lower mortality (p=0.14). Retrospective 183 hospitalized pediatric COVID-19 patients in Iran, showing no significant difference in mortality with in unadjusted results. | ||
Jun 14 2023 |
et al., Journal of Infection and Public Health, doi:10.1016/j.jiph.2023.06.011 | When Antivirals Backfire: An Evaluation of Favipiravir’s Clinical Outcomes in Critically Ill Patients with COVID-19: A Multicenter Cohort Study |
| 17% higher mortality (p=0.51), 47% longer ventilation (p=0.008), and 50% longer ICU admission (p=0.01). PSM retrospective 1,218 COVID-19 ICU patients in Saudi Arabia, showing no significant difference in mortality, and longer ICU/MV time with favipiravir treatment. | ||
Jun 1 2023 |
et al., Stem Cell Reports, doi:10.1016/j.stemcr.2023.05.007 | Parallel use of human stem cell lung and heart models provide insights for SARS-CoV-2 treatment |
| In vitro study showing that SARS-CoV-2 cell entry differs across cell types. ACE2 was required for infection in both lung and cardiac cells, but TMPRSS2 cleavage was required in lung cells, while the endosomal pathway was required in card.. | ||
May 24 2023 |
et al., Frontiers in Pediatrics, doi:10.3389/fped.2023.1127582 | Prevalence and associating factors of long COVID in pediatric patients during the Delta and the Omicron variants |
| 14% lower long COVID (p=0.34). Prospective analysis of 802 COVID-19 pediatric patients in Thailand, showing no significant difference in long COVID with favipiravir treatment in unadjusted results. | ||
May 4 2023 |
et al., Pathophysiology, doi:10.3390/pathophysiology30020016 | Duration of SARS-CoV-2 RNA Shedding Is Significantly Influenced by Disease Severity, Bilateral Pulmonary Infiltrates, Antibiotic Treatment, and Diabetic Status: Consideration for Isolation Period |
| 51% improved viral clearance (p=0.02). Retrospective 162 hospitalized COVID-19 patients in Indonesia, showing lower incidence of delayed viral clearance with favipiravir treatment in unadjusted results. | ||
Apr 5 2023 |
et al., BMC Infectious Diseases, doi:10.1186/s12879-023-08835-3 (date from preprint) | Clinical antiviral efficacy of favipiravir in early COVID-19 (PLATCOV): an open-label, randomised, controlled, adaptive platform trial |
| 6% worse viral clearance (p=0.42). High conflict of interest RCT with very low risk patients, high existing immunity, and a post-hoc change to exclude patients more likely to benefit. There was no significant difference in viral clearance with favipiravir among patients wi.. | ||
Mar 21 2023 |
et al., NCT04918927 | Favipiravir and/or Nitazoxanide: a Randomized, Double-blind, Placebo-controlled Trial of Early Antiviral Therapy in COVID-19 (FANTAZE) |
| 120 patient favipiravir early treatment RCT with results not reported over 2 years after completion. The protocol has been published [trialsjournal.biomedcentral.com]. | ||
Mar 1 2023 |
, K., Yakugaku Zasshi, doi:10.1248/yakushi.22-00169-1 | Pharmacokinetic Study of Antiviral Drugs in Patients with COVID-19 |
| Pharmacokinetics study measuring the blood concentration of favipiravir in 7 critical patients in Japan, showing concentrations below the EC50 in 33 of 36 samples when using the standard dosing regimen. Authors note that patient character.. | ||
Feb 20 2023 |
et al., Tropical Medicine and Infectious Disease, doi:10.3390/tropicalmed8020129 | Liver Injury in Favipiravir-Treated COVID-19 Patients: Retrospective Single-Center Cohort Study |
| Retrospective 362 COVID-19 patients showing significant liver injury in favipiravir-treated patients compared to untreated controls. | ||
Feb 15 2023 |
et al., Saudi Pharmaceutical Journal, doi:10.1016/j.jsps.2023.02.004 | Comprehensive evaluation of six interventions for hospitalized patients with COVID-19: A propensity score matching study |
| 14% higher mortality (p=0.13), 2% higher progression (p=0.83), 19% longer ICU admission (p=0.005), and 29% longer hospitalization (p=0.001). PSM retrospective 29 hospitals in Saudi Arabia, showing higher mortality with favipiravir treatment, without statistical significance. | ||
Feb 9 2023 |
et al., The Lancet Regional Health - Southeast Asia, doi:10.1016/j.lansea.2023.100167 | Clinical and treatment factors associated with the mortality of COVID-19 patients admitted to a referral hospital in Indonesia |
| 76% lower mortality (p=0.0005). Retrospective 689 hospitalized patients in Indonesia, showing lower mortality with favipiravir treatment. | ||
Jan 28 2023 |
et al., Advances in Respiratory Medicine, doi:10.3390/arm91010004 | Favipiravir in the Treatment of Outpatient COVID-19: A Multicenter, Randomized, Triple-Blind, Placebo-Controlled Clinical Trial |
| 105% higher hospitalization (p=0.43). RCT 77 outpatients in Iran, showing increased hospitalization with treatment, without statistical significance. Favipiravir 1600mg daily for five days. 21% of favipiravir patients did not complete treatment. | ||
Jan 19 2023 |
et al., Preprints, doi:10.20944/preprints202301.0341.v1 | Towards Predicting Length of Stay and Identification of Cohort Risk Factors Using Self-Attention Based Transformers and Association Mining: Covid-19 as Phenotype |
| Deep learning model for the prediction of hospitalization time for COVID-19 based on 311 patients in Saudi Arabia. Authors report shorter hospitalization time for HCQ and favipiravir, but do not provide details. | ||
Jan 3 2023 |
et al., Sabuncuoglu Serefeddin Health Sciences, doi:10.55895/sshs.1213382 | Effect of favipiravir use on INR, PT, aPTT tests of COVID-19 patients |
| Retrospective 100 patients in Turkey analyzing the effects of favipiravir on coagulation parameters in COVID-19 patients. Results showed prothrombin time (PT) and international normalized ratio (INR) were significantly prolonged in the fa.. | ||
Dec 31 2022 |
et al., Acta Clinica Croatica, doi:10.20471/acc.2022.61.03.05 | Effects of Hydroxychloroquine Plus Favipiravir Treatment on the Clinical Course and Biomarkers in Hospitalized COVID-19 Patients with Pneumonia |
| 88% improved recovery (p=0.02), 2% longer hospitalization (p=0.74), and 3% lower hospital discharge (p=1). Retrospective 69 COVID-19 patients in Turkey, showing improved fever recovery with the addition of favipiravir to HCQ, but no significant difference in discharge, ICU admission, or hospitalization time. | ||
Nov 24 2022 |
et al., Pharmaceuticals, doi:10.3390/ph15121456 | Analyzing the Difference in the Length of Stay (LOS) in Moderate to Severe COVID-19 Patients Receiving Hydroxychloroquine or Favipiravir |
| 80% lower mortality (p=0.49), 75% longer hospitalization (p=0.63), and 40% lower hospital discharge (p=0.74). Retrospective 200 hospitalized COVID-19 patients in Saudi Arabia, showing no significant difference in outcomes between HCQ and favipiravir. | ||
Nov 11 2022 |
et al., Medicine, doi:10.1097/MD.0000000000031681 | Early antiviral and supervisory dexamethasone treatment improve clinical outcomes of nonsevere COVID-19 patients |
| Retrospective 1,940 outpatients in Thailand, showing lower risk of clinical deterioration with early vs. late favipiravir treatment. | ||
Nov 1 2022 |
et al., eBioMedicine, doi:10.1016/j.ebiom.2022.104322 | Safety and efficacy of four drug regimens versus standard-of-care for the treatment of symptomatic outpatients with COVID-19: A randomised, open-label, multi-arm, phase 2 clinical trial |
| 13% higher progression (p=0.89), 23% slower recovery (p=0.42), and 67% worse viral clearance (p=0.13). High COI low-risk patient RCT in South Africa, showing no significant differences with favipiravir plus nitazoxanide. There were no deaths and no COVID-19 hospitalizations for favipiravir plus nitazoxanide. More patients were seropositive.. | ||
Sep 22 2022 |
et al., The Lancet Respiratory Medicine, doi:10.1016/S2213-2600(22)00412-X (date from preprint) | Favipiravir in patients hospitalised with COVID-19 (PIONEER trial): a multicentre, open-label, phase 3, randomised controlled trial of early intervention versus standard care |
| 26% lower mortality (p=0.24), 24% lower ventilation (p=0.21), and 6% improved recovery (p=0.53). PIONEER very late treatment RCT showing lower mortality and mechanical ventilation with favipiravir, without statistical significance. The conclusion "favipiravir is not efficacious in treating hospitalised adult patients with COVID-.. | ||
Sep 15 2022 |
et al., Iranian Journal of Science and Technology, Transactions A: Science, doi:10.1007/s40995-022-01351-0 | Evaluation of the Costs and Outcomes of COVID-19 Therapeutic Regimens in Hospitalized Patients in Shiraz |
| 68% lower mortality (p=0.2). Retrospective 2,174 hospitalized patients showing significantly shorter length of stay with favipiravir treatment. | ||
Sep 10 2022 |
et al., Tropical Medicine and Infectious Disease, doi:10.3390/tropicalmed7090238 | Clinical Course and Outcomes among COVID-19 Patients at the Hospitel in Bangkok: A Retrospective Study |
| 227% higher progression (p=0.005). Retrospective 514 patients in Thailand, showing higher risk of progression with favipiravir treatment. | ||
Sep 6 2022 |
et al., Clinical Infectious Diseases, doi:10.1093/cid/ciac712 | Favipiravir in patients with early mild-to-moderate COVID-19: a randomized controlled trial |
| 2% lower progression (p=1), 4% improved recovery (p=0.79), and 14% faster viral clearance (p<0.0001). RCT low-risk (1 death in the control arm) patients in the USA, showing no significant differences with favipiravir. A majority of trial outcomes were modified after completion: [clinicaltrials.gov]. 44% of patients had no detectable viral.. | ||
Sep 5 2022 |
et al., Drug Delivery, doi:10.1080/10717544.2022.2118398 | Pulmonary delivery of favipiravir inhalation solution for COVID-19 treatment: in vitro characterization, stability, in vitro cytotoxicity, and antiviral activity using real time cell analysis |
| In vitro study of a favipiravir solution for inhalation, showing effective antiviral activity for SARS-CoV-2 with significantly lower doses than typically used with oral administration. | ||
Aug 31 2022 |
et al., Frontiers in Medicine, doi:10.3389/fmed.2022.894126 | The association of antiviral drugs with COVID-19 morbidity: The retrospective analysis of a nationwide COVID-19 cohort |
| 184% higher ventilation (p=0.01), 181% higher ICU admission (p=0.001), and 100% longer hospitalization (p=0.001). Retrospective 1,472 hospitalized patients in Turkey, showing a higher ICU admission and ventilation with favipiravir. Results may be subject to confounding by indication. | ||
Jun 29 2022 |
et al., Advances in Virology, doi:10.1155/2022/9240941 | Effectiveness of Early Favipiravir Therapy in Hospitalised COVID-19 Patients |
| 96% lower mortality (p<0.0001), 21% lower ICU admission (p=0.45), and 16% shorter hospitalization (p<0.0001). Retrospective 103 hospitalized patients in Saudi Arabia, showing lower mortality with favipiravir in unadjusted results, and greater efficacy for treatment within 3 days of admission. | ||
Jun 28 2022 |
, S., SiSli Etfal Hastanesi Tip Bulteni / The Medical Bulletin of Sisli Hospital, doi:10.14744/SEMB.2021.35902 | Favipiravir Experience in COVID-19 Patients at a Tertiary Center Intensive Care Unit |
| 16% lower mortality (p=0.38) and 10% lower ventilation (p=0.75). Retrospective 100 ICU patients in Turkey, showing improved survival with favipiravir vs. lopinavir/ritonavir. | ||
Jun 21 2022 |
et al., Journal of Ayub Medical College Abbottabad, doi:10.55519/JAMC-03-10305 | Favipiravir efficacy and safety for the treatment of severe coronavirus 2019: a retrospective study |
| 3% lower mortality (p=0.81). Retrospective 1,699 ICU patients in Saudi Arabia, 193 treated with favipiravir, showing no significant difference in mortality. | ||
Jun 15 2022 |
et al., Mediterranean Journal of Infection Microbes and Antimicrobials, doi:10.4274/mjima.galenos.2022.2022.30 | Efficacy of Favipiravir in the Treatment of Moderate COVID-19 Patients: A Randomized, Open-label, Controlled Clinical Trial |
| 34% lower hospitalization (p=0.24). RCT 78 patients in Iran, showing improved recovery with favipiravir treatment. | ||
Jun 15 2022 |
et al., Antibiotics, doi:10.3390/antibiotics11060805 | Real-World Effectiveness and Optimal Dosage of Favipiravir for Treatment of COVID-19: Results from a Multicenter Observational Study in Thailand |
| Retrospective 63 hospitalized patients in Thailand treated with favipiravir showing a lower favipiravir loading dose negatively associated with clinical improvement. | ||
Jun 14 2022 |
et al., eClinicalMedicine, doi:10.1016/j.eclinm.2022.101703 | Favipiravir in early symptomatic COVID-19, a randomised placebo-controlled trial |
| 1% higher need for oxygen therapy (p=1) and 56% higher hospitalization (p=0.38). RCT with 99 favipiravir and 100 placebo patients in Australia, all except one being outpatients, showing no significant differences with treatment. | ||
Jun 8 2022 |
et al., medRxiv, doi:10.1101/2022.06.06.22275902 | Early Treatment of Favipiravir in COVID-19 Patients Without Pneumonia: A Multicentre, Open-Labelled, Randomized Control Study |
| 64% faster improvement (p=0.0005), 43% lower progression (p=0.25), and 4% worse viral clearance (p=0.87). RCT 93 patients in Thailand showing significantly faster clinical improvement with favipiravir treatment. 1800mg favipiravir bid day 1, 800mg bid 5-14 days until PCR-. | ||
Jun 7 2022 |
et al., Bratislava Medical Journal, doi:10.4149/BLL_2022_082 | The factors affecting the prolonged PCR positivity in COVID-19 patients |
| 86% improved viral clearance (p=0.03). Retrospective 126 patients in Turkey, showing lower risk of PCR+ at day 14 with favipiravir treatment. | ||
May 23 2022 |
et al., International Journal of Applied Sciences: Current and Future Research Trends, 13:1 | Efficacy of Favipiravir in the Treatment of Mild to Moderate COVID-19 Patients in Erbil: A Controlled Clinical Trial |
| 97% lower mortality (p<0.0001), 60% lower hospitalization (p=0.001), and 97% improved recovery (p<0.0001). Prospective study with 125 favipiravir patients and 125 patients declining favipiravir treatment, showing lower mortality and improved recovery with treatment. All patients received vitamin C, D, and zinc. Favipiravir 3200mg day 1, follow.. | ||
May 17 2022 |
et al., Expert Review of Clinical Pharmacology, doi:10.1080/17512433.2022.2078701 | Favipiravir-based treatment for outcomes of patients with COVID-19: a systematic review and meta-analysis of randomized controlled trials |
| Systematic review and meta analysis of favipiravir RCTs, showing improved viral clearance and recovery, but no significant difference for mortality, ICU admission, or ventilation. | ||
May 13 2022 |
et al., Clinical Infection in Practice, doi:10.1016/j.clinpr.2022.100145 | Safety and Efficacy of Favipiravir for the management of COVID-19 Patients: A Randomized Control Trial |
| 89% greater improvement (p=0.005) and 92% improved viral clearance (p=0.0008). RCT hospitalized patients in Bangladesh, showing faster recovery and viral clearance with favipiravir treatment. | ||
May 3 2022 |
et al., International Journal of General Medicine, doi:10.2147/IJGM.S349241 | Evaluation of the Safety and Efficacy of Favipiravir in Adult Indian Patients with Mild-to-Moderate COVID-19 in a Real-World Setting |
| Prospective single-arm study of 1,083 patients receiving favipiravir in India, showing one death and no new safety issues. | ||
May 1 2022 |
et al., Mutagenesis, doi:10.1093/mutage/geac011 | DNA damage in peripheral blood lymphocytes of severely ill COVID-19 patients in relation to inflammatory markers and parameters of hemostasis |
| Observational study of 24 severely ill hospitalized COVID-19 patients showing significantly higher DNA damage in peripheral blood lymphocytes compared to 15 healthy controls. Favipiravir was associated with increased DNA damage. | ||
Apr 22 2022 |
et al., SSRN, doi:10.2139/ssrn.3889346 | The efficacy and adverse effects of favipiravir on COVID-19 patients: a systematic review and meta-analysis of published clinical trials and observational studies |
| Systematic review and meta analysis of 17 favipiravir trials, showing improved viral clearance and recovery. | ||
Apr 18 2022 |
et al., Viruses, doi:10.3390/v14040841 | Lethal Mutagenesis of RNA Viruses and Approved Drugs with Antiviral Mutagenic Activity |
| Review of lethal mutagenesis for RNA viruses, as used by molnupiravir, favipiravir, and ribavirin. Authors note the potential for permanently modifying the genomes of patients while causing teratogenicity or embryotoxicity, and the potent.. | ||
Apr 8 2022 |
et al., Antibiotics, doi:10.3390/antibiotics11040498 | Antiviral Used among Non-Severe COVID-19 Cases in Relation to Time till Viral Clearance: A Retrospective Cohort Study |
| 3% slower viral clearance (p=0.09). Retrospective hospitalized patients in the United Arab Emirates, showing no significant difference in viral clearance with different combinations of HCQ, AZ, favipiravir, and lopinavir/ritonavir. | ||
Mar 24 2022 |
et al., Viruses, doi:10.3390/v14040670 | Longitudinal Analysis of Neutralizing Potency against SARS-CoV-2 in the Recovered Patients after Treatment with or without Favipiravir |
| 7% shorter hospitalization (p=0.84) and 55% faster viral clearance (p=0.04). Retrospective 17 COVID+ patients treated with favipiravir and 17 matched controls in Japan, showing faster viral clearance with treatment. Favipiravir 3600mg day one, 1600mg per day for up to 14 days. | ||
Mar 23 2022 |
et al., Scientific Reports, doi:10.1038/s41598-022-08794-w | Randomized controlled trial of favipiravir, hydroxychloroquine, and standard care in patients with mild/moderate COVID-19 disease |
| 76% lower ICU admission (p=0.2), 42% worse recovery (p=0.51), and 43% improved viral clearance (p=0.21). RCT with 54 favipiravir, 51 HCQ, and 52 SOC hospitalized patients in Bahrain, showing no significant differences. Viral clearance improved with both treatments, but did not reach statistical significance with the small sample size. | ||
Mar 21 2022 |
et al., Infectious Diseases and Therapy, doi:10.1007/s40121-022-00617-9 | Effectiveness of Favipiravir on Nonsevere, Early-Stage COVID-19 in Japan: A Large Observational Study Using the COVID-19 Registry Japan |
| 13% lower mortality (p=0.59), 2% higher ventilation (p=0.93), and 18% lower progression (p=0.1). Retrospective database analysis of 7,654 hospitalized patients in Japan, showing no significant differences with favipiravir treatment. NCGM-G-003494-0. | ||
Mar 17 2022 |
et al., Acta Medica, doi:10.32552/2022.ActaMedica.719 | Comparison of Favipiravir to Hydroxychloroquine Plus Azithromycin in the Treatment of Patients with Non-critical COVID-19: A Single-center, Retrospective, Propensity Score-matched Study |
| 67% lower mortality (p=1), 200% higher ICU admission (p=1), and 11% longer hospitalization (p=0.9). PSM retrospective 260 late stage hospitalized COVID-19 pneumonia patients in Turkey, showing no significant difference between favipiravir and HCQ. | ||
Mar 24 2022 |
et al., Journal of Medical Virology, doi:10.1002/jmv.27724 | Efficacy and safety of favipiravir plus interferon-beta versus lopinavir/ritonavir plus interferon-beta in moderately ill patients with COVID-19: A randomized clinical trial |
| 68% lower mortality (p=0.15), 35% lower ICU admission (p=0.51), 25% shorter hospitalization (p=0.14), and 18% improved viral clearance (p=0.24). RCT comparing favipiravir and lopinavir/ritonavir, showing no significant differences. All patients received interferon-beta. Favipiravir 1600mg bid for the first day and 600mg bid for the following 4 days. | ||
Mar 7 2022 |
et al., Pathophysiology, doi:10.3390/pathophysiology29010009 | Evaluation of Antibacterial and Antiviral Drug Effectiveness in COVID-19 Therapy: A Data-Driven Retrospective Approach |
| 85% lower mortality (p=0.05). Retrospective hospitalized patients in Indonesia, showing lower mortality and shorter hospitalization with favipiravir. | ||
Mar 4 2022 |
et al., Frontiers in Medicine, doi:10.3389/fmed.2022.826247 | Favipiravir Effectiveness and Safety in Hospitalized Moderate-Severe COVID-19 Patients: Observational Prospective Multicenter Investigation in Saudi Arabia |
| 263% higher mortality (p=0.04), 41% lower need for oxygen therapy (p<0.0001), and 40% longer hospitalization (p=0.03). Prospective observational study of 598 hospitalized patients in Saudi Arabia, showing higher risk of mortality and longer hospitalization time with favipiravir. | ||
Mar 3 2022 |
et al., Respiratory Medicine and Research, doi:10.1016/j.resmer.2022.100900 | Characteristics and outcomes of COVID-19 patients with IPF: A multi-center retrospective study |
| 38% lower mortality (p=0.51). Retrospective 46 idiopathic pulmonary fibrosis patients with COVID-19 in Turkey, showing lower mortality with favipiravir in unadjusted results, without statistical significance. | ||
Mar 1 2022 |
et al., International Journal of Infectious Diseases, doi:10.1016/j.ijid.2021.12.109 | Efficacy of Favipiravir in treatment of mild & moderate COVID-19 infection in Nepal: a multi-center, randomized, open-labelled, phase III clinical trial |
| 40% worse improvement (p=0.57). Preliminary report for an RCT in Nepal with 38 favipiravir patients and 32 control patients, showing no significant differences. There were no serious side effects. | ||
Feb 28 2022 |
et al., Journal of Clinical Virology Plus, doi:10.1016/j.jcvp.2022.100068 | Factors Associated with Death and ICU Referral among COVID-19 Patients Hospitalized in the Secondary Referral Academic Hospital in East Jakarta, Indonesia |
| 48% lower mortality (p=0.21). Retrospective 477 hospitalized patients in Indonesia, showing lower mortality with favipiravir in unadjusted results, not reaching statistical significance. | ||
Feb 15 2022 |
et al., Journal of Infection and Public Health, doi:10.1016/j.jiph.2022.01.013 | Overview of Clinical Outcome and Therapeutic Effectiveness of Favipiravir in Patients with COVID-19 Admitted to Intensive Care Unit, Riyadh, Saudi Arabia |
| 7% lower mortality (p=0.49), 9% higher ARDS (p=0.63), 34% longer ICU admission (p=0.001), and 37% longer hospitalization (p=0.001). Retrospective 269 favipiravir ICU patients in Saudi Arabia and 269 matched controls receiving different treatments, showing no significant difference. | ||
Feb 15 2022 |
et al., PLOS Medicine, doi:10.1371/journal.pmed.1004120 (date from preprint) | Favipiravir, lopinavir-ritonavir, or combination therapy (FLARE): A randomised, double-blind, 2 × 2 factorial placebo-controlled trial of early antiviral therapy in COVID-19 |
| 28% improved viral clearance (p=0.03). 240 patient RCT comparing favipiravir, favipiravir + LPV/r, LPV/r, and placebo, showing improved viral clearance with favipiravir, but no significant difference for LPV/r. Efficacy was lower in the combined favipiravir + LPV/r arm, where .. | ||
Feb 1 2022 |
et al., The Brazilian Journal of Infectious Diseases, doi:10.1016/j.bjid.2022.102328 | The effect of favipiravir versus hydroxychloroquine on clinical and laboratory findings in COVID-19 in healthcare workers |
| 79% lower hospitalization (p=0.001), 11% slower recovery (p=0.51), and 22% faster viral clearance (p=0.001). Retrospective 237 low-risk healthcare workers in Turkey, 123 treated with favipiravir and 114 treated with HCQ, showing lower hospitalization and faster viral clearance with favipiravir, and similar improvement. This study is subject to s.. | ||
Jan 28 2022 |
et al., Environmental and Molecular Mutagenesis, doi:10.1002/em.22471 | Human genetic risk of treatment with antiviral nucleoside analog drugs that induce lethal mutagenesis: the special case of molnupiravir |
| Review of antiviral nucleoside analog drugs that induce lethal mutagenesis, including molnupiravir and favipiravir, and the potential mutagenic risks to human DNA and human mitochondrial DNA. Author recommends monitoring for mutagenicity,.. | ||
Jan 12 2022 |
et al., bioRxiv, doi:10.1101/2022.01.11.475889 | Favipiravir, umifenovir and camostat mesylate: a comparative study against SARS-CoV-2 |
| In vitro and in silico study showing that the combination of favipiravir and umifenovir or camostat mesylate has greater antiviral efficacy than single drug treatment. | ||
Jan 11 2022 |
et al., Clinical Microbiology and Infection, doi:10.1016/j.cmi.2021.12.026 | Efficacy of favipiravir in adults with mild COVID-19: a randomized, double-blind, multicenter, placebo-controlled trial clinical trial |
| 619% higher ICU admission (p=0.11), 219% higher hospitalization (p=0.16), 12% slower recovery (p=0.51), and 15% slower viral clearance (p=0.51). RCT with 112 favipiravir and 119 control patients showing no significant differences in outcomes. Viral clearance and clinical recovery for patients treated within 48 hours was better than those treated later. NCT04464408. | ||
Dec 7 2021 |
et al., Open Forum Infectious Diseases, doi:10.1093/ofid/ofab56310 | US201 Study: A Phase 2, Randomized Proof-of-Concept Trial of Favipiravir for the Treatment of COVID-19 |
| 20% longer hospitalization, 58% improved recovery (p=0.08), and 47% faster viral clearance (p=0.04). Small very late treatment RCT in the USA, with 25 favipiravir and 25 control patients, showing faster viral clearance with treatment. The benefit was only seen in patients <8 days from symptom onset. There were no significant differences .. | ||
Nov 30 2021 |
et al., Journal of Infection and Public Health, doi:10.1016/j.jiph.2022.08.011 (date from preprint) | Favipiravir for the Treatment of Coronavirus Disease 2019 Pneumonia; a Propensity Score-matched Cohort Study |
| 33% lower mortality (p=0.5), 2% worse recovery (p=0.73), and 44% improved viral clearance (p<0.0001). PSM retrospective with 1,493 patients, showing significantly improved viral clearance with favipiravir. There were no significant differences in clinical improvement or mortality. Mortality was lower (2.1% vs 3.1%), without statistical si.. | ||
Nov 24 2021 |
et al., Clinical Infectious Diseases, doi:10.1093/cid/ciac312 (date from preprint) | Favipiravir for treatment of outpatients with asymptomatic or uncomplicated COVID-19: a double-blind randomized, placebo-controlled, phase 2 trial |
| 89% lower hospitalization (p=0.06), 30% lower progression (p=0.56), 19% worse recovery (p=0.43), and 32% worse viral clearance (p=0.24). Small RCT 116 mITT patients in the USA, 59 treated with favipiravir, showing no significant differences with treatment. | ||
Nov 19 2021 |
et al., Clinical Infectious Diseases, doi:10.1093/cid/ciab962 | Efficacy of Early Treatment with Favipiravir on Disease Progression among High Risk COVID-19 Patients: A Randomized, Open-Label Clinical Trial |
| 1154% higher mortality (p=0.08), 20% higher ventilation (p=0.76), and 9% higher ICU admission (p=0.84). RCT 500 hospitalized patients in Malaysia, showing no significant differences with favipiravir treatment. | ||
Nov 9 2021 |
et al., medRxiv, doi:10.1101/2021.11.08.21265884 | Favipiravir In Adults with Moderate to Severe COVID-19: A Phase 3 Multicentre, Randomized, Double-Blind, Placebo-Controlled Trial |
| 29% higher mortality (p=0.54), 33% higher ventilation (p=0.54), 2% higher ICU admission (p=0.54), and 1% slower recovery (p=0.94). Late stage RCT with 353 hospitalized patients, showing no significant differences with favipiravir treatment overall, however a trend towards benefit was seen within patients treated relatively early, including a statistically significant.. | ||
Nov 1 2021 |
et al., Kesmas: National Public Health Journal, doi:10.21109/kesmas.v16i4.5433 | The Effectiveness and Safety of Favipiravir in COVID-19 Hospitalized Patients in Bali, Indonesia |
| 54% improved recovery (p=0.03). Retrospective 192 hospitalized patients in Indonesia, 96 patients treated with favipiravir, showing improved recovery with treatment. Only the abstract is currently available. | ||
Oct 5 2021 |
et al., SSRN Electronic Journal, doi:10.2139/ssrn.3936499 | Various Combinations of Favipiravir, Lopinavir-Ritonavir, Darunavir-Ritonavir, High-Dose Oseltamivir, and Hydroxychloroquine for the Treatment of COVID-19: A Randomized Controlled Trial (FIGHT-COVID-19 Study) |
| 23% lower mortality (p=0.66), 60% lower progression (p=0.009), and 9% faster viral clearance (p=0.43). RCT 200 moderate/severe patients in Thailand, showing significantly lower progression with favipiravir vs. oseltamivir. This paper contains multiple data issues and the preprint had not been published in a journal. The manuscript title an.. | ||
Sep 30 2021 |
et al., Iranian Journal of Pharmaceutical Research, doi:10.22037/ijpr.2021.115510.15401 | Favipiravir Effects on the Control of Clinical Symptoms of Hospitalized COVID-19 Cases: An Experience with Iranian Formulated Dosage Form |
| 41% lower ICU admission (p=0.36), 6% improved recovery (p=0.76), and 25% shorter hospitalization (p=0.03). Small 62 patient late stage RCT in Iran comparing favipiravir and lopinavir/ritonavir, showing significant improvement in fever, cough, and dyspnea with favipiravir on day 5. There was no significant difference in mortality, ICU admission.. | ||
Sep 14 2021 |
et al., International Journal of General Medicine, 2021:14 | Effectiveness and Safety of Favipiravir Compared to Hydroxychloroquine for Management of Covid-19: A Retrospective Study |
| 57% lower mortality (p=0.05). Retrospective hospitalized patients in Saudi Arabia, showing lower mortality with favipiravir compared to HCQ, not quite reaching statistical significance. Authors do not indicate the factors behind which therapy was chosen. May be subjec.. | ||
Sep 9 2021 |
et al., Southeast Asian Journal of Tropical Medicine and Public Health, 52:4 | Assessment of outcomes following implementation of antiviral treatment guidelines for COVID-19 during the first wave in Thailand |
| 68% lower progression (p=0.003). Retrospective 744 hospitalized patients in Thailand, showing lower risk of a poor outcome for favipiravir treatment within 4 days of symptom onset. Early treatment with CQ/HCQ and lopinavir/ritonavir or darunavir/ritonavir also showed low.. | ||
Sep 2 2021 |
et al., Frontiers in Pharmacology, doi:10.3389/fphar.2021.683296 | Favipiravir Versus Arbidol for Clinical Recovery Rate in Moderate and Severe Adult COVID-19 Patients: A Prospective, Multicenter, Open-Label, Randomized Controlled Clinical Trial |
| 74% lower progression (p=0.37), 20% lower need for oxygen therapy (p=0.42), and 20% improved recovery (p=0.15). Very late stage (9 days from symptom onset) RCT with 116 favipiravir patients and 120 arbidol patients in China, showing no significant difference in clinical recovery (relief of fever and cough, respiratory frequency ≤24 times/min, and o.. | ||
Aug 31 2021 |
et al., | Clinical efficacy of the antiviral drug favipiravir in the complex treatment of patients with COVID-19 coronavirus infection |
| 88% greater improvement (p<0.0001) and 50% improved viral clearance (p=0.18). Retrospective 40 favipiravir patients in Kazakhstan and 40 controls, showing faster recovery and viral clearance with treatment. | ||
Aug 28 2021 |
et al., Journal of Infection and Public Health, doi:10.1016/j.jiph.2021.08.030 | COVID-19 related treatment and outcomes among COVID-19 ICU patients: A retrospective cohort study |
| 79% higher mortality (p=0.5). Retrospective 118 ICU patients in Saudi Arabia showing no significant differences in unadjusted results with zinc, vitamin D, and favipiravir treatment. | ||
Aug 27 2021 |
et al., Infectious Diseases and Therapy, doi:10.1007/s40121-021-00517-4 | Efficacy and Safety of Favipiravir in Moderate COVID-19 Pneumonia Patients without Oxygen Therapy: A Randomized, Phase III Clinical Trial |
| 37% faster recovery (p=0.01). RCT 156 patients in Japan, 107 treated with favipiravir, showing significant improvement in a composite outcome defined as the time to improvement in temperature, SpO2, CT findings, and recovery to PCR-. | ||
Aug 24 2021 |
et al., Journal of Infection and Public Health, doi:10.1016/j.jiph.2021.08.022 | Favipiravir versus Standard of Care in Patients with Severe COVID-19 Infections: A Retrospective Comparative Study |
| 42% higher mortality (p=0.1), 90% higher ICU admission (p=0.02), and 11% slower recovery (p=0.17). Retrospective 226 COVID-19 pneumonia patients, 110 treated with favipiravir, showing higher mortality (p=0.1) and ICU admission (p=0.02) with treatment in multivariate analysis. | ||
Jun 18 2021 |
et al., PLOS One, doi:10.1371/journal.pone.0252302 | An in vitro study of dual drug combinations of anti-viral agents, antibiotics, and/or hydroxychloroquine against the SARS-CoV-2 virus isolated from hospitalized patients in Surabaya, Indonesia |
| In vitro study of combinations of drugs showing antiviral efficacy of HCQ alone and in combination with AZ, favipiravir, and doxycycline. No high levels of cytotoxicity were observed, and authors conclude that using a combination of drugs.. | ||
Jun 1 2021 |
et al., NCT04411433 | Efficacy and Safety of Hydroxychloroquine and Favipiravir in the Treatment of Mild to Moderate COVID-19 |
| 1,008 patient favipiravir early treatment RCT with results not reported over 4 years after completion. | ||
May 19 2021 |
et al., Current Medical Research and Opinion, doi:10.1080/03007995.2021.1920900 | Effectiveness and safety of favipiravir compared to supportive care in moderately to critically ill COVID-19 patients: a retrospective study with propensity score matching sensitivity analysis |
| 56% higher mortality (p=0.26), 90% lower ventilation (p<0.0001), and 49% higher hospital discharge (p<0.0001). Retrospective 234 favipiravir and 223 control patients in Saudi Arabia, showing shorter time to discharge and lower progression to ventilation, but no significant difference in mortality. | ||
May 5 2021 |
et al., Journal of microbiology, epidemiology and immunobiology, doi:10.36233/0372-9311-114 | Favipiravir: the hidden threat of mutagenic action |
| Review of the mutagenic effect of favipiravir and associated concerns. | ||
Apr 29 2021 |
et al., Journal of Medical Virology, doi:10.1002/jmv.27053 | Decreased In-Hospital Mortality Associated with Aspirin Administration in Hospitalized Patients Due to Severe COVID-19 |
| 26% lower mortality (p=0.28). Retrospective 991 hospitalized patients in Iran focusing on aspirin use but also showing results for HCQ, remdesivir, and favipiravir. | ||
Apr 28 2021 |
et al., Respiratory Medicine, doi:10.1016/j.rmed.2021.106433 | The predictors of COVID-19 mortality in a nationwide cohort of Turkish patients |
| 84% higher mortality (p=0.29). Retrospective 1,500 hospitalized late stage (median SaO2 87.7) patients in Turkey, showing no significant difference in mortality with treatment. | ||
Apr 21 2021 |
et al., International Immunopharmacology, doi:10.1016/j.intimp.2021.107702 | Favipiravir in the treatment of patients with SARS-CoV-2 RNA recurrent positive after discharge: a multicenter, open-label, randomized trial |
| 59% improved viral clearance (p=0.06). RCT with 55 patients (36 favipiravir, 19 control) who were PCR+ after recovery, showing improved viral clearance with treatment. | ||
Apr 19 2021 |
, Fujita Health University | Favipiravir Observational Study Interim Report 3 |
| Retrospective analysis of favipiravir use in 10,986 hospitalized patients, including analysis of changes in clinical status and side effects. Common adverse events were uric acid level increase and liver function enzyme increase. Authors .. | ||
Apr 17 2021 |
et al., Journal of Infection and Chemotherapy, doi:10.1016/j.jiac.2021.04.013 | Early favipiravir treatment was associated with early defervescence in non-severe COVID-19 patients |
| Retrospective 41 favipiravir patients finding that early treatment was more successful. | ||
Mar 11 2021 |
et al., International Immunopharmacology, doi:10.1016/j.intimp.2021.107522 | Safety and efficacy of Favipiravir in moderate to severe SARS-CoV-2 pneumonia |
| 19% higher mortality (p=0.54), 53% higher ventilation (p=0.15), and 19% higher ICU admission (p=0.56). RCT late stage patients (median SpO2 89), 193 treated with favipiravir, 187 with lopinavir/ritonavir, showing no significant differences in mortality, intubation, or ICU admission. | ||
Mar 8 2021 |
et al., medRxiv, doi:10.1101/2021.03.05.21251351 | A single-center retrospective cohort study of Covid-19 medications: Remdesivir, Favipiravir, Methylprednisolone, Dexamethasone, and Interferon β1a and their combinations |
| Retrospective 324 hospitalized patients in Iran reporting on the use remdesivir, favipiravir, methylprednisolone, dexamethasone, and Interferon β1a and their combinations. There is no control group in this study. | ||
Feb 4 2021 |
et al., Research Square, doi:10.21203/rs.3.rs-175340/v1 | Benefits of Treatment With Favipiravir in Hospitalized Patients for COVID-19: a Retrospective Observational Case-control Study |
| Retrospective 144 COVID-19 patients in Turkey, one group receiving FPV after a mean of 4.7 days, a second group after a mean of 8.6 days, and all groups receiving HCQ. No improvement in clinical outcomes was seen with the addition of FPV,.. | ||
Jan 25 2021 |
et al., Archives of Virology, doi:10.1007/s00705-021-04956-9 | RETRACTED: Efficacy of favipiravir in COVID-19 treatment: a multi-center randomized study |
| This study was retracted. | ||
Jan 14 2021 |
et al., Research Square, doi:10.21203/rs.3.rs-142868/v1 | Early Onset Favipiravir Saves Lives |
| Retrospective 180 hospitalized patients showing lower mortality when Favipiravir is given earlier. 17% of patients given Favipiravir within 3 days died, compared to 38% when given after 3 days. | ||
Nov 17 2020 |
et al., Antimicrobial Agents and Chemotherapy, doi:10.1128/AAC.01897-20 | A Prospective, Randomized, Open-Label Trial of Early versus Late Favipiravir Therapy in Hospitalized Patients with COVID-19 |
| Small RCT comparing late and very late (7 and 14 days from fever onset) favipiravir. Viral clearance was non-statistically significantly improved with relatively early treatment. There was a reduction in time to defervescence, and a signi.. | ||
Nov 16 2020 |
et al., International Journal of Infectious Diseases, doi:10.1016/j.ijid.2020.11.142 | Efficacy and Safety of Favipiravir, an Oral RNA-Dependent RNA Polymerase Inhibitor, in Mild-to-Moderate COVID-19: A Randomized, Comparative, Open-Label, Multicenter, Phase 3 Clinical Trial |
| 29% faster recovery (p=0.07) and 27% faster viral clearance (p=0.1). RCT with 75 favipiravir patients and 75 control patients showing improved recovery with treatment. | ||
Nov 9 2020 |
et al., International Journal of Infectious Diseases, doi:10.1016/j.ijid.2020.11.008 | Randomized Controlled Open Label Trial on the Use of Favipiravir Combined with Inhaled Interferon beta-1b in Hospitalized Patients with Moderate to Severe COVID-19 Pneumonia |
| 15% lower mortality (p=1), 2% higher ICU admission (p=1), and 10% worse recovery (p=0.82). Small 89 patient RCT comparing favipiravir and inhaled interferon with HCQ for moderate to severe COVID-19 pneumonia, not finding significant differences. There was no control group. | ||
Nov 5 2020 |
et al., NCT04542694 | Study of Favipiravir Compared to Standard of Care in Hospitalized Patients With COVID-19 |
| 14% improved recovery (p=0.06), 70% higher hospital discharge (p=0.0001), 33% lower pneumonia (p=0.007), and 90% improved viral clearance (p<0.0001). RCT 200 patients showing improvements in clinical recovery and viral clearance with favipiravir. There is no paper available but results are posted in clinicaltrials.gov. | ||
Oct 26 2020 |
et al., SSRN, doi:10.2139/ssrn.3696907 | Phase 3 Trial of Coronavir (Favipiravir) in Patients with Mild to Moderate COVID-19 |
| 39% faster recovery (p=0.007) and 22% improved viral clearance (p=0.16). RCT 168 patients, 112 receiving favipiravir and 56 SOC, showing shorter time to clinical improvement and faster viral clearance with favipiravir. | ||
Oct 25 2020 |
et al., European Journal of Pharmaceutical Sciences, doi:10.1016/j.ejps.2020.105631 | Clinical Outcomes and Plasma Concentrations of Baloxavir Marboxil and Favipiravir in COVID-19 Patients: An Exploratory Randomized, Controlled Trial |
| 422% higher ICU admission (p=0.21), 11% improved recovery (p=1), and 422% worse viral clearance (p=0.21). Small late stage RCT with 10 favipiravir, 10 baloxavir marboxil, and 10 control patients in China, showing no significant differences. | ||
Sep 30 2020 |
et al., Biomedicine & Pharmacotherapy, doi:10.1016/j.biopha.2020.110825 | Tocilizumab combined with favipiravir in the treatment of COVID-19: A multicenter trial in a small sample size |
| Small study with 14 combined favipiravir/tocilizumab, 7 favipiravir, and 5 tocilizumab patients suggesting that tocilizumab combined with or without favipiravir can improve pulmonary inflammation and inhibit progression. | ||
Aug 9 2020 |
et al., Clinical Infectious Diseases, doi:10.1093/cid/ciaa1176 | AVIFAVIR for Treatment of Patients with Moderate COVID-19: Interim Results of a Phase II/III Multicenter Randomized Clinical Trial |
| 46% improved viral clearance (p=0.03) and 67% lower hospital discharge (p=0.51). Interim results for a small RCT with 40 favipiravir and 20 control patients showing faster viral clearance with favipiravir. There is limited data in this report to evaluate the results. 75% of the control group received HCQ/CQ. | ||
Jun 19 2020 |
et al., bioRxiv, doi:10.1101/2020.06.19.159053 | Favipiravir at high doses has potent antiviral activity in SARS-CoV-2−infected hamsters, whereas hydroxychloroquine lacks activity |
| Animal study with Syrian hamsters, showing antiviral activity with favipiravir. | ||
Mar 18 2020 |
et al., Engineering, doi:10.1016/j.eng.2020.03.007 | Experimental Treatment with Favipiravir for COVID-19: An Open-Label Control Study |
| 69% lower pneumonia (p=0.04) and 71% improved viral clearance (p=0.03). Comparison of 35 FPV patients and 35 LPV/RTV patients, showing significant improvements in chest CT and faster viral clearance with FPV. | ||
References
Abdulaziz et al., Clinical Features and Prognosis of Acute Kidney Injury in Hospital-Admitted Patients with COVID-19 in Egypt: A Single-Center Experience, Mansoura Medical Journal, doi:10.58775/2735-3990.1433.
Ülger et al., Experimental evaluation of favipiravir (T-705)-induced liver and kidney toxicity in rats, Food and Chemical Toxicology, doi:10.1016/j.fct.2025.115472.
El-Fetouh et al., Experimental Studies on Some Drugs Used in Covid-19 Treatment (Favipiravir and Dexamethasone) in Albino Rats, Journal of Advanced Veterinary Research, 13:10, www.advetresearch.com/index.php/AVR/article/view/1635.
Almutairi et al., Liver Injury in Favipiravir-Treated COVID-19 Patients: Retrospective Single-Center Cohort Study, Tropical Medicine and Infectious Disease, doi:10.3390/tropicalmed8020129.
Siby et al., Temporal Trends in Serious Adverse Events Associated with Oral Antivirals During the COVID-19 Pandemic: Insights from the FAERS Database (2020–2023), Open Forum Infectious Diseases, doi:10.1093/ofid/ofaf695.1825.
Ozhan et al., Evaluation of the cardiopulmonary effects of repurposed COVID-19 therapeutics in healthy rats, Scientific Reports, doi:10.1038/s41598-025-31048-4.
Ülger (B) et al., Evaluation of the effects of favipiravir (T-705) on the lung tissue of healty rats: An experimental study, Food and Chemical Toxicology, doi:10.1016/j.fct.2025.115235.
Zhirnov et al., Favipiravir: the hidden threat of mutagenic action, Journal of microbiology, epidemiology and immunobiology, doi:10.36233/0372-9311-114.
Waters et al., Human genetic risk of treatment with antiviral nucleoside analog drugs that induce lethal mutagenesis: the special case of molnupiravir, Environmental and Molecular Mutagenesis, doi:10.1002/em.22471.
Hadj Hassine et al., Lethal Mutagenesis of RNA Viruses and Approved Drugs with Antiviral Mutagenic Activity, Viruses, doi:10.3390/v14040841.
Shum, C., An investigational study into the drug-associated mutational signature in SARS-CoV-2 viruses, The University of Hong Kong, PhD Thesis, hub.hku.hk/handle/10722/344396.
Shiraki et al., Convenient screening of the reproductive toxicity of favipiravir and antiviral drugs in Caenorhabditis elegans, Heliyon, doi:10.1016/j.heliyon.2024.e35331.
Cenikli et al., Does Favipiravir interact with DNA? Design of electrochemical DNA nanobiosensor to investigate the interaction between DNA and Favipiravir used in the treatment of COVID-19, Talanta, doi:10.1016/j.talanta.2025.128084.
Mihaljevic et al., DNA damage in peripheral blood lymphocytes of severely ill COVID-19 patients in relation to inflammatory markers and parameters of hemostasis, Mutagenesis, doi:10.1093/mutage/geac011.