High vs Low Dose Proton Pump Inhibitor (PPI) related Mortality in Hospitalized Coronavirus Disease-19 (COVID-19): A Retrospective Cohort Study
et al., Journal Of The Indonesian Medical Association, doi:10.47830/jinma-vol.72.2-2022-802, Aug 2022
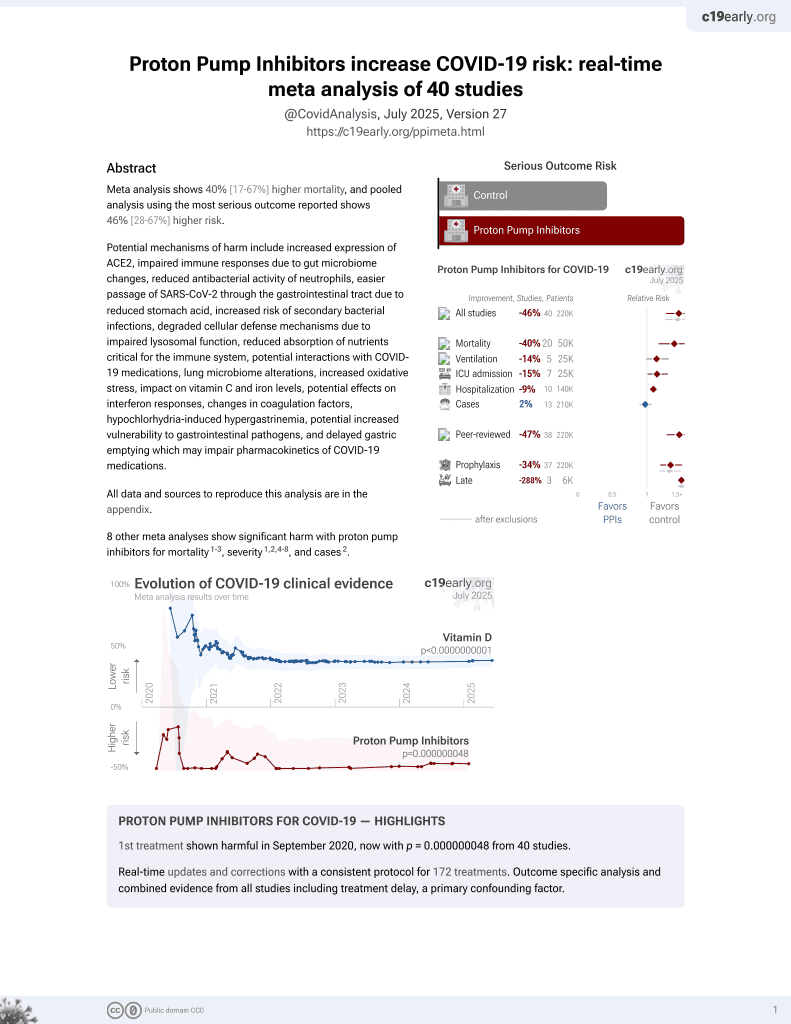
PPIs for COVID-19
1st treatment shown to increase risk in
September 2020, now with p = 0.000000048 from 40 studies.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective hospitalized COVID-19 patients in Indonesia showing higher mortality with high dose proton pump inhibitor (PPI) use compared to low dose.
|
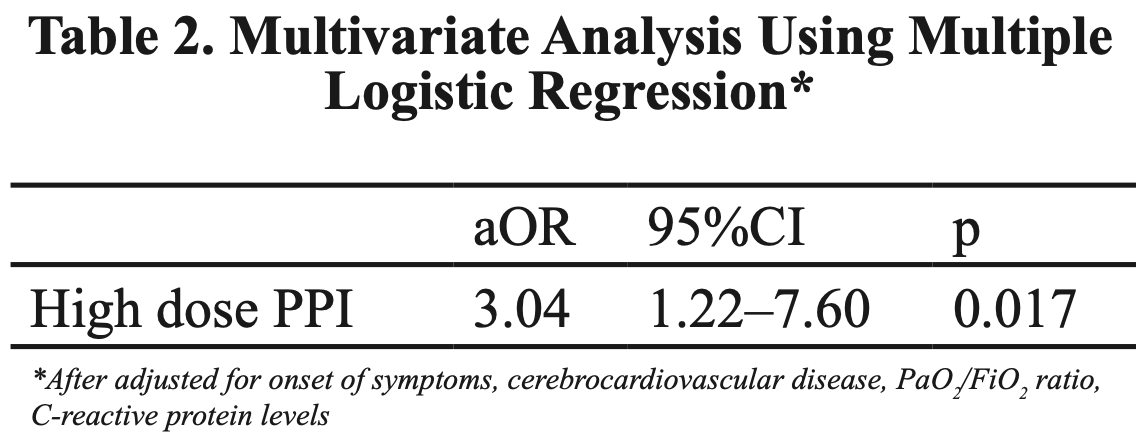
risk of death, 204.0% higher, OR 3.04, p = 0.02, treatment 216, control 149, adjusted per study, multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Liwang et al., 3 Aug 2022, retrospective, Indonesia, peer-reviewed, median age 55.0, 4 authors, study period June 2021 - September 2021.
Contact: fr_archy02@yahoo.com.
High vs Low Dose Proton Pump Inhibitor (PPI) related Mortality in Hospitalized Coronavirus Disease-19 (COVID-19): A Retrospective Cohort Study
Introduction: The role of proton pump inhibitor (PPI) in Coronavirus Disease-19 (COVID-19 ) is still debatable. PPI is commonly used to prevent or treat upper gastrointestinal bleeding and/or dyspeptic symptoms. However, previous studies showed that PPI may lead to adverse outcomes in COVID-19 patients, thus the dose of PPI may play an important role. This study aimed to compare the risk of mortality between high vs low dose PPI in hospitalized COVID-19 patients. Methods: We performed retrospective cohort study from two COVID-19 referral centers in Jakarta between June 2021 and September 2021. We included hospitalized COVID-19 patients, moderate-critically ill cases, who had been given intravenous PPI for more than 7 days. We defined high dose PPI for omeprazole >40 mg/day or pantoprazole >40 mg/day, and low dose PPI for omeprazole ≤40 mg/day or pantoprazole ≤40 mg/day. Results: Of the total 365 patients (median age[Q1-Q3] 55 [45-64] years old), 216 subjects were given high dose PPI. Subjects with high dose PPI had a significantly higher mortality rate than the low dose PPI according to bivariate analysis (54.2% vs 26.1%; p<0.001), but quite similar length of stay (median[Q1-Q3] 12.5 [9-16] vs 13 [9-18] days). After conducting a multivariate analysis to control the confounders, we found that high dose PPI still led to higher mortality (aOR 3.04; 95%CI 1.22-7.60; p=0.017). Conclusion: High dose PPI may increase risk of mortality in hospitalized COVID-19 patients.
Conflicts of Interest None
References
Almario, Chey, Spiegel, Increased risk of covid-19 among users of proton pump inhibitors, Am J Gastroenterol
Bruno, Zaccari, Rocco, Scalese, Panetta et al., Proton pump inhibitors and dysbiosis: Current knowledge and aspects to be clarified, World journal of gastroenterology
Fossmark, Martinsen, Waldum, Adverse effects of proton pump inhibitors-evidence and plausibility, Int J Mol Sci
Freedberg, Kim, Yang, The risks and benefits of long-term use of proton pump inhibitors: expert review and best practice advice from the American Gastroenterological Association, Gastroenterology
Hamai, Iwamoto, Ohshimo, Wakabayashi, Ihara et al., Use of proton pump inhibitors is associated with increased mortality due to nosocomial pneumonia in bedridden patients receiving tube feeding, Geriatr Gerontol Int
Hamming, Timens, Bulthuis, Lely, Navis et al., Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus: a first step in understanding SARS pathogenesis, J Pathol
Kamal, Khan, Sharma, Imam, Howden, Lack of consistent associations between pharmacologic gastric acid suppression and adverse outcomes in patients with coronavirus disease 2019: meta-analysis of observational studies, Gastroenterology
Kim, Kim, Wolf, .60 0.017 *After adjusted for onset of symptoms, cerebrocardiovascular disease, PaO 2 /FiO 2 ratio, C-reactive protein levels Table 2. Multivariate Analysis Using Multiple Logistic Regression, Eur J Clin Pharmacol
Laheij, Sturkenboom, Hassing, Dieleman, Stricker et al., Risk of community-acquired pneumonia and use of gastric acid-suppressive drugs, JAMA
Lee, Ha, Yeniova, Moon, Kim et al., Severe clinical outcomes of COVID-19 associated with proton pump inhibitors: a nationwide cohort study with propensity score matching, Gut
Li, An, Yu, Jiao, Canarutto et al., Do proton pump inhibitors influence SARS-CoV-2 related outcomes? A meta-analysis, Gut
Luxenburger, Sturm, Biever, Rieg, Duerschmied et al., Treatment with proton pump inhibitors increases the risk of secondary infections and ARDS in hospitalized patients with COVID-19: coincidence or underestimated risk factor?, J Intern Med
Ramachandran, Perisetti, Gajendran, Louis, Bansal et al., Pre-hospitalization proton pump inhibitor use and clinical outcomes in COVID-19, European Journal of Gastroenterology & Hepatology
Zhang, Li, Wu, Ling, Qian et al., Analysis of the effect of proton-pump inhibitors on the course of COVID-19, J Inflamm Res
DOI record:
{
"DOI": "10.47830/jinma-vol.72.2-2022-802",
"ISSN": [
"2654-3796",
"2089-1067"
],
"URL": "http://dx.doi.org/10.47830/jinma-vol.72.2-2022-802",
"abstract": "<jats:p>Introduction: The role of proton pump inhibitor (PPI) in Coronavirus Disease-19 (COVID-19) is still debatable. PPI is commonly used to prevent or treat upper gastrointestinal bleeding and/or dyspeptic symptoms. However, previous studies showed that PPI may lead to adverse outcomes in COVID-19 patients, thus the dose of PPI may play an important role. This study aimed to compare the risk of mortality between high vs low dose PPI in hospitalized COVID-19 patients.
\nMethods: We performed retrospective cohort study from two COVID-19 referral centers in Jakarta between June 2021 and September 2021. We included hospitalized COVID-19 patients, moderate-critically ill cases, who had been given intravenous PPI for more than 7 days. We defined high dose PPI for omeprazole >40 mg/day or pantoprazole >40 mg/day, and low dose PPI for omeprazole ≤40 mg/day or pantoprazole ≤40 mg/day.
\nResults: Of the total 365 patients (median age[Q1–Q3] 55 [45–64] years old), 216 subjects were given high dose PPI. Subjects with high dose PPI had a significantly higher mortality rate than the low dose PPI according to bivariate analysis (54.2% vs 26.1%; p<0.001), but quite similar length of stay (median[Q1–Q3] 12.5 [9–16] vs 13 [9–18] days). After conducting a multivariate analysis to control the confounders, we found that high dose PPI still led to higher mortality (aOR 3.04; 95%CI 1.22–7.60; p=0.017).
\nConclusion: High dose PPI may increase risk of mortality in hospitalized COVID-19 patients.</jats:p>",
"author": [
{
"affiliation": [],
"family": "Liwang",
"given": "Frans",
"sequence": "first"
},
{
"affiliation": [],
"family": "Prihartono",
"given": "Nurhayati Adnan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Harareed",
"given": "Haya",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Panjaitan",
"given": "Lucas Welfried",
"sequence": "additional"
}
],
"container-title": "Journal Of The Indonesian Medical Association",
"container-title-short": "J Indon Med Assoc",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
8,
6
]
],
"date-time": "2022-08-06T06:27:26Z",
"timestamp": 1659767246000
},
"deposited": {
"date-parts": [
[
2022,
8,
6
]
],
"date-time": "2022-08-06T06:27:35Z",
"timestamp": 1659767255000
},
"indexed": {
"date-parts": [
[
2022,
8,
6
]
],
"date-time": "2022-08-06T06:41:49Z",
"timestamp": 1659768109690
},
"is-referenced-by-count": 0,
"issue": "2",
"issued": {
"date-parts": [
[
2022,
8,
3
]
]
},
"journal-issue": {
"issue": "2",
"published-online": {
"date-parts": [
[
2022,
8,
6
]
]
}
},
"link": [
{
"URL": "https://mki-ojs.idionline.org/jurnal/article/download/802/241",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://mki-ojs.idionline.org/jurnal/article/download/802/241",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "27170",
"original-title": [],
"page": "59-65",
"prefix": "10.47830",
"published": {
"date-parts": [
[
2022,
8,
3
]
]
},
"published-online": {
"date-parts": [
[
2022,
8,
3
]
]
},
"publisher": "Ikatan Dokter Indonesia",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://mki-ojs.idionline.org/jurnal/article/view/802"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "High vs Low Dose Proton Pump Inhibitor (PPI) related Mortality in Hospitalized Coronavirus Disease-19 (COVID-19): A Retrospective Cohort Study",
"type": "journal-article",
"volume": "72"
}