Treatment with proton pump inhibitors is associated with secondary bacterial infections and sepsis in patients with COVID-19: a retrospective analysis of their joint impact on in-hospital prognosis
et al., Annals of Medicine, doi:10.1080/07853890.2024.2399761, Oct 2024
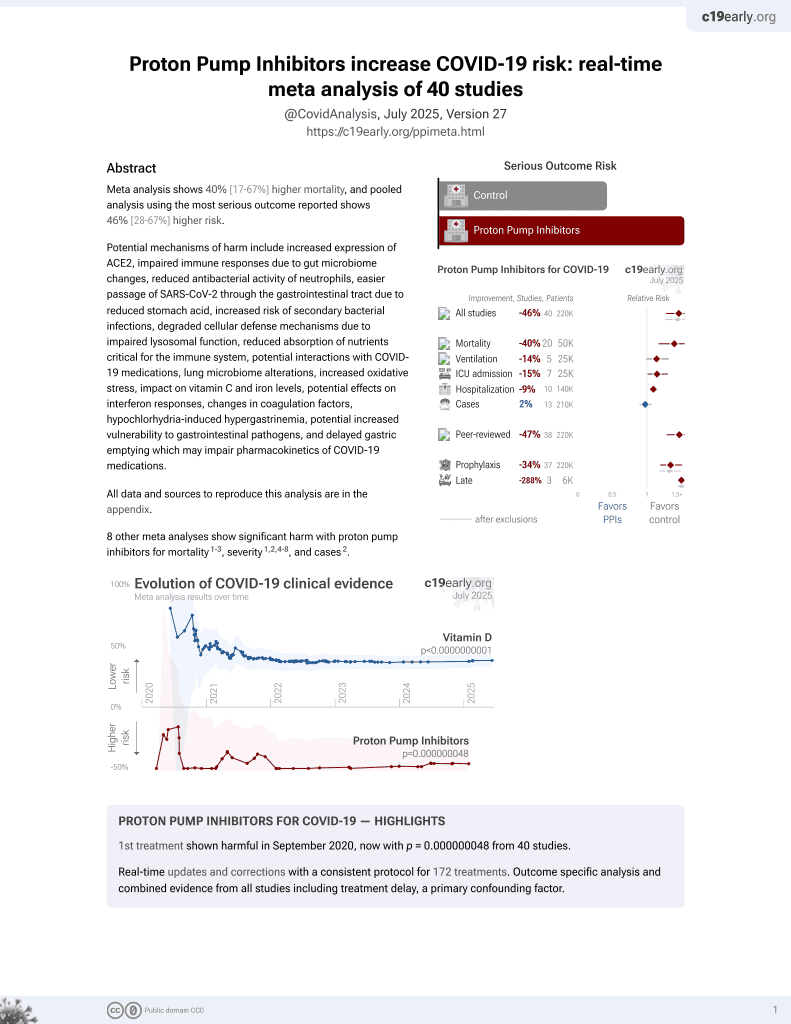
PPIs for COVID-19
1st treatment shown to increase risk in
September 2020, now with p = 0.000000048 from 40 studies.
6,400+ studies for
210+ treatments. c19early.org
|
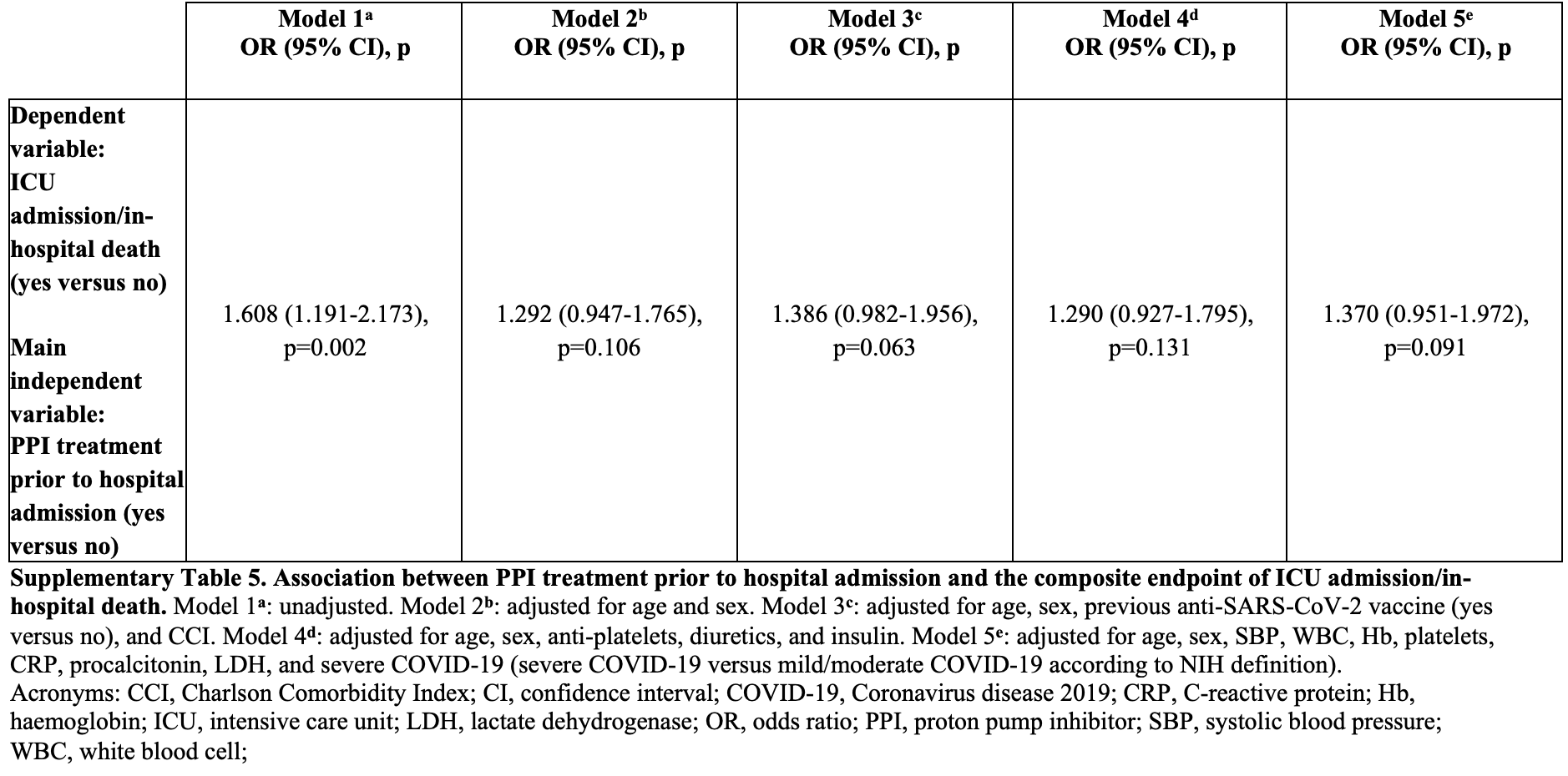
Retrospective 1,087 hospitalized COVID-19 patients showing significantly increased risk of secondary bacterial infections (SBIs) and secondary bacterial sepsis (SBS) sepsis with pre-admission proton pump inhibitor (PPI) use. Combined ICU admission/mortality was higher but without statistical significance.
|
risk of death/ICU, 37.0% higher, OR 1.37, p = 0.09, treatment 447, control 640, adjusted per study, multivariable, model 5, RR approximated with OR.
|
|
risk of miscellaneous, 95.5% higher, OR 1.96, p < 0.001, treatment 447, control 640, adjusted per study, SBI, multivariable, model 5, RR approximated with OR.
|
|
risk of miscellaneous, 67.0% higher, OR 1.67, p = 0.002, treatment 447, control 640, adjusted per study, SBS, multivariable, model 5, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Bianconi et al., 30 Oct 2024, retrospective, Italy, peer-reviewed, 11 authors.
Treatment with proton pump inhibitors is associated with secondary bacterial infections and sepsis in patients with COVID-19: a retrospective analysis of their joint impact on in-hospital prognosis
Annals of Medicine, doi:10.1080/07853890.2024.2399761
Introduction and objectives. secondary bacterial infections (sBis) contribute to worse in-hospital outcomes in patients with coronavirus disease 2019 . treatment with proton pump inhibitors (PPis) is associated with an increased risk of bacterial infections in different clinical settings. however, the association between PPi treatment prior to hospital admission and the occurrence of either sBis or secondary bacterial sepsis (sBs) as well as their joint impact on clinical outcomes of patients hospitalized for cOViD-19 are not clarified. Patients and methods. We retrospectively analyzed preadmission PPi use, in-hospital occurrence of sBis and sBs, and in-hospital outcomes of a cohort of patients hospitalized for cOViD-19. Results. among 1087 patients, 447 (41%) were on PPi treatment prior to hospital admission. During the hospital stay, 197 (18%) and 223 (20%) patients were diagnosed with sBis and sBs, respectively. the composite endpoint of intensive care unit (icU) admission/in-hospital death was met by 214 (20%) patients. Preadmission PPi treatment was independently associated with up to a 2.1-fold and 1.7-fold increased risk of sBis and sBs, respectively. the occurrence of sBs was independently associated with up to a 2.2-fold increased risk of icU admission/in-hospital death. a significant preadmission PPi treatment x sBs interaction emerged in predicting icU admission/ in-hospital death (F = 5.221, p interaction = 0.023). Conclusions. PPi treatment prior to hospital admission for cOViD-19 is associated with an increased risk of sBis and sBs. in addition, it interacts with sBs in predicting in-hospital prognosis. an appropriate use of PPis may attenuate the risk of adverse clinical outcomes during hospitalization for cOViD-19.
Ethics approval statement this study was conducted according to the guidelines of the Declaration of helsinki and approved by the local ethics committee (ceR Umbria, protocol code: 18342/20/OV; date of approval: 7 May 2020).
Author contributions conception and design: V.B. and M.P. analysis and interpretation of the data: V.B., M.R.M., F.F., F.R., s.D., V.Z., M.c., a.s., a.G., R.l., R.P., and M.P. Drafting of the paper: V.B., F.R., and M.P. Revising the paper critically for intellectual content: V.B., M.R.M., a.s., and M.P. Final approval of the version to be published and agreement to be accountable for all aspects of the work: V.B., M.R.M., F.F., F.R., s.D., V.Z., M.c., a.s., a.G., R.l., R.P., and M.P.
Disclosure statement the authors declare that they have no conflicts of interest with respect to the research, authorship, and/or publication of this manuscript. No financial or personal relationships with individuals or organizations have influenced or could be perceived to have influenced the work presented in this paper.
References
Bavishi, Dupont Hl, systematic review: the use of proton pump inhibitors and increased susceptibility to enteric infection, aliment Pharmacol ther, doi:10.1111/j.1365-2036.2011.04874.x
Benson Aa, Katz Lh, the association between proton pump inhibitors and cOViD-19 is confounded by hyperglycemia in a population-based study, Front Pharmacol, doi:10.3389/fphar.2022.791074
Bianconi, Mannarino, Figorilli, the detrimental impact of elevated ferritin to iron ratio on in-hospital prognosis of patients with cOViD-19, expert Rev Mol Diagn, doi:10.1080/14737159.2022.2052047
Bianconi, Mannarino, Ramondino, lipoprotein(a) does not predict thrombotic events and in-hospital outcomes in patients with cOViD-19, J clin Med, doi:10.3390/jcm12103543
Bianconi, Mannarino, the impact of statin therapy on in-hospital prognosis and endothelial function of patients at high-to-very high cardiovascular risk admitted for cOViD-19, J Med Virol
Biever, treatment with proton pump inhibitors increases the risk of secondary infections and aRDs in hospitalized patients with cOViD-19: coincidence or underestimated risk factor?, J intern Med, doi:10.1111/joim.13121
Boster, Ml, Reducing the inappropriate use of proton pump inhibitors in an internal medicine residency clinic, cureus, doi:10.7759/cureus.6609
Charlson Me, Guidi, charlson comorbidity index: a critical review of clinimetric properties, Psychother Psychosom, doi:10.1159/000521288
Cheng Vc, Jh, a novel risk factor associated with colonization by carbapenemase-producing enterobacteriaceae: use of proton pump inhibitors in addition to antimicrobial treatment, infect control hosp epidemiol, doi:10.1017/ice.2016.202
Christian, Martinez-Martinez L, eUcast guidelines for detection of resistance mechanisms and specific resistances of clinical and/or epidemiological importance, Version
De Bruyn A, Verellen S, Bruckers, secondary infection in cOViD-19 critically ill patients: a retrospective single-center evaluation, BMc infect Dis, doi:10.1186/s12879-022-07192-x
De Jager Cp, Pc, Gemen, Proton pump inhibitor therapy predisposes to community-acquired streptococcus pneumoniae pneumonia, aliment Pharmacol ther, doi:10.1111/apt.12069
Fatima, the use of proton pump inhibitors and cOViD-19: a systematic review and meta-analysis, trop Med infect Dis, doi:10.3390/tropicalmed7030037
Franchi C, Mannucci, Nobili, Use and prescription appropriateness of drugs for peptic ulcer and gastrooesophageal reflux disease in hospitalized older people, eur J clin Pharmacol, doi:10.1007/s00228-019-02815-w
Ga, Fanous, Viral strategies predisposing to respiratory bacterial superinfections, Pediatr Pulmonol, doi:10.1002/ppul.24699
Gulmez, Frederiksen, Use of proton pump inhibitors and the risk of community acquired pneumonia: a population-based case-control study, arch intern Med, doi:10.1001/archinte.167.9.950
Gupta A, Madhavan, extrapulmonary manifestations of cOViD-19, Nat Med, doi:10.1038/s41591-020-0968-3
Hoque, Mishu Id, Microbial co-infections in cOViD-19: associated microbiota and underlying mechanisms of pathogenesis, Microb Pathog, doi:10.1016/j.micpath.2021.104941
Jeon Cy, Lim, Use of acid-suppressive drugs and risk of pneumonia: a systematic review and meta-analysis, cMaJ, doi:10.1503/cmaj.092129
Js, Watson L, Parmasad, Prevalence and outcomes of co-infection and superinfection with saRs-coV-2 and other pathogens: a systematic review and meta-analysis, Plos One, doi:10.1371/journal.pone.0251170
Kostev, Galle, Proton pump inhibitor use is associated with a variety of infections in patients with liver cirrhosis, Medicine, doi:10.1097/MD.0000000000023436
Koyyada, long-term use of proton pump inhibitors as a risk factor for various adverse manifestations, therapie, doi:10.1016/j.therap.2020.06.019
Langford, antimicrobial resistance in patients with cOViD-19: a systematic review and meta-analysis, lancet Microbe, doi:10.1016/S2666-5247(22)00355-X
Li, Cai, Risk factors of secondary infections in severe and critical patients hospitalized with cOViD-19; a case-control study, Research square, doi:10.21203/rs.3.rs-55958/vl
Li, Xx, Yu, Do proton pump inhibitors influence saRs-coV-2 related outcomes? a meta-analysis, Gut, doi:10.1136/gutjnl-2020-323366
Liu, Jakobs, Rink, Proton-pump inhibitors suppress t cell response by shifting intracellular zinc distribution, int J Mol sci, doi:10.3390/ijms24021191
Lombardo L, Foti, Ruggia, increased incidence of small intestinal bacterial overgrowth during proton pump inhibitor therapy, clin Gastroenterol hepatol, doi:10.1016/j.cgh.2009.12.022
Ma, Goodrich, Me, Proton pump inhibitors alter the composition of the gut microbiota, Gut, doi:10.1136/gutjnl-2015-310861
Mbuntcha Hg, Kuete, What approaches to thwart bacterial efflux pumps-mediated resistance? antibiotics, doi:10.3390/antibiotics11101287
Miller, Binnicker, a guide to utilization of the microbiology laboratory for diagnosis of infectious diseases: 2018 update by the infectious diseases society of america and the american society for microbiology, clin infect Dis, doi:10.1093/cid/ciy584
Namazi, Jowkar, a succinct review of the general and immunological pharmacologic effects of proton pump inhibitors, J clin Pharm ther, doi:10.1111/j.1365-2710.2008.00907.x
Okur, Omeprazole inhibits natural killer cell functions, Dig Dis sci, doi:10.1007/s10620-007-9869-2
Oliva, Risk factors and effect on mortality of superinfections in a newly established cOViD-19 respiratory sub-intensive care unit at University hospital in Rome, BMc Pulm Med, doi:10.1186/s12890-023-02315-9
Pirro, Mannarino, Ministrini, effects of a nutraceutical combination on lipids, inflammation and endothelial integrity in patients with subclinical inflam-mation: a randomized clinical trial, sci Rep, doi:10.1038/srep23587
Pourajam S, Kalantari, secondary bacterial infection and clinical characteristics in patients with cOViD-19 admitted to two intensive care units of an academic hospital in iran during the first wave of the pandemic, Front cell infect Microbiol, doi:10.3389/fcimb.2022.784130
Qin C, Zhou L, Hu, Dysregulation of immune response in patients with coronavirus 2019 (cOViD-19) in Wuhan, china, clin infect Dis, doi:10.1093/cid/ciaa248
Rababa, h a. the inappropriate use of proton pump inhibitors and its associated factors among community-dwelling older adults, heliyon, doi:10.1016/j.heliyon.2021.e07595
Ramachandran, Perisetti A, Gajendran, Pre-hospitalization proton pump inhibitor use and clinical outcomes in cOViD-19, eur J Gastroenterol hepatol, doi:10.1097/MEG.0000000000002013
Rf, the interface between cOViD-19 and bacterial healthcare-associated infections, clin Microbiol infect, doi:10.1016/j.cmi.2021.06.001
St, long-term proton pump inhibitors induces recurrent urinary tract infections: a case study, iOP conf ser earth environ sci, doi:10.1088/1755-1315/293/1/012017
Willems, Mc, Kaiser, association of proton pump inhibitor use with risk of acquiring drug-resistant enterobacterales, JaMa Netw Open, doi:10.1001/jamanetworkopen.2023.0470
Zedtwitz-Liebenstein, Patruta, Omeprazole treatment diminishes intra-and extracellular neutrophil reactive oxygen production and bactericidal activity, crit care Med, doi:10.1097/00003246-200205000-00026
Zhang, Dong, Liu Gh, Risk and protective factors for cOViD-19 morbidity, severity, and mortality, clin Rev allergy immunol, doi:10.1007/s12016-022-08921-5
Zhou Sj, Sq, Ma, association of proton pump inhibitors with the occurrence of gut-derived bacteraemia in patients with haematological malignancy after chemotherapy, hematology, doi:10.1080/10245332.2016.1142711