COVID-19 in familial Mediterranean fever: Clinical course and complications related to primary disease
et al., Modern Rheumatology, doi:10.1093/mr/roac074, Jul 2022
Colchicine for COVID-19
5th treatment shown to reduce risk in
September 2020, now with p = 0.0000049 from 54 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
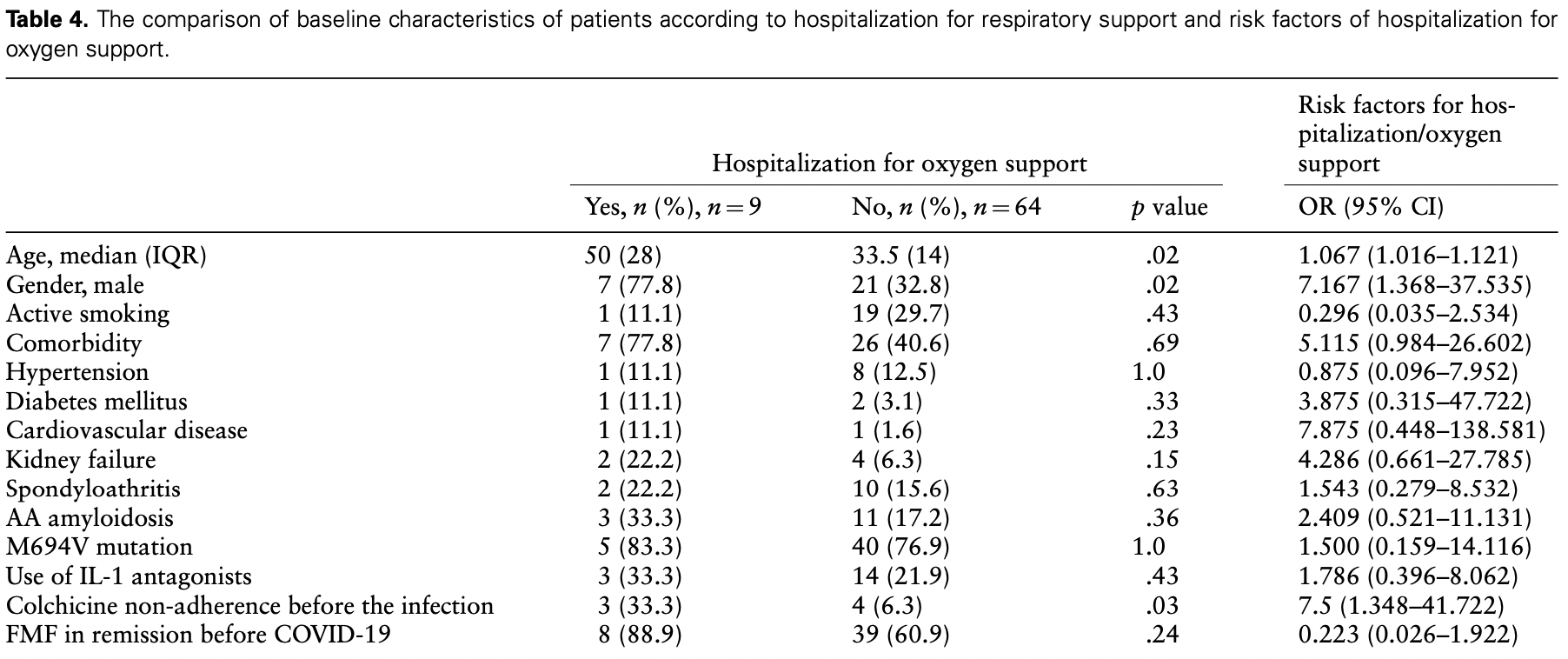
Retrospective 73 familial Mediterranean fever patients with COVID-19 in Turkey, showing significantly higher risk of hospitalization for respiratory support with non-adherence to colchicine treatment before the infection.
|
risk of oxygen therapy, 78.8% lower, RR 0.21, p = 0.04, treatment 6 of 66 (9.1%), control 3 of 7 (42.9%), NNT 3.0, inverted to make RR<1 favor treatment, odds ratio converted to relative risk.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Avanoglu Guler et al., 21 Jul 2022, retrospective, Turkey, peer-reviewed, median age 39.5, 14 authors.
Contact: aslihanavanoglu@gmail.com.
COVID-19 in familial Mediterranean fever: Clinical course and complications related to primary disease
Modern Rheumatology, doi:10.1093/mr/roac074
Objectives: To evaluate the impact of familial Mediterranean fever (FMF) features on the clinical course and outcomes of coronavirus disease 2019 (COVID-19) and clinical course of FMF after COVID-19. Methods: Consecutive FMF patients with COVID-19 were enrolled from three referral hospitals. Clinical features of FMF and detailed COVID-19 information were obtained from patient interviews and medical records. Results: Seventy-three FMF patients were included in the study. 94.5% of patients had clinical symptoms of COVID-19. We found 24.7% hospitalization, 12.3% respiratory support, 4.1% intensive care unit admission, 6.8% complication, and 1.4% mortality rate in patients. The risk factors of hospitalization for respiratory support were male gender [OR: 7.167 (95% CI: 1.368-37.535)], greater age [OR: 1.067 (95% CI: 1.016-1.121)], and non-adherence to colchicine treatment before the infection [OR: 7.5 (95% CI: 1.348-41.722)]. One-third of patients had reported attacks after COVID-19. The patterns of triggered attacks were fever, peritonitis, pleuritis, transient arthritis, chronic knee mono-arthritis, and protracted febrile myalgia. Conclusions: FMF characteristics were not associated with worse outcomes of COVID-19. Colchicine non-adherence was the risk factor of hospitalization for oxygen support. The rate of FMF attacks after COVID-19 is prominently increased, with some of them being protracted and destructive.
Conflict of interest None declared.
Ethics approval and consent to participate and for publication This study was approved by the Ministry of Health and Gazi University Hospital Ethics Committee (protocol number: 322, 29/03/2021) and followed the guidelines from Helsinki Declaration. All patients signed the informed consent, including consent for publication.
References
Bourguiba, Delplanque, Vinit, Clinical course of COVID-19 in a cohort of 342 familial Mediterranean fever patients with a long-term treatment by colchicine in a French endemic area, Ann Rheum Dis, doi:10.1136/annrheumdis-2020-218707
Esatoglu, Tascilar, Babao G Lu, COVID-19 among patients with inflammatory rheumatic diseases, Front Immunol, doi:10.3389/fimmu.2021.651715
Freeman, Swartz, Targeting the NLRP3 inflammasome in severe COVID-19, Front Immunol, doi:10.3389/fimmu.2020.01518
Gao, Ding, Dong, Risk factors for severe and critically ill COVID-19 patients: a review, Allergy, doi:10.1111/all.14657
Guan, Ni, Hu, Clinical characteristics of coronavirus disease 2019 in China, N Engl J Med, doi:10.1056/NEJMoa2002032
Gustine, Jones, Immunopathology of hyperinflammation in COVID-19, Am J Pathol, doi:10.1016/j.ajpath.2020.08.009
Günendi, Yurdakul, Bodur, The impact of COVID-19 on familial Mediterranean fever: a nationwide study, Rheumatol Int, doi:10.1007/s00296-021-04892-6
Güven, Erden, Karaka S Ö, COVID-19 outcomes in patients with familial Mediterranean fever: a retrospective cohort study, Rheumatol Int, doi:10.1007/s00296-021-04812-8
Henderson, Canna, Schulert, On the alert for cytokine storm: immunopathology in COVID-19, Arthritis Rheumatol, doi:10.1002/art.41285
Huang, Wang, Li, features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet, doi:10.1016/s0140-6736(20)30183-5
Issa, Merhi, Panossian, SARS-CoV-2 and ORF3a: nonsynonymous mutations, functional domains, and viral pathogenesis, mSystems, doi:10.1128/mSystems.00266-20
Kharouf, Ishay, Kenig, Incidence and course of COVID-19 hospitalisations among patients with familial Mediterranean fever, Rheumatology, doi:10.1093/rheumatology/keab577
Kow, Lee, Ramachandram, The effect of colchicine on mortality outcome and duration of hospital stay in patients with COVID-19: a meta-analysis of randomised trials, Immun Inflamm Dis, doi:10.1002/iid3.562
Kukuy, Beckerman, Dinour, Amyloid storm: acute kidney injury and massive proteinuria, rapidly progressing to end-stage kidney disease in AA amyloidosis of familial Mediterranean fever, Rheumatology, doi:10.1093/rheumatology/keaa772
Leung, Hui, Kraus, Colchicine-update on mechanisms of action and therapeutic uses, Semin Arthritis Rheum, doi:10.1016/j.semarthrit.2015.06.013
Livneh, Langevitz, Zemer, Criteria for the diagnosis of familial Mediterranean fever, Arthritis Rheum, doi:10.1002/art.1780401023
Qin, Zhou, Hu, Dysregulation of Immune response in patients with coronavirus 2019 (COVID-19) in Wuhan, China, Clin Infect Dis, doi:10.1093/cid/ciaa248
Schultze, Aschenbrenner, COVID-19 and the human innate immune system, Cell, doi:10.1016/j.cell.2021.02.029
Stella, Lamkanfi, Portincasa, Familial Mediterranean fever and COVID-19: friends or foes?, Front Immunol, doi:10.3389/fimmu.2020.574593
Strangfeld, Sch Ä Fer, Gianfrancesco, Factors associated with COVID-19-related death in people with rheumatic diseases: results from the COVID-19 global rheumatology alliance physician-reported registry, Ann Rheum Dis, doi:10.1136/annrheumdis-2020-219498
Tufan, Lachmann, Familial Mediterranean fever, from pathogenesis to treatment: a contemporary review, Turk J Med Sci, doi:10.3906/sag-2008-11
Tufan, Matucci-Cerinic, Immune dysfunction in COVID-19 and judicious use of antirheumatic drugs for the treatment of hyperinflammation, Turk J Med Sci, doi:10.3906/sag-2110-179
Wang, Hu, Hu, Clinical characteristics of 138 hospitalised patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China, JAMA, doi:10.1001/jama.2020.1585
Xu, Shi, Wang, Pathological findings of COVID-19 associated with acute respiratory distress syndrome, Lancet Respir Med, doi:10.1016/s2213-2600(20)30076-x
Yang, Shen, Li, Plasma IP-10 and MCP-3 levels are highly associated with disease severity and predict the progression of COVID-19, J Allergy Clin Immunol, doi:10.1016/j.jaci.2020.04.027
Özen, Sag, Ben-Chetrit, Defining colchicine resistance/intolerance in patients with familial Mediterranean fever: a modified-Delphi consensus approach, Rheumatology, doi:10.1093/rheumatology/keaa863
DOI record:
{
"DOI": "10.1093/mr/roac074",
"ISSN": [
"1439-7595",
"1439-7609"
],
"URL": "http://dx.doi.org/10.1093/mr/roac074",
"abstract": "<jats:title>ABSTRACT</jats:title>\n <jats:sec>\n <jats:title>Objectives</jats:title>\n <jats:p>To evaluate the impact of familial Mediterranean fever (FMF) features on the clinical course and outcomes of coronavirus disease 2019 (COVID-19) and clinical course of FMF after COVID-19.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Methods</jats:title>\n <jats:p>Consecutive FMF patients with COVID-19 were enrolled from three referral hospitals. Clinical features of FMF and detailed COVID-19 information were obtained from patient interviews and medical records.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Results</jats:title>\n <jats:p>Seventy-three FMF patients were included in the study. 94.5% of patients had clinical symptoms of COVID-19. We found 24.7% hospitalization, 12.3% respiratory support, 4.1% intensive care unit admission, 6.8% complication, and 1.4% mortality rate in patients. The risk factors of hospitalization for respiratory support were male gender [OR: 7.167 (95% CI: 1.368–37.535)], greater age [OR: 1.067 (95% CI: 1.016–1.121)], and non-adherence to colchicine treatment before the infection [OR: 7.5 (95% CI: 1.348–41.722)]. One-third of patients had reported attacks after COVID-19. The patterns of triggered attacks were fever, peritonitis, pleuritis, transient arthritis, chronic knee mono-arthritis, and protracted febrile myalgia.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Conclusions</jats:title>\n <jats:p>FMF characteristics were not associated with worse outcomes of COVID-19. Colchicine non-adherence was the risk factor of hospitalization for oxygen support. The rate of FMF attacks after COVID-19 is prominently increased, with some of them being protracted and destructive.</jats:p>\n </jats:sec>",
"author": [
{
"ORCID": "http://orcid.org/0000-0001-9866-9797",
"affiliation": [
{
"name": "Faculty of Medicine Hospital, Department of Rheumatology , Gazi University, Ankara, Turkey"
}
],
"authenticated-orcid": false,
"family": "Avanoglu Guler",
"given": "Aslihan",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0001-9026-9641",
"affiliation": [
{
"name": "Faculty of Medicine Hospital, Department of Rheumatology, Dokuz Eylul University , Izmir, Turkey"
}
],
"authenticated-orcid": false,
"family": "Yuce Inel",
"given": "Tuba",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Faculty of Medicine Hospital, Department of Rheumatology, Eskisehir Osmangazi University , Eskisehir, Turkey"
}
],
"family": "Kasifoglu",
"given": "Timucin",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Faculty of Medicine Hospital, Department of Internal Medicine, Gazi University , Ankara, Tukey"
}
],
"family": "Coskun",
"given": "Cansu",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Faculty of Medicine Hospital, Department of Rheumatology , Gazi University, Ankara, Turkey"
}
],
"family": "Karadeniz",
"given": "Hazan",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Faculty of Medicine Hospital, Department of Rheumatology , Gazi University, Ankara, Turkey"
}
],
"family": "Yildirim",
"given": "Derya",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Faculty of Medicine Hospital, Department of Rheumatology , Gazi University, Ankara, Turkey"
}
],
"family": "Bilici",
"given": "Reyhan",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Faculty of Medicine Hospital, Department of Rheumatology , Gazi University, Ankara, Turkey"
}
],
"family": "Satis",
"given": "Hasan",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Faculty of Medicine Hospital, Department of Rheumatology , Gazi University, Ankara, Turkey"
}
],
"family": "Kucuk",
"given": "Hamit",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Faculty of Medicine Hospital, Department of Rheumatology , Gazi University, Ankara, Turkey"
}
],
"family": "Haznedaroglu",
"given": "Seminur",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Faculty of Medicine Hospital, Department of Rheumatology , Gazi University, Ankara, Turkey"
}
],
"family": "Goker",
"given": "Berna",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Faculty of Medicine Hospital, Department of Rheumatology , Gazi University, Ankara, Turkey"
}
],
"family": "Ozturk",
"given": "Mehmet Akif",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Faculty of Medicine Hospital, Department of Rheumatology, Dokuz Eylul University , Izmir, Turkey"
}
],
"family": "Sari",
"given": "Ismail",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Faculty of Medicine Hospital, Department of Rheumatology , Gazi University, Ankara, Turkey"
}
],
"family": "Tufan",
"given": "Abdurrahman",
"sequence": "additional"
}
],
"container-title": "Modern Rheumatology",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
7,
21
]
],
"date-time": "2022-07-21T08:08:59Z",
"timestamp": 1658390939000
},
"deposited": {
"date-parts": [
[
2022,
7,
26
]
],
"date-time": "2022-07-26T09:44:31Z",
"timestamp": 1658828671000
},
"indexed": {
"date-parts": [
[
2022,
7,
27
]
],
"date-time": "2022-07-27T04:56:42Z",
"timestamp": 1658897802384
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
7,
21
]
]
},
"language": "en",
"license": [
{
"URL": "https://academic.oup.com/pages/standard-publication-reuse-rights",
"content-version": "am",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
7,
21
]
],
"date-time": "2022-07-21T00:00:00Z",
"timestamp": 1658361600000
}
}
],
"link": [
{
"URL": "https://academic.oup.com/mr/advance-article-pdf/doi/10.1093/mr/roac074/45067024/roac074.pdf",
"content-type": "application/pdf",
"content-version": "am",
"intended-application": "syndication"
},
{
"URL": "https://academic.oup.com/mr/advance-article-pdf/doi/10.1093/mr/roac074/45067024/roac074.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "286",
"original-title": [],
"prefix": "10.1093",
"published": {
"date-parts": [
[
2022,
7,
21
]
]
},
"published-online": {
"date-parts": [
[
2022,
7,
21
]
]
},
"publisher": "Oxford University Press (OUP)",
"reference": [
{
"DOI": "10.1016/s2213-2600(20)30076-x",
"article-title": "Pathological findings of COVID-19 associated with acute respiratory distress syndrome",
"author": "Xu",
"doi-asserted-by": "publisher",
"first-page": "420",
"journal-title": "Lancet Respir Med",
"key": "2022072609441799300_R1",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2002032",
"article-title": "Clinical characteristics of coronavirus disease 2019 in China",
"author": "Guan",
"doi-asserted-by": "publisher",
"first-page": "1708",
"journal-title": "N Engl J Med",
"key": "2022072609441799300_R2",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.1585",
"article-title": "Clinical characteristics of 138 hospitalised patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China",
"author": "Wang",
"doi-asserted-by": "publisher",
"first-page": "1061",
"journal-title": "JAMA",
"key": "2022072609441799300_R3",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1111/all.14657",
"article-title": "Risk factors for severe and critically ill COVID-19 patients: a review",
"author": "Gao",
"doi-asserted-by": "publisher",
"first-page": "428",
"journal-title": "Allergy",
"key": "2022072609441799300_R4",
"volume": "76",
"year": "2021"
},
{
"DOI": "10.1016/j.ajpath.2020.08.009",
"article-title": "Immunopathology of hyperinflammation in COVID-19",
"author": "Gustine",
"doi-asserted-by": "publisher",
"first-page": "4",
"journal-title": "Am J Pathol",
"key": "2022072609441799300_R5",
"volume": "191",
"year": "2021"
},
{
"DOI": "10.1016/j.cell.2021.02.029",
"article-title": "COVID-19 and the human innate immune system",
"author": "Schultze",
"doi-asserted-by": "publisher",
"first-page": "1671",
"journal-title": "Cell",
"key": "2022072609441799300_R6",
"volume": "184",
"year": "2021"
},
{
"DOI": "10.1016/j.jaci.2020.04.027",
"article-title": "Plasma IP-10 and MCP-3 levels are highly associated with disease severity and predict the progression of COVID-19",
"author": "Yang",
"doi-asserted-by": "publisher",
"first-page": "119",
"journal-title": "J Allergy Clin Immunol",
"key": "2022072609441799300_R7",
"volume": "146",
"year": "2020"
},
{
"DOI": "10.3906/sag-2110-179",
"article-title": "Immune dysfunction in COVID-19 and judicious use of antirheumatic drugs for the treatment of hyperinflammation",
"author": "Tufan",
"doi-asserted-by": "publisher",
"first-page": "3391",
"journal-title": "Turk J Med Sci",
"key": "2022072609441799300_R8",
"volume": "51",
"year": "2021"
},
{
"DOI": "10.1002/art.41285",
"article-title": "On the alert for cytokine storm: immunopathology in COVID-19",
"author": "Henderson",
"doi-asserted-by": "publisher",
"first-page": "1059",
"journal-title": "Arthritis Rheumatol",
"key": "2022072609441799300_R9",
"volume": "72",
"year": "2020"
},
{
"DOI": "10.3906/sag-2008-11",
"article-title": "Familial Mediterranean fever, from pathogenesis to treatment: a contemporary review",
"author": "Tufan",
"doi-asserted-by": "publisher",
"first-page": "1591",
"journal-title": "Turk J Med Sci",
"key": "2022072609441799300_R10",
"volume": "50",
"year": "2020"
},
{
"DOI": "10.3389/fimmu.2020.01518",
"article-title": "Targeting the NLRP3 inflammasome in severe COVID-19",
"author": "Freeman",
"doi-asserted-by": "publisher",
"journal-title": "Front Immunol",
"key": "2022072609441799300_R11",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1128/mSystems.00266-20",
"article-title": "SARS-CoV-2 and ORF3a: nonsynonymous mutations, functional domains, and viral pathogenesis",
"author": "Issa",
"doi-asserted-by": "publisher",
"journal-title": "mSystems",
"key": "2022072609441799300_R12",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1093/rheumatology/keaa772",
"article-title": "Amyloid storm: acute kidney injury and massive proteinuria, rapidly progressing to end-stage kidney disease in AA amyloidosis of familial Mediterranean fever",
"author": "Kukuy",
"doi-asserted-by": "publisher",
"first-page": "3235",
"journal-title": "Rheumatology (Oxford)",
"key": "2022072609441799300_R13",
"volume": "60",
"year": "2021"
},
{
"DOI": "10.1016/j.semarthrit.2015.06.013",
"article-title": "Colchicine—update on mechanisms of action and therapeutic uses",
"author": "Leung",
"doi-asserted-by": "publisher",
"first-page": "341",
"journal-title": "Semin Arthritis Rheum",
"key": "2022072609441799300_R14",
"volume": "45",
"year": "2015"
},
{
"DOI": "10.1002/iid3.562",
"article-title": "The effect of colchicine on mortality outcome and duration of hospital stay in patients with COVID-19: a meta-analysis of randomised trials",
"author": "Kow",
"doi-asserted-by": "publisher",
"first-page": "255",
"journal-title": "Immun Inflamm Dis",
"key": "2022072609441799300_R15",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.1093/cid/ciaa248",
"article-title": "Dysregulation of Immune response in patients with coronavirus 2019 (COVID-19) in Wuhan, China",
"author": "Qin",
"doi-asserted-by": "publisher",
"first-page": "762",
"journal-title": "Clin Infect Dis",
"key": "2022072609441799300_R16",
"volume": "71",
"year": "2020"
},
{
"DOI": "10.1016/s0140-6736(20)30183-5",
"article-title": "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China",
"author": "Huang",
"doi-asserted-by": "publisher",
"first-page": "497",
"journal-title": "Lancet",
"key": "2022072609441799300_R17",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1002/art.1780401023",
"article-title": "Criteria for the diagnosis of familial Mediterranean fever",
"author": "Livneh",
"doi-asserted-by": "publisher",
"first-page": "1879",
"journal-title": "Arthritis Rheum",
"key": "2022072609441799300_R18",
"volume": "40",
"year": "1997"
},
{
"DOI": "10.1093/rheumatology/keaa863",
"article-title": "Defining colchicine resistance/intolerance in patients with familial Mediterranean fever: a modified-Delphi consensus approach",
"author": "Özen",
"doi-asserted-by": "publisher",
"first-page": "3799",
"journal-title": "Rheumatology (Oxford)",
"key": "2022072609441799300_R19",
"volume": "60",
"year": "2021"
},
{
"DOI": "10.3389/fimmu.2021.651715",
"article-title": "COVID-19 among patients with inflammatory rheumatic diseases",
"author": "Esatoglu",
"doi-asserted-by": "publisher",
"journal-title": "Front Immunol",
"key": "2022072609441799300_R20",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1007/s00296-021-04812-8",
"article-title": "COVID-19 outcomes in patients with familial Mediterranean fever: a retrospective cohort study",
"author": "Güven",
"doi-asserted-by": "publisher",
"first-page": "715",
"journal-title": "Rheumatol Int",
"key": "2022072609441799300_R21",
"volume": "41",
"year": "2021"
},
{
"DOI": "10.1136/annrheumdis-2020-218707",
"article-title": "Clinical course of COVID-19 in a cohort of 342 familial Mediterranean fever patients with a long-term treatment by colchicine in a French endemic area",
"author": "Bourguiba",
"doi-asserted-by": "publisher",
"first-page": "539",
"journal-title": "Ann Rheum Dis",
"key": "2022072609441799300_R22",
"volume": "80",
"year": "2020"
},
{
"DOI": "10.1007/s00296-021-04892-6",
"article-title": "The impact of COVID-19 on familial Mediterranean fever: a nationwide study",
"author": "Günendi",
"doi-asserted-by": "publisher",
"first-page": "1447",
"journal-title": "Rheumatol Int",
"key": "2022072609441799300_R23",
"volume": "41",
"year": "2021"
},
{
"DOI": "10.1093/rheumatology/keab577",
"article-title": "Incidence and course of COVID-19 hospitalisations among patients with familial Mediterranean fever",
"author": "Kharouf",
"doi-asserted-by": "publisher",
"first-page": "Si85",
"journal-title": "Rheumatology (Oxford)",
"key": "2022072609441799300_R24",
"volume": "60",
"year": "2021"
},
{
"DOI": "10.1136/annrheumdis-2020-219498",
"article-title": "Factors associated with COVID-19-related death in people with rheumatic diseases: results from the COVID-19 global rheumatology alliance physician-reported registry",
"author": "Strangfeld",
"doi-asserted-by": "publisher",
"first-page": "930",
"journal-title": "Ann Rheum Dis",
"key": "2022072609441799300_R25",
"volume": "80",
"year": "2021"
},
{
"DOI": "10.3389/fimmu.2020.574593",
"article-title": "Familial Mediterranean fever and COVID-19: friends or foes?",
"author": "Stella",
"doi-asserted-by": "publisher",
"journal-title": "Front Immunol",
"key": "2022072609441799300_R26",
"volume": "11",
"year": "2020"
}
],
"reference-count": 26,
"references-count": 26,
"relation": {},
"resource": {
"primary": {
"URL": "https://academic.oup.com/mr/advance-article/doi/10.1093/mr/roac074/6647632"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Rheumatology"
],
"subtitle": [],
"title": "COVID-19 in familial Mediterranean fever: Clinical course and complications related to primary disease",
"type": "journal-article"
}
