Feb 21 |
Colchicine reduces COVID-19 risk: real-time meta-analysis of 54 studies (Version 67) | |
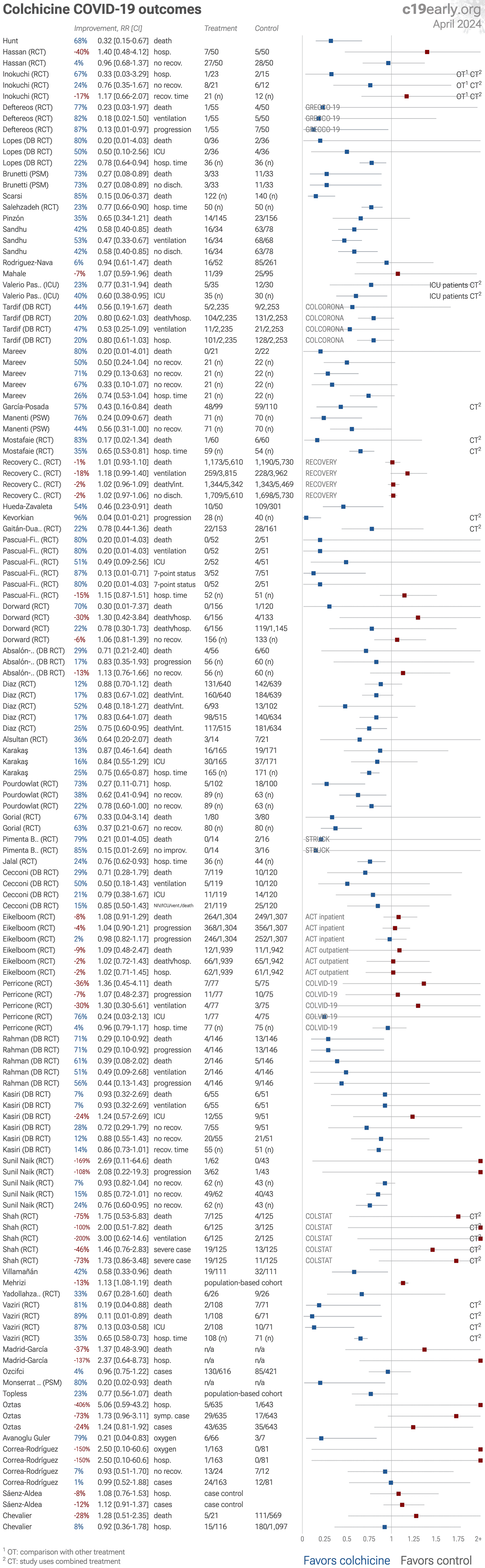
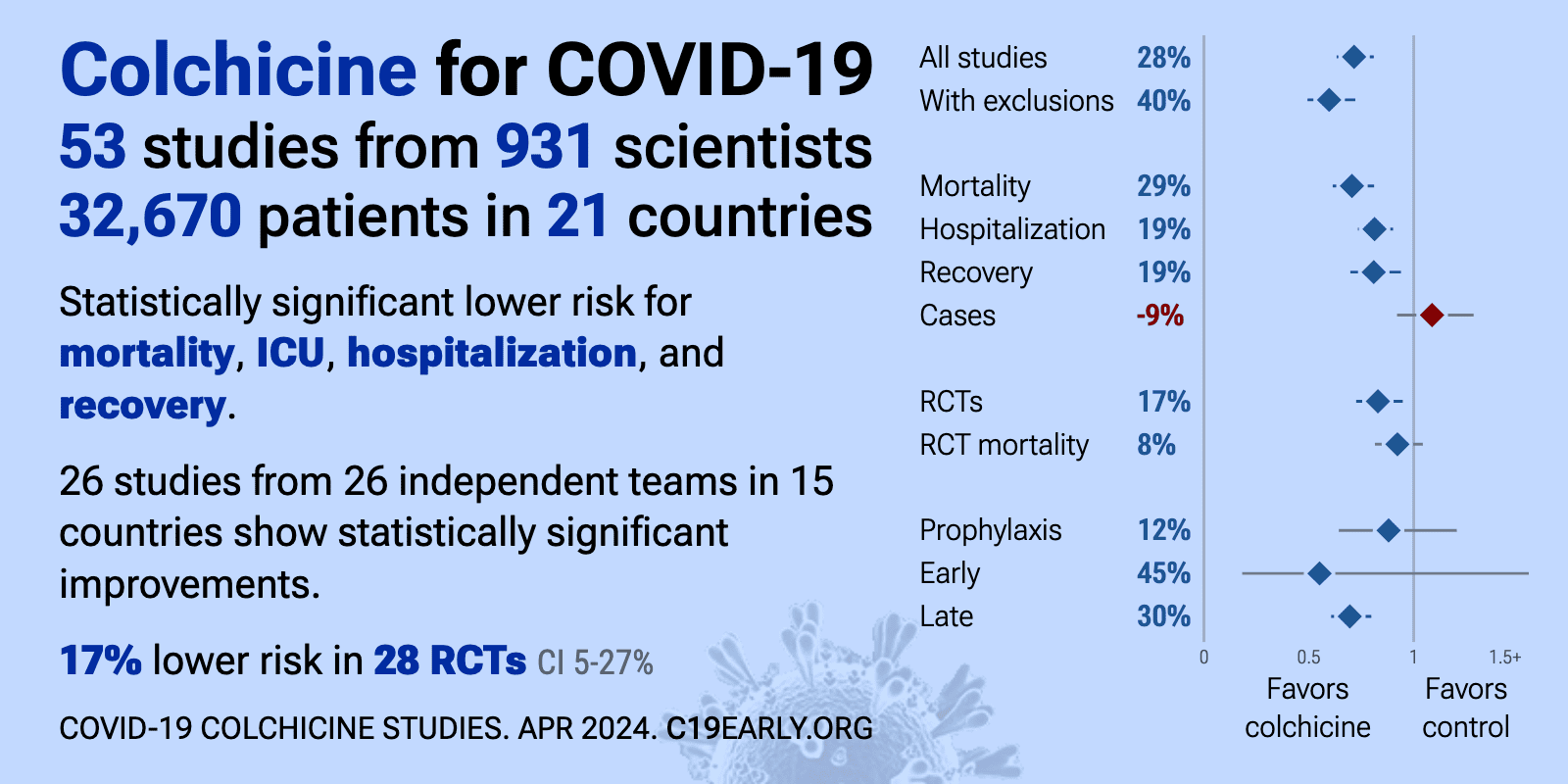
| Significantly lower risk is seen for mortality, ICU admission, hospitalization, and recovery. 24 studies from 24 independent teams in 14 countries show significant benefit. Meta-analysis using the most serious outcome reported shows.. | ||
Oct 20 2025 |
et al., JAMA Internal Medicine, doi:10.1001/jamainternmed.2025.5408 | Effectiveness of Colchicine for the Treatment of Long COVID |
| 16% lower long COVID (p=0.01). RCT 346 long COVID patients in India, showing no significant difference in functional capacity, respiratory function, or inflammatory markers with colchicine. | ||
Sep 2 2025 |
et al., medRxiv, doi:10.1101/2025.08.29.25334732 | Long-term follow-up of treatment comparisons in RECOVERY: a randomised, open-label, platform trial for patients hospitalised with COVID-19 |
| 6-month followup of RECOVERY patients. Results are reported within the respective trials for each treatment. | ||
Apr 15 2025 |
, V., MDPI AG, doi:10.20944/preprints202504.1220.v1 | Prevention and Treatment of COVID-19 and Influenza with Bromhexine and High Doses of Colchicine |
| Review of bromhexine and colchicine for COVID-19 and influenza prevention and treatment. | ||
Aug 24 2024 |
et al., Journal of Clinical Medicine, doi:10.3390/jcm13175013 | Prevalence and Risk Factors of Headache Associated with COVID-19 |
| 98% lower long COVID (p=1) and 28% improvement (p=1). Retrospective 295 hospitalized COVID-19 patients in Slovakia showing 35% prevalence of headache, of which 41% of patients had persistent headache 12-15 months after infection. Authors' analysis of long COVID headache is only for the subgr.. | ||
Aug 11 2024 |
et al., Cells, doi:10.3390/cells13161331 | Spike Protein of SARS-CoV-2 Activates Cardiac Fibrogenesis through NLRP3 Inflammasomes and NF-κB Signaling |
| In vitro study showing that the SARS-CoV-2 spike protein can activate cardiac fibroblasts through ACE2-dependent mechanisms, leading to cardiac fibrosis via the NLRP3 inflammasome and NF-κB signaling pathways. The results suggest that COV.. | ||
May 28 2024 |
et al., Journal of Cardiovascular Medicine, doi:10.2459/JCM.0000000000001639 | Edoxaban and/or colchicine for patients with coronavirus disease 2019 managed in the out-of-hospital setting (CONVINCE): a randomized clinical trial |
| 4% higher hospitalization (p=0.98), 5% higher need for oxygen therapy (p=0.97), 40% improvement (p=0.97), and 11% improved viral clearance (p=0.77). Early terminated RCT with 14 colchicine, 13 edoxaban, 16 colchicine+edoxaban, and 16 control patients, showing no significant difference in outcomes with treatment up to 7 days after PCR diagnosis. | ||
May 15 2024 |
et al., Cureus, doi:10.7759/cureus.60364 | Colchicine and/or Naltrexone for Hospitalized COVID-19 Patients Not Requiring High Levels of Ventilatory Support (COLTREXONE): A Prospective, Randomized, Open-Label Trial |
| 65% lower ICU admission (p=0.11), 43% improved recovery (p=0.14), 34% lower need for oxygen therapy (p=0.34), and 20% shorter hospitalization (p=0.13). Open-label RCT 137 hospitalized COVID-19 patients, showing lower progression to ICU/step-down ICU and improved recovery with colchicine, both without statistical significance. The primary outcome was changed mid-trial due to the low numbe.. | ||
Apr 20 2024 |
et al., BMC Pulmonary Medicine, doi:10.1186/s12890-024-03001-0 | The role of colchicine in the management of COVID-19: a meta-analysis |
| 65% lower mortality (p=0.01), 60% lower ventilation (p=0.09), 71% lower ICU admission (p=0.08), and 93% lower need for oxygen therapy (p<0.0001). Systematic review and meta-analysis of 8 studies (4 RCTs) involving 16,488 COVID-19 patients showed significantly lower mortality and need for oxygen therapy with colchicine. | ||
Apr 13 2024 |
et al., Cureus, doi:10.7759/cureus.58164 | High-Dose Colchicine: Key Factor in the Treatment of Morbidly Obese COVID-19 Patients |
| Case series of 3 morbidly obese COVID-19 patients, 2 outpatients and 1 hospitalized, showing rapid recovery with a therapeutic regimen including high-dose colchicine (5 mg loading dose followed by 1-3 mg daily maintenance dose). Authors h.. | ||
Mar 19 2024 |
et al., The Kurume Medical Journal, doi:10.2739/kurumemedj.MS7012003 | Oral Colchicine and Low-Dose Aspirin Combination Therapy for Non-elderly, Non-severe, Early Time From Onset, Adult Outpatients with Coronavirus Disease 2019 (COVID-19) during “The Fifth Pandemic Wave” in Japan |
| 67% lower hospitalization (p=0.55) and 24% improved recovery (p=0.72). RCT 38 low risk outpatients in Japan, showing no significant differences for colchicine and low-dose aspirin compared to loxoprofen. Hospitalization was lower, without statistical significance (4.3% vs. 13.3%, p=0.34). There were no criti.. | ||
Mar 6 2024 |
et al., Heliyon, doi:10.1016/j.heliyon.2024.e27373 | Investigating efficacy of colchicine plus phenolic monoterpenes fraction as a potential treatment for patients diagnosed with COVID-19: A randomized controlled parallel clinical trial |
| 81% lower mortality (p=0.03), 87% lower ICU admission (p=0.002), and 35% shorter hospitalization (p<0.0001). RCT 179 hospitalized COVID-19 patients showing lower mortality, ICU admission, and hospitalization duration with colchicine plus phenolic monoterpenes compared to standard care alone. The intervention group received 0.8 mg/day colchicine .. | ||
Feb 29 2024 |
et al., Coronaviruses, doi:10.2174/0126667975271636231109051950 | Colchicine with Infliximab Compared to Infliximab in Hospitalized Patients with COVID-19 Pneumonia: An Open-label Randomized Trial |
| 33% lower mortality (p=0.54). Open-label RCT with 52 severe COVID-19 pneumonia patients showing no significant differences in mortality with colchicine. All patients received infliximab and remdesivir. | ||
Dec 18 2023 |
et al., Frontiers in Public Health, doi:10.3389/fpubh.2023.1280434 | Drug prescription patterns and their association with mortality and hospitalization duration in COVID-19 patients: insights from big data |
| 13% higher mortality (p<0.0001). Retrospective study of 917,198 hospitalized COVID-19 cases covered by the Iran Health Insurance Organization over 26 months showing that antithrombotics, corticosteroids, and antivirals reduced mortality while diuretics, antibiotics, and.. | ||
Oct 20 2023 |
, V., Pharmacia, doi:10.3897/pharmacia.70.e112550 | Comparison of treatment of COVID-19 with inhaled bromhexine, higher doses of colchicine and hymecromone with WHO-recommended paxlovid, molnupiravir, remdesivir, anti-IL-6 receptor antibodies and baricitinib |
| Review of treatment of COVID-19 with inhaled bromhexine, higher doses of colchicine and hymecromone compared to WHO-recommended paxlovid, molnupiravir, remdesivir, anti-IL-6 receptor antibodies, and baricitinib. The author argues that the.. | ||
Jun 13 2023 |
et al., Research Square, doi:10.21203/rs.3.rs-3049708/v1 | The effects of probiotic Lactobacillus acidophilus and colchicine on the control of symptoms, duration, and disease progression of mild and moderate cases of COVID-19: A randomized controlled clinical trial |
| 40% higher hospitalization (p=0.76) and 4% improved recovery (p=1). RCT 150 patients in Egypt showing no significant difference in outcomes with colchicine. SOC included vitamin C, D, and zinc. Colchicine 0.5mg tid days 1-3, bid days 4-7. | ||
May 17 2023 |
et al., Elsevier BV, doi:10.2139/ssrn.4447127 | Does Colchicine Reduce Mortality in Patients with Covid-19 Clinical Syndrome? An Umbrella Review of Published Meta-Analyses |
| 32% lower mortality (p<0.0001). Umbrella review of 18 colchicine meta analyses, showing significantly lower COVID-19 mortality with colchicine. | ||
Mar 23 2023 |
et al., Eur. J. Hosp. Pharm., doi:10.1136/ejhpharm-2023-eahp.56 | Targeting patients with pneumonia by COVID-19 that could be beneficiated by colchicine |
| 42% lower mortality (p=0.03). Retrospective 111 hospitalized COVID-19 pneumonia patients treated with colchicine and 111 matched controls, showing lower mortality with colchicine treatment. | ||
Mar 22 2023 |
et al., Frontiers in Medicine, doi:10.3389/fmed.2023.1152587 | CovAID: Identification of factors associated with severe COVID-19 in patients with inflammatory rheumatism or autoimmune diseases |
| 28% higher mortality (p=0.54) and 8% lower hospitalization (p=0.83). Retrospective 1,213 rheumatic disease patients in France, showing no significant difference with colchicine use in univariate analysis. | ||
Feb 24 2023 |
et al., BMJ Open, doi:10.1136/bmjopen-2022-067910 | Colchicine and high-intensity rosuvastatin in the treatment of non-critically ill patients hospitalised with COVID-19: a randomised clinical trial |
| 75% higher mortality (p=0.54), 200% higher ventilation (p=0.28), and 46% higher severe cases (p=0.34). RCT 250 late stage (80% on oxygen) hospitalized patients in the USA, showing no significant differences with combined colchicine/rosuvastatin treatment. There was a trend towards increased risk, which authors note may be due to chance bec.. | ||
Jan 21 2023 |
et al., Contemporary Clinical Trials Communications, doi:10.1016/j.conctc.2023.101070 | Effect of colchicine and aspirin given together in patients with moderate COVID-19 |
| 7% improved recovery (p=0.21). RCT 122 hospitalized patients in India, showing improved recovery with colchicine treatment. All patients received aspirin. There was one death and higher progression in the colchicine arm, however 3 patients in the colchicine arm had bas.. | ||
Jan 16 2023 |
et al., Journal of Investigative Medicine, doi:10.1177/10815589221141815 | The effects of colchicine on hospitalized COVID-19 patients: A randomized, double-blind, placebo-controlled clinical trial |
| 7% lower mortality (p=1), 7% lower ventilation (p=1), 24% higher ICU admission (p=0.63), and 28% improved recovery (p=0.59). Very late treatment (10 days from onset) RCT 110 patients in Iran, showing no significant difference in outcomes with colchicine. Colchicine 2mg loading dose followed by 0.5mg bid for 7 days. | ||
Jan 13 2023 |
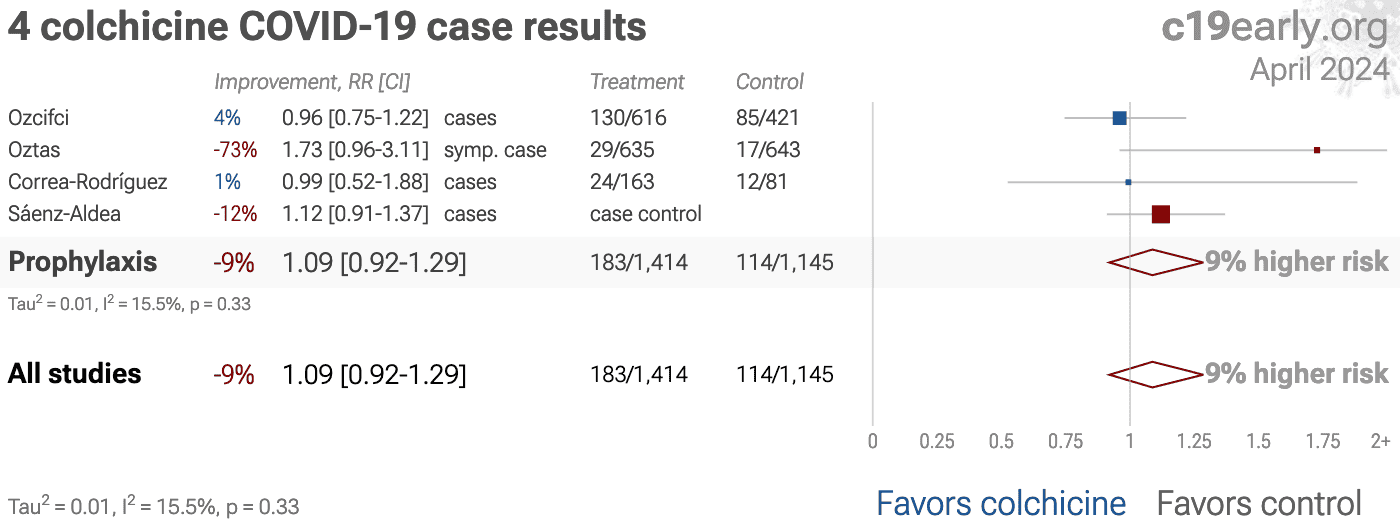
et al., Journal of Medical Virology, doi:10.1002/jmv.28496 | Colchicine and risk of hospitalisation due to COVID-19: a population-based study |
| 8% higher hospitalization (p=0.68) and 12% more cases (p=0.68). Retrospective 86,652 patients in Spain, showing no significant difference in cases and hospitalization with colchicine use. The different risk for patients prescribed colchicine may not be fully adjusted for. See [onlinelibrary.wiley.com]. | ||
Dec 31 2022 |
et al., Journal of Physiology and Pharmacology, doi:10.26402/jpp.2022.3.09 | Colchicine anti-inflammatory therapy for non-intensive care unit hospitalized COVID-19 patients: results from a pilot open-label, randomized controlled clinical trial |
| 34% improved recovery (p=0.11). Open-label RCT 96 hospitalized COVID-19 patients in Pakistan showing no significant difference in clinical outcomes with colchicine treatment, however baseline severity was not comparable - 85% vs. 56% had SpO2 <93 (p = 0.003), with the Q.. | ||
Dec 13 2022 |
et al., PeerJ, doi:10.7717/peerj.14290 | Determination of PaO2/FiO2 after 24 h of invasive mechanical ventilation and ΔPaO2/FiO2 at 24 h as predictors of survival in patients diagnosed with ARDS due to COVID-19 |
| 33% higher mortality (p=0.33). Retrospective 200 patients with ARDS due to COVID-19 on invasive mechanical ventilation, showing no significant difference in mortality with colchicine treatment. The Cox proportional hazards result is from [journals.plos.org]. | ||
Nov 16 2022 |
et al., PLOS ONE, doi:10.1371/journal.pone.0277790 | Efficacy of colchicine in patients with moderate COVID-19: A double-blinded, randomized, placebo-controlled trial |
| 71% lower mortality (p=0.04) and 71% lower progression (p=0.04). RCT 300 patients in Bangladesh, published 2 years after completion, showing significantly lower mortality with treatment at 28 days (not significant at 14 days). 1.2mg colchicine on day 1 followed by 0.6mg for 13 days. | ||
Oct 31 2022 |
et al., European Journal of Internal Medicine, doi:10.1016/j.ejim.2022.10.016 | Treatment with COLchicine in hospitalized patients affected by COVID-19: the COLVID-19 trial |
| 36% higher mortality (p=0.77), 7% higher progression (p=1), 76% lower ICU admission (p=0.21), and 4% shorter hospitalization (p=0.69). RCT 152 hospitalized patients in Italy, showing no significant difference in outcomes with colchicine treatment. Table 2 shows 13% of patients treated with antivirals in the colchicine arm, however 16.9% were treated with one specific ant.. | ||
Oct 10 2022 |
et al., The Lancet Respiratory Medicine, doi:10.1016/S2213-2600(22)00299-5 | Colchicine and aspirin in community patients with COVID-19 (ACT): an open-label, factorial, randomised, controlled trial |
| 9% higher mortality (p=0.84), 2% higher combined mortality/hospitalization (p=0.93), and 2% higher hospitalization (p=0.92). Late (5.4 days) outpatient RCT showing no significant difference in outcomes with colchicine treatment. Authors include a meta analysis of 6 colchicine RCTs, however there were 19 RCTs as of the publication date [c19colchicine.com]. | ||
Oct 10 2022 |
et al., The Lancet Respiratory Medicine, doi:10.1016/S2213-2600(22)00298-3 | Colchicine and the combination of rivaroxaban and aspirin in patients hospitalised with COVID-19 (ACT): an open-label, factorial, randomised, controlled trial |
| 8% higher mortality (p=0.38) and 4% higher progression (p=0.58). RCT very late stage (baseline SpO2 80%) patients, showing no significant differences with colchicine treatment. | ||
Sep 29 2022 |
et al., Clinical Drug Investigation, doi:10.1007/s40261-022-01201-2 | FRAGILE-COLCOVID19: A Clinical Trial Based on Early Administration of an Oral Combination of Colchicine and Prednisone in Elderly Patients with COVID-19 in Geriatric Facilities |
| 16% higher mortality (p=1) and 42% improvement (p=0.25). RCT 54 elderly patients in Spain comparing colchicine + prednisone vs. dexamethasone, showing lower combined mortality/therapeutic failure with colchicine + prednisone, but no significant difference in mortality. Data appears unreliable, .. | ||
Sep 19 2022 |
et al., Medicina Clínica (English Edition), doi:10.1016/j.medcle.2022.08.009 | Clinical course of Covid-19 in a cohort of patients with Behçet disease |
| 150% higher need for oxygen therapy (p=1), 150% higher hospitalization (p=1), 7% improved recovery (p=1), and 1% fewer cases (p=1). Retrospective 244 Behçet disease patients in Spain, showing no significant difference in outcomes with colchicine treatment. Confounding by indication may significantly affect results - colchicine may be prescribed more often for more ser.. | ||
Jul 27 2022 |
et al., Journal of Advances in Medicine and Medical Research, doi:10.9734/jammr/2022/v34i2031503 | The Potential Role of Colchicine in Reducing Mortality and Mechanical Ventilation Rates in COVID-19 Infection: A Meta-analysis |
| 37% lower mortality (p=0.001). Meta analysis of 12 colchicine studies, showing significantly lower mortality with treatment. | ||
Jul 21 2022 |
et al., Modern Rheumatology, doi:10.1093/mr/roac074 | COVID-19 in familial Mediterranean fever: Clinical course and complications related to primary disease |
| 79% lower need for oxygen therapy (p=0.04). Retrospective 73 familial Mediterranean fever patients with COVID-19 in Turkey, showing significantly higher risk of hospitalization for respiratory support with non-adherence to colchicine treatment before the infection. | ||
Jun 29 2022 |
et al., Journal of General Internal Medicine, doi:10.1007/s11606-022-07701-3 | Medications Associated with Lower Mortality in a SARS-CoV-2 Positive Cohort of 26,508 Veterans |
| 68% lower mortality (p=0.003). Retrospective 26,508 consecutive COVID+ veterans in the USA, showing lower mortality with multiple treatments including colchicine. Treatment was defined as drugs administered ≥50% of the time within 2 weeks post-COVID+, and may be a cont.. | ||
Jun 2 2022 |
et al., Scientific Reports, doi:10.1038/s41598-022-13424-6 | Efficacy of short-course colchicine treatment in hospitalized patients with moderate to severe COVID-19 pneumonia and hyperinflammation: a randomized clinical trial |
| 29% lower mortality (p=0.62), 50% lower ventilation (p=0.29), 21% lower ICU admission (p=0.67), and 15% improvement (p=0.62). RCT 240 hospitalized patients with COVID-19 pneumonia, mean 9 days from the onset of symptoms, showing no significant differences with colchicine treatment. EudraCT 2020-001841-38. | ||
May 5 2022 |
et al., Indian Journal of Rheumatology, doi:10.4103/injr.injr_264_21 | Effectiveness of colchicine among patients with COVID-19 infection: A randomized, open-labeled, clinical trial |
| 24% shorter hospitalization (p=0.009). Open label RCT of colchicine showing improved recovery with treatment. Only the abstract is currently available. Colchicine 0.5mg bid for 14 days. | ||
Apr 28 2022 |
et al., Revista da Sociedade Brasileira de Medicina Tropical, doi:10.1590/0037-8682-0565-2022 (date from preprint) | Efficacy and safety of Ixekizumab vs. low-dose IL-2 vs. Colchicine vs. standard of care in the treatment of patients hospitalized with moderate-to-critical COVID-19: A pilot randomized clinical trial (STRUCK: Survival Trial Using Cytokine Inhibitors) |
| 85% greater improvement (p=0.23). Open label RCT late stage hospitalized patients in Brazil with 14 colchicine and 16 SOC patients, showing lower mortality and improved recovery with treatment, without statistical significance. Authors note that the colchicine group had o.. | ||
Apr 12 2022 |
et al., Annals of Medicine and Surgery, doi:10.1016/j.amsu.2022.103593 | Randomized controlled trial of colchicine add on to the standard therapy in moderate and severe corona virus Disease-19 infection |
| 63% improved recovery (p=0.001). RCT with 80 colchicine and 80 control patients, showing improved recovery with treatment. SOC included vitamin C, vitamin D, and zinc. | ||
Apr 5 2022 |
et al., PLOS ONE, doi:10.1371/journal.pone.0266245 | Safety and efficacy of colchicine in COVID-19 patients: A systematic review and meta-analysis of randomized control trials |
| Meta analysis of 5 colchicine RCTs (currently there are RCTs) finding that treatment significantly reduced COVID-19 severity. | ||
Mar 21 2022 |
et al., Journal of Medical Virology, doi:10.1002/jmv.27731 | Frequency and Severity of COVID-19 in Patients with Various Rheumatic Diseases Treated Regularly with Colchicine or Hydroxychloroquine |
| 406% higher hospitalization (p=0.12), 73% more symptomatic cases (p=0.07), and 24% more cases (p=0.35). Retrospective 635 HCQ users and 643 household contacts, showing higher risk with colchicine in unadjusted results. Patients with conditions leading to the use of colchicine may have significantly different baseline risk, e.g. [Topless]. | ||
Feb 2 2022 |
et al., Phytotherapy Research, doi:10.1002/ptr.7319 | Efficacy and safety of colchicine treatment in patients with COVID-19: A prospective, multicenter, randomized clinical trial |
| 73% lower hospitalization (p=0.004) and 38% improved recovery (p=0.03). RCT 202 patients in Iran, 102 treated with colchicine, showing lower hospitalization and improved clinical outcomes with treatment. | ||
Jan 31 2022 |
et al., The Journal of Infection in Developing Countries, doi:10.3855/jidc.14924 | Reducing length of hospital stay with colchicine |
| 13% lower mortality (p=0.72), 16% lower ICU admission (p=0.5), and 25% shorter hospitalization (p=0.0001). Retrospective 356 hospitalized COVID-19 patients, shorter hospitalization time with colchicine treatment. There were no statistically significant differences for mortality or ICU admission. Significantly lower mortality was seen with high.. | ||
Jan 28 2022 |
et al., The Lancet Rheumatology, doi:10.1016/S2665-9913(21)00401-X | Gout and the risk of COVID-19 diagnosis and death in the UK Biobank: a population-based study |
| 23% lower mortality (p=0.12). UK Biobank retrospective showing a higher risk of COVID-19 cases and mortality for patients with gout. Among patients with gout, mortality risk was lower for those on colchicine, OR 1.06 [0.60-1.89], compared to those without colchicine, .. | ||
Jan 12 2022 |
et al., Diabetes & Metabolic Syndrome: Clinical Research & Reviews, doi:10.1016/j.dsx.2022.102395 | Effect of colchicine on mortality in patients with COVID-19 – A systematic review and meta-analysis |
| Systematic review and meta analysis showing that colchicine was associated with lower mortality in COVID-19 patients: All studies: RR 0.66 [95%CI 0.53, 0.83], p < 0.001; I2: 42% RCTs: RR 0.81 [95%CI 0.54, 1.20], p = 0.29; I2: 10% The RCT .. | ||
Jan 8 2022 |
et al., Pharmaceuticals, doi:10.3390/ph15010078 | A Case-Control of Patients with COVID-19 to Explore the Association of Previous Hospitalisation Use of Medication on the Mortality of COVID-19 Disease: A Propensity Score Matching Analysis |
| 80% lower mortality (p=0.02). PSM retrospective 3,712 hospitalized patients in Spain, showing lower mortality with existing use of azithromycin, bemiparine, budesonide-formoterol fumarate, cefuroxime, colchicine, enoxaparin, ipratropium bromide, loratadine, mepyramine.. | ||
Dec 31 2021 |
et al., Interdisciplinary Perspectives on Infectious Diseases, doi:10.1155/2021/2129006 | Efficacy of Colchicine and Budesonide in Improvement Outcomes of Patients with Coronavirus Infection 2019 in Damascus, Syria: A Randomized Control Trial |
| 36% lower mortality (p=0.7) and 20% shorter hospitalization. Small RCT 49 severe condition hospitalized patients in Syria, showing lower mortality with colchicine and shorter hospitalization time with both colchicine and budesonide (all of these were not statistically significant). | ||
Dec 30 2021 |
et al., Immunity, Inflammation and Disease, doi:10.1002/iid3.562 | The effect of colchicine on mortality outcome and duration of hospital stay in patients with COVID‐19: A meta‐analysis of randomized trials |
| Meta-analysis of 10 randomized controlled trials with 17,976 COVID-19 patients showing significantly shorter hospitalization with colchicine treatment. Mortality was lower but without statistical significance. | ||
Dec 29 2021 |
et al., JAMA Network Open, doi:10.1001/jamanetworkopen.2021.41328 | Effect of Colchicine vs Usual Care Alone on Intubation and 28-Day Mortality in Patients Hospitalized With COVID-19 |
| 12% lower mortality (p=0.3) and 17% lower combined mortality/intubation (p=0.08). Very late stage RCT (O2 88%, 84% on oxygen) with 1,279 hospitalized patients in Argentina, showing lower mortality and lower combined mortality/ventilation, statistically significant only for the combined outcome and per-protocol analysis.. | ||
Nov 25 2021 |
et al., Rheumatology International, doi:10.1007/s00296-021-05056-2 | The incidence, clinical characteristics, and outcome of COVID-19 in a prospectively followed cohort of patients with Behçet’s syndrome |
| 4% fewer cases (p=0.72). Prospective analysis of 1,047 Behçet’s syndrome patients in Turkey, showing no significant difference in cases with colchicine use. | ||
Nov 9 2021 |
et al., Journal of General Internal Medicine, doi:10.1007/s11606-021-07203-8 | Colchicine Is Safe Though Ineffective in the Treatment of Severe COVID-19: a Randomized Clinical Trial (COLCHIVID) |
| 29% lower mortality (p=0.74), 17% lower progression (p=0.67), and 13% worse recovery (p=0.59). Very late stage RCT with 56 colchicine and 60 control patients in Mexico, showing no significant differences. | ||
Sep 23 2021 |
et al., British Journal of General Practice, doi:10.3399/BJGP.2022.0083 (date from preprint) | Colchicine for COVID-19 in the community (PRINCIPLE): a randomised, controlled, adaptive platform trial |
| 70% lower mortality (p=0.43), 30% higher combined mortality/hospitalization (p=0.66), and 6% worse recovery (p=0.67). Late treatment RCT with 156 colchicine patients in the UK, showing no significant differences. c19 early .org PRINCIPLE trial selective reporting delays Results for effective but politically inconvenient treatments were withheld for very .. | ||
Sep 11 2021 |
et al., International Journal of General Medicine, doi:10.2147/IJGM.S329810 | Colchicine in Recently Hospitalized Patients with COVID-19: A Randomized Controlled Trial (COL-COVID) |
| 80% lower mortality (p=0.24), 80% lower ventilation (p=0.24), 87% improved 7-point scale results (p=0.03), and 15% longer hospitalization (p=0.34). RCT with 52 colchicine patients and 51 control patients, showing lower risk of clinical deterioration with treatment. COL-COVID. NCT04350320. | ||
Aug 23 2021 |
et al., Life, doi:10.3390/life11080864 | Repurposing Colchicine in Treating Patients with COVID-19: A Systematic Review and Meta-Analysis |
| 43% lower mortality (p=0.008) and 33% lower ventilation (p=0.15). Meta analysis of 11 colchicine studies showing significantly lower mortality with treatment. | ||
Jul 18 2021 |
et al., European Journal of Clinical Investigation, doi:10.1111/eci.13645 | Colchicine use might be associated with lower mortality in COVID‐19 patients: A meta‐analysis |
| 65% lower mortality (p<0.0001). Meta analysis of 9 colchicine studies showing significantly lower mortality with treatment. | ||
Jul 10 2021 |
et al., eClinicalMedicine, doi:10.1016/j.eclinm.2021.101242 | Effectiveness of rosuvastatin plus colchicine, emtricitabine/tenofovir and combinations thereof in hospitalized patients with COVID-19: a pragmatic, open-label randomized trial |
| 22% lower mortality (p=0.38). RCT 633 hospitalized patients in Colombia, 153 treated with colchicine + rosuvastatin, 160 treated with emtricitabine + tenofovir, and 159 treated with the combination of both regimens. Statistically significant improvement was seen only .. | ||
Jul 10 2021 |
et al., International Journal of Immunopathology and Pharmacology, doi:10.1177/20587384211031763 | The effectiveness of Colchicine as an anti-inflammatory drug in the treatment of coronavirus disease 2019: Meta-analysis |
| 36% lower mortality (p<0.0001). Meta analysis of 10 studies showing significantly lower COVID-19 mortality with colchicine. | ||
Jun 30 2021 |
et al., Journal of Infection, doi:10.1016/j.jinf.2021.02.008 | Oral corticoid, aspirin, anticoagulant, colchicine, and furosemide to improve the outcome of hospitalized COVID-19 patients - the COCAA-COLA cohort study |
| 96% lower progression (p=0.0005). Observational study in France with 28 hospitalized patients treated with prednisone/furosemide/colchicine/salicylate/direct anti-Xa inhibitor, and 40 control patients, showing lower combined mortality, ventilation, or high-flow oxygen the.. | ||
Jun 18 2021 |
et al., BMJ Open, doi:10.1136/bmjopen-2020-046799 | Platform Randomised trial of INterventions against COVID-19 In older peoPLE (PRINCIPLE): protocol for a randomised, controlled, open-label, adaptive platform, trial of community treatment of COVID-19 syndromic illness in people at higher risk |
| Protocol paper for the PRINCIPLE trial. For the colchicine arm see [Dorward], for budesonide see [Yu], and for ivermectin see [Hayward]. | ||
Jun 10 2021 |
et al., Revista Peruana de Medicina Experimental y Salud Pública, doi:10.17843/rpmesp.2021.382.7158 | Factores asociados a la muerte por COVID-19 en pacientes admitidos en un hospital público en Tacna, Perú |
| 54% lower mortality (p=0.03). Retrospective 450 late stage (median oxygen saturation 86%) COVID+ hospitalized patients in Peru, showing lower mortality with colchicine treatment. | ||
May 18 2021 |
et al., The Lancet Respiratory Medicine, doi:10.1016/S2213-2600(21)00435-5 (date from preprint) | Colchicine in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial |
| 1% higher mortality (p=0.85), 18% higher ventilation (p=0.06), 2% higher combined mortality/intubation (p=0.47), and 2% lower hospital discharge (p=0.44). RCT with 5,610 colchicine and 5,730 control patients showing mortality RR 1.01 [0.93-1.10]. Very late stage treatment, median 9 days after symptom onset, baseline 32% ventilation (5% invasive). ISRCTN 50189673. 6-month results are from [.. | ||
Apr 30 2021 |
et al., The American Journal of Cardiology, doi:10.1016/j.amjcard.2021.02.005 | Meta-analysis of the Effect of Colchicine on Mortality and Mechanical Ventilation in COVID-19 |
| 38% lower mortality (p=0.0004) and 25% lower ventilation (p=0.27). Meta analysis of 8 studies, showing significantly lower COVID-19 mortality with colchicine. | ||
Mar 24 2021 |
et al., PLOS ONE, doi:10.1371/journal.pone.0248276 | Reduced mortality in COVID-19 patients treated with colchicine: Results from a retrospective, observational study |
| 76% lower mortality (p=0.005) and 44% improved recovery (p=0.05). IPTW retrospective 141 COVID-19 patients (83% hospitalized), 71 treated with colchicine and 70 matched control patients, showing lower mortality and faster recovery with treatment. | ||
Mar 14 2021 |
et al., Clinical and Experimental Pharmacology and Physiology, doi:10.1111/1440-1681.13488 | Colchicine treatment can improve outcomes of coronavirus disease 2019 (COVID-19): A systematic review and meta-analysis |
| Meta analysis concluding that colchicine can reduce severity and mortality in COVID-19 patients, mortality OR 0.43 [0.32-0.58]. | ||
Mar 6 2021 |
et al., Journal of Infection and Public Health, doi:10.1016/j.jiph.2021.02.013 | Clinical outcomes of patients hospitalized for COVID-19 and evidence-based on the pharmacological management reduce mortality in a region of the Colombian Caribbean |
| 57% lower mortality (p=0.01). Retrospective 209 hospitalized patients in Colombia, showing lower mortality with antibiotics + LMWH + corticosteroids + colchicine in multivariable analysis. | ||
Feb 28 2021 |
et al., Kardiologiia, doi:10.18087/cardio.2021.2.n1560 | Proactive anti-inflammatory therapy with colchicine in the treatment of advanced stages of new coronavirus infection. The first results of the COLORIT study |
| 50% improved recovery (p=0.06) and 26% shorter hospitalization (p=0.08). Small trial with 21 colchicine patients and 22 control patients in Russia, showing improved recovery with treatment. The trial was originally an RCT, however randomization to the control arm was stopped after 5 patients, and 17 retrospect.. | ||
Jan 31 2021 |
et al., Therapeutic Advances in Musculoskeletal Disease, doi:10.1177/1759720x211002684 | Influence of colchicine prescription in COVID-19-related hospital admissions: a survival analysis |
| 37% higher mortality (p=0.57) and 137% higher hospitalization (p=0.2). Retrospective 9,379 patients attending a rheumatology outpatient clinic in Spain, showing higher mortality and hospitalization with colchicine use, without statistical significance. | ||
Jan 27 2021 |
et al., The Lancet Respiratory Medicine, doi:10.1016/S2213-2600(21)00222-8 (date from preprint) | Colchicine for community-treated patients with COVID-19 (COLCORONA): a phase 3, randomised, double-blinded, adaptive, placebo-controlled, multicentre trial |
| 44% lower mortality (p=0.3), 20% lower combined mortality/hospitalization (p=0.08), 47% lower ventilation (p=0.09), and 20% lower hospitalization (p=0.09). RCT for relatively low risk outpatients, 2235 treated with colchicine a mean of 5.3 days after the onset of symptoms, and 2253 controls, showing lower mortality, ventilation, and hospitalization with treatment. This study was submitted to.. | ||
Jan 7 2021 |
et al., PLOS ONE, doi:10.1371/journal.pone.0245025 | A multi-mechanism approach reduces length of stay in the ICU for severe COVID-19 patients |
| 23% lower mortality (p=0.6) and 40% shorter ICU admission (p=0.03). Retrospective 65 ICU patients in the USA and Honduras, showing shorter ICU stay with combined treatment including colchicine, LMWH, tocilizumab, dexamethasone, and methylprednisolone. | ||
Dec 31 2020 |
et al., Indian Journal of Critical Care Medicine, doi:10.5005/jp-journals-10071-23599 | A Retrospective Observational Study of Hypoxic COVID-19 Patients Treated with Immunomodulatory Drugs in a Tertiary Care Hospital |
| 7% higher mortality (p=0.83). Retrospective 134 hospitalized COVID-19 patients in India, showing no significant difference with colchicine treatment in unadjusted results. | ||
Nov 5 2020 |
et al., Mayo Clinic Proceedings: Innovations, Quality & Outcomes, doi:10.1016/j.mayocpiqo.2020.10.007 | Clinical characteristics and risk factors for mortality of hospitalized patients with COVID-19 in a community hospital: A retrospective cohort study |
| 6% lower mortality (p=0.87). Retrospective 313 patients, mostly critical stage and mostly requiring respiratory support. Confounding by indication likely. | ||
Oct 27 2020 |
et al., Canadian Journal of Infectious Diseases and Medical Microbiology, doi:10.1155/2020/8865954 | A Case Control Study to Evaluate the Impact of Colchicine on Patients Admitted to the Hospital with Moderate to Severe COVID-19 Infection |
| 42% lower mortality (p=0.0006), 53% lower ventilation (p<0.0001), 42% higher hospital discharge (p=0.0006), and 5% shorter hospitalization. Prospective cohort study of hospitalized patients in the USA, 34 treated with colchicine, showing lower mortality and intubation with treatment. | ||
Oct 23 2020 |
et al., Research Square, doi:10.21203/rs.3.rs-94922/v1 | Clinical Outcome of Patients with COVID-19 Pneumonia Treated with Corticosteroids and Colchicine in Colombia |
| 35% lower mortality (p=0.18). Retrospective 301 pneumonia patients in Colombia showing lower mortality with colchicine treatment. | ||
Sep 21 2020 |
et al., Mediterranean Journal of Rheumatology, doi:10.31138/mjr.33.2.232 (date from preprint) | The Impact of Colchicine on COVID-19 patients: A Clinical Trial Study |
| 23% shorter hospitalization (p=0.001). Open label RCT with 100 hospitalized patients in Iran, 50 treated with colchicine, showing shorter hospitalization time with treatment. There were no deaths. | ||
Sep 14 2020 |
et al., Annals of the Rheumatic Diseases, doi:10.1136/annrheumdis-2020-217712 | Association between treatment with colchicine and improved survival in a single-centre cohort of adult hospitalised patients with COVID-19 pneumonia and acute respiratory distress syndrome |
| 85% lower mortality (p<0.0001). Retrospective 122 colchicine patients and 140 control patients in Italy, showing lower mortality with treatment. Confounding may be significant: the groups were recruited during different time periods of a rapidly evolving epidemic - the .. | ||
Sep 14 2020 |
et al., Journal of Clinical Medicine, doi:10.3390/jcm9092961 | Colchicine to Weather the Cytokine Storm in Hospitalized Patients with COVID-19 |
| 73% lower mortality (p=0.03) and 73% higher hospital discharge (p=0.03). PSM matched analysis from consecutive hospitalized patients, with 33 colchicine and 33 control matched patients, showing lower mortality with treatment. | ||
Aug 12 2020 |
et al., RMD Open, doi:10.1136/rmdopen-2020-001455 (date from preprint) | Beneficial effects of colchicine for moderate to severe COVID-19: a randomised, double-blinded, placebo-controlled clinical trial |
| 22% shorter hospitalization (p=0.01). RCT with 36 colchicine and 36 control patients, showing reduced length of hospitalization and oxygen therapy with treatment. | ||
Jun 24 2020 |
et al., JAMA Network Open, doi:10.1001/jamanetworkopen.2020.13136 | Effect of Colchicine vs Standard Care on Cardiac and Inflammatory Biomarkers and Clinical Outcomes in Patients Hospitalized With Coronavirus Disease 2019: The GRECCO-19 Randomized Clinical Trial |
| 77% lower mortality (p=0.19), 82% lower ventilation (p=0.1), and 87% lower progression (p=0.05). RCT with 55 patients treated with colchicine and 50 control patients, showing lower mortality and ventilation with treatment. | ||