Proton Pump Inhibitors were adopted
in 1 country.
Recent:Hjärtström.
Feb 9 |
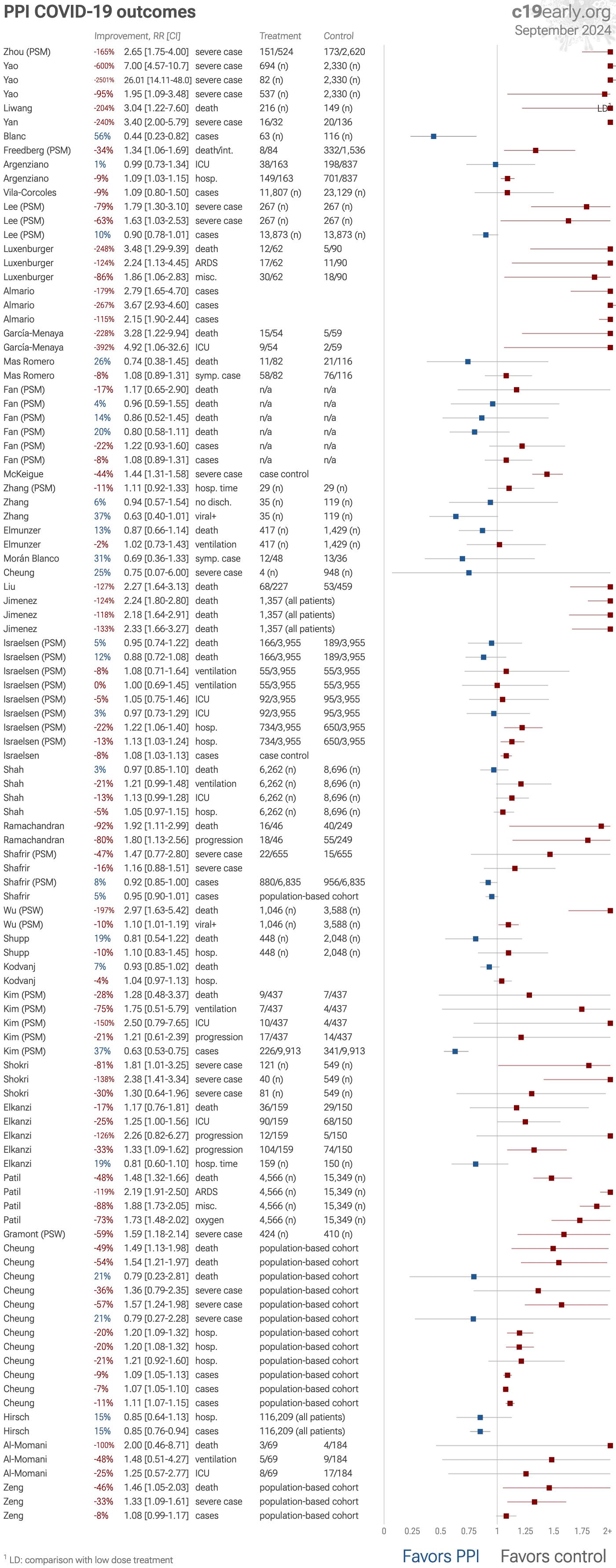
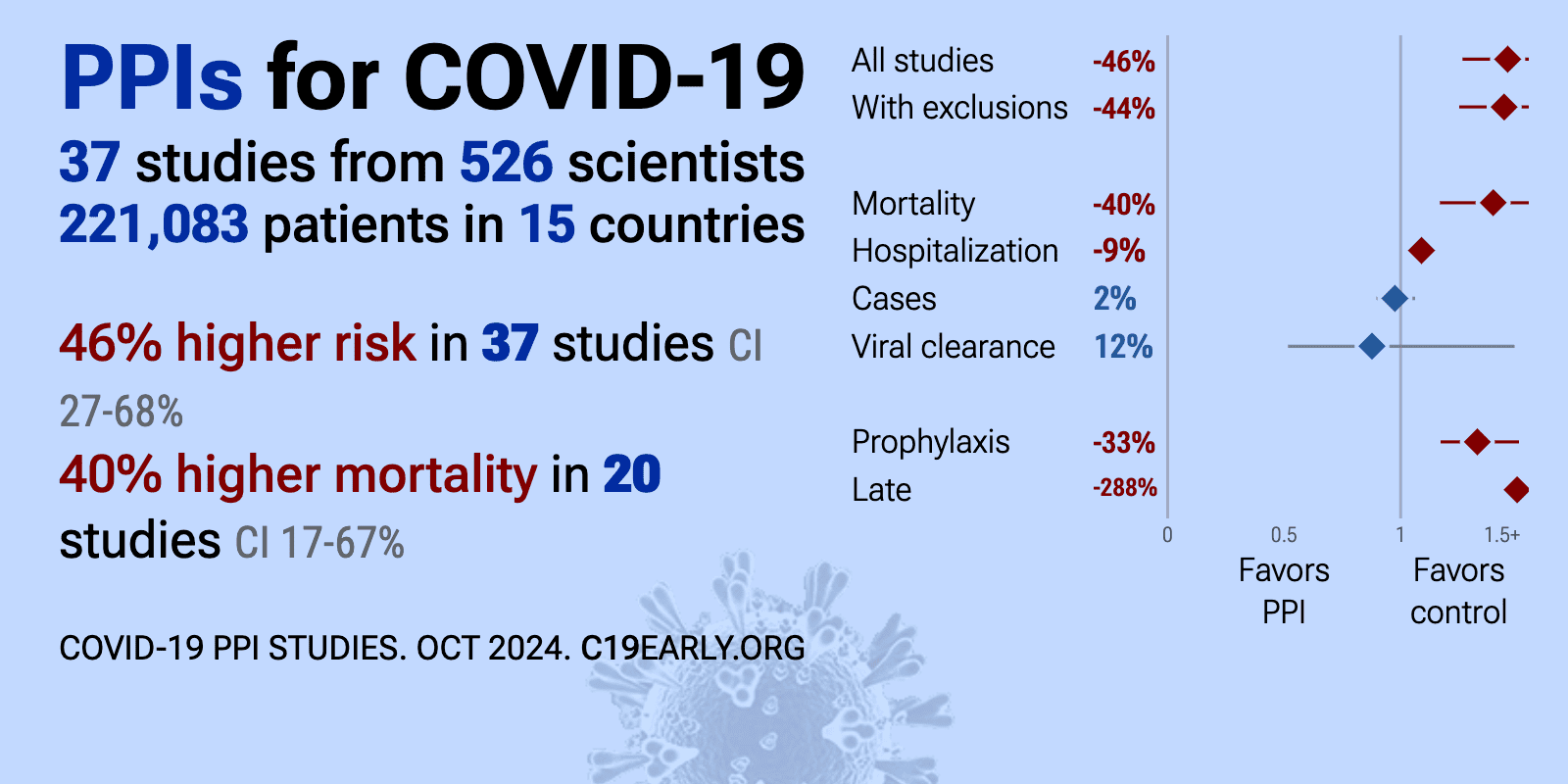
Proton Pump Inhibitors increase COVID-19 risk: real-time meta-analysis of 40 studies (Version 27) | |
| Meta-analysis shows 40% [17‑67%] higher mortality, and pooled analysis using the most serious outcome reported shows 46% [28‑67%] higher risk. Control Proton Pump InhibitorsPPIs Potential mechanisms of harm include i.. | ||
Oct 28 2025 |
et al., medRxiv, doi:10.1101/2025.10.27.25338863 | Polypharmacy and Proton Pump Inhibitor Use Independently Predict One-Year Mortality in Critical COVID-19: An Explainable AI–Based Survival Analysis |
| 743% higher mortality (p<0.0001). Retrospective 497 critically ill COVID-19 patients in Swedish ICUs showing proton pump inhibitor use associated with higher one-year mortality. The machine-learning survival model obscures conventional HR calculation; however, the additiv.. | ||
Jan 29 2025 |
et al., Clinical Kidney Journal, doi:10.1093/ckj/sfaf030 | COVID-19 among Kidney Transplant Recipients: Evaluating Risk Factors During the Initial Phase of the Pandemic |
| 58% higher combined mortality/hospitalization (p=0.0002). Retrospective 5,824 kidney transplant recipients in Sweden showing proton pump inhibitor use associated with higher risk of severe COVID-19. | ||
Oct 30 2024 |
et al., Annals of Medicine, doi:10.1080/07853890.2024.2399761 | Treatment with proton pump inhibitors is associated with secondary bacterial infections and sepsis in patients with COVID-19: a retrospective analysis of their joint impact on in-hospital prognosis |
| 37% higher combined mortality/ICU admission (p=0.09) and 96% worse results (p=0.0001). Retrospective 1,087 hospitalized COVID-19 patients showing significantly increased risk of secondary bacterial infections (SBIs) and secondary bacterial sepsis (SBS) sepsis with pre-admission proton pump inhibitor (PPI) use. Combined ICU.. | ||
Oct 25 2024 |
et al., Cureus, doi:10.7759/cureus.72385 | Association Between the Use of Proton Pump Inhibitors and Severe Clinical Outcomes in COVID-19 Patients: A Retrospective Observational Study |
| 57% higher hospitalization (p=0.15). Retrospective 506 outpatients in Oman showing no significant association between proton pump inhibitor (PPI) use and COVID-19 hospitalization in unadjusted results. | ||
Jul 16 2024 |
et al., eLife, doi:10.7554/elife.94973 | Associations of proton pump inhibitors with susceptibility to influenza, pneumonia, and COVID-19: Evidence from a large population-based cohort study |
| 46% higher mortality (p=0.02), 33% higher severe cases (p=0.004), and 8% more cases (p=0.1). UK Biobank retrospective with 160,923 patients showing increased risks of influenza, pneumonia, COVID-19 severity, and COVID-19 mortality with proton pump inhibitor (PPI) use. | ||
Jun 30 2024 |
et al., Annals of Medicine, doi:10.1080/07853890.2024.2355581 | Proton pump inhibitors and gastrointestinal symptoms among patients with COVID-19 infection |
| 100% higher mortality (p=0.39), 48% higher ventilation (p=0.54), and 25% higher ICU admission (p=0.64). Retrospective 254 hospitalized COVID-19 patients in Jordan showing higher rates of gastrointestinal symptoms such as abdominal pain and diarrhea with proton pump inhibitor (PPI) use. There were no significant differences for mortality, ve.. | ||
Jun 27 2024 |
et al., The Journal of Pediatrics, doi:10.1016/j.jpeds.2024.114179 | Proton Pump Inhibitors and Risk of COVID-19 Infection in Children |
| 15% lower hospitalization (p=0.27) and 15% fewer cases (p=0.002). Retrospective 116,209 pediatric patients showing lower risk of COVID-19 with PPI use. There was no significant difference for hospitalization. | ||
May 5 2024 |
et al., Journal of Gastroenterology and Hepatology, doi:10.1111/jgh.16601 | Proton pump inhibitors associated with severe COVID‐19 among two‐dose but not three‐dose vaccine recipients |
| 49% higher mortality (p=0.005), 36% higher severe cases (p=0.27), 20% higher hospitalization (p=0.0003), and 9% more cases (p<0.0001). Retrospective 627,514 patients in Hong Kong showing slightly higher risk of COVID-19 with pre-vaccination proton pump inhibitor (PPI) use in two-dose or three-dose vaccine recipients, and higher risk of hospitalization and severe outcomes.. | ||
Apr 15 2024 |
et al., Age and Ageing, doi:10.1093/ageing/afae082 | Proton pump inhibitors and risk of severe COVID-19 in older people |
| 59% higher severe cases (p=0.002). Retrospective 834 elderly patients in France showing higher risk of severe COVID-19 with PPI use, and increasing risk with increasing dosage. | ||
Mar 30 2024 |
et al., International Journal of Biomedical Science and Travel Medicine, doi:10.22225/ijbstm.1.1.2024.19-23 | Different Outcome in COVID-19 Patients with or without PPI Use: A Systematic Review and Meta-analysis |
| 99% higher severe cases (p=0.01). Meta analysis of 7 studies with over 30,000 COVID-19 patients showing 2 times higher risk of worse outcomes with proton pump inhibitor (PPI) use. | ||
Dec 31 2023 |
et al., Gastro Hep Advances, doi:10.1016/j.gastha.2022.08.004 | Factors Associated With Poor Outcomes Among Patients With SARS-CoV-2 Coronavirus Infection and Gastrointestinal Symptoms |
| 48% higher mortality (p<0.0001), 119% higher ARDS (p<0.0001), 88% worse results (p<0.0001), and 73% higher need for oxygen therapy (p<0.0001). Retrospective 19,915 hospitalized COVID-19 patients with gastrointestinal symptoms, showing that use of proton pump inhibitors or H2 receptor antagonists was associated with higher mortality, ARDS, sepsis, and ventilator or oxygen require.. | ||
Nov 17 2023 |
et al., Academic Journal of Gastroenterology & Hepatology, doi:10.33552/AJGH.2023.03.000568 | Effect of Preadmission Proton Pump Inhibitor (PPI) on the clinical outcome of Covid-19 Hospitalised Patients during the Pandemic |
| 17% higher mortality (p=0.49), 25% higher ICU admission (p=0.05), 126% higher progression (p=0.14), and 19% shorter hospitalization (p=0.18). Retrospective 309 hospitalized patients showing higher risk of severe cases (ASA≥3) with PPI use. | ||
Oct 1 2023 |
et al., JAMA Pediatrics, doi:10.1001/jamapediatrics.2023.2900 | Proton Pump Inhibitor Use and Risk of Serious Infections in Young Children |
| Analysis of 1.2 million children in France showing increased risk of serious infection with proton pump inhibitor (PPI) use. PPI exposure was associated with higher risk of infections in the digestive tract, ear/nose/throat, lower respira.. | ||
Mar 31 2023 |
et al., Annales Pharmaceutiques Françaises, doi:10.1016/j.pharma.2022.08.013 | What is the role of proton pump inhibitors consumption on the clinical presentation and severity of COVID-19 infection? |
| 81% higher severe cases (p=0.05) and 78% higher mortality (p=0.21). Retrospective 670 COVID-19 patients in Iran showing significantly higher COVID-19 severity scores and more symptomatic presentation in patients with a history of proton pump inhibitor (PPI) use. Adjusted results are only provided for seve.. | ||
Mar 21 2023 |
et al., Journal of Korean Medical Science, doi:10.3346/jkms.2023.38.e99 | Histamine-2 Receptor Antagonists and Proton Pump Inhibitors Are Associated With Reduced Risk of SARS-CoV-2 Infection Without Comorbidities Including Diabetes, Hypertension, and Dyslipidemia: A Propensity Score-Matched Nationwide Cohort Study |
| 28% higher mortality (p=0.63), 75% higher ventilation (p=0.37), 150% higher ICU admission (p=0.11), and 21% higher progression (p=0.6). PSM retrospective in South Korea, showing lower risk of COVID-19 cases with H2RA (including famotidine) and PPI use, but no significant difference in severe outcomes (results provided for the combined groups only). | ||
Oct 5 2022 |
et al., British Journal of Clinical Pharmacology, doi:10.1111/bcp.15525 | People exposed to proton‐pump inhibitors shortly preceding COVID‐19 diagnosis are not at an increased risk of subsequent hospitalizations and mortality: A nationwide matched cohort study |
| 7% lower mortality (p=0.12) and 4% higher hospitalization (p=0.32). Retrospective 433,609 COVID-19 patients in Croatia showing no significant difference in mortality or hospitalization risk with proton-pump inhibitor (PPI) use before COVID-19 diagnosis compared to matched controls with PPI-requiring morbi.. | ||
Aug 31 2022 |
et al., Gastroenterology Research, doi:10.14740/gr1545 | Proton Pump Inhibitors Use and Increased Risk of Spontaneous Bacterial Peritonitis in Cirrhotic Patients: A Retrospective Cohort Analysis |
| Retrospective 107,750 cirrhotic patients showing increased risk of spontaneous bacterial peritonitis (SBP) with proton pump inhibitor (PPI) use. PPI use was the strongest predictor of SBP, with patients on PPIs 4.24 times more likely to d.. | ||
Aug 3 2022 |
et al., Journal Of The Indonesian Medical Association, doi:10.47830/jinma-vol.72.2-2022-802 | High vs Low Dose Proton Pump Inhibitor (PPI) related Mortality in Hospitalized Coronavirus Disease-19 (COVID-19): A Retrospective Cohort Study |
| 204% higher mortality (p=0.02). Retrospective hospitalized COVID-19 patients in Indonesia showing higher mortality with high dose proton pump inhibitor (PPI) use compared to low dose. | ||
May 9 2022 |
et al., Scientific Reports, doi:10.1038/s41598-022-11680-0 | Proton pump inhibitor therapy usage and associated hospitalization rates and critical care outcomes of COVID-19 patients |
| 19% lower mortality (p=0.32) and 10% higher hospitalization (p=0.51). Retrospective 2,594 COVID-19 patients in the United States showing no significant association between proton pump inhibitor (PPI) use and COVID-19 severity, including need for hospitalization or 30-day mortality. There was increasing mort.. | ||
Feb 28 2022 |
et al., Tropical Medicine and Infectious Disease, doi:10.3390/tropicalmed7030037 | The Use of Proton Pump Inhibitors and COVID-19: A Systematic Review and Meta-Analysis |
| 12% higher mortality (p=0.05), 84% higher severe cases (p<0.0001), and 5% more cases (p=0.01). Meta-analysis of 14 studies with 477,157 COVID-19 patients showing PPI use was associated with higher cases, poor outcomes, and mortality. | ||
Feb 19 2022 |
et al., Journal of Global Health, doi:10.7189/jogh.12.05005 | Use of proton pump inhibitors are associated with higher mortality in hospitalized patients with COVID-19 |
| 197% higher mortality (p=0.0004) and 10% worse viral clearance (p=0.02). Retrospective 4,634 hospitalized COVID-19 patients in China, showing higher mortality and slower viral clearance with proton pump inhibitor (PPI) use. Authors hypothesize that PPIs may increase susceptibility to COVID-19 by increasing ACE.. | ||
Feb 4 2022 |
et al., Frontiers in Pharmacology, doi:10.3389/fphar.2022.791074 | The Association Between Proton Pump Inhibitors and COVID-19 is Confounded by Hyperglycemia in a Population-Based Study |
| 47% higher severe cases (p=0.32) and 8% fewer cases (p=0.06). Retrospective 255,355 adults in Israel showing no significant association between proton pump inhibitor (PPI) use and SARS-CoV-2 positivity or COVID-19 severity. | ||
Jan 31 2022 |
et al., Japanese Journal of Infectious Diseases, doi:10.7883/yoken.JJID.2021.074 | Does Proton Pump Inhibitor Use Lead to a Higher Risk of Coronavirus Disease 2019 Infection and Progression to Severe Disease? a Meta-analysis |
| 91% higher mortality (p=0.09), 67% higher severe cases (p<0.0001), 362% worse results (p<0.0001), and 64% more cases (p=0.39). Meta-analysis of 14 studies with over 268,683 subjects showing proton pump inhibitor (PPI) use was associated with increased risk of severe disease and increased risk of secondary infection. Mortality and cases were higher, without statis.. | ||
Jan 31 2022 |
et al., Therapeutic Advances in Gastroenterology, doi:10.1177/17562848221104365 | Impact of proton pump inhibitors on the in-hospital outcome of COVID-19 patients: a retrospective study |
| 600% higher severe cases (p<0.0001). Retrospective 3,024 hospitalized COVID-19 patients in China showing increased risk of the composite outcome of ICU admission, mechanical ventilation, or death with proton pump inhibitor (PPI) use. Intravenous administration was significan.. | ||
Nov 30 2021 |
et al., European Journal of Gastroenterology & Hepatology, doi:10.1097/MEG.0000000000002013 | Pre-hospitalization proton pump inhibitor use and clinical outcomes in COVID-19 |
| 92% higher mortality (p=0.02) and 80% higher progression (p=0.02). Retrospective 295 hospitalized COVID-19 patients showing higher mortality and acute respiratory distress syndrome (ARDS) with pre-hospitalization proton pump inhibitor (PPI) use. Authors hypothesize that hypochlorhydria caused by PPIs may.. | ||
Oct 18 2021 |
et al., Gut, doi:10.1136/gutjnl-2021-325701 | Proton-pump inhibitor use is not associated with severe COVID-19-related outcomes: a propensity score-weighted analysis of a national veteran cohort |
| 3% lower mortality (p=0.66), 21% higher ventilation (p=0.06), 13% higher ICU admission (p=0.06), and 5% higher hospitalization (p=0.26). Retrospective 14,958 US veterans who tested positive for SARS-CoV-2, showing no significant difference in severe COVID-19 outcomes (mechanical ventilation, death, ICU admission, or hospitalization) with proton pump inhibitor (PPI) use com.. | ||
Sep 30 2021 |
et al., Clinical Gastroenterology and Hepatology, doi:10.1016/j.cgh.2021.05.011 | Proton Pump Inhibitor Use Is Not Strongly Associated With SARS-CoV-2 Related Outcomes: A Nationwide Study and Meta-analysis |
| 5% lower mortality (p=0.7), 8% higher ventilation (p=0.73), 5% higher ICU admission (p=0.8), and 22% higher hospitalization (p=0.005). Retrospective 83,224 SARS-CoV-2 cases and 332,799 controls in Denmark showing increased risk of infection and hospital admission with proton pump inhibitor (PPI) use, but no significant association with ICU admission or mortality. | ||
Aug 31 2021 |
et al., Archives of Medical Research, doi:10.1016/j.arcmed.2021.03.004 | Proton Pump Inhibitors: Current Use and the Risk of Coronavirus Infectious Disease 2019 Development and its Related Mortality. Meta-analysis |
| 67% higher mortality (p<0.0001) and 19% more cases (p=0.61). Meta-analysis of 6 studies with 195,230 participants showing significantly higher COVID-19 mortality with PPI use. | ||
Aug 20 2021 |
et al., Frontiers in Medicine, doi:10.3389/fmed.2021.637885 | Acid pH Increases SARS-CoV-2 Infection and the Risk of Death by COVID-19 |
| 124% higher mortality (p<0.0001). In vitro study showing lower pH increased ACE2 expression and viral load on SARS-CoV-2 infection, and retrospective study showing proton pump inhibitor use, which is correlated with low gastric pH-related diseases, was associated with hig.. | ||
May 31 2021 |
et al., Clinical Microbiology and Infection, doi:10.1016/j.cmi.2021.01.008 | Proton pump inhibitor use and risk for recurrent Clostridioides difficile infection: a systematic review and meta-analysis |
| Meta-analysis of 16 studies with 57,477 patients showing significantly higher risk of recurrent Clostridioides difficile infection (CDI) in patients prescribed proton pump inhibitors (PPIs) compared to those not prescribed PPIs. The assoc.. | ||
May 27 2021 |
et al., American Journal of Gastroenterology, doi:10.14309/ajg.0000000000001311 | Increased ACE2 Levels and Mortality Risk of Patients With COVID-19 on Proton Pump Inhibitor Therapy |
| 127% higher mortality (p=0.001). Prospective study showing COVID- PPI users had higher salivary ACE2 expression, and retrospective analysis of 694 hospitalized COVID-19 patients, showing higher mortality with PPI use. | ||
Apr 30 2021 |
et al., Gastroenterology, doi:10.1053/j.gastro.2020.05.098 | Association Between Famotidine Use and COVID-19 Severity in Hong Kong: A Territory-wide Study |
| 25% lower severe cases (p=0.8). Retrospective 952 COVID-19 patients in Hong Kong, showing no significant difference in severe disease with famotidine use or PPI use. | ||
Apr 30 2021 |
et al., Pulmonary Pharmacology & Therapeutics, doi:10.1016/j.pupt.2021.101989 | Antihistamines and azithromycin as a treatment for COVID-19 on primary health care – A retrospective observational study in elderly patients |
| 31% fewer symptomatic cases (p=0.34). Retrospective 84 elderly nursing home residents in Spain showing no mortality, hospitalization, or ICU admission with early treatment with antihistamines alone or in combination with azithromycin. | ||
Apr 11 2021 |
et al., Pharmacological Reports, doi:10.1007/s43440-021-00263-x | Proton pump inhibitor on susceptibility to COVID-19 and its severity: a systematic review and meta-analysis |
| 85% higher severe cases (p=0.01) and 56% more cases (p=0.47). Meta-analysis of 12 studies with 290,455 patients showing increased risk of poor outcomes with proton pump inhibitor (PPI) use in COVID-19 patients, but not increased susceptibility. | ||
Mar 31 2021 |
et al., Gastroenterology, doi:10.1053/j.gastro.2020.11.007 | Association Between Preadmission Acid Suppressive Medication Exposure and Severity of Illness in Patients Hospitalized With COVID-19 |
| 13% lower mortality (p=0.31) and 2% higher ventilation (p=0.89). Retrospective 1,846 hospitalized COVID-19 patients in North America showing no significant association between preadmission proton pump inhibitor (PPI) use and mechanical ventilation or mortality. Results do not account for the risk of.. | ||
Feb 28 2021 |
et al., Journal of Inflammation Research, doi:10.2147/JIR.S292303 | Analysis of the Effect of Proton-Pump Inhibitors on the Course of COVID-19 |
| 11% longer hospitalization (p=0.29), 6% higher hospital discharge (p=0.82), and 37% improved viral clearance (p=0.05). Retrospective 154 hospitalized moderate COVID-19 patients in China showing no significant difference in viral clearance time or hospital stay duration with proton pump inhibitor (PPI) use. There was no association between PPI use and vira.. | ||
Feb 22 2021 |
et al., BMC Medicine, doi:10.1186/s12916-021-01907-8 | Relation of severe COVID-19 to polypharmacy and prescribing of psychotropic drugs: the REACT-SCOT case-control study |
| 44% higher severe cases (p<0.0001). Retrospective 4,251 severe COVID-19 cases and 36,738 matched controls in Scotland showing increased risk of severe COVID-19 with PPI use and antihistamine H1RA use. Adjusted results are only provided for the patients not in care homes (2,.. | ||
Jan 31 2021 |
et al., Gastroenterology, doi:10.1053/j.gastro.2020.09.028 | Effect of Acid Suppressants on the Risk of COVID-19: A Propensity Score-Matched Study Using UK Biobank |
| 17% higher mortality (p=0.69) and 22% more cases (p=0.15). PSM retrospective 9,469 UK Biobank participants tested for COVID-19, showing no significant association between proton pump inhibitor (PPI) or histamine-2 receptor antagonist (H2RA) use and risk of SARS-CoV-2 infection or COVID-19 mortali.. | ||
Dec 31 2020 |
et al., Digestive and Liver Disease, doi:10.1016/j.dld.2020.10.001 | Proton pump inhibitor use is associated with increased risk of severity and mortality from coronavirus disease 2019 (COVID-19) infection |
| 72% higher mortality (p=0.04) and 35% higher severe cases (p=0.002). Meta analysis of 6 studies with 5,884 COVID-19 patients showing significantly higher severity and mortality with proton pump inhibitor (PPI) usage. | ||
Dec 4 2020 |
et al., Gut, doi:10.1136/gutjnl-2020-323668 | Proton pump inhibitor or famotidine use and severe COVID-19 disease: a propensity score-matched territory-wide study |
| 165% higher severe cases (p=0.0001). Retrospective 4,445 COVID+ patients in China, showing higher risk of combined death/intubation/ICU with famotidine and with PPIs. | ||
Nov 10 2020 |
et al., Gut, doi:10.1136/gutjnl-2020-323366 | Do proton pump inhibitors influence SARS-CoV-2 related outcomes? A meta-analysis |
| 67% higher severe cases (p=0.003). Meta analysis of 16 studies from 10 countries with a total of 318,261 participants, showing current proton pump inhibitor (PPI) use was associated with higher risk of severe COVID-19 outcomes, but not with increased susceptibility to SARS.. | ||
Oct 27 2020 |
et al., PLOS ONE, doi:10.1371/journal.pone.0241030 | COVID-19 outbreak in long-term care facilities from Spain. Many lessons to learn |
| 26% lower mortality (p=0.44) and 8% more symptomatic cases (p=0.54). Retrospective 1,084 residents from 6 long-term care facilities in Spain showing no signficant difference in cases and mortality with PPI use in unadjusted results. | ||
Oct 20 2020 |
et al., Journal of Internal Medicine, doi:10.1111/joim.13183 | Use of proton pump inhibitors and risk of adverse clinical outcomes from COVID‐19: a meta‐analysis |
| 46% higher severe cases (p<0.0001) and 191% worse results (p=0.0006). Meta analysis of 5 studies with 37,372 total patients showing significantly increased odds of severe/fatal COVID-19 and significantly higher risk of secondary infections with proton pump inhibitor (PPI) use. | ||
Sep 16 2020 |
et al., Frontiers in Pharmacology, doi:10.3389/fphar.2020.570721 | Outcomes and Laboratory and Clinical Findings of Asthma and Allergic Patients Admitted With Covid-19 in a Spanish University Hospital |
| 228% higher mortality (p=0.008) and 392% higher ICU admission (p=0.02). Retrospective 113 hospitalized COVID-19 patients in Spain showing higher mortality and ICU admission with PPI use. | ||
Aug 25 2020 |
et al., American Journal of Gastroenterology, doi:10.14309/ajg.0000000000000798 | Increased Risk of COVID-19 Among Users of Proton Pump Inhibitors |
| 179% more cases (p=0.0001). Survey of 53,130 individuals with a history of GI symptoms showing increased risk of COVID-19 positivity with proton pump inhibitor (PPI) use, especially twice-daily PPI use. There was a dose-response relationship between PPI use and COVI.. | ||
Jul 31 2020 |
et al., Journal of Internal Medicine, doi:10.1111/joim.13121 | Treatment with proton pump inhibitors increases the risk of secondary infections and ARDS in hospitalized patients with COVID‐19: coincidence or underestimated risk factor? |
| 248% higher mortality (p=0.02), 124% higher ARDS (p=0.02), and 86% worse results (p=0.03). Retrospective 152 hospitalized COVID-19 patients showing increased risk of secondary infections, ARDS, and mortality with proton pump inhibitor (PPI) use. Authors hypothesize that reduced gastric acid production from PPIs leads to bacteri.. | ||
Jul 30 2020 |
et al., Gut, doi:10.1136/gutjnl-2020-322248 | Severe clinical outcomes of COVID-19 associated with proton pump inhibitors: a nationwide cohort study with propensity score matching |
| 79% higher severe cases (p=0.009) and 10% fewer cases (p=0.11). PSM retrospective 132,316 patients in South Korea, showing significantly higher risk of severe COVID-19 with PPI use, but no significant difference in cases. | ||
Jul 25 2020 |
et al., The Journal of Clinical Hypertension, doi:10.1111/jch.13948 | Use of distinct anti‐hypertensive drugs and risk for COVID‐19 among hypertensive people: A population‐based cohort study in Southern Catalonia, Spain |
| 9% more cases (p=0.58). Retrospective 34,936 hypertensive outpatients in Spain showing no significant difference in COVID-19 cases with PPIs and antihistamine H1RAs. | ||
May 29 2020 |
et al., BMJ, doi:10.1136/bmj.m1996 | Characterization and clinical course of 1000 patients with coronavirus disease 2019 in New York: retrospective case series |
| 1% lower ICU admission (p=1) and 9% higher hospitalization (p=0.01). Retrospective 1,000 hospitalized COVID-19 patients in New York City showing high rates of acute kidney injury, inpatient dialysis, prolonged intubation times, and length of stay compared to previous cohorts. | ||
May 21 2020 |
et al., Gastroenterology, doi:10.1053/j.gastro.2020.05.053 | Famotidine Use Is Associated With Improved Clinical Outcomes in Hospitalized COVID-19 Patients: A Propensity Score Matched Retrospective Cohort Study |
| 34% higher combined mortality/intubation (p=0.01). PSM retrospective 1,620 hospitalized patients in the USA, showing higher risk of combined death/intubation with PPI treatment. | ||
May 2 2020 |
et al., Preprints, doi:10.20944/preprints202005.0016.v1 | Interest of Proton Pump Inhibitors in Reducing the Occurrence of COVID-19: A Case-Control Study |
| 56% fewer cases (p=0.005). Retrospective 179 elderly patients in France, showing higher risk of COVID-19 cases with acetaminophen use, without statistical significance. | ||
Mar 23 2020 |
et al., medRxiv, doi:10.1101/2020.03.19.20038539 | Clinical Characteristics of Coronavirus Disease 2019 in Hainan, China |
| 240% higher severe cases (p<0.0001). Retrospective 168 hospitalized COVID-19 patients in China showing higher risk of severe cases with acid suppression drugs. | ||
Jun 1 2017 |
et al., JAMA Internal Medicine, doi:10.1001/jamainternmed.2017.0212 | Association of Gastric Acid Suppression With Recurrent Clostridium difficile Infection |
| Meta-analysis of 16 observational studies with 7,703 patients showing increased risk of recurrent C. difficile infection with gastric acid suppressant use (PPIs alone or PPIs/H2RAs). | ||
Dec 31 2015 |
et al., Genetics and Molecular Research, doi:10.4238/2015.July.3.25 | Proton pump inhibitor use and risk of spontaneous bacterial peritonitis in cirrhotic patients: a systematic review and meta-analysis |
| Meta analysis of 17 observational studies with 8,204 patients showing 2-fold increased risk of spontaneous bacterial peritonitis (SBP) and overall bacterial infection with proton pump inhibitor (PPI) use in cirrhotic patients with ascites.. | ||