Relation of severe COVID-19 to polypharmacy and prescribing of psychotropic drugs: the REACT-SCOT case-control study
et al., BMC Medicine, doi:10.1186/s12916-021-01907-8, EUPAS35558, Feb 2021
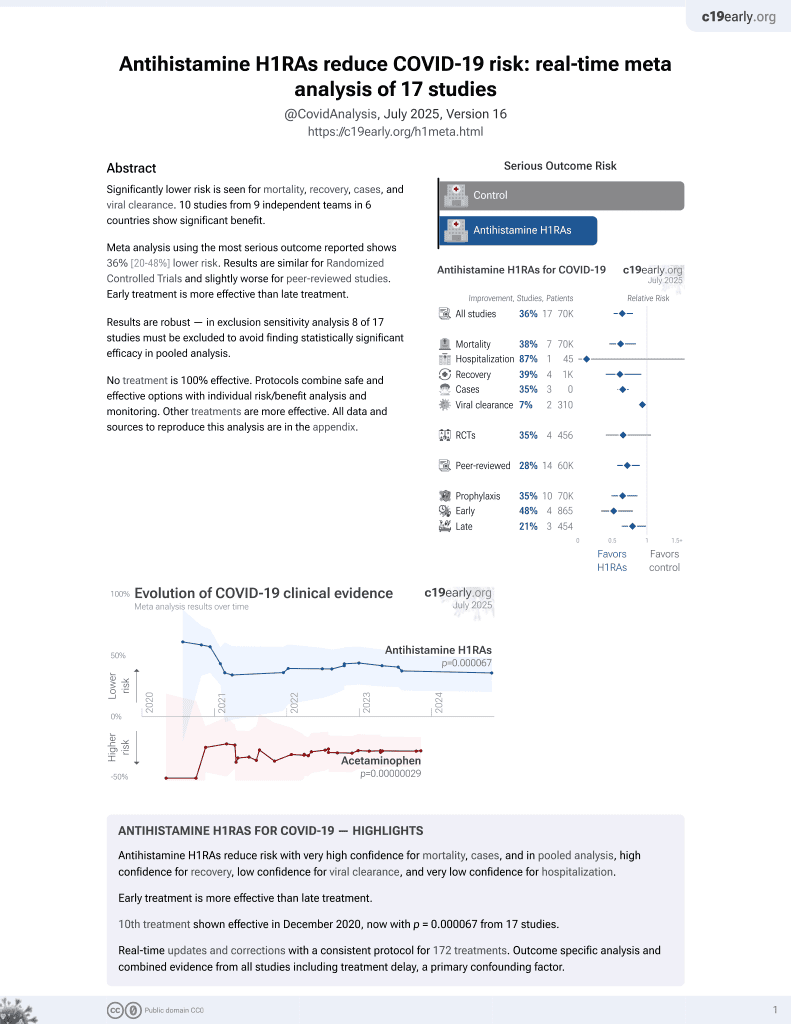
11th treatment shown to reduce risk in
December 2020, now with p = 0.000052 from 17 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
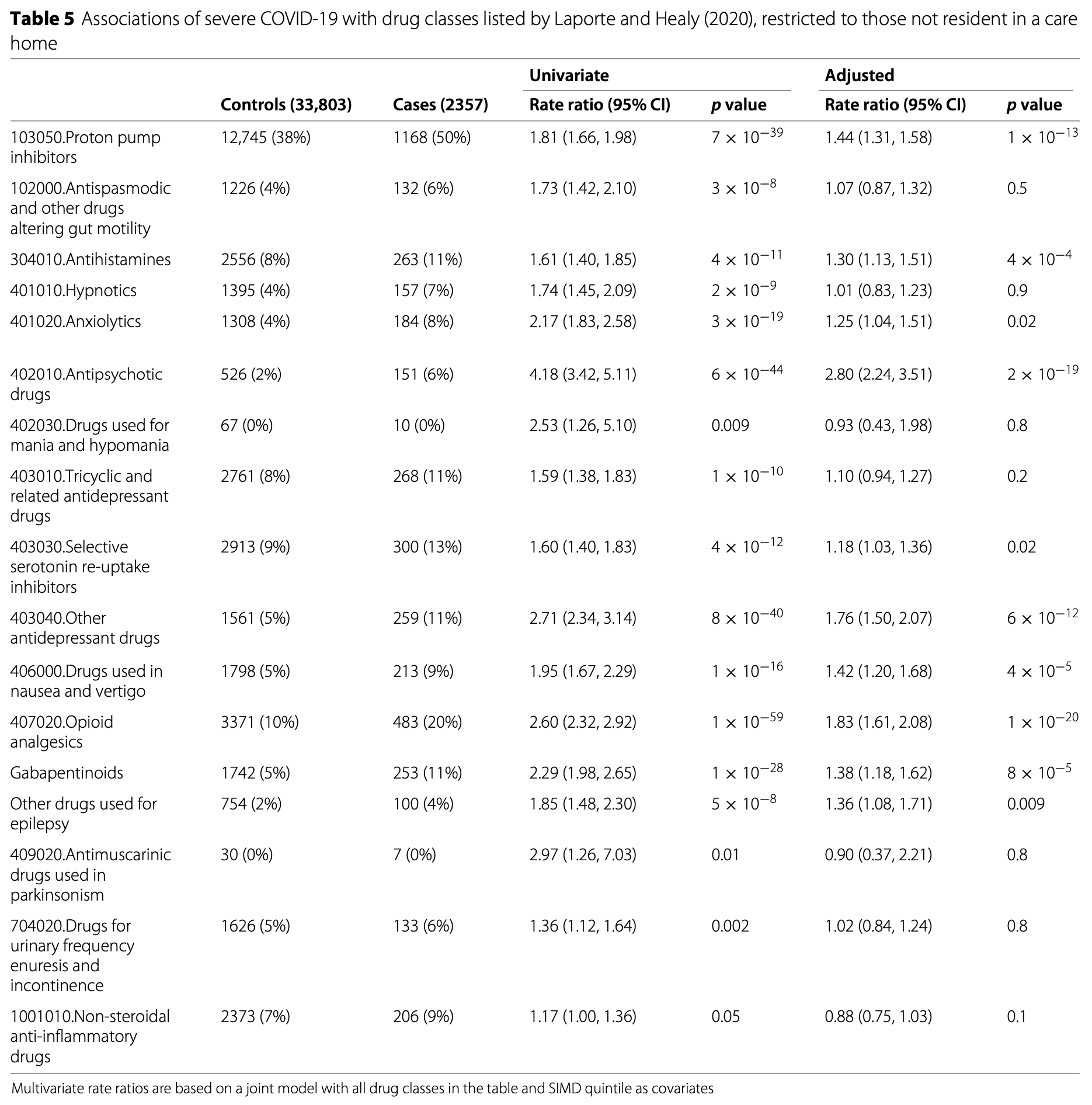
Retrospective 4,251 severe COVID-19 cases and 36,738 matched controls in Scotland showing increased risk of severe COVID-19 with PPI use and antihistamine H1RA use. Adjusted results are only provided for the patients not in care homes (2,357 cases and 33,803 controls).
Study covers proton pump inhibitors and antihistamine H1RAs.
|
risk of severe case, 30.0% higher, OR 1.30, p < 0.001, treatment 263 of 2,357 (11.2%) cases,
2,556 of 33,803 (7.6%) controls, adjusted per study, case control OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
McKeigue et al., 22 Feb 2021, retrospective, Scotland, peer-reviewed, 18 authors, trial EUPAS35558.
Contact: paul.mckeigue@ed.ac.uk (corresponding author).
Relation of severe COVID-19 to polypharmacy and prescribing of psychotropic drugs: the REACT-SCOT case-control study
BMC Medicine, doi:10.1186/s12916-021-01907-8
Background: The objective of this study was to investigate the relation of severe COVID-19 to prior drug prescribing. Methods: Severe cases were defined by entry to critical care or fatal outcome. For this matched case-control study (REACT-SCOT), all 4251 cases of severe COVID-19 in Scotland since the start of the epidemic were matched for age, sex and primary care practice to 36,738 controls from the population register. Records were linked to hospital discharges since June 2015 and dispensed prescriptions issued in primary care during the last 240 days. Results: Severe COVID-19 was strongly associated with the number of non-cardiovascular drug classes dispensed. This association was strongest in those not resident in a care home, in whom the rate ratio (95% CI) associated with dispensing of 12 or more drug classes versus none was 10.8 (8.8, 13.3), and in those without any of the conditions designated as conferring increased risk of COVID-19. Of 17 drug classes postulated at the start of the epidemic to be "medications compromising COVID", all were associated with increased risk of severe COVID-19 and these associations were present in those without any of the designated risk conditions. The fraction of cases in the population attributable to exposure to these drug classes was 38%. The largest effect was for antipsychotic agents: rate ratio 4. 18 (3.42, 5.11). Other drug classes with large effects included proton pump inhibitors (rate ratio 2.20 (1.72, 2.83) for = 2 defined daily doses/day), opioids (3.66 (2.68, 5.01) for = 50 mg morphine equivalent/day) and gabapentinoids. These associations persisted after adjusting for covariates and were stronger with recent than with non-recent exposure. Conclusions: Severe COVID-19 is associated with polypharmacy and with drugs that cause sedation, respiratory depression, or dyskinesia; have anticholinergic effects; or affect the gastrointestinal system. These associations are not easily explained by co-morbidity. Measures to reduce the burden of mortality and morbidity from COVID-19 should (Continued on next page)
Supplementary Information The online version contains supplementary material available at https://doi.org/10.1186/s12916-021-01907-8. Additional file 1: Supplementary information.
Authors' contributions PM, DA, CR, RW, JM, SH and HC provided substantial contributions to the conception or design and drafting of the manuscript. NL, ASP, DG and JM provided substantial contributions to the data acquisition. SK, AW, JB, SM and BG provided substantial contributions to the data analysis or interpretation. All authors contributed to revising the manuscript critically for important intellectual content and approved the final manuscript.
Ethics approval and consent to participate This study was conducted under approvals from the Public Benefit and Privacy Panel for Health and Social Care that allow Public Health Scotland staff to link datasets. Datasets were de-identified before analysis.
Consent for publication Not applicable.
Competing interests HC receives research support and honoraria and is a member of advisory panels or speaker bureaus for Sanofi Aventis, Regeneron, Novartis, Novo-Nordisk and Eli Lilly. HC receives or has recently received non-binding research support from AstraZeneca and Novo-Nordisk. SH received honoraria from Gilead.
Publisher's Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Alexander, Debono, Mammen, Iorio, Aryal et al., COVID-19 research has overall low methodological quality thus far: case in point for chloroquine/hydroxychloroquine, J Clin Epidemiol
Alvarez-Madrazo, Mctaggart, Nangle, Nicholson, Bennie, Data resource profile: the Scottish national prescribing information system (PIS), Int J Epidemiol
Appleton, Abel, Payne, Cardiovascular polypharmacy is not associated with unplanned hospitalisation: evidence from a retrospective cohort study, BMC Fam Pract, doi:10.1186/1471-2296-15-58
Aronson, Ferner, Drugs and the renin-angiotensin system in covid-19, BMJ, doi:10.1136/bmj.m1313
Bruzzi, Green, Byar, Brinton, Schairer, Estimating the population attributable risk for multiple risk factors using case-control data, Am J Epidemiol
Connors, Levy, COVID-19 and its implications for thrombosis and anticoagulation, Blood J Am Soc Hematol
De Abajo, Rodríguez-Martín, Lerma, Mejía-Abril, Aguilar et al., Use of renin-angiotensin-aldosterone system inhibitors and risk of COVID-19 requiring admission to hospital: a case-population study, Lancet
Edelman, Gordon, Crothers, Akgün, Bryant et al., Association of prescribed opioids with increased risk of community-acquired pneumonia among patients with and without HIV, JAMA Intern Med
Fastboom, Holm, Nyman, State, Läkemedelsanvändningen Hos Personer Som Intensivvårdats Eller Avlidit till Följd av Covid-19, Socialstyrelsen
Hallas, Pottegård, Use of self-controlled designs in pharmacoepidemiology, J Intern Med
Laporte, Healy, Data-based Medicine Americas Ltd
Leelakanok, Holcombe, Lund, Gu, Schweizer, Association between polypharmacy and death: a systematic review and meta-analysis, J Am Pharmacists Assoc
Luo, Xiao, Chen, Changes in proton pump inhibitor prescribing trend over the past decade and pharmacists' effect on prescribing practice at a tertiary hospital, BMC Health Serv Res
Macbride-Stewart, Guthrie, Marwick, Hurding, National Therapeutic Indicators in Scotland and Financial Incentives, Int J Popul Data Sci, doi:10.23889/ijpds.v4i3.1230
Maclure, Mittleman, Should we use a case-crossover design?, Annu Rev Public Health
Mancia, Rea, Ludergnani, Apolone, Corrao, Renin?angiotensin?aldosterone system blockers and the risk of Covid-19, N Engl J Med
Mckeigue, Weir, Bishop, Mcgurnaghan, Kennedy et al., Rapid Epidemiological Analysis of Comorbidities and Treatments as risk factors for COVID-19 in Scotland (REACT-SCOT): a population-based case-control study, PLoS Med
Nhs, Who's at Higher Risk from Coronavirus
Pasina, Elli, Nobili, Ianes, Overuse of proton pump inhibitors in nursing homes: an Italian multicenter observational study, Pharmacoepidemiol Drug Saf
Ramirez, Lei, Borobia, Piñana, Fudio et al., Overuse of PPIs in patients at admission, during treatment, and at discharge in a tertiary Spanish hospital, Curr Clin Pharmacol
Sarkar, Hennessy, Yang, Proton-pump inhibitor use and the risk for community-acquired pneumonia, Ann Intern Med
Shi, Sun, Hu, Enteric involvement of SARS-CoV-2: Implications for the COVID-19 management, transmission, and infection control, Virulence
Trifirò, Gambassi, Sen, Caputi, Bagnardi et al., Association of community-acquired pneumonia with antipsychotic drug use in elderly patients: a nested case-control study, Ann Intern Med
Weiner, Malek, Price, The opioid crisis and its consequences, Transplantation
Wiese, Griffin, Schaffner, Stein, Greevy et al., Opioid analgesic use and risk for invasive pneumococcal diseases: a nested case?control study, Ann Intern Med
DOI record:
{
"DOI": "10.1186/s12916-021-01907-8",
"ISSN": [
"1741-7015"
],
"URL": "http://dx.doi.org/10.1186/s12916-021-01907-8",
"abstract": "<jats:title>Abstract</jats:title><jats:sec>\n <jats:title>Background</jats:title>\n <jats:p>The objective of this study was to investigate the relation of severe COVID-19 to prior drug prescribing.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Methods</jats:title>\n <jats:p>Severe cases were defined by entry to critical care or fatal outcome. For this matched case-control study (REACT-SCOT), all 4251 cases of severe COVID-19 in Scotland since the start of the epidemic were matched for age, sex and primary care practice to 36,738 controls from the population register. Records were linked to hospital discharges since June 2015 and dispensed prescriptions issued in primary care during the last 240 days.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Results</jats:title>\n <jats:p>Severe COVID-19 was strongly associated with the number of non-cardiovascular drug classes dispensed. This association was strongest in those not resident in a care home, in whom the rate ratio (95% CI) associated with dispensing of 12 or more drug classes versus none was 10.8 (8.8, 13.3), and in those without any of the conditions designated as conferring increased risk of COVID-19. Of 17 drug classes postulated at the start of the epidemic to be “medications compromising COVID”, all were associated with increased risk of severe COVID-19 and these associations were present in those without any of the designated risk conditions. The fraction of cases in the population attributable to exposure to these drug classes was 38%. The largest effect was for antipsychotic agents: rate ratio 4.18 (3.42, 5.11). Other drug classes with large effects included proton pump inhibitors (rate ratio 2.20 (1.72, 2.83) for = 2 defined daily doses/day), opioids (3.66 (2.68, 5.01) for = 50 mg morphine equivalent/day) and gabapentinoids. These associations persisted after adjusting for covariates and were stronger with recent than with non-recent exposure.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Conclusions</jats:title>\n <jats:p>Severe COVID-19 is associated with polypharmacy and with drugs that cause sedation, respiratory depression, or dyskinesia; have anticholinergic effects; or affect the gastrointestinal system. These associations are not easily explained by co-morbidity. Measures to reduce the burden of mortality and morbidity from COVID-19 should include reinforcing existing guidance on reducing overprescribing of these drug classes and limiting inappropriate polypharmacy.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Registration</jats:title>\n <jats:p>ENCEPP number https://EUPAS35558</jats:p>\n </jats:sec>",
"alternative-id": [
"1907"
],
"article-number": "51",
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "25 August 2020"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "11 January 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "22 February 2021"
},
{
"group": {
"label": "Consent for publication",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1,
"value": "Not applicable."
},
{
"group": {
"label": "Competing interests",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "HC receives research support and honoraria and is a member of advisory panels or speaker bureaus for Sanofi Aventis, Regeneron, Novartis, Novo-Nordisk and Eli Lilly. HC receives or has recently received non-binding research support from AstraZeneca and Novo-Nordisk. SH received honoraria from Gilead."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-5217-1034",
"affiliation": [],
"authenticated-orcid": false,
"family": "McKeigue",
"given": "Paul M.",
"sequence": "first"
},
{
"affiliation": [],
"name": "on behalf of Public Health Scotland COVID-19 Health Protection Study Group",
"sequence": "first"
},
{
"affiliation": [],
"family": "Kennedy",
"given": "Sharon",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Weir",
"given": "Amanda",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bishop",
"given": "Jen",
"sequence": "additional"
},
{
"affiliation": [],
"family": "McGurnaghan",
"given": "Stuart J.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "McAllister",
"given": "David",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Robertson",
"given": "Chris",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wood",
"given": "Rachael",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lone",
"given": "Nazir",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Murray",
"given": "Janet",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Caparrotta",
"given": "Thomas M.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Smith-Palmer",
"given": "Alison",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Goldberg",
"given": "David",
"sequence": "additional"
},
{
"affiliation": [],
"family": "McMenamin",
"given": "Jim",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Guthrie",
"given": "Bruce",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hutchinson",
"given": "Sharon",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Colhoun",
"given": "Helen M.",
"sequence": "additional"
}
],
"container-title": "BMC Medicine",
"container-title-short": "BMC Med",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2021,
2,
22
]
],
"date-time": "2021-02-22T02:02:59Z",
"timestamp": 1613959379000
},
"deposited": {
"date-parts": [
[
2021,
2,
22
]
],
"date-time": "2021-02-22T02:03:51Z",
"timestamp": 1613959431000
},
"indexed": {
"date-parts": [
[
2024,
7,
19
]
],
"date-time": "2024-07-19T00:54:48Z",
"timestamp": 1721350488291
},
"is-referenced-by-count": 38,
"issue": "1",
"issued": {
"date-parts": [
[
2021,
2,
22
]
]
},
"journal-issue": {
"issue": "1",
"published-print": {
"date-parts": [
[
2021,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
2,
22
]
],
"date-time": "2021-02-22T00:00:00Z",
"timestamp": 1613952000000
}
},
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
2,
22
]
],
"date-time": "2021-02-22T00:00:00Z",
"timestamp": 1613952000000
}
}
],
"link": [
{
"URL": "http://link.springer.com/content/pdf/10.1186/s12916-021-01907-8.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "http://link.springer.com/article/10.1186/s12916-021-01907-8/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "http://link.springer.com/content/pdf/10.1186/s12916-021-01907-8.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1186",
"published": {
"date-parts": [
[
2021,
2,
22
]
]
},
"published-online": {
"date-parts": [
[
2021,
2,
22
]
]
},
"published-print": {
"date-parts": [
[
2021,
12
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1136/bmj.m1313",
"author": "JK Aronson",
"doi-asserted-by": "publisher",
"first-page": "m1313",
"journal-title": "BMJ",
"key": "1907_CR1",
"unstructured": "Aronson JK, Ferner RE. Drugs and the renin-angiotensin system in covid-19. BMJ. 2020; 369:m1313. https://doi.org/10.1136/bmj.m1313.",
"volume": "369",
"year": "2020"
},
{
"key": "1907_CR2",
"unstructured": "Laporte J-R, Healy D. In the midst of the SARS-CoV-2 pandemia, caution is needed with drugs that increase the risk of pneumonia: Data-based Medicine Americas Ltd; 2020. https://rxisk.org/medications-compromising-covidinfections/."
},
{
"DOI": "10.1371/journal.pmed.1003374",
"author": "PM McKeigue",
"doi-asserted-by": "publisher",
"first-page": "1003374",
"journal-title": "PLoS Med",
"key": "1907_CR3",
"unstructured": "McKeigue PM, Weir A, Bishop J, McGurnaghan SJ, Kennedy S, McAllister D, et al. Rapid Epidemiological Analysis of Comorbidities and Treatments as risk factors for COVID-19 in Scotland (REACT-SCOT): a population-based case-control study. PLoS Med. 2020; 17:1003374.",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.1093/ije/dyw060",
"author": "S Alvarez-Madrazo",
"doi-asserted-by": "publisher",
"first-page": "714",
"journal-title": "Int J Epidemiol",
"key": "1907_CR4",
"unstructured": "Alvarez-Madrazo S, McTaggart S, Nangle C, Nicholson E, Bennie M. Data resource profile: the Scottish national prescribing information system (PIS). Int J Epidemiol. 2016; 45:714–5.",
"volume": "45",
"year": "2016"
},
{
"DOI": "10.1186/1471-2296-15-58",
"author": "SC Appleton",
"doi-asserted-by": "publisher",
"first-page": "58",
"journal-title": "BMC Fam Pract",
"key": "1907_CR5",
"unstructured": "Appleton SC, Abel GA, Payne RA. Cardiovascular polypharmacy is not associated with unplanned hospitalisation: evidence from a retrospective cohort study. BMC Fam Pract. 2014; 15:58. https://doi.org/10.1186/1471-2296-15-58.",
"volume": "15",
"year": "2014"
},
{
"key": "1907_CR6",
"unstructured": "NHS. Who’s at Higher Risk from Coronavirus. 2020. https://www.nhs.uk/conditions/coronaviruscovid-19/people-at-higher-risk/whos-at-higher-risk-fromcoronavirus/."
},
{
"DOI": "10.1093/oxfordjournals.aje.a114174",
"author": "P Bruzzi",
"doi-asserted-by": "publisher",
"first-page": "904",
"journal-title": "Am J Epidemiol",
"key": "1907_CR7",
"unstructured": "Bruzzi P, Green SB, Byar DP, Brinton LA, Schairer C. Estimating the population attributable risk for multiple risk factors using case-control data. Am J Epidemiol. 1985; 122:904–14.",
"volume": "122",
"year": "1985"
},
{
"DOI": "10.1146/annurev.publhealth.21.1.193",
"author": "M Maclure",
"doi-asserted-by": "publisher",
"first-page": "193",
"journal-title": "Annu Rev Public Health",
"key": "1907_CR8",
"unstructured": "Maclure M, Mittleman MA. Should we use a case-crossover design?Annu Rev Public Health. 2000; 21:193–221.",
"volume": "21",
"year": "2000"
},
{
"DOI": "10.1056/NEJMoa2006923",
"author": "G Mancia",
"doi-asserted-by": "publisher",
"first-page": "2431",
"journal-title": "N Engl J Med",
"key": "1907_CR9",
"unstructured": "Mancia G, Rea F, Ludergnani M, Apolone G, Corrao G. Renin?angiotensin?aldosterone system blockers and the risk of Covid-19. N Engl J Med. 2020; 382:2431–40.",
"volume": "382",
"year": "2020"
},
{
"author": "JM Connors",
"first-page": "2033—40",
"journal-title": "Blood J Am Soc Hematol",
"key": "1907_CR10",
"unstructured": "Connors JM, Levy JH. COVID-19 and its implications for thrombosis and anticoagulation. Blood J Am Soc Hematol. 2020; 135:2033—40.",
"volume": "135",
"year": "2020"
},
{
"DOI": "10.1016/j.jclinepi.2020.04.016",
"author": "PE Alexander",
"doi-asserted-by": "publisher",
"first-page": "120",
"journal-title": "J Clin Epidemiol",
"key": "1907_CR11",
"unstructured": "Alexander PE, Debono VB, Mammen MJ, Iorio A, Aryal K, Deng D, et al. COVID-19 research has overall low methodological quality thus far: case in point for chloroquine/hydroxychloroquine. J Clin Epidemiol. 2020; 123:120–6.",
"volume": "123",
"year": "2020"
},
{
"DOI": "10.1016/j.japh.2017.06.002",
"doi-asserted-by": "crossref",
"key": "1907_CR12",
"unstructured": "Leelakanok N, Holcombe AL, Lund BC, Gu X, Schweizer ML. Association between polypharmacy and death: a systematic review and meta-analysis. J Am Pharmacists Assoc; 57:729–38."
},
{
"DOI": "10.23889/ijpds.v4i3.1230",
"doi-asserted-by": "publisher",
"key": "1907_CR13",
"unstructured": "MacBride-Stewart S, Guthrie B, Marwick C, Hurding S. National Therapeutic Indicators in Scotland and Financial Incentives. Int J Popul Data Sci. 2019;4(3). https://doi.org/10.23889/ijpds.v4i3.1230."
},
{
"DOI": "10.1001/jamainternmed.2018.6101",
"author": "EJ Edelman",
"doi-asserted-by": "publisher",
"first-page": "297",
"journal-title": "JAMA Intern Med",
"key": "1907_CR14",
"unstructured": "Edelman EJ, Gordon KS, Crothers K, Akgün K, Bryant KJ, Becker WC, et al. Association of prescribed opioids with increased risk of community-acquired pneumonia among patients with and without HIV. JAMA Intern Med. 2019; 179:297–304.",
"volume": "179",
"year": "2019"
},
{
"DOI": "10.1111/joim.12186",
"author": "J Hallas",
"doi-asserted-by": "publisher",
"first-page": "581",
"journal-title": "J Intern Med",
"key": "1907_CR15",
"unstructured": "Hallas J, Pottegård A. Use of self-controlled designs in pharmacoepidemiology. J Intern Med. 2014; 275:581–9.",
"volume": "275",
"year": "2014"
},
{
"key": "1907_CR16",
"unstructured": "Fastboom J, Holm J, Nyman A, State M. Läkemedelsanvändningen Hos Personer Som Intensivvårdats Eller Avlidit till Följd av Covid-19. Socialstyrelsen. 2020. https://www.socialstyrelsen.se/globalassets/sharepointdokument/dokument-webb/ovrigt/faktabladlakemedelsanvandning-covid19.pdf."
},
{
"DOI": "10.7326/M17-1907",
"author": "AD Wiese",
"doi-asserted-by": "publisher",
"first-page": "396",
"journal-title": "Ann Intern Med",
"key": "1907_CR17",
"unstructured": "Wiese AD, Griffin MR, Schaffner W, Stein CM, Greevy RA, Mitchel EF, et al. Opioid analgesic use and risk for invasive pneumococcal diseases: a nested case?control study. Ann Intern Med. 2018; 168:396–404.",
"volume": "168",
"year": "2018"
},
{
"DOI": "10.7326/0003-4819-152-7-201004060-00006",
"author": "G Trifirò",
"doi-asserted-by": "publisher",
"first-page": "418",
"journal-title": "Ann Intern Med",
"key": "1907_CR18",
"unstructured": "Trifirò G, Gambassi G, Sen EF, Caputi AP, Bagnardi V, Brea J, et al. Association of community-acquired pneumonia with antipsychotic drug use in elderly patients: a nested case-control study. Ann Intern Med. 2010; 152:418–25.",
"volume": "152",
"year": "2010"
},
{
"DOI": "10.7326/0003-4819-149-6-200809160-00005",
"author": "M Sarkar",
"doi-asserted-by": "publisher",
"first-page": "391",
"journal-title": "Ann Intern Med",
"key": "1907_CR19",
"unstructured": "Sarkar M, Hennessy S, Yang Y-X. Proton-pump inhibitor use and the risk for community-acquired pneumonia. Ann Intern Med. 2008; 149:391–8.",
"volume": "149",
"year": "2008"
},
{
"DOI": "10.1080/21505594.2020.1794410",
"author": "J Shi",
"doi-asserted-by": "publisher",
"first-page": "941",
"journal-title": "Virulence",
"key": "1907_CR20",
"unstructured": "Shi J, Sun J, Hu Y. Enteric involvement of SARS-CoV-2: Implications for the COVID-19 management, transmission, and infection control. Virulence. 2020; 11:941–4.",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1186/s12913-018-3358-5",
"author": "H Luo",
"doi-asserted-by": "publisher",
"first-page": "537",
"journal-title": "BMC Health Serv Res",
"key": "1907_CR21",
"unstructured": "Luo H, Fan Q, Xiao S, Chen K. Changes in proton pump inhibitor prescribing trend over the past decade and pharmacists’ effect on prescribing practice at a tertiary hospital. BMC Health Serv Res. 2018; 18:537.",
"volume": "18",
"year": "2018"
},
{
"DOI": "10.1002/pds.4963",
"author": "L Pasina",
"doi-asserted-by": "publisher",
"first-page": "461",
"journal-title": "Pharmacoepidemiol Drug Saf",
"key": "1907_CR22",
"unstructured": "Pasina L, Novella A, Elli C, Nobili A, Ianes A. Overuse of proton pump inhibitors in nursing homes: an Italian multicenter observational study. Pharmacoepidemiol Drug Saf. 2020; 29:461–6.",
"volume": "29",
"year": "2020"
},
{
"DOI": "10.2174/157488410793352067",
"author": "E Ramirez",
"doi-asserted-by": "publisher",
"first-page": "288",
"journal-title": "Curr Clin Pharmacol",
"key": "1907_CR23",
"unstructured": "Ramirez E, Lei SH, Borobia AM, Piñana E, Fudio S, Muñoz R, et al. Overuse of PPIs in patients at admission, during treatment, and at discharge in a tertiary Spanish hospital. Curr Clin Pharmacol. 2010; 5:288–97.",
"volume": "5",
"year": "2010"
},
{
"DOI": "10.1097/TP.0000000000001671",
"author": "SG Weiner",
"doi-asserted-by": "publisher",
"first-page": "678",
"journal-title": "Transplantation",
"key": "1907_CR24",
"unstructured": "Weiner SG, Malek SK, Price CN. The opioid crisis and its consequences. Transplantation. 2017; 101:678–81.",
"volume": "101",
"year": "2017"
},
{
"DOI": "10.1016/S0140-6736(20)31030-8",
"author": "FJ de Abajo",
"doi-asserted-by": "publisher",
"first-page": "1705",
"journal-title": "Lancet (London, England)",
"key": "1907_CR25",
"unstructured": "de Abajo FJ, Rodríguez-Martín S, Lerma V, Mejía-Abril G, Aguilar M, García-Luque A, et al. Use of renin-angiotensin-aldosterone system inhibitors and risk of COVID-19 requiring admission to hospital: a case-population study. Lancet (London, England). 2020; 395:1705–14.",
"volume": "395",
"year": "2020"
}
],
"reference-count": 25,
"references-count": 25,
"relation": {
"has-preprint": [
{
"asserted-by": "object",
"id": "10.1101/2020.07.23.20160747",
"id-type": "doi"
}
]
},
"resource": {
"primary": {
"URL": "https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-021-01907-8"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Relation of severe COVID-19 to polypharmacy and prescribing of psychotropic drugs: the REACT-SCOT case-control study",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "19"
}
mckeigue