Mar 1 |
Hydrogen Peroxide reduces COVID-19 risk: real-time meta-analysis of 8 studies (Version 5) | |
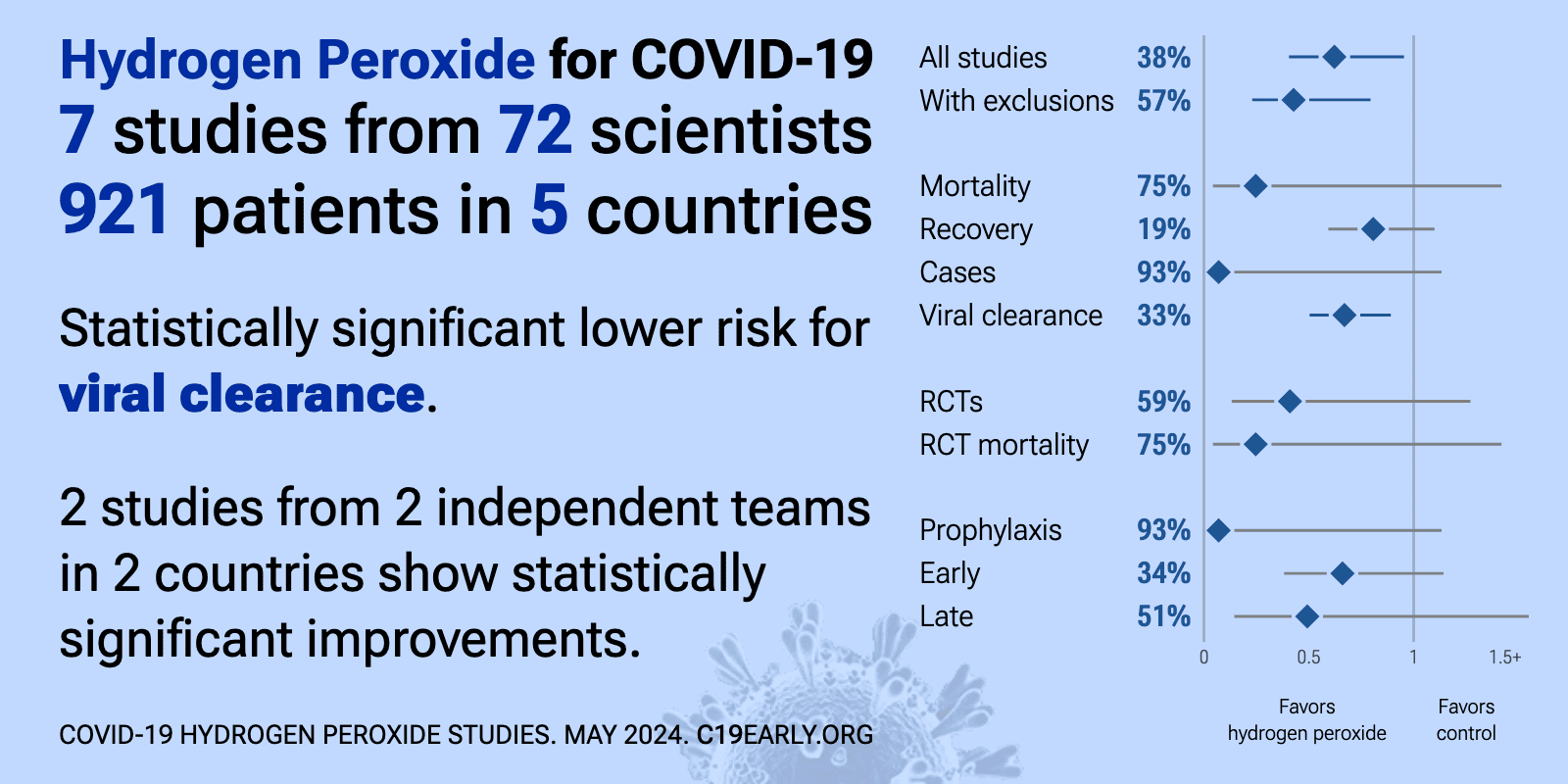
| Significantly lower risk is seen for viral clearance. 2 studies from 2 independent teams in 2 countries show significant benefit. Meta-analysis using the most serious outcome reported shows 39% [6‑60%] lower risk. Results are b.. | ||
Jun 10 2025 |
et al., Japanese Dental Science Review, doi:10.1016/j.jdsr.2025.05.001 | Antiseptics as effective virucidal agents against SARS-CoV-2: Systematic review and Bayesian network meta-analysis |
| Bayesian network meta-analysis of 26 studies evaluating the effectiveness of oral and nasal antiseptics against SARS-CoV-2 viral load, finding that povidone-iodine was the most effective. Hydrogen peroxide and chlorhexidine also showed si.. | ||
Dec 9 2024 |
et al., JDR Clinical & Translational Research, doi:10.1177/23800844241296840 | A Cetylpyridinium Chloride Oral Rinse Reduces Salivary Viral Load in Randomized Controlled Trials |
| 4% improved viral clearance (p=0.98). Two RCTs with a total of 247 recently diagnosed COVID-19 patients showing a significant reduction in salivary SARS-CoV-2 viral load 30 minutes after rinsing with a cetylpyridinium chloride (CPC) mouthwash compared to rinsing with saline o.. | ||
Oct 21 2024 |
et al., Current Research in Microbial Sciences, doi:10.1016/j.crmicr.2024.100293 | Antiseptics: An expeditious third force in the prevention and management of coronavirus diseases |
| Review of the use of nasopharyngeal/oropharyngeal virucidal agents such as povidone-iodine, chlorhexidine, cetylpyridinium chloride, hydrogen peroxide, and others for preventing the spread of COVID-19 and other coronavirus diseases. Autho.. | ||
May 16 2024 |
et al., Journal of Dentistry, doi:10.1016/j.jdent.2024.105082 | Satisfaction with Government Recommended Pre-Procedural Mouth Rinses in the Mitigation of Covid-19 in Hong Kong SAR: A Triple Blind Randomized Controlled Clinical Trial |
| RCT 228 dental patients showing high satisfaction and acceptability of three pre-procedural mouthrinses (povidone-iodine, hydrogen peroxide, and chlorhexidine digluconate) recommended by the Hong Kong government for mitigating COVID-19 tr.. | ||
Feb 19 2024 |
et al., Current Oral Health Reports, doi:10.1007/s40496-024-00368-1 | Antiviral Mechanism and Clinical Benefits of Mouthwash Active Against SARS-CoV-2 |
| Review of antiviral mechanisms and clinical benefits of mouthwashes for SARS-CoV-2, including chlorhexidine (CHX), cetylpyridinium chloride (CPC), ethyl lauroyl arginate (ELA), hydrogen peroxide (HP), povidone-iodine (PVP-I), and anionic.. | ||
Nov 30 2023 |
et al., International Dental Journal, doi:10.1016/j.identj.2023.08.010 | Mouthwash Effects on the Oral Microbiome: Are They Good, Bad, or Balanced? |
| Review of the effects of commonly used mouthwashes on the oral microbiome, which includes bacteria, viruses, bacteriophages, and fungi. While certain mouthwashes have proven antimicrobial actions and clinical effectiveness, more recent me.. | ||
Nov 18 2023 |
et al., NCT04409873 | Antiseptic Mouthwash / Pre-Procedural Rinse on SARS-CoV-2 Load (COVID-19) (AMPoL) |
| 67% improved recovery (p=1). Early terminated RCT with very limited information reported in the registry and only one patient showing symptoms. There is not enough information to assess the viral load results in the registry - the protocol indicates right-censoring f.. | ||
Oct 11 2023 |
et al., Japanese Dental Science Review, doi:10.1016/j.jdsr.2023.09.003 | Efficacy of different mouthwashes against COVID-19: A systematic review and network meta-analysis |
| Systematic review and network meta-analysis evaluating the effectiveness of antiseptic mouthwashes in reducing SARS-CoV-2 viral load in saliva based on data from 14 randomized clinical trials and 21 in vitro studies. The study found that .. | ||
Oct 11 2023 |
et al., BMC Infectious Diseases, doi:10.1186/s12879-023-08669-z | Efficacy of mouthwash on reducing salivary SARS-CoV-2 viral load and clinical symptoms: a systematic review and meta-analysis |
| Systematic review and meta-analysis of 13 randomized controlled trials with a total of 832 participants analyzing the efficacy of mouthwash on reducing salivary SARS-CoV-2 viral load and clinical symptoms in COVID-19 patients. Authors fou.. | ||
Aug 4 2023 |
et al., Scientific Reports, doi:10.1038/s41598-023-39308-x | Efficacy of three antimicrobial mouthwashes in reducing SARS-CoV-2 viral load in the saliva of hospitalized patients: a randomized controlled pilot study |
| RCT 40 late stage (mean 8 days from onset) patients, showing no significant difference in short-term viral load measured by PCR with hydrogen peroxide mouthwash. | ||
Jun 12 2023 |
et al., Biomedicines, doi:10.3390/biomedicines11061694 | Preprocedural Viral Load Effects of Oral Antiseptics on SARS-CoV-2 in Patients with COVID-19: A Systematic Review |
| Systematic review of 14 RCTs, showing significant reductions in short-term viral load with mouth rinses cetylpyridinium chloride, β-cyclodextrin and citrox, hydrogen peroxide, chlorhexidine, povidone-iodine, hypochlorous acid, saline, and.. | ||
Dec 13 2022 |
et al., Journal of Oral Microbiology, doi:10.1080/20002297.2022.2152179 | Antimicrobial oral lavage reduces the SARS-CoV-2 load in intubated patients: randomized clinical trial |
| 72% improved viral clearance (p=0.49). RCT 24 intubated patients treated with hydrogen peroxide + chlorhexidine oral rinse, and 19 with chlorhexidine, showing viral load reductions immediately after and 30/60 minutes later, with statistical significance only for immediate redu.. | ||
Aug 31 2022 |
et al., Journal of Hospital Infection, doi:10.1016/j.jhin.2022.05.007 | Further observations on hydrogen peroxide antisepsis and COVID-19 cases among healthcare workers and inpatients |
| 93% fewer cases (p=0.06). Retrospective 458 healthcare workers in Ghana, showing lower COVID-19 cases with hydrogen peroxide prophylaxis (oral and nasal rinse), without statistical significance. | ||
Jul 31 2022 |
et al., Trials, doi:10.1186/s13063-020-04634-2 | A quadruple blind, randomised controlled trial of gargling agents in reducing intraoral viral load among hospitalised COVID-19 patients: A structured summary of a study protocol for a randomised controlled trial |
| Estimated 50 patient hydrogen peroxide early treatment RCT with results not reported over 3 years after estimated completion. | ||
Jul 31 2022 |
et al., International Journal of Translational Medicine, doi:10.3390/ijtm2030030 | The In Vitro Virucidal Effects of Mouthwashes on SARS-CoV-2 |
| Review of in vitro studies of mouthwashes, showing antiviral activity for SARS-CoV-2 with many compounds including PVP-I, cetylpyridinium chloride, chlorohexidine gluconate, dequalinium chloride, benzalkonium chloride, anionic phthalocyan.. | ||
Jul 28 2022 |
et al., American Journal of Otolaryngology, doi:10.1016/j.amjoto.2022.103549 | Efficacy of antiseptic mouthrinses against SARS-CoV-2: A prospective randomized placebo-controlled pilot study |
| Mouthrinse RCT in Italy comparing short-term viral load after a single 60 second treatment with povidone-iodine, hydrogen peroxide, chlorhexidine, and saline. The greatest efficacy was seen with povidone-iodine, especially for patients wi.. | ||
Jul 27 2022 |
et al., Emerging Microbes & Infections, doi:10.1080/22221751.2022.2098059 | Effect of oral antiseptics in reducing SARS-CoV-2 infectivity: evidence from a randomized double-blind clinical trial |
| 75% improved viral load. RCT hospitalized patients testing viral load shortly after a single mouthwash with PVP-I, hydrogen peroxide, cetylpyridinium chloride, chlorhexidine, and water. For PVP-I, there were only 5 patients with viable virus at baseline. Cross-tr.. | ||
Jul 21 2022 |
et al., Eur. J. Gen. Dent., doi:10.1055/s-0042-1747958 | Reduction in SARS-CoV-2 Oral Viral Load with Prophylactic Mouth Rinse |
| RCT 116 patients in Iran, showing lower short term viral load with mouth rinses chlorhexidine, hydrogen peroxide, and povidone-iodine. Chlorhexidine and hydrogen peroxide were the most effective. | ||
Jun 21 2022 |
et al., West Africa Journal of Medicine, doi:10.55891/wajm.v39i1.98 | Efficacy of Hexetidine, Thymol and Hydrogen Peroxide-Containing Oral Antiseptics in Reducing Sars-Cov-2 Virus in the Oral Cavity: A Pilot Study |
| 66 patient short-term viral load analysis for mouthwashing with hexetidine, thymol, and hydrogen peroxide, reporting improved viral clearance at 2 hours with hydrogen peroxide, without statistical significance. Limited information is prov.. | ||
Apr 5 2022 |
et al., Journal of South Asian Federation of Obstetrics and Gynaecology, doi:10.5005/jp-journals-10006-1986 | Prospective Randomized Double-blind Placebo-controlled Study to Assess the Effects of Nano-ozonized Hydrogen Peroxide Nebulization on Results of RTPCR for Novel Coronavirus thus Infectivity and Clinical Course among Moderately Sick COVID-19 Patients |
| 46% lower need for oxygen therapy (p<0.0001), 36% faster recovery (p<0.0001), and 45% faster viral clearance (p<0.0001). RCT 40 patients in India, showing improved recovery with nebulized hydrogen peroxide. | ||
Feb 28 2022 |
et al., NCT04931004 | Oral Rinse to Reduced Expelled Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) During COVID-19 Infection |
| Estimated 90 patient hydrogen peroxide early treatment RCT with results not reported over 4 years after estimated completion. | ||
Jan 31 2022 |
et al., The Saudi Dental Journal, doi:10.1016/j.sdentj.2022.01.005 | Is hydrogen peroxide an effective mouthwash for reducing the viral load of SARS-CoV-2 in dental clinics? |
| Analysis of hydrogen peroxide use in a dental clinic. Portable air cleaners with HEPA filters were placed in a dental clinic waiting room and treatment rooms. After 3 months, filters were tested for SARS-CoV-2. Virus was detected on filte.. | ||
Jan 28 2022 |
et al., Frontiers in Drug Delivery, doi:10.3389/fddev.2023.1164671 (date from preprint) | On a model-based approach to improve intranasal spray targeting for respiratory viral infections |
| Computational fluid dynamics study of nasal spray administration in 2 subjects showing 100x improvement in nasopharyngeal drug delivery using a new spray placement protocol. The study also found the optimal droplet size range for nasophar.. | ||
Dec 22 2021 |
et al., Scientific Reports, doi:10.1038/s41598-021-03461-y | Clinical evaluation of antiseptic mouth rinses to reduce salivary load of SARS-CoV-2 |
| 32% improved viral load (p=0.7). Small very late (>50% 7+ days from symptom onset, 9 PVP-I patients) RCT testing mouthwashing with cetylpyridinium chloride, chlorhexidine, povidone-iodine, hydrogen peroxide, and distilled water, showing no significant differences. Over 3.. | ||
Oct 25 2021 |
et al., Enfermedades Infecciosas y Microbiología Clínica, doi:10.1016/j.eimc.2021.10.005 | Utility of mouth rinses with povidone-iodine and hydrogen peroxide in patients with COVID-19 |
| 12% improved viral clearance (p=0.67). Small prospective study with 31 patients gargling povidone-iodine, 17 hydrogen peroxide, and 40 control patients, showing lower viral load mid-recovery with povidone-iodine, without reaching statistical significance. Oropharyngeal only, a.. | ||
Aug 3 2021 |
et al., Epidemiology and Health, doi:10.4178/epih.e2021051 | Hydrogen peroxide as an auxiliary treatment for COVID-19 in Brazil: a randomized double-blind clinical trial |
| 34% lower ICU admission (p=1), 1% worse recovery (p=0.97), and 31% lower long COVID (p=0.54). RCT very late treatment (>9 days from onset) comparing hydrogen peroxide + mint essence with water + mint essence, showing no significant differences. | ||
Jul 3 2021 |
et al., Evidence-Based Complementary and Alternative Medicine, doi:10.1155/2021/5592042 | Hydrogen Peroxide as an Adjuvant Therapy for COVID-19: A Case Series of Patients and Caregivers in the Mexico City Metropolitan Area |
| Case series of 23 COVID-19 patients and 28 caregivers in Mexico using hydrogen peroxide treatment and prophylaxis. There was no transmission to caregivers. Patients mainly recovered well, reporting feeling “completely better” at 9.5 days .. | ||
Jun 11 2021 |
et al., The Journal of the American Dental Association, doi:10.1016/j.adaj.2021.05.021 | Estimating salivary carriage of severe acute respiratory syndrome coronavirus 2 in nonsymptomatic people and efficacy of mouthrinse in reducing viral load |
| Small RCT comparing mouthrinsing with saline, 1% hydrogen peroxide, 0.12% chlorhexidine, and 0.5% povidone-iodine, showing significant reductions in salivary viral load for all 4 mouthrinses at 15 and 45 minutes after rinsing. | ||
May 1 2021 |
et al., Epidemiology and Health, doi:10.4178/epih.e2021032 | Effectiveness of hydrogen peroxide as auxiliary treatment for hospitalized COVID-19 patients in Brazil: preliminary results of a randomized double-blind clinical trial |
| 50% lower ICU admission (p=1), 6% greater improvement (p=0.91), and 7% higher hospital discharge (p=0.61). RCT very late treatment (>10 days from onset) comparing hydrogen peroxide + mint essence with water + mint essence, showing no significant differences. | ||
Mar 1 2021 |
et al., medRxiv, doi:10.1101/2021.02.25.21252488 | Povidone iodine, hydrogen peroxide and chlorhexidine mouthwashes reduce SARS-CoV2 burden in whole mouth fluid and respiratory droplets |
| 50% improved viral clearance (p=0.18). Study of SARS-CoV-2 burden in whole mouth fluid and respiratory droplets with povidone iodine, hydrogen peroxide, and chlorhexidine mouthwashes in 36 hospitalized COVID-19 patients using PCR and rapid antigen testing. There were significa.. | ||
Nov 30 2020 |
et al., medRxiv, doi:10.1101/2020.11.27.20234997 | A Randomized trial on the regular use of potent mouthwash in COVID-19 treatment |
| 86% lower mortality (p=0.24), 86% lower ventilation (p=0.24), and 18% improved viral clearance (p=0.16). RCT for mouthwash containing hydrogen peroxide 2% and chlorhexidine gluconate, showing higher discharge, shorter hospital stay, less intubation, and lower mortality with treatment. | ||
Jun 5 2020 |
et al., Function, doi:10.1093/function/zqaa002 | Potential Role of Oral Rinses Targeting the Viral Lipid Envelope in SARS-CoV-2 Infection |
| Review of the mechanisms of action and studies supporting oral rinsing for the prevention of transmission of SARS-CoV-2, including chlorhexidine, cetylpyridinium chloride, hydrogen peroxide, and povidone-iodine. | ||