Efficacy is variant dependent. In Vitro research suggests a lack of efficacy for omicron BA.2.75.2, BA.4.6, and BQ.1.11, BA.5, BA.2.75, XBB2,3, XBB.1.53, XBB.1.9.13, XBB.1.9.3, XBB.1.5.24, XBB.1.16, XBB.2.9, BQ.1.1.45, CL.1, and CH.1.14. US EUA has been revoked. mAb use may create new variants that spread globally5-7, and may be associated with increased risk of autoimmune disease8, prolonged viral loads, clinical deterioration, and immune escape6,9-13 .
Tixagevimab/cilgavimab was adopted
in 33 countries.
Recent:Ngiam Martin-Blondel.
Feb 27 |
Tixagevimab/cilgavimab reduced COVID-19 risk: real-time meta-analysis of 19 studies (Version 32) | |
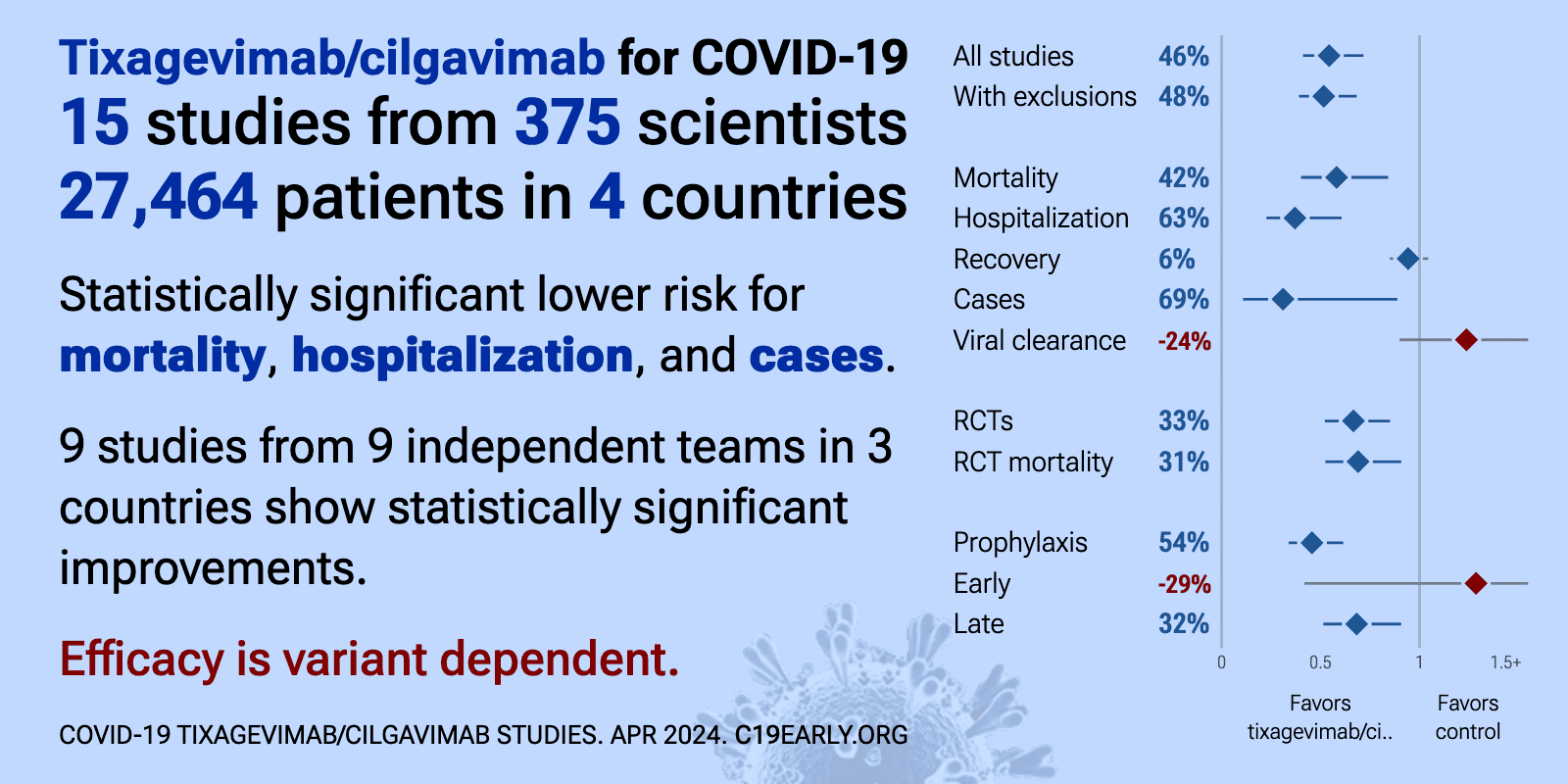
| Significantly lower risk is seen for mortality, hospitalization, and cases. 9 studies from 9 independent teams in 3 countries show significant benefit. Meta-analysis using the most serious outcome reported shows 34% [11‑51%] lo.. | ||
Jan 31 |
et al., International Journal of Infectious Diseases, doi:10.1016/j.ijid.2026.108435 | Early administration of neutralising monoclonal antibodies and post-acute sequelae of COVID-19 |
| Retrospective 19,689 hospitalized COVID-19 patients in Singapore showing no significant reduction in overall post-acute sequelae of COVID-19 (PASC) with early monoclonal antibody treatment, but increased risk of autoimmune complications. .. | ||
Dec 31 2025 |
et al., iScience, doi:10.1016/j.isci.2025.114226 | Viral clearance and escape during therapy of COVID-19 outpatients: A prospective cohort study |
| Prospective cohort study of 114 high-risk COVID-19 outpatients showing that monoclonal antibody treatments with suboptimal neutralizing activity against infecting variants resulted in higher viral loads and increased emergence of escape m.. | ||
Oct 1 2025 |
et al., Infection and Drug Resistance, doi:10.2147/IDR.S540928 | The Emergence of Escape Mutations in COVID-19 Following Anti-Spike Monoclonal Antibody Treatment: How Do We Tackle It? |
| Review of treatment-emergent resistance to anti-spike monoclonal antibodies in COVID-19 patients. Monotherapies like bamlanivimab and sotrovimab showed very high resistance rates, while combination approaches had lower risk. The rapid evo.. | ||
Aug 29 2025 |
et al., Open Forum Infectious Diseases, doi:10.1093/ofid/ofaf542 | Rapid Elimination of Culturable SARS-CoV-2 With Intramuscular or Intravenous Administration of Antiviral Monoclonal Antibody Therapy |
| RCT 313 outpatients showing that that intramuscular delivery of tixagevimab/cilgavimab is as effective as intravenous administration for viral clearance. | ||
May 21 2025 |
et al., Scientific Reports, doi:10.1038/s41598-025-02240-3 | Dose-dependent impact of tixagevimab–cilgavimab as primary prevention against SARS-CoV-2 in immunocompromised individuals |
| 70% more cases (p=0.08). Retrospective 597 immunocompromised individuals showing no significant difference in infection rates over the entire study period. However, when truncating data to November 1, 2022 (before resistant variants dominated), effectiveness incr.. | ||
Mar 13 2025 |
et al., Eurosurveillance, doi:10.2807/1560-7917.ES.2025.30.10.2400252 | Impact of SARS-CoV-2 variant mutations on susceptibility to monoclonal antibodies and antiviral drugs: a non-systematic review, April 2022 to October 2024 |
| Review of SARS-CoV-2 variant mutations and their impact on susceptibility to monoclonal antibodies and antivirals. Mutations in the ORF1ab region led to decreased susceptibility to paxlovid, while nsp12 mutations reduced efficacy for remd.. | ||
Feb 6 2025 |
et al., Clinical Microbiology and Infection, doi:10.1016/j.cmi.2025.02.002 | Long-term outcomes of passive immunotherapy for COVID-19: a pooled analysis of a large multinational platform randomized clinical trial |
| 23% lower mortality (p=0.08) and 3% lower combined mortality/hospitalization (p=0.77). Analysis of 2,311 hospitalized COVID-19 patients from four randomized controlled trials (ACTIV-3/TICO) showing no significant difference in long-term mortality with sotrovimab, amubarvimab/romlusevimab, tixagevimab-cilgavimab, or ensovibep. | ||
Jan 29 2025 |
et al., Open Forum Infectious Diseases, doi:10.1093/ofid/ofae631.2172 | Evaluating the use of Monoclonal Antibodies - Sotrovimab, Casirivimab/Imedvimab (REGEN-COV) and Tixagevimab/Cilgavimab (EVUSHELD) for COVID-19 Treatment in Singapore |
| 8% lower ICU admission (p=1) and 33% lower need for oxygen therapy (p=0.17). PSM retrospective 366 hospitalized COVID-19 patients in Singapore showing no statistically significant reduction in severe outcomes with monoclonal antibodies (mAbs), except for lower oxygen use in patients treated with sotrovimab during .. | ||
Sep 19 2024 |
et al., Antiviral Research, doi:10.1016/j.antiviral.2024.106006 | Identification of antibody-resistant SARS-CoV-2 mutants via N4-Hydroxycytidine mutagenesis |
| In vitro selection study identifying SARS-CoV-2 spike mutations that confer resistance to therapeutic antibodies. Using a Wuhan-like strain and omicron B.1.1.529, the authors used sequential mutagenesis with the molnupiravir active compou.. | ||
Aug 11 2024 |
, D., Current Topics in Microbiology and Immunology, doi:10.1007/82_2024_268 | Monoclonal Antibody Therapies Against SARS-CoV-2: Promises and Realities |
| Review of monoclonal antibodies for SARS-CoV-2. Author notes that the omicron variant has reset achievements to date. | ||
Aug 8 2024 |
et al., Clinical Infectious Diseases, doi:10.1093/cid/ciae408 | Single monoclonal antibodies should not be used for COVID-19 therapy: a call for antiviral stewardship |
| Review arguing against use of single monoclonal antibodies for COVID-19 treatment, particularly in immunosuppressed patients, due to the risk of rapidly selecting for resistant viral variants. Authors suggest that while monoclonal antibod.. | ||
Aug 5 2024 |
et al., Viral Immunology, doi:10.1089/vim.2024.0034 | Effective Treatment of COVID-19 Infection with Repurposed Drugs: Case Reports |
| Review of the successful treatment of COVID-19 using existing medications including HCQ, AZ, ivermectin, famotidine, monoclonal antibodies, and others. Authors note that the typical treatment of severe viral infections with multiple thera.. | ||
May 28 2024 |
et al., BMC Infectious Diseases, doi:10.1186/s12879-024-09269-1 | Management of immunosuppression in lung transplant recipients and COVID-19 outcomes: an observational retrospective cohort-study |
| 10% higher progression (p=1). Retrospective 91 lung transplant recipients with COVID-19 showing no significant difference in poor outcomes with casirivimab/imdevimab or tixagevimab/cilgavimab prophylaxis in univariate analysis. | ||
Apr 30 2024 |
et al., European Review for Medical and Pharmacological Sciences, doi:10.26355/eurrev_202404_35925 | The safety signal detection and analysis of monoclonal antibodies against SARS-CoV-2 based on real-world evidence – the suitable selectivity for different populations |
| FDA adverse event reporting analysis for bebtelovimab, tixagevimab/cilgavimab, and sotrovimab, showing distinct safety profiles with concerning adverse events for each drug. Bebtelovimab showed the highest associations with gastrointestin.. | ||
Mar 31 2024 |
et al., American Journal of Transplantation, doi:10.1016/j.ajt.2024.03.011 | Longitudinal outcomes of COVID-19 in solid organ transplant recipients from 2020 to 2023 |
| 26% lower severe cases (p=0.48). Retrospective 1,975 solid organ transplant recipients with COVID-19 showing lower risk of severe cases with tixagevimab/cilgavimab prophylaxis, without statistical significance. | ||
Mar 30 2024 |
et al., Infection, doi:10.1007/s15010-024-02223-y | SARS-CoV-2 journey: from alpha variant to omicron and its sub-variants |
| Review of SARS-CoV-2 variants showing increased transmissibility, disease severity, and immune escape with mutations in the spike protein receptor binding domain. Authors cover variants from the initial D614G mutation through omicron sub-.. | ||
Feb 16 2024 |
et al., Journal of Infection, doi:10.1016/j.jinf.2024.106120 | Tixagevimab-cilgavimab (AZD7442) for the treatment of patients hospitalized with COVID-19 (DisCoVeRy): a phase 3, randomized, double-blind, placebo-controlled trial |
| 40% lower mortality (p=0.17), 18% worse 7-point scale results (p=0.52), 1% faster recovery (p=0.93), and 9% higher hospital discharge (p=0.49). RCT 173 hospitalized COVID-19 patients showing no significant difference in clinical status, time to recovery, viral clearance, or mortality with tixagevimab/cilgavimab. Mortality was lower, without statistical significance. The trial was.. | ||
Nov 30 2023 |
et al., iScience, doi:10.1016/j.isci.2023.108147 | Antiviral efficacy against and replicative fitness of an XBB.1.9.1 clinical isolate |
| In vitro and animal study showing that the SARS-CoV-2 omicron subvariant XBB.1.9.1 has similar antigenicity, antiviral susceptibility, and replicative ability compared to XBB.1.5. Casirivimab, imdevimab, tixagevimab, cilgavimab, sotrovima.. | ||
Nov 23 2023 |
et al., The Journal of Infectious Diseases, doi:10.1093/infdis/jiad523 | Spike protein genetic evolution in patients at high-risk of severe COVID-19 treated by monoclonal antibodies |
| Prospective study of 264 high-risk COVID-19 patients treated with monoclonal antibodies. Tixagevimab/cilgavimab was associated with 5 times higher risk of emergence of mutations. Treatment with sotrovimab was linked to mutations associate.. | ||
Oct 20 2023 |
et al., Frontiers in Immunology, doi:10.3389/fimmu.2023.1259725 | Real-world clinical effectiveness of Tixagevimab/Cilgavimab and Regdanvimab monoclonal antibodies for COVID-19 treatment in Omicron variant-dominant period |
| Prospective study of 77 COVID-19 outpatients showing improved efficacy with tixagevimab/cilgavimab compared to regdanvimab during Omicron variant dominance. | ||
Sep 28 2023 |
et al., Vaccines, doi:10.3390/vaccines11101533 | In Vitro Efficacy of Antivirals and Monoclonal Antibodies against SARS-CoV-2 Omicron Lineages XBB.1.9.1, XBB.1.9.3, XBB.1.5, XBB.1.16, XBB.2.4, BQ.1.1.45, CH.1.1, and CL.1 |
| In vitro study showing sharply reduced neutralization of SARS-CoV-2 variants XBB.1.9.1, XBB.1.9.3, XBB.1.5, XBB.1.16, XBB.2.4, BQ.1.1.45, CH.1.1, and CL.1 with monoclonal antibodies cilgavimab, tixagevimab, imdevimab, etsevimab, casirivim.. | ||
Sep 27 2023 |
et al., Microorganisms, doi:10.3390/microorganisms11102417 | Prevalence of SARS-CoV-2 Omicron Sublineages and Spike Protein Mutations Conferring Resistance against Monoclonal Antibodies in a Swedish Cohort during 2022–2023 |
| Analysis of 7,950 SARS-CoV-2 samples from central Sweden collected between March 2022 and May 2023 tracking the prevalence of omicron sublineages and mutations in the spike protein conferring resistance to monoclonal antibodies over time... | ||
Sep 6 2023 |
et al., Crohn's & Colitis 360, doi:10.1093/crocol/otad047 | Tixagevimab and Cilgavimab (Evusheld) as Pre-exposure Prophylaxis for COVID-19 in Patients With Inflammatory Bowel Disease: A Propensity Matched Cohort Study |
| 12% lower hospitalization (p=0.81) and 35% more cases (p=0.18). TriNetX PSM retrospective 408 IBD patients receiving tixagevimab/cilgavimab and matched controls, showing no significant difference in COVID-19 cases or hospitalization. | ||
Aug 10 2023 |
et al., Drug Resistance Updates, doi:10.1016/j.drup.2023.100991 | Analysis of SARS-CoV-2 mutations associated with resistance to therapeutic monoclonal antibodies that emerge after treatment |
| Review of reports of treatment-emergent resistance to COVID-19 monoclonal antibodies (mAbs), showing that some post-mAb treatment mutations appeared to spread globally soon after the mAb was introduced, raising concerns about transmission.. | ||
Aug 8 2023 |
et al., Hemasphere, doi:10.1097/01.HS9.0000973036.97124.6c | COVID-19 infection among CAR-T cell therapy recipients: A single center experience |
| 19% lower hospitalization (p=0.77). Retrospective 64 COVID+ CAR-T cell therapy recipients, showing lower hospitalization with tixagevimab/cilgavimab prophylaxis in unadjusted results, without statistical significance. | ||
May 12 2023 |
et al., Transplantation Direct, doi:10.1097/txd.0000000000001485 | Pre-exposure Prophylaxis with Tixagevimab-cilgavimab did not Reduce Severity of COVID-19 in Lung Transplant Recipients with Breakthrough Infection |
| 96% higher ventilation (p=0.58), 210% higher ICU admission (p=0.33), 53% lower hospitalization (p=0.18), and 29% fewer symptomatic cases (p=0.14). Retrospective 546 lung transplant recipients, 203 receiving tixagevimab/cilgavimab, and 343 out of state or declining treatment, showing a trend towards lower incidence of cases, but no significant difference in clinical outcomes. | ||
Jan 19 2023 |
et al., Preprints, doi:10.20944/preprints202301.0359.v1 | Preliminary Evidence of Good Safety Profile and Outcomes of Early Treatment With Tixagevimab/Cilgavimab Compared to Previously Employed Monoclonal Antibodies for COVID-19 in Immunocompromised Patients |
| 368% higher mortality (p=0.32), 33% lower hospitalization (p=1), and 24% worse viral clearance (p=0.3). Retrospective immunocompromised patients, showing no significant difference between tixagevimab/cilgavimab and other mAbs. | ||
Jan 8 2023 |
et al., Reviews in Medical Virology, doi:10.1002/rmv.2420 | Efficacy and safety of tixagevimab‐cilgavimab as pre‐exposure prophylaxis for COVID‐19: A systematic review and meta‐analysis |
| 83% lower mortality (p=0.05), 87% lower hospitalization (p<0.0001), 87% lower severe cases (p<0.0001), and 76% fewer cases (p<0.0001). Meta analysis of 6 studies showing significantly lower COVID-19 cases, hospitalization, severity, and mortality with tixagevimab/cilgavimab prophylaxis. | ||
Dec 31 2022 |
et al., American Journal of Transplantation, doi:10.1111/ajt.17128 | Tixagevimab/cilgavimab pre-exposure prophylaxis is associated with lower breakthrough infection risk in vaccinated solid organ transplant recipients during the omicron wave |
| 86% lower mortality (p=0.25), 83% lower hospitalization (p=0.12), and 66% fewer cases (p=0.001). Retrospective cohort study of 444 solid organ transplant recipients showing significantly lower risk of SARS-CoV-2 breakthrough infections with tixagevimab/cilgavimab pre-exposure prophylaxis compared to controls during the omicron period. | ||
Nov 17 2022 |
et al., bioRxiv, doi:10.1101/2022.11.17.516888 | Resistance of Omicron subvariants BA.2.75.2, BA.4.6 and BQ.1.1 to neutralizing antibodies |
| In vitro study suggesting a lack of efficacy for tixagevimab/vilgavimab with BA.2.75.2, BQ.1.1, and BA.4.6. | ||
Oct 31 2022 |
et al., Kidney International, doi:10.1016/j.kint.2022.07.008 | COVID-19 morbidity decreases with tixagevimab–cilgavimab preexposure prophylaxis in kidney transplant recipient nonresponders or low-vaccine responders |
| 92% lower mortality (p=0.07), 96% lower ICU admission (p=0.001), 95% lower hospitalization (p=0.001), and 99% fewer symptomatic cases (p=0.001). Retrospective 430 kidney transplant recipients showing significantly lower symptomatic COVID-19 and hospitalization with tixagevimab/cilgavimab preexposure prophylaxis compared to 97 patients who did not receive it, during an omicron wave. | ||
Oct 31 2022 |
et al., Clinical Infectious Diseases, doi:10.1093/cid/ciac855 | Effectiveness of Evusheld in Immunocompromised Patients: Propensity Score-Matched Analysis |
| 59% lower hospitalization (p=0.02) and 25% fewer cases (p=0.03). Retrospective 732 immunocompromised patients in Israel treated with tixagevimab/cilgavimab, and 2,812 matched controls, showing significantly lower cases and hospitalization with treatment. | ||
Jul 29 2022 |
et al., Clinical Infectious Diseases, doi:10.1093/cid/ciac625 | Association between AZD7442 (tixagevimab-cilgavimab) administration and SARS-CoV-2 infection, hospitalization and mortality |
| 92% lower combined mortality/hospitalization (p=0.01) and 47% fewer cases (p=0.01). Retrospective 825 immunocompromised individuals treated with tixagevimab-cilgavimab and 4229 untreated in Israel, showing significantly lower infection and hospitalization/death with treatment. Omicron was the dominant variant. | ||
Jul 11 2022 |
et al., Cancer, doi:10.1002/cncr.34354 | Seroconversion and outcomes after initial and booster COVID‐19 vaccination in adults with hematologic malignancies |
| 76% lower mortality (p=0.32) and 90% fewer cases (p=0.03). Retrospective 378 patients with hematologic malignancies analyzing seroconversion and outcomes post-vaccination. Among 25 seronegative patients after booster vaccination who received tixagevimab/cilgavimab prophylaxis, no COVID-19 infecti.. | ||
Jul 8 2022 |
et al., The Lancet Respiratory Medicine, doi:10.1016/S2213-2600(22)00215-6 | Tixagevimab–cilgavimab for treatment of patients hospitalised with COVID-19: a randomised, double-blind, phase 3 trial |
| 23% lower mortality (p=0.08), 3% lower combined mortality/hospitalization (p=0.77), and 7% improved recovery (p=0.21). RCT with 710 hospitalized patients treated with tixagevimab/cilgavimab, and 707 placebo patients, showing lower mortality with treatment. Long-term results are reported in [Mourad] | ||
Jun 21 2022 |
, S., Drugs, doi:10.1007/s40265-022-01731-1 | Tixagevimab + Cilgavimab: First Approval |
| Review of tixagevimab + cilgavimab for the prevention and treatment of COVID-19. Tixagevimab and cilgavimab are long-acting monoclonal antibodies that bind to distinct sites on the SARS-CoV-2 spike protein. In March 2022, the combination .. | ||
Jun 7 2022 |
et al., The Lancet Respiratory Medicine, doi:10.1016/S2213-2600(22)00180-1 | Efficacy and safety of intramuscular administration of tixagevimab–cilgavimab for early outpatient treatment of COVID-19 (TACKLE): a phase 3, randomised, double-blind, placebo-controlled trial |
| no change in mortality (p=1), 50% lower severe cases (p=0.01), and 57% lower hospitalization (p=0.002). RCT 910 outpatients in the USA, 456 treated with tixagevimab/cilgavimab, showing significantly lower severe cases and hospitalization with treatment, but no difference in mortality. | ||
May 29 2022 |
et al., medRxiv, doi:10.1101/2022.05.28.22275716 | Tixagevimab/Cilgavimab for Prevention of COVID-19 during the Omicron Surge: Retrospective Analysis of National VA Electronic Data |
| 64% lower mortality (p=0.004), 69% lower combined death/hospitalization/cases (p<0.0001), 87% lower hospitalization (p=0.04), and 66% fewer cases (p=0.03). PSM retrospective 1,848 immunocompromised patients given tixagevimab/cilgavimab prophylaxis, showing lower mortality, hospitalization, and cases. | ||
Apr 20 2022 |
et al., New England Journal of Medicine, doi:10.1056/NEJMoa2116620 | Intramuscular AZD7442 (Tixagevimab–Cilgavimab) for Prevention of Covid-19 |
| 86% lower mortality (p=0.11) and 82% fewer symptomatic cases (p<0.0001). PrEP RCT with 3,441 tixagevimab/cilgavimab patients and 1,731 control patients, showing lower risk of symptomatic cases with treatment. | ||
Dec 8 2021 |
et al., Clinical Infectious Diseases, doi:10.1093/cid/ciac899 (date from FDA disclosure of results) | AZD7442 (Tixagevimab/Cilgavimab) for Post-exposure Prophylaxis of Symptomatic COVID-19 |
| 42% fewer symptomatic cases (p=0.06). 1,121 patient PEP RCT showing lower symptomatic cases with tixagevimab/cilgavimab, without statistical significance. | ||
Dec 8 2021 |
et al., Open Forum Infectious Diseases, doi:10.1093/ofid/ofab466.1646 | PROVENT: Phase 3 Study of Efficacy and Safety of AZD7442 (Tixagevimab/Cilgavimab) for Pre-exposure Prophylaxis of COVID-19 in Adults |
| 86% lower mortality (p=0.11) and 76% fewer symptomatic cases (p=0.0005). PrEP RCT with 3,441 tixagevimab/cilgavimab patients and 1,731 control patients, showing lower risk of symptomatic cases with treatment. Followup data is from [fda.gov]. | ||
References
Planas et al., Resistance of Omicron subvariants BA.2.75.2, BA.4.6 and BQ.1.1 to neutralizing antibodies, bioRxiv, doi:10.1101/2022.11.17.516888.
Haars et al., Prevalence of SARS-CoV-2 Omicron Sublineages and Spike Protein Mutations Conferring Resistance against Monoclonal Antibodies in a Swedish Cohort during 2022–2023, Microorganisms, doi:10.3390/microorganisms11102417.
Uraki et al., Antiviral efficacy against and replicative fitness of an XBB.1.9.1 clinical isolate, iScience, doi:10.1016/j.isci.2023.108147.
Pochtovyi et al., In Vitro Efficacy of Antivirals and Monoclonal Antibodies against SARS-CoV-2 Omicron Lineages XBB.1.9.1, XBB.1.9.3, XBB.1.5, XBB.1.16, XBB.2.4, BQ.1.1.45, CH.1.1, and CL.1, Vaccines, doi:10.3390/vaccines11101533.
Focosi et al., Analysis of SARS-CoV-2 mutations associated with resistance to therapeutic monoclonal antibodies that emerge after treatment, Drug Resistance Updates, doi:10.1016/j.drup.2023.100991.
Leducq et al., Spike protein genetic evolution in patients at high-risk of severe COVID-19 treated by monoclonal antibodies, The Journal of Infectious Diseases, doi:10.1093/infdis/jiad523.
Bruhn et al., Somatic hypermutation shapes the viral escape profile of SARS-CoV-2 neutralising antibodies, eBioMedicine, doi:10.1016/j.ebiom.2025.105770.
Ngiam et al., Early administration of neutralising monoclonal antibodies and post-acute sequelae of COVID-19, International Journal of Infectious Diseases, doi:10.1016/j.ijid.2026.108435.
Choudhary et al., Emergence of SARS-CoV-2 Resistance with Monoclonal Antibody Therapy, medRxiv, doi:10.1101/2021.09.03.21263105.
Günther et al., Variant-specific humoral immune response to SARS-CoV-2 escape mutants arising in clinically severe, prolonged infection, medRxiv, doi:10.1101/2024.01.06.24300890.
Casadevall et al., Single monoclonal antibodies should not be used for COVID-19 therapy: a call for antiviral stewardship, Clinical Infectious Diseases, doi:10.1093/cid/ciae408.