Proton pump inhibitor on susceptibility to COVID-19 and its severity: a systematic review and meta-analysis
et al., Pharmacological Reports, doi:10.1007/s43440-021-00263-x, PROSPERO CRD42020224286, Apr 2021
PPIs for COVID-19
1st treatment shown to increase risk in
September 2020, now with p = 0.000000048 from 40 studies.
6,400+ studies for
210+ treatments. c19early.org
|
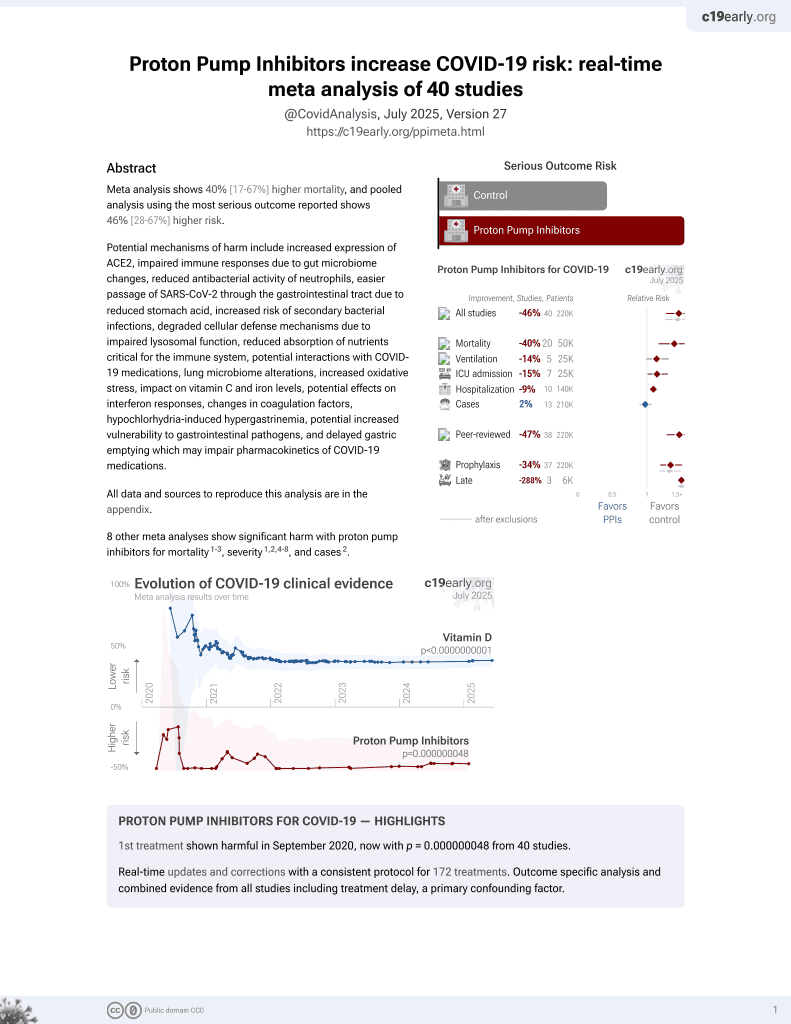
Meta-analysis of 12 studies with 290,455 patients showing increased risk of poor outcomes with proton pump inhibitor (PPI) use in COVID-19 patients, but not increased susceptibility.
8 meta-analyses show significant harm with proton pump inhibitors for mortality1-3,
severity1,2,4-8 , and
cases2.
Currently there are 40 proton pump inhibitors for COVID-19 studies, showing 40% higher mortality [17‑67%], 14% higher ventilation [-1‑32%], 15% higher ICU admission [1‑30%], 9% higher hospitalization [3‑16%], and 2% fewer cases [-6‑10%].
|
risk of severe case, 85.0% higher, OR 1.85, p = 0.01, RR approximated with OR.
|
|
risk of case, 56.0% higher, OR 1.56, p = 0.47, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Hariyanto et al., Proton pump inhibitor use is associated with increased risk of severity and mortality from coronavirus disease 2019 (COVID-19) infection, Digestive and Liver Disease, doi:10.1016/j.dld.2020.10.001.
2.
Fatima et al., The Use of Proton Pump Inhibitors and COVID-19: A Systematic Review and Meta-Analysis, Tropical Medicine and Infectious Disease, doi:10.3390/tropicalmed7030037.
3.
Toubasi et al., Proton Pump Inhibitors: Current Use and the Risk of Coronavirus Infectious Disease 2019 Development and its Related Mortality. Meta-analysis, Archives of Medical Research, doi:10.1016/j.arcmed.2021.03.004.
4.
Wardhana et al., Different Outcome in COVID-19 Patients with or without PPI Use: A Systematic Review and Meta-analysis, International Journal of Biomedical Science and Travel Medicine, doi:10.22225/ijbstm.1.1.2024.19-23.
5.
Yan et al., Does Proton Pump Inhibitor Use Lead to a Higher Risk of Coronavirus Disease 2019 Infection and Progression to Severe Disease? a Meta-analysis, Japanese Journal of Infectious Diseases, doi:10.7883/yoken.JJID.2021.074.
6.
Li et al., Do proton pump inhibitors influence SARS-CoV-2 related outcomes? A meta-analysis, Gut, doi:10.1136/gutjnl-2020-323366.
Pranata et al., 11 Apr 2021, peer-reviewed, 8 authors, trial PROSPERO CRD42020224286.
Contact: sherlylawrensia@gmail.com, joshuahenrina@gmail.com, antonia.lukito@uph.edu, lukito_ant@yahoo.com, lukito@uph.edu, raymond_pranata@hotmail.com, ianhuang2108@gmail.com, lim.michael.a@gmail.com, tutykuswardhani@unud.ac.id, tutykuswardhani@yahoo.com, dnwib.dps@centrin.net.id.
Proton pump inhibitor on susceptibility to COVID-19 and its severity: a systematic review and meta-analysis
Pharmacological Reports, doi:10.1007/s43440-021-00263-x
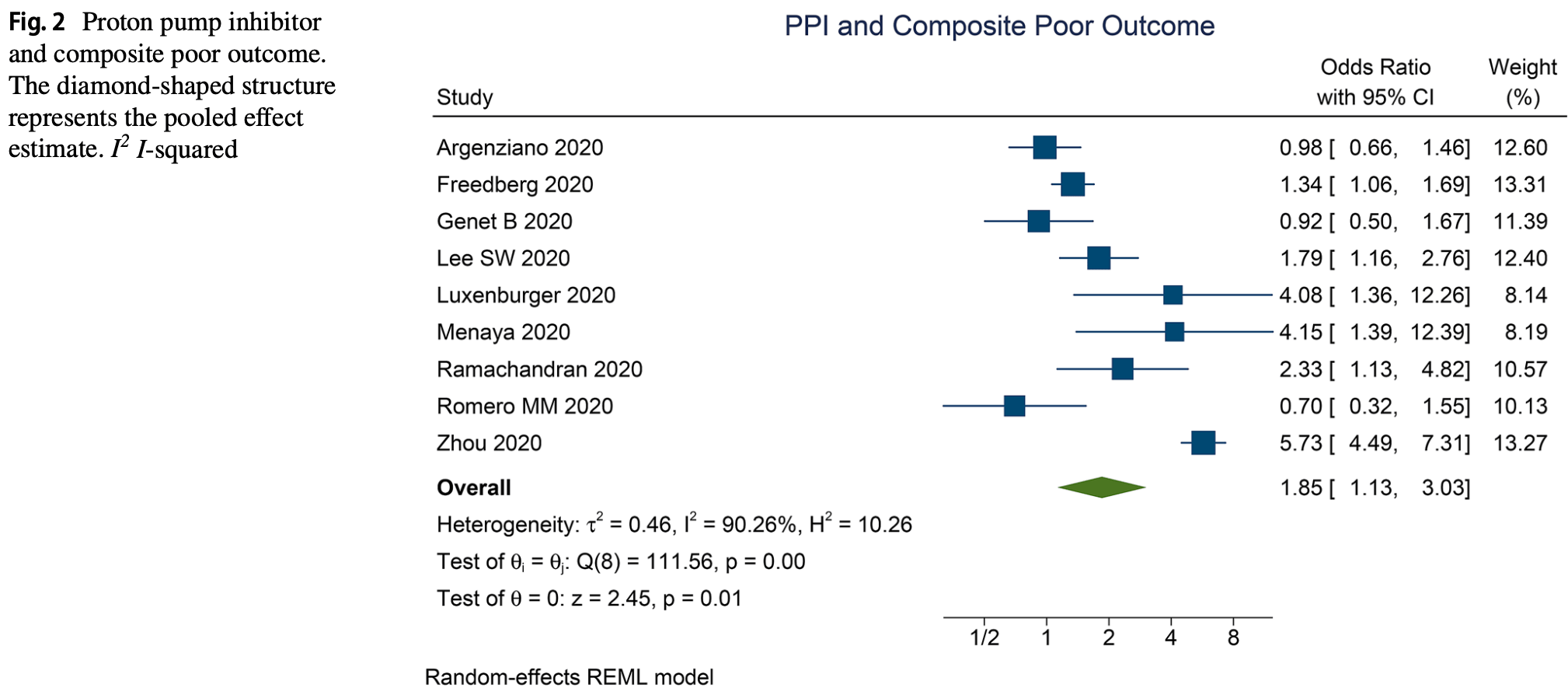
Background The negative impacts of proton pump inhibitor (PPI), including the risk of pneumonia and mortality, have been reported previously. This meta-analysis aimed to address the current interest of whether the administration of PPI could increase the susceptibility and risk of poor outcome in COVID-19. Methods We performed a systematic literature search from PubMed, Embase, EBSCOhost, and EuropePMC databases up until 3 December 2020. The main outcome was composite poor outcome which comprised of mortality and severe COVID-19. Severe COVID-19 in this study was defined as patients with COVID-19 that fulfill the criteria for severe CAP, including the need for intensive unit care or mechanical ventilation. The secondary outcome was susceptibility, based on cohort comparing COVID-19 positive and COVID-19 negative participants. Results There were a total of 290,455 patients from 12 studies in this meta-analysis. PPI use was associated with increased composite poor outcome (OR 1.85 [1.13, 3 .03], p = 0.014; I 2 90.26%). Meta-regression analysis indicate that the association does not vary by age (OR 0.97 [0.92, 1.02], p = 0.244), male (OR 1.05 [0.99, 1.11], p = 0.091), hypertension (OR 9.98 [0.95, 1.02], p = 0.317), diabetes (OR 0.99 [0.93, 1.05], p = 0.699), chronic kidney disease (OR 1.01 [0.93, 1.10], p = 0.756), nonsteroidal anti-inflammatory drug use (OR 1.02 [0.96, 1.09], p = 0.499), and pre-admission/in-hospital PPI use (OR 0.77 [0.26, 2.31], p = 0.644). PPI use was not associated with the susceptibility to COVID-19 (OR 1.56 [0.48, 5 .05], p = 0.46; I 2 99.7%). Conclusion This meta-analysis showed a potential association between PPI use and composite poor outcome, but not susceptibility.
Declarations Conflict of interest The authors declare that they have no conflict of interest. Publisher's Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Almario, Chey, Spiegel, Increased risk of COVID-19 among users of proton pump inhibitors, Am J Gastroenterol, doi:10.14309/ajg.0000000000000798
Andhika, Huang, Wijaya, Severity of COVID-19 in endstage kidney disease patients on chronic dialysis, Ther Apher Dial, doi:10.1111/1744-9987.13597
Argenzian, Bruc, Slate, Tia, Baldwi et al., Characterization and clinical course of 1000 patients with coronavirus disease 2019 in New York: retrospective case series, BMJ, doi:10.1136/bmj.m1996
Bateman, Bykov, Choudhry, Schneeweiss, Gagne et al., Type of stress ulcer prophylaxis and risk of nosocomial pneumonia in cardiac surgical patients: Cohort study, BMJ, doi:10.1136/bmj.f5416
Bavishi, Dupont, Systematic review: the use of proton pump inhibitors and increased susceptibility to enteric infection, Aliment Pharmacol Ther, doi:10.1111/j.1365-2036.2011.04874.x
Bialek, Bowen, Chow, Curns, Gierke et al., Geographic differences in COVID-19 cases, deaths, and incidence-United States, February 12-April 7, 2020, MMWR Morb Mortal Wkly Rep, doi:10.15585/mmwr.mm6915e4
Bramer, Rethlefsen, Kleijnen, Franco, Optimal database combinations for literature searches in systematic reviews: a prospective exploratory study, Syst Rev, doi:10.1186/s13643-017-0644-y
Charpiat, Bleyzac, Tod, Proton pump inhibitors are risk factors for viral infections: even for COVID-19?, Clin Drug Investig, doi:10.1007/s40261-020-00963-x
Corsonello, Lattanzio, Bustacchini, Garasto, Cozza et al., Adverse events of proton pump inhibitors: potential mechanisms, Curr Drug Metab, doi:10.2174/1389200219666171207125351
Darnell, Subbarao, Feinstone, Taylor, Inactivation of the coronavirus that induces severe acute respiratory syndrome, SARS-CoV J Virol Methods, doi:10.1016/j.jviromet.2004.06.006
Eom, Jeon, Lim, Cho, Park et al., Use of acid-suppressive drugs and risk of pneumonia: a systematic review and meta-analysis, CMAJ, doi:10.1503/cmaj.092129
Genet, Vidal, Cohen, Boully, Beunardeau et al., COVID-19 in-hospital mortality and use of reninangiotensin system blockers in geriatrics patients, J Am Med Dir Assoc, doi:10.1016/j.jamda.2020.09.004
Gusenbauer, Haddaway, Which academic search systems are suitable for systematic reviews or meta-analyses? Evaluating retrieval qualities of Google Scholar, PubMed, and 26 other resources, Res Synth Methods, doi:10.1002/jrsm.1378
Hamming, Timens, Bulthuis, Lely, Navis et al., Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis, J Pathol, doi:10.1002/path.1570
Hao, Sotudian, Wang, Xu, Hu et al., Early prediction of level-of-care requirements in patients with COVID-19, Elife, doi:10.7554/eLife.60519
Lamers, Beumer, Van Der Vaart, Knoops, Puschhof et al., SARS-CoV-2 productively infects human gut enterocytes, Science, doi:10.1126/science.abc1669
Lee, Ha, Yeniova, Moon, Kim et al., Severe clinical outcomes of COVID-19 associated with proton pump inhibitors: a nationwide cohort study with propensity score matching, Gut, doi:10.1136/gutjnl-2020-322248
Leonard, Marshall, Moayyedi, Systematic review of the risk of enteric infection in patients taking acid suppression, Am J Gastroenterol, doi:10.1111/j.1572-0241.2007.01275.x
Lim, Pranata, Huang, Yonas, Soeroto et al., Multiorgan failure with emphasis on acute kidney injury and severity of COVID-19: systematic review and meta-analysis, Can J Kidney Heal Dis, doi:10.1177/2054358120938573
Lo, Chan, Proton pump inhibitor use and the risk of small intestinal bacterial overgrowth: a meta-analysis, Clin Gastroenterol Hepatol, doi:10.1016/j.cgh.2012.12.011
Lukito, Pranata, Henrina, Lim, Lawrensia et al., The Effect of metformin consumption on mortality in hospitalized COVID-19 patients: a systematic review and meta-analysis, Diabetes Metab Syndr Clin Res Rev, doi:10.1016/j.dsx.2020.11.006
Luxenburger, Sturm, Biever, Rieg, Duerschmied et al., Treatment with proton pump inhibitors increases the risk of secondary infections and ARDS in hospitalized patients with COVID-19: coincidence or underestimated risk factor?, J Intern Med, doi:10.1111/joim.13121
Metlay, Waterer, Long, Anzueto, Brozek et al., Diagnosis and treatment of adults with communityacquired pneumonia, Am J Respir Crit Care Med, doi:10.1164/rccm.201908-1581ST
Namazi, Jowkar, A succinct review of the general and immunological pharmacologic effects of proton pump inhibitors, J Clin Pharm Ther, doi:10.1111/j.1365-2710.2008.00907.x
Pranata, Lim, Yonas, Vania, Lukito et al., Body mass index and outcome in patients with COVID-19: a dose-response meta-analysis, Diabetes Metab, doi:10.1016/j.diabet.2020.07.005
Pranata, Permana, Huang, Lim, Soetedjo et al., The use of renin angiotensin system inhibitor on mortality in patients with coronavirus disease 2019 (COVID-19): a systematic review and meta-analysis, Diabetes Metab Syndr Clin Res Rev, doi:10.1016/j.dsx.2020.06.047
Pranata, Supriyadi, Huang, Permana, Lim et al., The association between chronic kidney disease and new onset renal replacement therapy on the outcome of COVID-19 patients: a meta-analysis, Clin Med Insights Circ Respir Pulm Med, doi:10.1177/1179548420959165
Qiu, Zhou, Zhang, Acid-suppressive drugs and risk of kidney disease: a systematic review and meta-analysis, J Gastroenterol Hepatol, doi:10.1111/jgh.14157
Ramachandran, Perisetti, Gajendran, Louis, Bansal et al., Pre-hospitalization proton pump inhibitor use and clinical outcomes in COVID-19, Eur J Gastroenterol Hepatol, doi:10.1097/meg.0000000000002013
Romero, Céspedes, Sahuquillo, Zamora, Ballesteros et al., COVID-19 outbreak in long-term care facilities from Spain. Many lessons to learn, PLoS ONE, doi:10.1371/journal.pone.0241030
Shea, Reeves, Wells, Thuku, Hamel et al., AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both, BMJ, doi:10.1136/bmj.j4008
Tarlow, Gubatan, Khan, Cholankeril, Are proton pump inhibitors contributing to SARS-COV-2 infection?, Am J Gastroenterol, doi:10.14309/ajg.0000000000000933
Vila-Corcoles, Satue-Gracia, Ochoa-Gondar, Torrente-Fraga, Gomez-Bertomeu et al., Use of distinct anti-hypertensive drugs and risk for COVID-19 among hypertensive people: a population-based cohort study in Southern Catalonia, Spain J Clin Hypertens, doi:10.1111/jch.13948
Vinet, Zhedanov, A "missing" family of classical orthogonal polynomials, J Phys A Math Theor, doi:10.1088/1751-8113/44/8/085201
Xiao, Tang, Zheng, Liu, Li et al., Evidence for gastrointestinal infection of SARS-CoV-2, Gastroenterology, doi:10.1053/j.gastro.2020.02.055
Xie, Bowe, Li, Xian, Balasubramanian et al., Proton pump inhibitors and risk of incident CKD and progression to ESRD, J Am Soc Nephrol, doi:10.1681/ASN.2015121377
Xie, Bowe, Li, Xian, Yan et al., Long-term kidney outcomes among users of proton pump inhibitors without intervening acute kidney injury, Kidney Int, doi:10.1016/j.kint.2016.12.021
Xie, Bowe, Yan, Xian, Li et al., Estimates of all cause mortality and cause specific mortality associated with proton pump inhibitors among US veterans: Cohort study, BMJ, doi:10.1136/bmj.l1580
Yonas, Alwi, Pranata, Huang, Lim et al., Effect of heart failure on the outcome of COVID-19-a meta analysis and systematic review, Am J Emerg Med, doi:10.1016/j.ajem.2020.07.009
Zhou, Wang, Lee, Wu, Cheung et al., Proton pump inhibitor or famotidine use and severe COVID-19 disease: a propensity score-matched territory-wide study, Gut, doi:10.1136/gutjnl-2020-323668
DOI record:
{
"DOI": "10.1007/s43440-021-00263-x",
"ISSN": [
"1734-1140",
"2299-5684"
],
"URL": "http://dx.doi.org/10.1007/s43440-021-00263-x",
"alternative-id": [
"263"
],
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "25 January 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Revised",
"name": "revised",
"order": 2,
"value": "10 March 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 3,
"value": "2 April 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 4,
"value": "11 April 2021"
},
{
"group": {
"label": "Declarations",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1
},
{
"group": {
"label": "Conflict of interest",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "The authors declare that they have no conflict of interest."
},
{
"label": "Free to read",
"name": "free",
"value": "This content has been made available to all."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-3998-6551",
"affiliation": [],
"authenticated-orcid": false,
"family": "Pranata",
"given": "Raymond",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0003-1189-8453",
"affiliation": [],
"authenticated-orcid": false,
"family": "Huang",
"given": "Ian",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lawrensia",
"given": "Sherly",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3763-2661",
"affiliation": [],
"authenticated-orcid": false,
"family": "Henrina",
"given": "Joshua",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7631-6835",
"affiliation": [],
"authenticated-orcid": false,
"family": "Lim",
"given": "Michael Anthonius",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lukito",
"given": "Antonia Anna",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kuswardhani",
"given": "Raden Ayu Tuty",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wibawa",
"given": "I. Dewa Nyoman",
"sequence": "additional"
}
],
"container-title": "Pharmacological Reports",
"container-title-short": "Pharmacol. Rep",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2021,
4,
11
]
],
"date-time": "2021-04-11T04:02:25Z",
"timestamp": 1618113745000
},
"deposited": {
"date-parts": [
[
2021,
11,
18
]
],
"date-time": "2021-11-18T05:12:15Z",
"timestamp": 1637212335000
},
"indexed": {
"date-parts": [
[
2024,
7,
19
]
],
"date-time": "2024-07-19T01:30:31Z",
"timestamp": 1721352631957
},
"is-referenced-by-count": 17,
"issue": "6",
"issued": {
"date-parts": [
[
2021,
4,
11
]
]
},
"journal-issue": {
"issue": "6",
"published-print": {
"date-parts": [
[
2021,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.springer.com/tdm",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
4,
11
]
],
"date-time": "2021-04-11T00:00:00Z",
"timestamp": 1618099200000
}
},
{
"URL": "https://www.springer.com/tdm",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
4,
11
]
],
"date-time": "2021-04-11T00:00:00Z",
"timestamp": 1618099200000
}
}
],
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1007/s43440-021-00263-x.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/article/10.1007/s43440-021-00263-x/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/content/pdf/10.1007/s43440-021-00263-x.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"page": "1642-1649",
"prefix": "10.1007",
"published": {
"date-parts": [
[
2021,
4,
11
]
]
},
"published-online": {
"date-parts": [
[
2021,
4,
11
]
]
},
"published-print": {
"date-parts": [
[
2021,
12
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1016/j.diabet.2020.07.005",
"author": "R Pranata",
"doi-asserted-by": "publisher",
"journal-title": "Diabetes Metab",
"key": "263_CR1",
"unstructured": "Pranata R, Lim MA, Yonas E, Vania R, Lukito AA, Siswanto BB, et al. Body mass index and outcome in patients with COVID-19: a dose–response meta-analysis. Diabetes Metab. 2020. https://doi.org/10.1016/j.diabet.2020.07.005.",
"year": "2020"
},
{
"DOI": "10.1016/j.ajem.2020.07.009",
"author": "E Yonas",
"doi-asserted-by": "publisher",
"journal-title": "Am J Emerg Med",
"key": "263_CR2",
"unstructured": "Yonas E, Alwi I, Pranata R, Huang I, Lim MA, Gutierrez EJ, et al. Effect of heart failure on the outcome of COVID-19—a meta analysis and systematic review. Am J Emerg Med. 2020. https://doi.org/10.1016/j.ajem.2020.07.009.",
"year": "2020"
},
{
"DOI": "10.1136/gutjnl-2020-322248",
"author": "SW Lee",
"doi-asserted-by": "publisher",
"first-page": "76",
"journal-title": "Gut",
"key": "263_CR3",
"unstructured": "Lee SW, Ha EK, Yeniova AÖ, Moon SY, Kim SY, Koh HY, et al. Severe clinical outcomes of COVID-19 associated with proton pump inhibitors: a nationwide cohort study with propensity score matching. Gut. 2021;70:76–84. https://doi.org/10.1136/gutjnl-2020-322248.",
"volume": "70",
"year": "2021"
},
{
"DOI": "10.1007/s40261-020-00963-x",
"author": "B Charpiat",
"doi-asserted-by": "publisher",
"first-page": "897",
"journal-title": "Clin Drug Investig",
"key": "263_CR4",
"unstructured": "Charpiat B, Bleyzac N, Tod M. Proton pump inhibitors are risk factors for viral infections: even for COVID-19? Clin Drug Investig. 2020;40:897–9. https://doi.org/10.1007/s40261-020-00963-x.",
"volume": "40",
"year": "2020"
},
{
"DOI": "10.1136/bmj.l1580",
"author": "Y Xie",
"doi-asserted-by": "publisher",
"first-page": "l1580",
"journal-title": "BMJ",
"key": "263_CR5",
"unstructured": "Xie Y, Bowe B, Yan Y, Xian H, Li T, Al-Aly Z. Estimates of all cause mortality and cause specific mortality associated with proton pump inhibitors among US veterans: Cohort study. BMJ. 2019;365:l1580. https://doi.org/10.1136/bmj.l1580.",
"volume": "365",
"year": "2019"
},
{
"DOI": "10.1136/bmj.f5416",
"author": "BT Bateman",
"doi-asserted-by": "publisher",
"first-page": "f5416",
"journal-title": "BMJ",
"key": "263_CR6",
"unstructured": "Bateman BT, Bykov K, Choudhry NK, Schneeweiss S, Gagne JJ, Polinski JM, et al. Type of stress ulcer prophylaxis and risk of nosocomial pneumonia in cardiac surgical patients: Cohort study. BMJ. 2013;347:f5416–f5416. https://doi.org/10.1136/bmj.f5416.",
"volume": "347",
"year": "2013"
},
{
"DOI": "10.1503/cmaj.092129",
"author": "CS Eom",
"doi-asserted-by": "publisher",
"first-page": "310",
"journal-title": "CMAJ",
"key": "263_CR7",
"unstructured": "Eom CS, Jeon CY, Lim JW, Cho EG, Park SM, Lee KS. Use of acid-suppressive drugs and risk of pneumonia: a systematic review and meta-analysis. CMAJ. 2011;183:310–9. https://doi.org/10.1503/cmaj.092129.",
"volume": "183",
"year": "2011"
},
{
"DOI": "10.1016/j.cgh.2012.12.011",
"author": "WK Lo",
"doi-asserted-by": "publisher",
"first-page": "483",
"journal-title": "Clin Gastroenterol Hepatol",
"key": "263_CR8",
"unstructured": "Lo WK, Chan WW. Proton pump inhibitor use and the risk of small intestinal bacterial overgrowth: a meta-analysis. Clin Gastroenterol Hepatol. 2013;11:483–90. https://doi.org/10.1016/j.cgh.2012.12.011.",
"volume": "11",
"year": "2013"
},
{
"DOI": "10.1111/j.1572-0241.2007.01275.x",
"author": "J Leonard",
"doi-asserted-by": "publisher",
"first-page": "2047",
"journal-title": "Am J Gastroenterol",
"key": "263_CR9",
"unstructured": "Leonard J, Marshall JK, Moayyedi P. Systematic review of the risk of enteric infection in patients taking acid suppression. Am J Gastroenterol. 2007;102:2047–56. https://doi.org/10.1111/j.1572-0241.2007.01275.x.",
"volume": "102",
"year": "2007"
},
{
"DOI": "10.1111/j.1365-2036.2011.04874.x",
"author": "C Bavishi",
"doi-asserted-by": "publisher",
"first-page": "1269",
"journal-title": "Aliment Pharmacol Ther",
"key": "263_CR10",
"unstructured": "Bavishi C, DuPont HL. Systematic review: the use of proton pump inhibitors and increased susceptibility to enteric infection. Aliment Pharmacol Ther. 2011;34:1269–81. https://doi.org/10.1111/j.1365-2036.2011.04874.x.",
"volume": "34",
"year": "2011"
},
{
"DOI": "10.14309/ajg.0000000000000798",
"author": "CV Almario",
"doi-asserted-by": "publisher",
"first-page": "1707",
"journal-title": "Am J Gastroenterol",
"key": "263_CR11",
"unstructured": "Almario CV, Chey WD, Spiegel BMR. Increased risk of COVID-19 among users of proton pump inhibitors. Am J Gastroenterol. 2020;115:1707–15. https://doi.org/10.14309/ajg.0000000000000798.",
"volume": "115",
"year": "2020"
},
{
"DOI": "10.1164/rccm.201908-1581ST",
"author": "JP Metlay",
"doi-asserted-by": "publisher",
"first-page": "E45",
"journal-title": "Am J Respir Crit Care Med",
"key": "263_CR12",
"unstructured": "Metlay JP, Waterer GW, Long AC, Anzueto A, Brozek J, Crothers K, et al. Diagnosis and treatment of adults with community-acquired pneumonia. Am J Respir Crit Care Med. 2019;200:E45-67. https://doi.org/10.1164/rccm.201908-1581ST.",
"volume": "200",
"year": "2019"
},
{
"DOI": "10.1097/meg.0000000000002013",
"author": "P Ramachandran",
"doi-asserted-by": "publisher",
"journal-title": "Eur J Gastroenterol Hepatol",
"key": "263_CR13",
"unstructured": "Ramachandran P, Perisetti A, Gajendran M, Jean-Louis F, Bansal P, Dwivedi AK, et al. Pre-hospitalization proton pump inhibitor use and clinical outcomes in COVID-19. Eur J Gastroenterol Hepatol. 2020. https://doi.org/10.1097/meg.0000000000002013 (Publish Ah:2020.07.12.20151084).",
"year": "2020"
},
{
"DOI": "10.1088/1751-8113/44/8/085201",
"author": "L Vinet",
"doi-asserted-by": "publisher",
"first-page": "e3",
"issue": "1129–1131",
"journal-title": "J Phys A Math Theor",
"key": "263_CR14",
"unstructured": "Vinet L, Zhedanov A. A “missing” family of classical orthogonal polynomials. J Phys A Math Theor. 2011;44(1129–1131):e3. https://doi.org/10.1088/1751-8113/44/8/085201.",
"volume": "44",
"year": "2011"
},
{
"DOI": "10.1136/gutjnl-2020-323668",
"author": "J Zhou",
"doi-asserted-by": "publisher",
"journal-title": "Gut",
"key": "263_CR15",
"unstructured": "Zhou J, Wang X, Lee S, Wu WKK, Cheung BMY, Zhang Q, et al. Proton pump inhibitor or famotidine use and severe COVID-19 disease: a propensity score-matched territory-wide study. Gut. 2020. https://doi.org/10.1136/gutjnl-2020-323668.",
"year": "2020"
},
{
"DOI": "10.1016/j.jamda.2020.09.004",
"author": "B Genet",
"doi-asserted-by": "publisher",
"first-page": "1539",
"journal-title": "J Am Med Dir Assoc",
"key": "263_CR16",
"unstructured": "Genet B, Vidal JS, Cohen A, Boully C, Beunardeau M, Marine Harlé L, et al. COVID-19 in-hospital mortality and use of renin-angiotensin system blockers in geriatrics patients. J Am Med Dir Assoc. 2020;21:1539–45. https://doi.org/10.1016/j.jamda.2020.09.004.",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.7554/eLife.60519",
"author": "B Hao",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Elife",
"key": "263_CR17",
"unstructured": "Hao B, Sotudian S, Wang T, Xu T, Hu Y, Gaitanidis A, et al. Early prediction of level-of-care requirements in patients with COVID-19. Elife. 2020;9:1–23. https://doi.org/10.7554/eLife.60519.",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1111/joim.13121",
"author": "H Luxenburger",
"doi-asserted-by": "publisher",
"first-page": "121",
"journal-title": "J Intern Med",
"key": "263_CR18",
"unstructured": "Luxenburger H, Sturm L, Biever P, Rieg S, Duerschmied D, Schultheiss M, et al. Treatment with proton pump inhibitors increases the risk of secondary infections and ARDS in hospitalized patients with COVID-19: coincidence or underestimated risk factor? J Intern Med. 2021;289:121–4. https://doi.org/10.1111/joim.13121.",
"volume": "289",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0241030",
"author": "M Mas Romero",
"doi-asserted-by": "publisher",
"first-page": "e0241030",
"journal-title": "PLoS ONE",
"key": "263_CR19",
"unstructured": "Mas Romero M, Avendaño Céspedes A, Tabernero Sahuquillo MT, Cortés Zamora EB, Gómez Ballesteros C, Sánchez-Flor Alfaro V, et al. COVID-19 outbreak in long-term care facilities from Spain. Many lessons to learn. PLoS ONE. 2020;15:e0241030. https://doi.org/10.1371/journal.pone.0241030.",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.15585/mmwr.mm6915e4",
"author": "S Bialek",
"doi-asserted-by": "publisher",
"first-page": "465",
"journal-title": "MMWR Morb Mortal Wkly Rep",
"key": "263_CR20",
"unstructured": "Bialek S, Bowen V, Chow N, Curns A, Gierke R, Hall A, et al. Geographic differences in COVID-19 cases, deaths, and incidence—United States, February 12–April 7, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:465–71. https://doi.org/10.15585/mmwr.mm6915e4.",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.14309/ajg.0000000000000933",
"author": "B Tarlow",
"doi-asserted-by": "publisher",
"first-page": "1920",
"journal-title": "Am J Gastroenterol",
"key": "263_CR21",
"unstructured": "Tarlow B, Gubatan J, Khan MA, Cholankeril G. Are proton pump inhibitors contributing to SARS-COV-2 infection? Am J Gastroenterol. 2020;115:1920–1. https://doi.org/10.14309/ajg.0000000000000933.",
"volume": "115",
"year": "2020"
},
{
"DOI": "10.1111/jch.13948",
"author": "A Vila-Corcoles",
"doi-asserted-by": "publisher",
"first-page": "1379",
"journal-title": "Spain J Clin Hypertens",
"key": "263_CR22",
"unstructured": "Vila-Corcoles A, Satue-Gracia E, Ochoa-Gondar O, Torrente-Fraga C, Gomez-Bertomeu F, Vila-Rovira A, et al. Use of distinct anti-hypertensive drugs and risk for COVID-19 among hypertensive people: a population-based cohort study in Southern Catalonia. Spain J Clin Hypertens. 2020;22:1379–88. https://doi.org/10.1111/jch.13948.",
"volume": "22",
"year": "2020"
},
{
"DOI": "10.1136/bmj.m1996",
"author": "MG Argenzian",
"doi-asserted-by": "publisher",
"journal-title": "BMJ",
"key": "263_CR23",
"unstructured": "Argenzian MG, Bruc SL, Slate CL, Tia JR, Baldwi MR, Barr RG, et al. Characterization and clinical course of 1000 patients with coronavirus disease 2019 in New York: retrospective case series. BMJ. 2020. https://doi.org/10.1136/bmj.m1996.",
"year": "2020"
},
{
"DOI": "10.1016/j.dsx.2020.06.047",
"author": "R Pranata",
"doi-asserted-by": "publisher",
"first-page": "983",
"journal-title": "Diabetes Metab Syndr Clin Res Rev",
"key": "263_CR24",
"unstructured": "Pranata R, Permana H, Huang I, Lim MA, Soetedjo NNM, Supriyadi R, et al. The use of renin angiotensin system inhibitor on mortality in patients with coronavirus disease 2019 (COVID-19): a systematic review and meta-analysis. Diabetes Metab Syndr Clin Res Rev. 2020;14:983–90. https://doi.org/10.1016/j.dsx.2020.06.047.",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1016/j.dsx.2020.11.006",
"author": "AA Lukito",
"doi-asserted-by": "publisher",
"first-page": "2177",
"journal-title": "Diabetes Metab Syndr Clin Res Rev",
"key": "263_CR25",
"unstructured": "Lukito AA, Pranata R, Henrina J, Lim MA, Lawrensia S, Suastika K. The Effect of metformin consumption on mortality in hospitalized COVID-19 patients: a systematic review and meta-analysis. Diabetes Metab Syndr Clin Res Rev. 2020;14:2177–83. https://doi.org/10.1016/j.dsx.2020.11.006.",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1136/bmj.j4008",
"author": "BJ Shea",
"doi-asserted-by": "publisher",
"journal-title": "BMJ",
"key": "263_CR26",
"unstructured": "Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017. https://doi.org/10.1136/bmj.j4008.",
"year": "2017"
},
{
"DOI": "10.1186/s13643-017-0644-y",
"author": "WM Bramer",
"doi-asserted-by": "publisher",
"journal-title": "Syst Rev",
"key": "263_CR27",
"unstructured": "Bramer WM, Rethlefsen ML, Kleijnen J, Franco OH. Optimal database combinations for literature searches in systematic reviews: a prospective exploratory study. Syst Rev. 2017. https://doi.org/10.1186/s13643-017-0644-y.",
"year": "2017"
},
{
"DOI": "10.1002/jrsm.1378",
"author": "M Gusenbauer",
"doi-asserted-by": "publisher",
"first-page": "181",
"journal-title": "Res Synth Methods",
"key": "263_CR28",
"unstructured": "Gusenbauer M, Haddaway NR. Which academic search systems are suitable for systematic reviews or meta-analyses? Evaluating retrieval qualities of Google Scholar, PubMed, and 26 other resources. Res Synth Methods. 2020;11:181–217. https://doi.org/10.1002/jrsm.1378.",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1016/j.jviromet.2004.06.006",
"author": "MER Darnell",
"doi-asserted-by": "publisher",
"first-page": "85",
"journal-title": "SARS-CoV J Virol Methods",
"key": "263_CR29",
"unstructured": "Darnell MER, Subbarao K, Feinstone SM, Taylor DR. Inactivation of the coronavirus that induces severe acute respiratory syndrome. SARS-CoV J Virol Methods. 2004;121:85–91. https://doi.org/10.1016/j.jviromet.2004.06.006.",
"volume": "121",
"year": "2004"
},
{
"DOI": "10.1002/path.1570",
"author": "I Hamming",
"doi-asserted-by": "publisher",
"first-page": "631",
"journal-title": "J Pathol",
"key": "263_CR30",
"unstructured": "Hamming I, Timens W, Bulthuis MLC, Lely AT, Navis GJ, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203:631–7. https://doi.org/10.1002/path.1570.",
"volume": "203",
"year": "2004"
},
{
"DOI": "10.1126/science.abc1669",
"author": "MM Lamers",
"doi-asserted-by": "publisher",
"first-page": "50",
"journal-title": "Science (80–)",
"key": "263_CR31",
"unstructured": "Lamers MM, Beumer J, Van Der Vaart J, Knoops K, Puschhof J, Breugem TI, et al. SARS-CoV-2 productively infects human gut enterocytes. Science (80–). 2020;369:50–4. https://doi.org/10.1126/science.abc1669.",
"volume": "369",
"year": "2020"
},
{
"DOI": "10.1053/j.gastro.2020.02.055",
"author": "F Xiao",
"doi-asserted-by": "publisher",
"first-page": "1831",
"journal-title": "Gastroenterology",
"key": "263_CR32",
"unstructured": "Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology. 2020;158:1831–3. https://doi.org/10.1053/j.gastro.2020.02.055 (e3).",
"volume": "158",
"year": "2020"
},
{
"DOI": "10.2174/1389200219666171207125351",
"author": "A Corsonello",
"doi-asserted-by": "publisher",
"first-page": "142",
"journal-title": "Curr Drug Metab",
"key": "263_CR33",
"unstructured": "Corsonello A, Lattanzio F, Bustacchini S, Garasto S, Cozza A, Schepisi R, et al. Adverse events of proton pump inhibitors: potential mechanisms. Curr Drug Metab. 2017;19:142–54. https://doi.org/10.2174/1389200219666171207125351.",
"volume": "19",
"year": "2017"
},
{
"DOI": "10.1111/j.1365-2710.2008.00907.x",
"author": "MR Namazi",
"doi-asserted-by": "publisher",
"first-page": "215",
"journal-title": "J Clin Pharm Ther",
"key": "263_CR34",
"unstructured": "Namazi MR, Jowkar F. A succinct review of the general and immunological pharmacologic effects of proton pump inhibitors. J Clin Pharm Ther. 2008;33:215–7. https://doi.org/10.1111/j.1365-2710.2008.00907.x.",
"volume": "33",
"year": "2008"
},
{
"DOI": "10.1111/jgh.14157",
"author": "T Qiu",
"doi-asserted-by": "publisher",
"first-page": "1566",
"journal-title": "J Gastroenterol Hepatol",
"key": "263_CR35",
"unstructured": "Qiu T, Zhou J, Zhang C. Acid-suppressive drugs and risk of kidney disease: a systematic review and meta-analysis. J Gastroenterol Hepatol. 2018;33:1566–73. https://doi.org/10.1111/jgh.14157.",
"volume": "33",
"year": "2018"
},
{
"DOI": "10.1681/ASN.2015121377",
"author": "Y Xie",
"doi-asserted-by": "publisher",
"first-page": "3153",
"journal-title": "J Am Soc Nephrol",
"key": "263_CR36",
"unstructured": "Xie Y, Bowe B, Li T, Xian H, Balasubramanian S, Al-Aly Z. Proton pump inhibitors and risk of incident CKD and progression to ESRD. J Am Soc Nephrol. 2016;27:3153–63. https://doi.org/10.1681/ASN.2015121377.",
"volume": "27",
"year": "2016"
},
{
"DOI": "10.1016/j.kint.2016.12.021",
"author": "Y Xie",
"doi-asserted-by": "publisher",
"first-page": "1482",
"journal-title": "Kidney Int",
"key": "263_CR37",
"unstructured": "Xie Y, Bowe B, Li T, Xian H, Yan Y, Al-Aly Z. Long-term kidney outcomes among users of proton pump inhibitors without intervening acute kidney injury. Kidney Int. 2017;91:1482–94. https://doi.org/10.1016/j.kint.2016.12.021.",
"volume": "91",
"year": "2017"
},
{
"DOI": "10.1177/1179548420959165",
"author": "R Pranata",
"doi-asserted-by": "publisher",
"first-page": "117954842095916",
"journal-title": "Clin Med Insights Circ Respir Pulm Med",
"key": "263_CR38",
"unstructured": "Pranata R, Supriyadi R, Huang I, Permana H, Lim MA, Yonas E, et al. The association between chronic kidney disease and new onset renal replacement therapy on the outcome of COVID-19 patients: a meta-analysis. Clin Med Insights Circ Respir Pulm Med. 2020;14:1179548420959165. https://doi.org/10.1177/1179548420959165.",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1177/2054358120938573",
"author": "MA Lim",
"doi-asserted-by": "publisher",
"first-page": "205435812093857",
"journal-title": "Can J Kidney Heal Dis",
"key": "263_CR39",
"unstructured": "Lim MA, Pranata R, Huang I, Yonas E, Soeroto AY, Supriyadi R. Multiorgan failure with emphasis on acute kidney injury and severity of COVID-19: systematic review and meta-analysis. Can J Kidney Heal Dis. 2020;7:205435812093857. https://doi.org/10.1177/2054358120938573.",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1111/1744-9987.13597",
"author": "R Andhika",
"doi-asserted-by": "publisher",
"journal-title": "Ther Apher Dial",
"key": "263_CR40",
"unstructured": "Andhika R, Huang I, Wijaya I. Severity of COVID-19 in end-stage kidney disease patients on chronic dialysis. Ther Apher Dial. 2020. https://doi.org/10.1111/1744-9987.13597.",
"year": "2020"
}
],
"reference-count": 40,
"references-count": 40,
"relation": {},
"resource": {
"primary": {
"URL": "https://link.springer.com/10.1007/s43440-021-00263-x"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Proton pump inhibitor on susceptibility to COVID-19 and its severity: a systematic review and meta-analysis",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "73"
}