Proton pump inhibitor or famotidine use and severe COVID-19 disease: a propensity score-matched territory-wide study
et al., Gut, doi:10.1136/gutjnl-2020-323668, Dec 2020
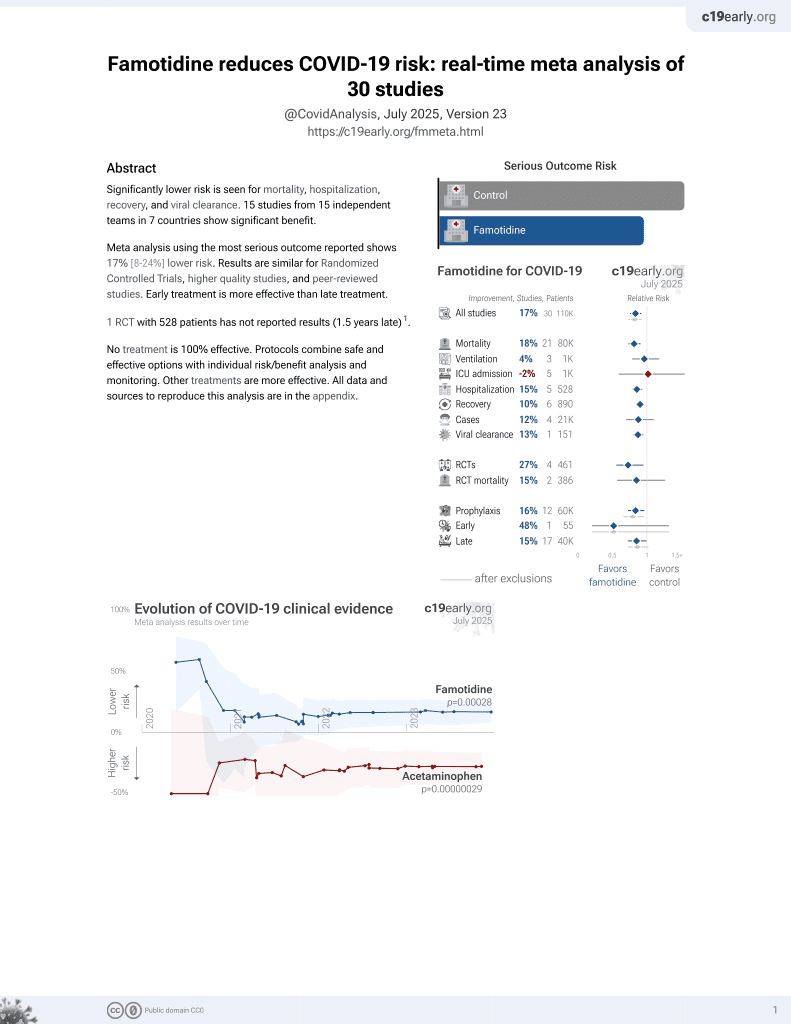
Famotidine for COVID-19
29th treatment shown to reduce risk in
October 2021, now with p = 0.00028 from 30 studies, recognized in 2 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 4,445 COVID+ patients in China, showing higher risk of combined death/intubation/ICU with famotidine and with PPIs.
Standard of Care (SOC) for COVID-19 in the study country,
China, is average with moderate efficacy for approved treatments1.
Study covers famotidine and proton pump inhibitors.
|
risk of severe case, 84.0% higher, HR 1.84, p < 0.001, treatment 72 of 519 (13.9%), control 198 of 2,595 (7.6%), adjusted per study, death/intubation/ICU, propensity score matching, multivariable, Cox proportional hazards.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Zhou et al., 4 Dec 2020, retrospective, propensity score matching, China, peer-reviewed, 7 authors, study period 1 January, 2020 - 22 August, 2020.
Upregulation of enteric alpha-synuclein as a possible link between inflammatory bowel disease and Parkinson’s disease
Gut, doi:10.1136/gutjnl-2020-323482
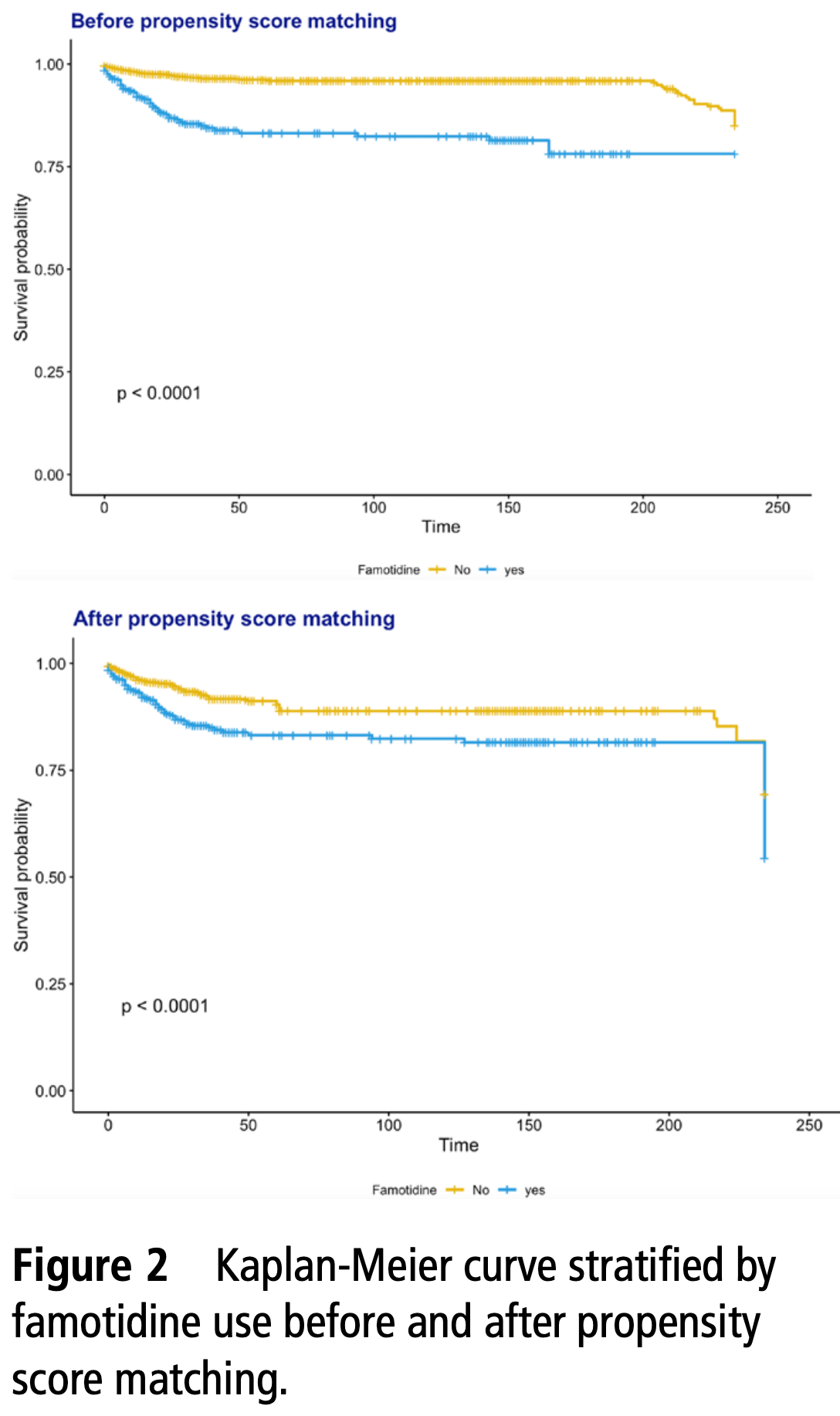
PostScript Figure 1 Kaplan-Meier curve stratified by proton pump inhibitor (PPI) use before and after propensity score matching. Figure 2 Kaplan-Meier curve stratified by famotidine use before and after propensity score matching. Provenance and peer review Not commissioned; externally peer reviewed.
Competing interests None declared.
Patient consent for publication Not required. ethics approval This study was approved by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster. Provenance and peer review Not commissioned; internally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise. This article is made freely available for use in accordance with BMJ's website terms and conditions for the duration of the covid-19 pandemic or until otherwise determined by BMJ. You may use, download and print the article for any lawful, non-commercial purpose (including text and data mining) provided that all copyright notices and trade marks are retained. Proton pump inhibitors and the risk of severe COVID-19: a post-hoc analysis from the Korean nationwide cohort We..
DOI record:
{
"DOI": "10.1136/gutjnl-2020-323668",
"ISSN": [
"0017-5749",
"1468-3288"
],
"URL": "http://dx.doi.org/10.1136/gutjnl-2020-323668",
"alternative-id": [
"10.1136/gutjnl-2020-323668"
],
"author": [
{
"affiliation": [],
"family": "Zhou",
"given": "Jiandong",
"sequence": "first"
},
{
"affiliation": [],
"family": "Wang",
"given": "Xiansong",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lee",
"given": "Sharen",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wu",
"given": "William Ka Kei",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cheung",
"given": "Bernard Man Yung",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6819-0686",
"affiliation": [],
"authenticated-orcid": false,
"family": "Zhang",
"given": "Qingpeng",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-5510-1253",
"affiliation": [],
"authenticated-orcid": false,
"family": "Tse",
"given": "Gary",
"sequence": "additional"
}
],
"container-title": [
"Gut"
],
"content-domain": {
"crossmark-restriction": true,
"domain": [
"bmj.com"
]
},
"created": {
"date-parts": [
[
2020,
12,
5
]
],
"date-time": "2020-12-05T01:16:51Z",
"timestamp": 1607131011000
},
"deposited": {
"date-parts": [
[
2021,
10,
20
]
],
"date-time": "2021-10-20T15:28:20Z",
"timestamp": 1634743700000
},
"funder": [
{
"DOI": "10.13039/501100001809",
"award": [
"72042018, 71972164 and 71672163"
],
"doi-asserted-by": "crossref",
"name": "National Natural Science Foundation of China"
},
{
"DOI": "10.13039/501100005847",
"award": [
"16171991"
],
"doi-asserted-by": "crossref",
"name": "Health and Medical Research Fund"
},
{
"award": [
"Theme‐Based Research Scheme (T32‐102/14N)"
],
"name": "Research Grants Council"
}
],
"indexed": {
"date-parts": [
[
2022,
1,
7
]
],
"date-time": "2022-01-07T20:09:25Z",
"timestamp": 1641586165944
},
"is-referenced-by-count": 21,
"issn-type": [
{
"type": "print",
"value": "0017-5749"
},
{
"type": "electronic",
"value": "1468-3288"
}
],
"issue": "10",
"issued": {
"date-parts": [
[
2020,
12,
4
]
]
},
"journal-issue": {
"issue": "10",
"published-online": {
"date-parts": [
[
2021,
9,
8
]
]
},
"published-print": {
"date-parts": [
[
2021,
10
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://bmj.com/coronavirus/usage",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2020,
12,
4
]
],
"date-time": "2020-12-04T00:00:00Z",
"timestamp": 1607040000000
}
}
],
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1136/gutjnl-2020-323668",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "239",
"original-title": [],
"page": "2012-2013",
"prefix": "10.1136",
"published": {
"date-parts": [
[
2020,
12,
4
]
]
},
"published-online": {
"date-parts": [
[
2020,
12,
4
]
]
},
"published-print": {
"date-parts": [
[
2021,
10
]
]
},
"publisher": "BMJ",
"reference": [
{
"article-title": "Severe clinical outcomes of COVID-19 associated with proton pump inhibitors: a nationwide cohort study with propensity score matching",
"author": "Lee",
"journal-title": "Gut",
"key": "2021102004101007000_70.10.2012.1",
"year": "2020"
},
{
"article-title": "Do proton pump inhibitors influence SARS-CoV-2 related outcomes? A meta-analysis",
"author": "Li",
"journal-title": "Gut",
"key": "2021102004101007000_70.10.2012.2",
"year": "2020"
},
{
"DOI": "10.1053/j.gastro.2020.05.053",
"doi-asserted-by": "publisher",
"key": "2021102004101007000_70.10.2012.3"
},
{
"DOI": "10.14309/ajg.0000000000000832",
"doi-asserted-by": "publisher",
"key": "2021102004101007000_70.10.2012.4"
},
{
"article-title": "Famotidine use is not associated with 30-day mortality: a Coarsened exact match study in 7158 hospitalized COVID-19 patients from a large healthcare system",
"author": "Yeramaneni",
"journal-title": "Gastroenterology",
"key": "2021102004101007000_70.10.2012.5",
"year": "2020"
},
{
"DOI": "10.1053/j.gastro.2020.05.098",
"doi-asserted-by": "crossref",
"key": "2021102004101007000_70.10.2012.6",
"unstructured": "Cheung KS , Hung IFN , Leung WK . Association between famotidine use and COVID-19 severity in Hong Kong: a territory-wide study. Gastroenterology 2020.doi:10.1053/j.gastro.2020.05.098"
}
],
"reference-count": 6,
"references-count": 6,
"relation": {},
"score": 1,
"short-container-title": [
"Gut"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Gastroenterology"
],
"subtitle": [],
"title": [
"Proton pump inhibitor or famotidine use and severe COVID-19 disease: a propensity score-matched territory-wide study"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1136/crossmarkpolicy",
"volume": "70"
}