Evaluating the use of Monoclonal Antibodies - Sotrovimab, Casirivimab/Imedvimab (REGEN-COV) and Tixagevimab/Cilgavimab (EVUSHELD) for COVID-19 Treatment in Singapore
et al., Open Forum Infectious Diseases, doi:10.1093/ofid/ofae631.2172, Jan 2025
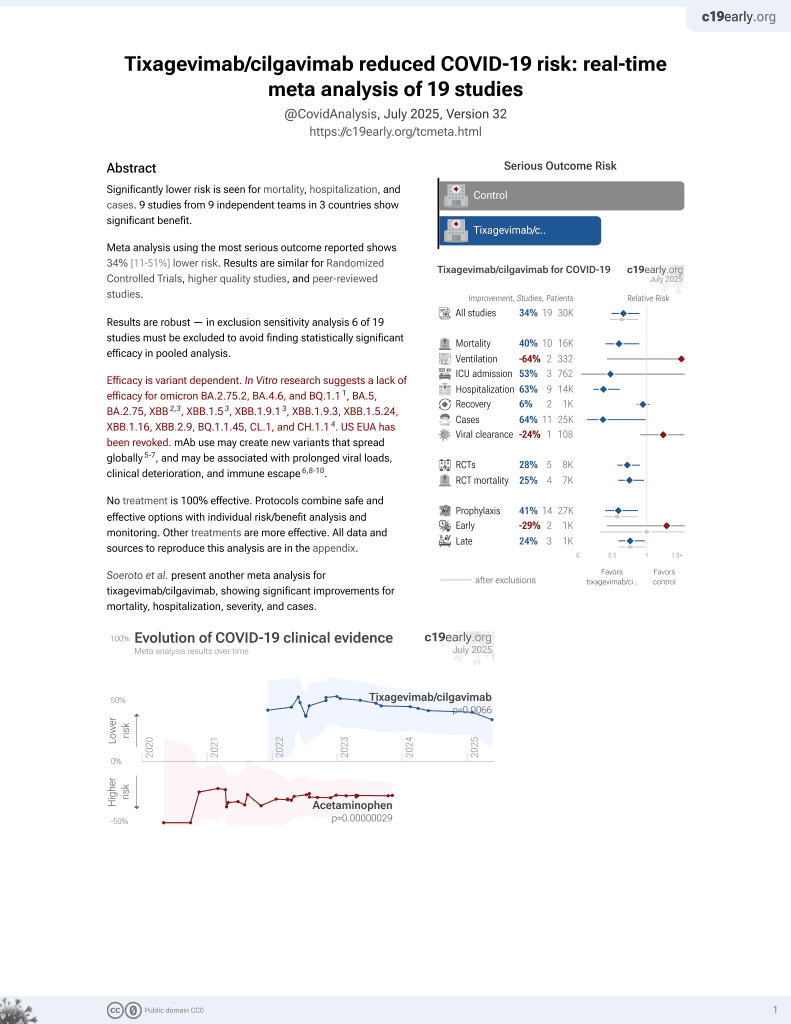
42nd treatment shown to reduce risk in
May 2022, now with p = 0.0066 from 19 studies, recognized in 33 countries.
Efficacy is variant dependent.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
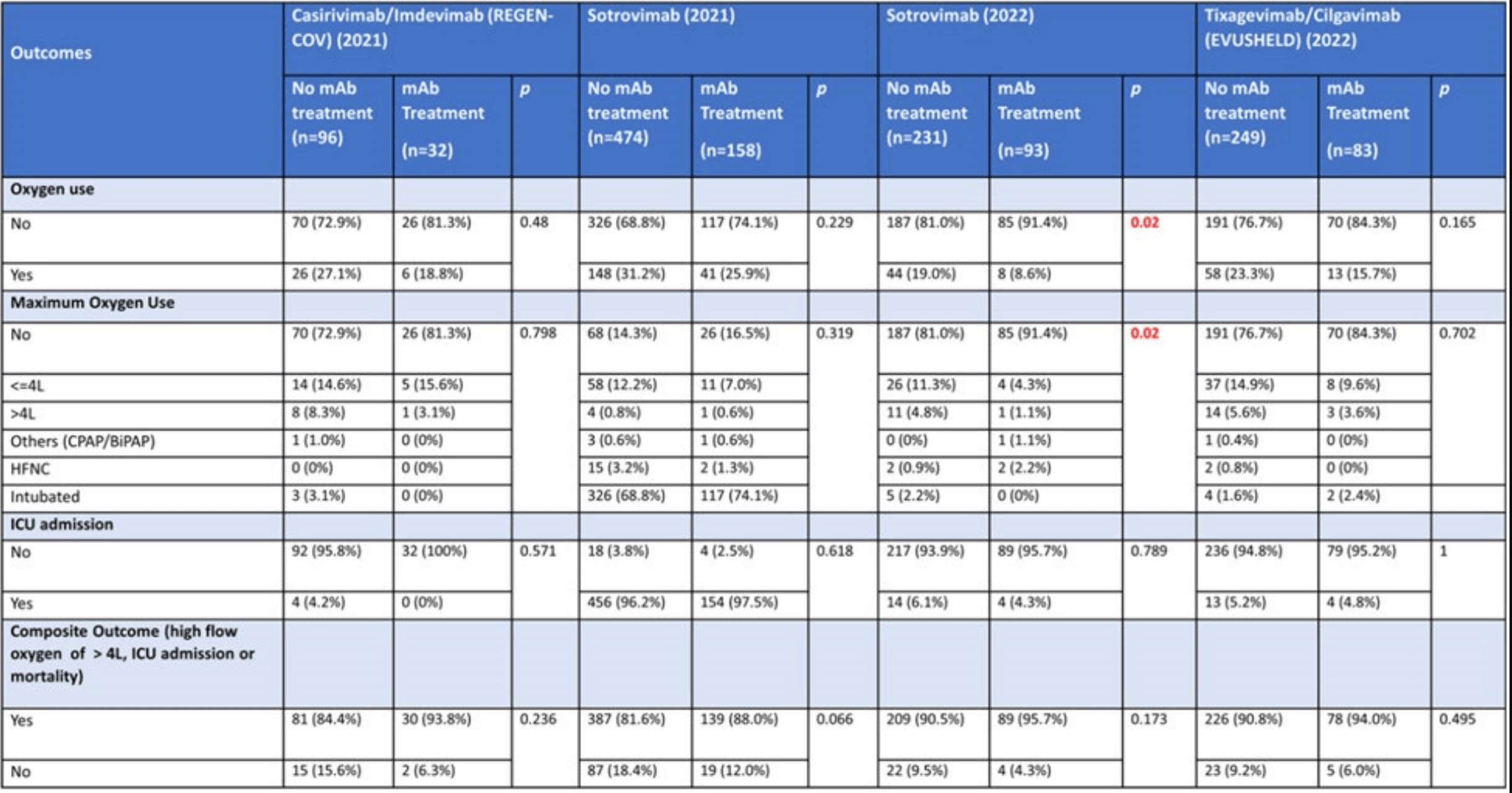
PSM retrospective 366 hospitalized COVID-19 patients in Singapore showing no statistically significant reduction in severe outcomes with monoclonal antibodies (mAbs), except for lower oxygen use in patients treated with sotrovimab during the Omicron wave. The 2021 numbers for sotrovimab do not appear to be reported correctly, for example showing >96% intubation and higher incidence of ICU admission than the composite outcome that includes ICU admission. Multiple numbers appear to have been transposed.
Efficacy is variant dependent. In Vitro research suggests a lack of efficacy for omicron BA.2.75.2, BA.4.6, BQ.1.11, BA.5, BA.2.75, XBB2,3, XBB.1.53, ХВВ.1.9.13, XBB.1.9.3, XBB.1.5.24, XBB.1.16, XBB.2.9, BQ.1.1.45, CL.1, and CH.1.14.
Study covers sotrovimab, casirivimab/imdevimab, and tixagevimab/cilgavimab.
|
risk of mechanical ventilation, 50.0% higher, RR 1.50, p = 0.64, treatment 2 of 83 (2.4%), control 4 of 249 (1.6%), propensity score matching.
|
|
risk of ICU admission, 7.7% lower, RR 0.92, p = 1.00, treatment 4 of 83 (4.8%), control 13 of 249 (5.2%), NNT 249, propensity score matching.
|
|
risk of oxygen therapy, 32.8% lower, RR 0.67, p = 0.17, treatment 13 of 83 (15.7%), control 58 of 249 (23.3%), NNT 13, propensity score matching.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Planas et al., Resistance of Omicron subvariants BA.2.75.2, BA.4.6 and BQ.1.1 to neutralizing antibodies, bioRxiv, doi:10.1101/2022.11.17.516888.
2.
Haars et al., Prevalence of SARS-CoV-2 Omicron Sublineages and Spike Protein Mutations Conferring Resistance against Monoclonal Antibodies in a Swedish Cohort during 2022–2023, Microorganisms, doi:10.3390/microorganisms11102417.
Chua et al., 29 Jan 2025, retrospective, Singapore, peer-reviewed, 9 authors.
Evaluating the use of Monoclonal Antibodies -Sotrovimab, Casirivimab/ Imedvimab (REGEN-COV) and Tixagevimab/Cilgavimab (EVUSHELD) for COVID-19 Treatment in Singapore
Identifying patients at higher risk for developing severe COVID-19-related complications (69%) • Incorporating new information about treatment options for non-hospitalized patients with COVID-19 (67%) • Ensure patients receive treatment within the appropriate therapeutic window (60%) • Educating patients on COVID-19 and available antiviral treatments (58%) • Screening patients for potential DDIs prior to COVID-19 antiviral initiation (55%) • Some of the barriers to implementing these practice changes include: • Patients present outside the recommended treatment window • Unfamiliar with potential drug-drug interactions for COVID-19 antivirals • Patient concerns or questions regarding available antivirals • Unfamiliar with guideline recommendations for available antivirals • Lack of time during office visits to educate patients on the importance of timely testing and treatment
chua