The Use of Proton Pump Inhibitors and COVID-19: A Systematic Review and Meta-Analysis
et al., Tropical Medicine and Infectious Disease, doi:10.3390/tropicalmed7030037, Feb 2022
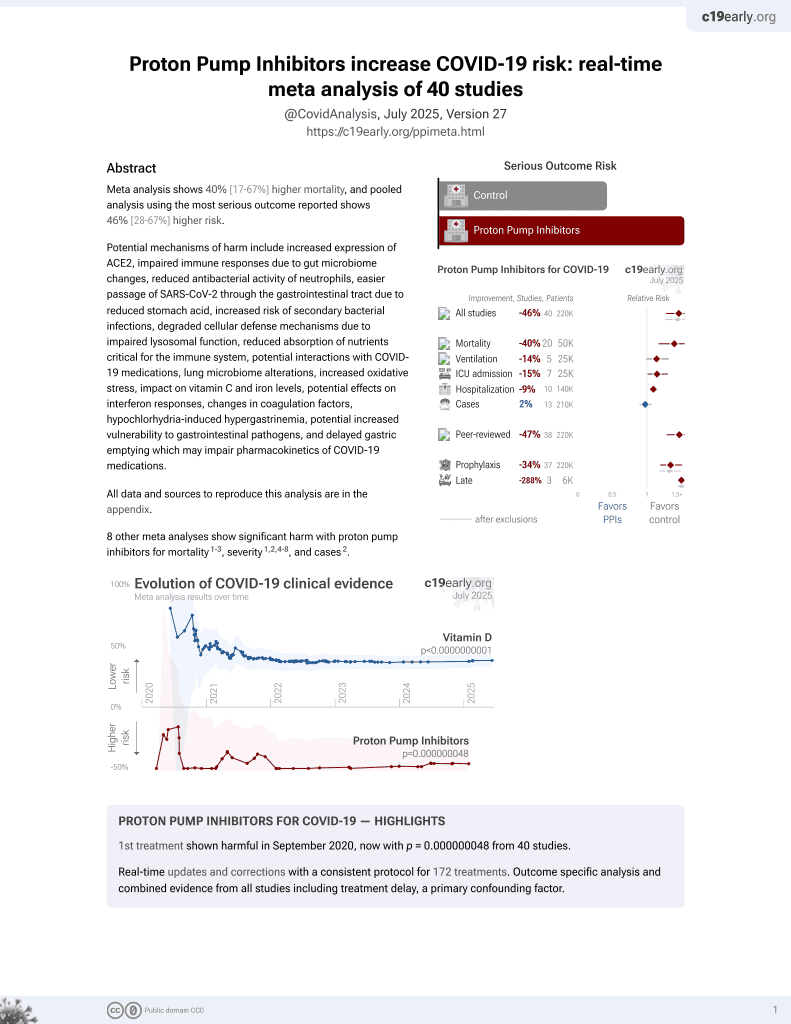
PPIs for COVID-19
1st treatment shown to increase risk in
September 2020, now with p = 0.000000048 from 40 studies.
6,400+ studies for
210+ treatments. c19early.org
|
Meta-analysis of 14 studies with 477,157 COVID-19 patients showing PPI use was associated with higher cases, poor outcomes, and mortality.
8 meta-analyses show significant harm with proton pump inhibitors for mortality1-3,
severity1,2,4-8 , and
cases2.
Currently there are 40 proton pump inhibitors for COVID-19 studies, showing 40% higher mortality [17‑67%], 14% higher ventilation [-1‑32%], 15% higher ICU admission [1‑30%], 9% higher hospitalization [3‑16%], and 2% fewer cases [-6‑10%].
|
risk of death, 12.0% higher, OR 1.12, p = 0.046, RR approximated with OR.
|
|
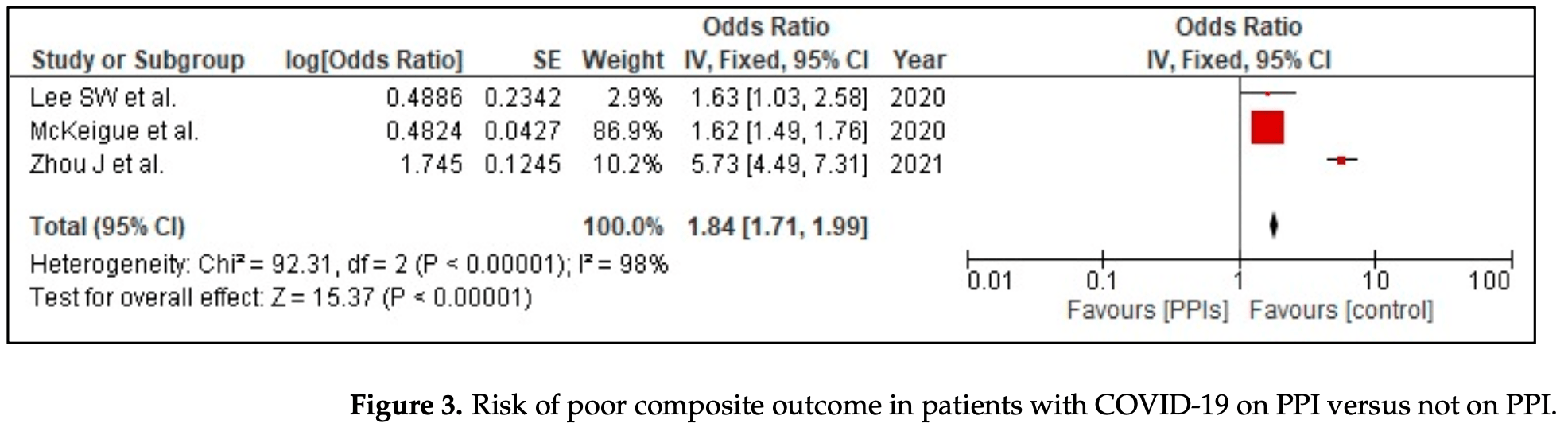
risk of severe case, 84.0% higher, OR 1.84, p < 0.001, RR approximated with OR.
|
|
risk of case, 5.0% higher, OR 1.05, p = 0.01, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Hariyanto et al., Proton pump inhibitor use is associated with increased risk of severity and mortality from coronavirus disease 2019 (COVID-19) infection, Digestive and Liver Disease, doi:10.1016/j.dld.2020.10.001.
2.
Fatima et al., The Use of Proton Pump Inhibitors and COVID-19: A Systematic Review and Meta-Analysis, Tropical Medicine and Infectious Disease, doi:10.3390/tropicalmed7030037.
3.
Toubasi et al., Proton Pump Inhibitors: Current Use and the Risk of Coronavirus Infectious Disease 2019 Development and its Related Mortality. Meta-analysis, Archives of Medical Research, doi:10.1016/j.arcmed.2021.03.004.
4.
Wardhana et al., Different Outcome in COVID-19 Patients with or without PPI Use: A Systematic Review and Meta-analysis, International Journal of Biomedical Science and Travel Medicine, doi:10.22225/ijbstm.1.1.2024.19-23.
5.
Yan et al., Does Proton Pump Inhibitor Use Lead to a Higher Risk of Coronavirus Disease 2019 Infection and Progression to Severe Disease? a Meta-analysis, Japanese Journal of Infectious Diseases, doi:10.7883/yoken.JJID.2021.074.
6.
Li et al., Do proton pump inhibitors influence SARS-CoV-2 related outcomes? A meta-analysis, Gut, doi:10.1136/gutjnl-2020-323366.
Fatima et al., 28 Feb 2022, peer-reviewed, 11 authors.
Contact: talalalmas.almas@gmail.com (corresponding author), kaneezfatima344@gmail.com, aimanrahim2001@gmail.com, zukhrufarshad200@gmail.com, adeenamusheer06@gmail.com, shan.lakhani@scholar.aku.edu, arshia.jahangir@scholar.aku.edu, abdullah.ahmed@scholar.aku.edu, ayra.siddiqui@scholar.aku.edu, saleha.qureshi@scholar.aku.edu, shilpa.golani@scholar.aku.edu.
The Use of Proton Pump Inhibitors and COVID-19: A Systematic Review and Meta-Analysis
Tropical Medicine and Infectious Disease, doi:10.3390/tropicalmed7030037
COVID-19 has proved to be a serious, and consequential disease that has affected millions of people globally. Previously, the adverse effects of proton pump inhibitors (PPI) have been observed with increasing the risk of pneumonia and COVID-19. This meta-analysis aims to address the relationship between the use of PPI and the severity of COVID-19 infection. We conducted a systemic literature search from PUBMED, Science Direct, and Cinahl from December 2019 to January 2022. Published and unpublished randomized control trials and cohort studies were included. Review Manager was used for all statistical analyses. In total, 14 studies were included in this systemic review and meta-analysis. Outcomes of interest include: (1) susceptibility of COVID-19 infection and (2) severity of COVID-19 (defined as the composite of poor outcomes: ICU admission, need for oxygen therapy, need for a ventilator, or death), and (3) mortality due to COVID-19. PPI use was marginally associated with a nominal but statistically significant increase in the risk of COVID-19 infection (OR 1.05 [1.01, 1.09]; I 2 97%, p = 0.007). PPI use also increased the risk of the composite poor outcome (OR 1.84 [1.71, 1.99]; I 2 98%, p < 0.00001) and mortality (OR 1.12 [1.00, 1.25]; I 2 84%, p = 0.05) in patients with COVID-19.
Informed Consent Statement: Not applicable.
Conflicts of Interest: The authors declare no conflict of interest.
References
Adir, Humbert, Saliba, COVID-19 risk and outcomes in adult asthmatic patients treated with biologics or systemic corticosteroids: Nationwide real-world evidence, J. Allergy Clin. Immunol, doi:10.1016/j.jaci.2021.06.006
Almario, Chey, Spiegel, Increased Risk of COVID-19 Among Users of Proton Pump Inhibitors, Am. J. Gastroenterol, doi:10.14309/ajg.0000000000000798
Arendse, Danser, Poglitsch, Touyz, Burnett et al., Novel Therapeutic Approaches Targeting the Renin-Angiotensin System and Associated Peptides in Hypertension and Heart Failure, Pharmacol. Rev, doi:10.1124/pr.118.017129
Biswas, Benedict, Lynch, Levine, Potential immunological consequences of pharmacological suppression of gastric acid production in patients with multiple sclerosis, BMC Med, doi:10.1186/1741-7015-10-57
Blanc, Waechter, Vogel, Schorr, Demuynck et al., Interest of Proton Pump Inhibitors in Reducing the Occurrence of COVID-19: A Case-Control Study, Preprints, doi:10.20944/preprints202005.0016.v1
Blanco, Bonilla, Homma, Suzuki, Fremont-Smith et al., Antihistamines and azithromycin as a treatment for COVID-19 on primary health care-A retrospective observational study in elderly patients, Pulm. Pharmacol. Ther, doi:10.1016/j.pupt.2021.101989
Brusselaers, Wahlin, Engstrand, Lagergren, Maintenance therapy with proton pump inhibitors and risk of gastric cancer: A nationwide population-based cohort study in Sweden, BMJ Open, doi:10.1136/bmjopen-2017-017739
Caplin, Khan, Savage, Rode, Varro et al., Expression and processing of gastrin in hepatocellular carcinoma, fibrolamellar carcinoma and cholangiocarcinoma, J. Hepatol, doi:10.1016/S0168-8278(99)80114-7
Cavalcoli, Zilli, Conte, Ciafardini, Massironi, Gastric neuroendocrine neoplasms and proton pump inhibitors: Fact or coincidence?, Scand. J. Gastroenterol, doi:10.3109/00365521.2015.1054426
Charpiat, Bleyzac, Tod, Proton Pump Inhibitors are Risk Factors for Viral Infections: Even for COVID-19?, Clin. Drug Investig, doi:10.1007/s40261-020-00963-x
Elmunzer, Wolf, Scheiman, Tierney, Taylor, Association Between Preadmission Acid Suppressive Medication Exposure and Severity of Illness in Patients Hospitalized With COVID-19, Gastroenterology, doi:10.1053/j.gastro.2020.11.007
Fan, Liu, Miyata, Dasarathy, Rotroff et al., Effect of Acid Suppressants on the Risk of COVID-19: A Propensity Score-Matched Study Using UK Biobank, Gastroenterology, doi:10.1053/j.gastro.2020.09.028
Fitzgibbon, Mills, The microbiota and immune-mediated diseases: Opportunities for therapeutic intervention, Eur. J. Immunol, doi:10.1002/eji.201948322
Ghebremariam, Cooke, Gerhart, Griego, Brower et al., Pleiotropic effect of the proton pump inhibitor esomeprazole leading to suppression of lung inflammation and fibrosis, J. Transl. Med, doi:10.1186/s12967-015-0614-x
Haastrup, Thompson, Søndergaard, Jarbøl, Side Effects of Long-Term Proton Pump Inhibitor Use: A Review, Basic Clin. Pharmacol. Toxicol, doi:10.1111/bcpt.13023
Hariyanto, Prasetya, Kurniawan, Proton pump inhibitor use is associated with increased risk of severity and mortality from coronavirus disease 2019 (COVID-19) infection, Dig. Liver Dis. Off. J. Ital. Soc. Gastroenterol. Ital. Assoc. Study Liver, doi:10.1016/j.dld.2020.10.001
Higgins, Thomas, Chandler, Cumpston, Li et al., Cochrane Handbook for Systematic Reviews of Interventions, version 6.2
Higgins, Thompson, Deeks, Altman, Measuring inconsistency in meta-analyses, BMJ, doi:10.1136/bmj.327.7414.557
Hoffmann, Kleine-Weber, Schroeder, Krüger, Herrler et al., SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor, Cell, doi:10.1016/j.cell.2020.02.052
Huh, Ji, Kang, Hong, Bae et al., Association of previous medications with the risk of COVID-19: A nationwide claims-based study from South Korea, MedRxiv, doi:10.1101/2020.05.04.20089904
Imhann, Bonder, Vila, Fu, Mujagic et al., Proton pump inhibitors affect the gut microbiome, Gut, doi:10.1136/gutjnl-2015-310376
Israelsen, Ernst, Lundh, Lundbo, Sandholdt et al., Proton Pump Inhibitor Use Is Not Strongly Associated With SARS-CoV-2 Related Outcomes: A Nationwide Study and Meta-analysis, Clin. Gastroenterol. Hepatol. Off. Clin. Pract. J. Am. Gastroenterol. Assoc, doi:10.1016/j.cgh.2021.05.011
Jordan, Adab, Cheng, COVID-19: Risk factors for severe disease and death, BMJ, doi:10.1136/bmj.m1198
Ksi Ądzyna, Szel Ąg, Paradowski, Overuse of proton pump inhibitors, Pol. Arch. Med. Wewn, doi:10.20452/pamw.2790
Laheij, Sturkenboom, Hassing, Dieleman, Stricker et al., Risk of community-acquired pneumonia and use of gastric acid-suppressive drugs, JAMA, doi:10.1001/jama.292.16.1955
Lee, Ha, Yeniova, Moon, Kim et al., Severe clinical outcomes of COVID-19 associated with proton pump inhibitors: A nationwide cohort study with propensity score matching, Gut, doi:10.1136/gutjnl-2020-322248
Lee, Yang, Yoo, Moon, Ha et al., Proton pump inhibitors and the risk of severe COVID-19: A post-hoc analysis from the Korean nationwide cohort, Gut, doi:10.1136/gutjnl-2020-323672
Li, Xie, Al-Aly, The association of proton pump inhibitors and chronic kidney disease: Cause or confounding?, Curr. Opin. Nephrol. Hypertens, doi:10.1097/MNH.0000000000000406
Liberati, Altman, Tetzlaff, Mulrow, Gøtzsche et al., The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration, PLoS Med
Lin, Chang, Lin, Hu, Hou et al., Proton Pump Inhibitors Increase the Risk of Autoimmune Diseases: A Nationwide Cohort Study, Front. Immunol, doi:10.3389/fimmu.2021.736036
Liu, Sloan, Owings, Figgins, Gauthier et al., Increased ACE2 Levels and Mortality Risk of Patients With COVID-19 on Proton Pump Inhibitor Therapy, Am. J. Gastroenterol, doi:10.14309/ajg.0000000000001311
Mckeigue, Kennedy, Weir, Bishop, Mcgurnaghan et al., Relation of severe COVID-19 to polypharmacy and prescribing of psychotropic drugs: The REACT-SCOT case-control study, BMC Med, doi:10.1186/s12916-021-01907-8
Palencia-Herrejón, Sánchez, Escobar, Gómez-Lus, Proton pump inhibitors and infection risk, Rev. Esp. Quimioter. Publ. Of. Soc. Esp. Quimioter
Pranata, Huang, Lawrensia, Henrina, Lim et al., Proton pump inhibitor on susceptibility to COVID-19 and its severity: A systematic review and meta-analysis, Pharmacol. Rep, doi:10.1007/s43440-021-00263-x
Price, Treacher, Reduced gastric acidity, proton pump inhibitors and increased severity of COVID-19 infections, Crit. Care, doi:10.1186/s13054-021-03497-6
Ramachandran, Perisetti, Gajendran, Jean-Louis, Bansal et al., Pre-hospitalization proton pump inhibitor use and clinical outcomes in COVID-19, Eur. J. Gastroenterol. Hepatol, doi:10.1097/MEG.0000000000002013
Sattar, Valabhji, Obesity as a Risk Factor for Severe COVID-19: Summary of the Best Evidence and Implications for Health Care, Curr. Obes. Rep, doi:10.1007/s13679-021-00448-8
Strategy, Supplementary Table 1. Search Strategy Used in Each Database Searched
Sultan, Nazareno, Gregor, Association between proton pump inhibitors and respiratory infections: A systematic review and meta-analysis of clinical trials, Can. J. Gastroenterol, doi:10.1155/2008/821385
Thornton, Lee, Publication bias in meta-analysis: Its causes and consequences, J. Clin. Epidemiol, doi:10.1016/S0895-4356(99)00161-4
Trifan, Stanciu, Girleanu, Stoica, Singeap et al., Proton pump inhibitors therapy and risk of Clostridium difficile infection: Systematic review and meta-analysis, World J. Gastroenterol, doi:10.3748/wjg.v23.i35.6500
Usman, Siddiqi, Khan, Ahmed, Ali et al., A Meta-analysis of the Relationship Between Renin-Angiotensin-Aldosterone System Inhibitors and COVID-19, Am. J. Cardiol, doi:10.1016/j.amjcard.2020.05.038
Vila-Corcoles, Satue-Gracia, Ochoa-Gondar, Torrente-Fraga, Gomez-Bertomeu et al., Use of distinct anti-hypertensive drugs and risk for COVID-19 among hypertensive people: A population-based cohort study in Southern Catalonia, Spain, J. Clin. Hypertens, doi:10.1111/jch.13948
Wang, Zhang, Du, Ma, Nan et al., Risk Factors for COVID-19 in Patients with Hypertension, Can. J. Infect. Dis. Med. Microbiol. J. Can. Mal. Infect. Microbiol. Med, doi:10.1155/2021/5515941
Xiang, Wong, So, Exploring Drugs and Vaccines Associated with Altered Risks and Severity of COVID-19: A UK Biobank Cohort Study of All ATC Level-4 Drug Categories Reveals Repositioning Opportunities, Pharmaceutics, doi:10.3390/pharmaceutics13091514
Zedtwitz-Liebenstein, Wenisch, Patruta, Parschalk, Daxböck et al., Omeprazole treatment diminishes intra-and extracellular neutrophil reactive oxygen production and bactericidal activity, Crit. Care Med, doi:10.1097/00003246-200205000-00026
Zhou, Wang, Lee, Wu, Cheung et al., Proton pump inhibitor or famotidine use and severe COVID-19 disease: A propensity score-matched territory-wide study, Gut, doi:10.1136/gutjnl-2020-323668
DOI record:
{
"DOI": "10.3390/tropicalmed7030037",
"ISSN": [
"2414-6366"
],
"URL": "http://dx.doi.org/10.3390/tropicalmed7030037",
"abstract": "<jats:p>COVID-19 has proved to be a serious, and consequential disease that has affected millions of people globally. Previously, the adverse effects of proton pump inhibitors (PPI) have been observed with increasing the risk of pneumonia and COVID-19. This meta-analysis aims to address the relationship between the use of PPI and the severity of COVID-19 infection. We conducted a systemic literature search from PUBMED, Science Direct, and Cinahl from December 2019 to January 2022. Published and unpublished randomized control trials and cohort studies were included. Review Manager was used for all statistical analyses. In total, 14 studies were included in this systemic review and meta-analysis. Outcomes of interest include: (1) susceptibility of COVID-19 infection and (2) severity of COVID-19 (defined as the composite of poor outcomes: ICU admission, need for oxygen therapy, need for a ventilator, or death), and (3) mortality due to COVID-19. PPI use was marginally associated with a nominal but statistically significant increase in the risk of COVID-19 infection (OR 1.05 [1.01, 1.09]; I2 97%, p = 0.007). PPI use also increased the risk of the composite poor outcome (OR 1.84 [1.71, 1.99]; I2 98%, p < 0.00001) and mortality (OR 1.12 [1.00, 1.25]; I2 84%, p = 0.05) in patients with COVID-19.</jats:p>",
"alternative-id": [
"tropicalmed7030037"
],
"author": [
{
"affiliation": [],
"family": "Fatima",
"given": "Kaneez",
"sequence": "first"
},
{
"affiliation": [],
"family": "Almas",
"given": "Talal",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lakhani",
"given": "Shan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jahangir",
"given": "Arshia",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9858-6155",
"affiliation": [],
"authenticated-orcid": false,
"family": "Ahmed",
"given": "Abdullah",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Siddiqui",
"given": "Ayra",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-7663-1170",
"affiliation": [],
"authenticated-orcid": false,
"family": "Rahim",
"given": "Aiman",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Qureshi",
"given": "Saleha Ahmed",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Arshad",
"given": "Zukhruf",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Golani",
"given": "Shilpa",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-2639-9366",
"affiliation": [],
"authenticated-orcid": false,
"family": "Musheer",
"given": "Adeena",
"sequence": "additional"
}
],
"container-title": "Tropical Medicine and Infectious Disease",
"container-title-short": "TropicalMed",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
3,
1
]
],
"date-time": "2022-03-01T01:11:57Z",
"timestamp": 1646097117000
},
"deposited": {
"date-parts": [
[
2022,
3,
9
]
],
"date-time": "2022-03-09T07:50:03Z",
"timestamp": 1646812203000
},
"indexed": {
"date-parts": [
[
2024,
7,
19
]
],
"date-time": "2024-07-19T01:38:03Z",
"timestamp": 1721353083860
},
"is-referenced-by-count": 15,
"issue": "3",
"issued": {
"date-parts": [
[
2022,
2,
28
]
]
},
"journal-issue": {
"issue": "3",
"published-online": {
"date-parts": [
[
2022,
3
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
2,
28
]
],
"date-time": "2022-02-28T00:00:00Z",
"timestamp": 1646006400000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2414-6366/7/3/37/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "37",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2022,
2,
28
]
]
},
"published-online": {
"date-parts": [
[
2022,
2,
28
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"key": "ref1",
"unstructured": "COVID Live-Coronavirus Statistics-Worldometerhttps://www.worldometers.info/coronavirus/"
},
{
"DOI": "10.1016/j.pupt.2021.101989",
"doi-asserted-by": "publisher",
"key": "ref2"
},
{
"DOI": "10.1016/j.amjcard.2020.05.038",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.1016/j.jaci.2021.06.006",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.1136/bmj.m1198",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.1007/s13679-021-00448-8",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.1155/2021/5515941",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.20452/pamw.2790",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"DOI": "10.1007/s40261-020-00963-x",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"DOI": "10.1097/MNH.0000000000000406",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.1111/bcpt.13023",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.1016/S0168-8278(99)80114-7",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.3109/00365521.2015.1054426",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"DOI": "10.1136/bmjopen-2017-017739",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.1016/j.cgh.2021.05.011",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.14309/ajg.0000000000000798",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.3390/pharmaceutics13091514",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.1097/MEG.0000000000002013",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.1053/j.gastro.2020.09.028",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"article-title": "The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration",
"author": "Liberati",
"first-page": "e1",
"journal-title": "PLoS Med.",
"key": "ref20",
"volume": "62",
"year": "2009"
},
{
"key": "ref21",
"unstructured": "Supplementary Table 1. Search Strategy Used in Each Database Searchedhttps://www.ijhpm.com/jufile?ar_sfile=44803"
},
{
"DOI": "10.1053/j.gastro.2020.11.007",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"DOI": "10.1136/gutjnl-2020-322248",
"doi-asserted-by": "publisher",
"key": "ref23"
},
{
"DOI": "10.14309/ajg.0000000000001311",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.1136/gutjnl-2020-323672",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"DOI": "10.1136/gutjnl-2020-323668",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.1186/s12916-021-01907-8",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.20944/preprints202005.0016.v1",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.1101/2020.05.04.20089904",
"doi-asserted-by": "publisher",
"key": "ref29"
},
{
"DOI": "10.1111/jch.13948",
"doi-asserted-by": "publisher",
"key": "ref30"
},
{
"DOI": "10.1136/bmj.327.7414.557",
"doi-asserted-by": "publisher",
"key": "ref31"
},
{
"key": "ref32",
"series-title": "Cochrane Handbook for Systematic Reviews of Interventions",
"year": "2021"
},
{
"DOI": "10.1016/S0895-4356(99)00161-4",
"doi-asserted-by": "publisher",
"key": "ref33"
},
{
"DOI": "10.1007/s43440-021-00263-x",
"doi-asserted-by": "publisher",
"key": "ref34"
},
{
"DOI": "10.1016/j.dld.2020.10.001",
"doi-asserted-by": "publisher",
"key": "ref35"
},
{
"DOI": "10.1186/s13054-021-03497-6",
"doi-asserted-by": "publisher",
"key": "ref36"
},
{
"DOI": "10.3748/wjg.v23.i35.6500",
"doi-asserted-by": "publisher",
"key": "ref37"
},
{
"DOI": "10.1124/pr.118.017129",
"doi-asserted-by": "publisher",
"key": "ref38"
},
{
"DOI": "10.1016/j.cell.2020.02.052",
"doi-asserted-by": "publisher",
"key": "ref39"
},
{
"DOI": "10.1155/2008/821385",
"doi-asserted-by": "publisher",
"key": "ref40"
},
{
"DOI": "10.1186/1741-7015-10-57",
"doi-asserted-by": "publisher",
"key": "ref41"
},
{
"article-title": "Proton pump inhibitors and infection risk",
"author": "Palencia-Herrejón",
"first-page": "4",
"journal-title": "Rev. Esp. Quimioter. Publ. Of. Soc. Esp. Quimioter.",
"key": "ref42",
"volume": "24",
"year": "2011"
},
{
"DOI": "10.1001/jama.292.16.1955",
"doi-asserted-by": "publisher",
"key": "ref43"
},
{
"DOI": "10.1186/s12967-015-0614-x",
"doi-asserted-by": "publisher",
"key": "ref44"
},
{
"DOI": "10.1097/00003246-200205000-00026",
"doi-asserted-by": "publisher",
"key": "ref45"
},
{
"DOI": "10.3389/fimmu.2021.736036",
"doi-asserted-by": "publisher",
"key": "ref46"
},
{
"DOI": "10.1136/gutjnl-2015-310376",
"doi-asserted-by": "publisher",
"key": "ref47"
},
{
"DOI": "10.1002/eji.201948322",
"doi-asserted-by": "publisher",
"key": "ref48"
}
],
"reference-count": 48,
"references-count": 48,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2414-6366/7/3/37"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "The Use of Proton Pump Inhibitors and COVID-19: A Systematic Review and Meta-Analysis",
"type": "journal-article",
"volume": "7"
}