Proton pump inhibitor therapy usage and associated hospitalization rates and critical care outcomes of COVID-19 patients
et al., Scientific Reports, doi:10.1038/s41598-022-11680-0, May 2022
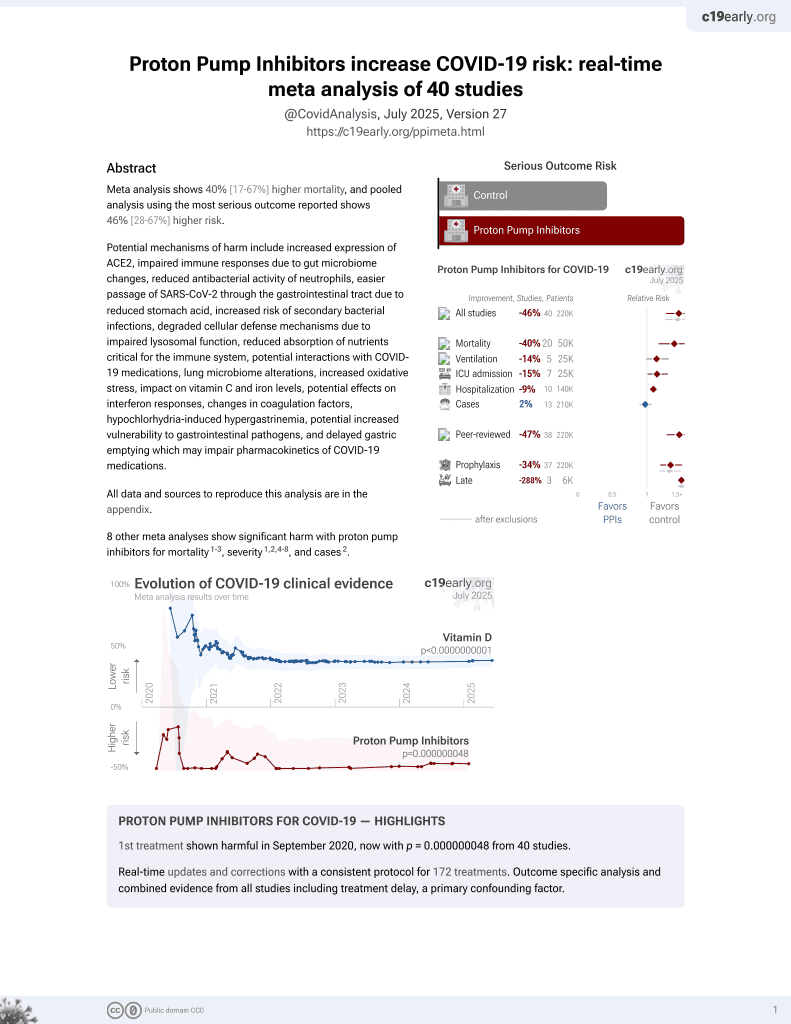
PPIs for COVID-19
1st treatment shown to increase risk in
September 2020, now with p = 0.000000048 from 40 studies.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 2,594 COVID-19 patients in the United States showing no significant association between proton pump inhibitor (PPI) use and COVID-19 severity, including need for hospitalization or 30-day mortality.
There was increasing mortality with increasing PPI use with 14%, 20%, and 27% mortality for low, standard, and high use, without statistical significance.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
risk of death, 19.0% lower, OR 0.81, p = 0.32, treatment 448, control 2,048, adjusted per study, multivariable, RR approximated with OR.
|
|
risk of hospitalization, 10.0% higher, OR 1.10, p = 0.51, treatment 448, control 2,048, adjusted per study, multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Shupp et al., 9 May 2022, retrospective, USA, peer-reviewed, mean age 52.6, 8 authors, study period March 2020 - August 2020.
Contact: brittney.shupp@sluhn.org.
Proton pump inhibitor therapy usage and associated hospitalization rates and critical care outcomes of COVID-19 patients
Scientific Reports, doi:10.1038/s41598-022-11680-0
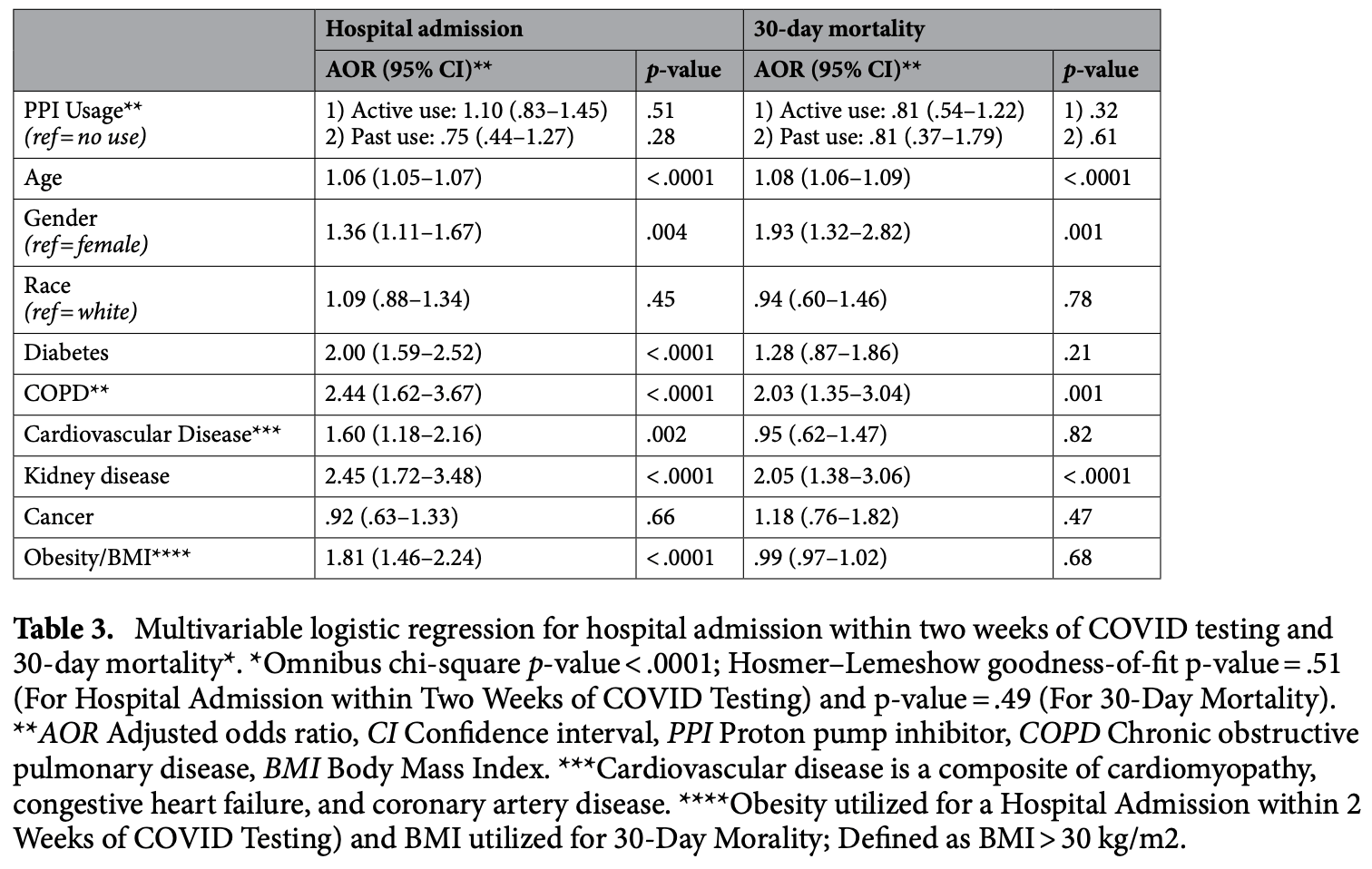
Proton Pump Inhibitors (PPI) are one of the most prescribed medications in the United States. However, PPIs have been shown to increase the risk of enteric infections. Our study aims to evaluate the correlation between PPI and COVID-19 severity. We performed a retrospective cohort study on patients who tested positive for SARS-CoV-2 from March to August 2020. Patients were categorized based on PPI user status. Primary outcomes included need for hospital or ICU admission and 30-day mortality. Secondary outcomes looked to determine the severity of COVID-19 infection and effect of comorbid conditions. 2,594 patients were reviewed. The primary outcomes of our study found that neither active nor past PPI use was associated with increased hospital admission or 30-day mortality following completion of multivariate analysis. Additionally, there was no association between COVID-19 infection and the strength of PPI dosing (low, standard, high). However, the following covariates were independently and significantly associated with increased admission: age, male gender, diabetes, COPD, composite cardiovascular disease, kidney disease, and obesity. The following covariates were associated with increased mortality: age, male gender, COPD, and kidney disease. In conclusion, the high risk features and comorbidities of PPI users were found to have a stronger correlation to severe COVID-19 infection and poor outcomes as opposed to the use of PPI therapy.
SARS-CoV-2 or Coronavirus Disease 2019 (COVID-19 ) is a viral disease that has surmounted into a global pandemic immensely impacting healthcare in the United States (US) and around the world. As of March 2022, there are over 446 million worldwide cases of recorded COVID-19 infections with over 80 million in the US alone and millions of high-risk individuals who remain unvaccinated 1 . The clinical manifestations of COVID-19 vary widely; however, those with severe COVID-19 illness typically have significant respiratory compromise 2-5 . Several risk factors for both susceptibility of infection and clinical outcomes have been proposed, including age greater than 65, diabetes, coronary artery disease and chronic obstructive pulmonary disorder (COPD) placing individuals at increased risk 6,7 . Additionally, proton pump inhibitor (PPI) use has been identified as a possible risk factor for increased severity for COVID-19 infection, yet this association has not been extensively studied. PPIs are one of the most common classes of medications prescribed in the US 8 . Their use however has been associated with increased risk of infections including pneumonia, Clostridium difficle and spontaneous bacterial peritonitis [9] [10] [11] [12] [13] . It is postulated that these infections may occur due to a decrease in gastric acid leading to a disruption of gut flora 9 . Studies evaluating the relationship between the severity of COVID-19 infection and PPI therapy are emerging, but the relationship is not well established...
Author contributions B.S.: Acquisition of data, interpretation/analysis of data, draft and substantive revision of manuscript. S.M.: Conception Acquisition of data, interpretation/analysis of data, draft manuscript. S.C.: Acquisition of data, interpretation/analysis of data, draft manuscript. N.P.: Acquisition of data, interpretation/analysis of data, draft manuscript. M.A.: Acquisition of data, interpretation/analysis of data, drafting of manuscript. JA.S.: Acquisition of data. JI.S.: Interpretation of data, drafting of manuscript. Y.S.: Conception of study, substantive revision of manuscript, approval of the submitted version of manuscript. All the above authors agree to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work.
Competing interests The authors declare no competing interests.
References
Almario, Chey, Spiegel, Increased risk of COVID-19 among users of proton pump inhibitors, Am. J. Gastroenterol
Almario, Chey, Spiegel, Increased risk of COVID-19 among users of proton pump inhibitors, Am. J. Gastroenterol
Bavishi, Dupont, Systematic review: the use of proton pump inhibitors and increased susceptibility to enteric infection, Aliment. Pharmacol. Ther
Bavishi, Dupont, Systematic review: the use of proton pump inhibitors and increased susceptibility to enteric infection, Aliment. Pharmacol. Ther, doi:10.1111/j.1365-2036.2011.04874.x
Cunningham, Proton pump inhibitors as a risk factor for Clostridium difficile diarrhoea, J. Hosp. Infect
Dalan, The ACE-2 in COVID-19: foe or friend?, Horm. Metab. Res
Darnell, Subbarao, Feinstone, Taylor, Inactivation of the coronavirus that induces severe acute respiratory syndrome, SARS-CoV, J. Virol. Methods
Freitas, Napimoga, Donalisio, Assessing the severity of COVID-19, Epidemiologia e Serviços de Saúde
Gao, Obesity is a risk factor for greater COVID-19 severity, Diabetes Care
Kotfis, Skonieczna-Żydecka, COVID-19: gastrointestinal symptoms and potential sources of SARS-CoV-2 transmission, Anaesthesiol. Intensive Ther
Lee, Ha, Yeniova, Severe clinical outcomes of COVID-19 associated with proton pump inhibitors: a nationwide cohort study with propensity score matching, GUT
Leonard, Marshall, Moayyedi, Systematic review of the risk of enteric infection in patients taking acid suppression, Am. J. Gastroenterol
Lo, Chan, Proton pump inhibitor use and the risk of small intestinal bacterial overgrowth: a meta-analysis, Clin. Gastroenterol. Hepatol
Lo, Chan, Proton pump inhibitor use and the risk of small intestinal bacterial overgrowth: a meta-analysis, Clin. Gastroenterol. Hepatol, doi:10.1016/j.cgh.2012.12.011
Luxenburger, Treatment with proton pump inhibitors increases the risk of secondary infections and ARDS in hospitalized patients with COVID-19: coincidence or underestimated risk factor?, J. Intern. Med, doi:10.1111/joim.13121
Macera, De Angelis, Sagnelli, Coppola, Covid, Clinical presentation of COVID-19: case series and review of the literature, Int. J. Environ. Res. Public Health
Moayyedi, Safety of proton pump inhibitors based on a large, multi-year, randomized trial of patients receiving rivaroxaban or aspirin, Gastroenterology
Neal, Scott, Slack, Logan, Omeprazole as a risk factor for campylobacter gastroenteritis: case-control study, BMJ
Ng, Tilg, COVID-19 and the gastrointestinal tract: more than meets the eye, Gut
Parohan, Risk factors for mortality in patients with Coronavirus disease 2019 (COVID-19) infection: a systematic review and meta-analysis of observational studies, Aging Male, doi:10.1080/13685538.2020.1774748
Pranata, Body mass index and outcome in patients with COVID-19: a dose-response meta-analysis, Diabetes Metab
Pranata, Proton pump inhibitor on susceptibility to COVID-19 and its severity: a systematic review and meta-analysis, Pharmacol. Rep
Ramachandran, Perisetti, Gajendran, Jean-Louise, Dwivedi et al., Prehospitalization proton pump inhibitor (PPI) use and clinical outcomes in COVID-19, medRxiv
Schumock, National trends in prescription drug expenditures and projections for 2016, Am. J. Health Syst. Pharm
Tarlow, Gubatan, Khan, Cholankeril, Are proton pump inhibitors contributing to SARS-COV-2 infection?, Am. J. Gastroenterol
Vaezi, Yang, Howden, Complications of proton pump inhibitor therapy, Gastroenterology
Vilcu, Association between acute gastroenteritis and continuous use of proton pump inhibitors during winter periods of highest circulation of enteric viruses, JAMA Netw. Open, doi:10.1001/jamanetworkopen.2019.16205
Wu, Mcgoogan, Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention, JAMA
Xiao, Evidence for gastrointestinal infection of SARSCoV-2, Gastroenterology
Zhou, Proton pump inhibitor or famotidine use and severe COVID-19 disease: a propensity score-matched territory-wide study, doi:10.1136/gutjnl-2020-323668
DOI record:
{
"DOI": "10.1038/s41598-022-11680-0",
"ISSN": [
"2045-2322"
],
"URL": "http://dx.doi.org/10.1038/s41598-022-11680-0",
"abstract": "<jats:title>Abstract</jats:title><jats:p>Proton Pump Inhibitors (PPI) are one of the most prescribed medications in the United States. However, PPIs have been shown to increase the risk of enteric infections. Our study aims to evaluate the correlation between PPI and COVID-19 severity. We performed a retrospective cohort study on patients who tested positive for SARS-CoV-2 from March to August 2020. Patients were categorized based on PPI user status. Primary outcomes included need for hospital or ICU admission and 30-day mortality. Secondary outcomes looked to determine the severity of COVID-19 infection and effect of comorbid conditions. 2,594 patients were reviewed. The primary outcomes of our study found that neither active nor past PPI use was associated with increased hospital admission or 30-day mortality following completion of multivariate analysis. Additionally, there was no association between COVID-19 infection and the strength of PPI dosing (low, standard, high). However, the following covariates were independently and significantly associated with increased admission: age, male gender, diabetes, COPD, composite cardiovascular disease, kidney disease, and obesity. The following covariates were associated with increased mortality: age, male gender, COPD, and kidney disease. In conclusion, the high risk features and comorbidities of PPI users were found to have a stronger correlation to severe COVID-19 infection and poor outcomes as opposed to the use of PPI therapy.</jats:p>",
"alternative-id": [
"11680"
],
"article-number": "7596",
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "19 November 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "12 April 2022"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "9 May 2022"
},
{
"group": {
"label": "Competing interests",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1,
"value": "The authors declare no competing interests."
}
],
"author": [
{
"affiliation": [],
"family": "Shupp",
"given": "Brittney",
"sequence": "first"
},
{
"affiliation": [],
"family": "Mehta",
"given": "Sagar V.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chirayath",
"given": "Subin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Patel",
"given": "Nishit",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Aiad",
"given": "Mina",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sapin",
"given": "Jared",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Stoltzfus",
"given": "Jill",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Schneider",
"given": "Yecheskel",
"sequence": "additional"
}
],
"container-title": "Scientific Reports",
"container-title-short": "Sci Rep",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2022,
5,
9
]
],
"date-time": "2022-05-09T17:23:40Z",
"timestamp": 1652117020000
},
"deposited": {
"date-parts": [
[
2022,
11,
25
]
],
"date-time": "2022-11-25T02:36:49Z",
"timestamp": 1669343809000
},
"indexed": {
"date-parts": [
[
2024,
7,
18
]
],
"date-time": "2024-07-18T09:54:04Z",
"timestamp": 1721296444119
},
"is-referenced-by-count": 8,
"issue": "1",
"issued": {
"date-parts": [
[
2022,
5,
9
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2022,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
5,
9
]
],
"date-time": "2022-05-09T00:00:00Z",
"timestamp": 1652054400000
}
},
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
5,
9
]
],
"date-time": "2022-05-09T00:00:00Z",
"timestamp": 1652054400000
}
}
],
"link": [
{
"URL": "https://www.nature.com/articles/s41598-022-11680-0.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.nature.com/articles/s41598-022-11680-0",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.nature.com/articles/s41598-022-11680-0.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1038",
"published": {
"date-parts": [
[
2022,
5,
9
]
]
},
"published-online": {
"date-parts": [
[
2022,
5,
9
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"key": "11680_CR1",
"unstructured": "“CDC COVID Data Tracker.” Centers for disease control and prevention. covid.cdc.gov/covid-data-tracker/ (2020)."
},
{
"DOI": "10.3390/ijerph17145062",
"author": "M Macera",
"doi-asserted-by": "publisher",
"first-page": "5062",
"issue": "14",
"journal-title": "Int. J. Environ. Res. Public Health.",
"key": "11680_CR2",
"unstructured": "Macera, M., De Angelis, G., Sagnelli, C., Coppola, N. & COVID, V. Clinical presentation of COVID-19: case series and review of the literature. Int. J. Environ. Res. Public Health. 17(14), 5062 (2020).",
"volume": "17",
"year": "2020"
},
{
"author": "AR Freitas",
"first-page": "e2020119",
"issue": "29",
"journal-title": "Epidemiologia e Serviços de Saúde.",
"key": "11680_CR3",
"unstructured": "Freitas, A. R., Napimoga, M. & Donalisio, M. R. Assessing the severity of COVID-19. Epidemiologia e Serviços de Saúde. 6(29), e2020119 (2020).",
"volume": "6",
"year": "2020"
},
{
"DOI": "10.5114/ait.2020.93867",
"author": "K Kotfis",
"doi-asserted-by": "publisher",
"first-page": "171",
"issue": "2",
"journal-title": "Anaesthesiol. Intensive Ther.",
"key": "11680_CR4",
"unstructured": "Kotfis, K. & Skonieczna-Żydecka, K. COVID-19: gastrointestinal symptoms and potential sources of SARS-CoV-2 transmission. Anaesthesiol. Intensive Ther. 52(2), 171 (2020).",
"volume": "52",
"year": "2020"
},
{
"DOI": "10.1136/gutjnl-2020-321195",
"author": "SC Ng",
"doi-asserted-by": "publisher",
"first-page": "973",
"issue": "6",
"journal-title": "Gut",
"key": "11680_CR5",
"unstructured": "Ng, S. C. & Tilg, H. COVID-19 and the gastrointestinal tract: more than meets the eye. Gut 69(6), 973–974 (2020).",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.2648",
"author": "Z Wu",
"doi-asserted-by": "publisher",
"first-page": "1239",
"journal-title": "JAMA",
"key": "11680_CR6",
"unstructured": "Wu, Z. & McGoogan, J. M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA 323, 1239 (2020).",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1080/13685538.2020.1774748",
"author": "M Parohan",
"doi-asserted-by": "publisher",
"journal-title": "Aging Male",
"key": "11680_CR7",
"unstructured": "Parohan, M. et al. Risk factors for mortality in patients with Coronavirus disease 2019 (COVID-19) infection: a systematic review and meta-analysis of observational studies. Aging Male https://doi.org/10.1080/13685538.2020.1774748 (2020).",
"year": "2020"
},
{
"DOI": "10.2146/ajhp160205",
"author": "GT Schumock",
"doi-asserted-by": "publisher",
"first-page": "1058",
"journal-title": "Am. J. Health Syst. Pharm.",
"key": "11680_CR8",
"unstructured": "Schumock, G. T. et al. National trends in prescription drug expenditures and projections for 2016. Am. J. Health Syst. Pharm. 73, 1058–1075 (2016).",
"volume": "73",
"year": "2016"
},
{
"DOI": "10.1053/j.gastro.2017.04.047",
"author": "MF Vaezi",
"doi-asserted-by": "publisher",
"first-page": "35",
"journal-title": "Gastroenterology",
"key": "11680_CR9",
"unstructured": "Vaezi, M. F., Yang, Y. X. & Howden, C. W. Complications of proton pump inhibitor therapy. Gastroenterology 153, 35–48 (2017).",
"volume": "153",
"year": "2017"
},
{
"DOI": "10.1016/S0195-6701(03)00088-4",
"author": "R Cunningham",
"doi-asserted-by": "publisher",
"first-page": "243",
"issue": "3",
"journal-title": "J. Hosp. Infect.",
"key": "11680_CR10",
"unstructured": "Cunningham, R. et al. Proton pump inhibitors as a risk factor for Clostridium difficile diarrhoea. J. Hosp. Infect. 54(3), 243–245 (2003).",
"volume": "54",
"year": "2003"
},
{
"DOI": "10.1016/j.cgh.2012.12.011",
"author": "WK Lo",
"doi-asserted-by": "publisher",
"first-page": "483",
"journal-title": "Clin. Gastroenterol. Hepatol.",
"key": "11680_CR11",
"unstructured": "Lo, W. K. & Chan, W. W. Proton pump inhibitor use and the risk of small intestinal bacterial overgrowth: a meta-analysis. Clin. Gastroenterol. Hepatol. 11, 483–490 (2013).",
"volume": "11",
"year": "2013"
},
{
"DOI": "10.1111/j.1572-0241.2007.01275.x",
"author": "J Leonard",
"doi-asserted-by": "publisher",
"first-page": "2047",
"journal-title": "Am. J. Gastroenterol.",
"key": "11680_CR12",
"unstructured": "Leonard, J., Marshall, J. K. & Moayyedi, P. Systematic review of the risk of enteric infection in patients taking acid suppression. Am. J. Gastroenterol. 102, 2047–2056 (2007).",
"volume": "102",
"year": "2007"
},
{
"DOI": "10.1111/j.1365-2036.2011.04874.x",
"author": "C Bavishi",
"doi-asserted-by": "publisher",
"first-page": "1269",
"journal-title": "Aliment. Pharmacol. Ther.",
"key": "11680_CR13",
"unstructured": "Bavishi, C. & DuPont, H. L. Systematic review: the use of proton pump inhibitors and increased susceptibility to enteric infection. Aliment. Pharmacol. Ther. 34, 1269–1281 (2011).",
"volume": "34",
"year": "2011"
},
{
"key": "11680_CR14",
"unstructured": "Gastro-esophageal reflux disease and dyspepsia in adults: investigation and management. National Institute for Health and Clinical Excellence. [updated 18 October 2019; cited 15 June 2020]; https://www.nice.org.uk/guidance/cg184 (2014)."
},
{
"DOI": "10.14309/ajg.0000000000000798",
"author": "CV Almario",
"doi-asserted-by": "publisher",
"first-page": "1707",
"journal-title": "Am. J. Gastroenterol.",
"key": "11680_CR15",
"unstructured": "Almario, C. V., Chey, W. D. & Spiegel, B. M. Increased risk of COVID-19 among users of proton pump inhibitors. Am. J. Gastroenterol. 115, 1707–1715 (2020).",
"volume": "115",
"year": "2020"
},
{
"DOI": "10.1053/j.gastro.2019.05.056",
"author": "P Moayyedi",
"doi-asserted-by": "publisher",
"first-page": "682",
"issue": "3",
"journal-title": "Gastroenterology",
"key": "11680_CR16",
"unstructured": "Moayyedi, P. et al. Safety of proton pump inhibitors based on a large, multi-year, randomized trial of patients receiving rivaroxaban or aspirin. Gastroenterology 157(3), 682–691 (2019).",
"volume": "157",
"year": "2019"
},
{
"DOI": "10.1136/bmj.312.7028.414",
"author": "KR Neal",
"doi-asserted-by": "publisher",
"first-page": "414",
"issue": "7028",
"journal-title": "BMJ",
"key": "11680_CR17",
"unstructured": "Neal, K. R., Scott, H. M., Slack, R. C. & Logan, R. F. Omeprazole as a risk factor for campylobacter gastroenteritis: case-control study. BMJ 312(7028), 414–415 (1996).",
"volume": "312",
"year": "1996"
},
{
"DOI": "10.1111/j.1365-2036.2011.04874.x",
"author": "C Bavishi",
"doi-asserted-by": "publisher",
"first-page": "1269",
"issue": "11–12",
"journal-title": "Aliment. Pharmacol. Ther.",
"key": "11680_CR18",
"unstructured": "Bavishi, C. & Dupont, H. L. Systematic review: the use of proton pump inhibitors and increased susceptibility to enteric infection. Aliment. Pharmacol. Ther. 34(11–12), 1269–1281. https://doi.org/10.1111/j.1365-2036.2011.04874.x (2011) (Epub 2011 Oct 17 PMID: 21999643).",
"volume": "34",
"year": "2011"
},
{
"DOI": "10.1016/j.cgh.2012.12.011",
"author": "WK Lo",
"doi-asserted-by": "publisher",
"first-page": "483",
"issue": "5",
"journal-title": "Clin. Gastroenterol. Hepatol.",
"key": "11680_CR19",
"unstructured": "Lo, W. K. & Chan, W. W. Proton pump inhibitor use and the risk of small intestinal bacterial overgrowth: a meta-analysis. Clin. Gastroenterol. Hepatol. 11(5), 483–490. https://doi.org/10.1016/j.cgh.2012.12.011 (2013) (Epub 2012 Dec 24 PMID: 23270866).",
"volume": "11",
"year": "2013"
},
{
"DOI": "10.1016/j.jviromet.2004.06.006",
"author": "ME Darnell",
"doi-asserted-by": "publisher",
"first-page": "85",
"issue": "1",
"journal-title": "J. Virol. Methods",
"key": "11680_CR20",
"unstructured": "Darnell, M. E., Subbarao, K., Feinstone, S. M. & Taylor, D. R. Inactivation of the coronavirus that induces severe acute respiratory syndrome, SARS-CoV. J. Virol. Methods 121(1), 85–91 (2004).",
"volume": "121",
"year": "2004"
},
{
"DOI": "10.1001/jamanetworkopen.2019.16205",
"author": "AM Vilcu",
"doi-asserted-by": "publisher",
"first-page": "e1916205",
"issue": "11",
"journal-title": "JAMA Netw. Open",
"key": "11680_CR21",
"unstructured": "Vilcu, A. M. et al. Association between acute gastroenteritis and continuous use of proton pump inhibitors during winter periods of highest circulation of enteric viruses. JAMA Netw. Open 2(11), e1916205. https://doi.org/10.1001/jamanetworkopen.2019.16205 (2019) (PMID:31774521;PMCID:PMC6902831).",
"volume": "2",
"year": "2019"
},
{
"DOI": "10.1053/j.gastro.2020.02.055",
"author": "F Xiao",
"doi-asserted-by": "publisher",
"first-page": "1831",
"issue": "6",
"journal-title": "Gastroenterology",
"key": "11680_CR22",
"unstructured": "Xiao, F. et al. Evidence for gastrointestinal infection of SARSCoV-2. Gastroenterology 158(6), 1831–1833 (2020).",
"volume": "158",
"year": "2020"
},
{
"author": "R Dalan",
"first-page": "25",
"issue": "5",
"journal-title": "Horm. Metab. Res.",
"key": "11680_CR23",
"unstructured": "Dalan, R. et al. The ACE-2 in COVID-19: foe or friend?. Horm. Metab. Res. 52(5), 25 (2020).",
"volume": "52",
"year": "2020"
},
{
"DOI": "10.1136/gutjnl-2020-322248",
"doi-asserted-by": "crossref",
"key": "11680_CR24",
"unstructured": "Lee, S. W., Ha, E.K., Yeniova, A. Ö., et al. Severe clinical outcomes of COVID-19 associated with proton pump inhibitors: a nationwide cohort study with propensity score matching. GUT 0: 1–9 (2020)."
},
{
"DOI": "10.1016/j.diabet.2020.07.005",
"author": "R Pranata",
"doi-asserted-by": "publisher",
"first-page": "101178",
"issue": "2",
"journal-title": "Diabetes Metab.",
"key": "11680_CR25",
"unstructured": "Pranata, R. et al. Body mass index and outcome in patients with COVID-19: a dose–response meta-analysis. Diabetes Metab. 47(2), 101178 (2021).",
"volume": "47",
"year": "2021"
},
{
"DOI": "10.2337/dc20-0682",
"author": "F Gao",
"doi-asserted-by": "publisher",
"first-page": "e72",
"issue": "7",
"journal-title": "Diabetes Care",
"key": "11680_CR26",
"unstructured": "Gao, F. et al. Obesity is a risk factor for greater COVID-19 severity. Diabetes Care 43(7), e72–e74 (2020).",
"volume": "43",
"year": "2020"
},
{
"author": "R Pranata",
"first-page": "1",
"journal-title": "Pharmacol. Rep.",
"key": "11680_CR27",
"unstructured": "Pranata, R. et al. Proton pump inhibitor on susceptibility to COVID-19 and its severity: a systematic review and meta-analysis. Pharmacol. Rep. 11, 1–8 (2021).",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1101/2020.07.12.20151084",
"doi-asserted-by": "crossref",
"key": "11680_CR28",
"unstructured": "Ramachandran, P., Perisetti, A., Gajendran, M., Jean-Louise, F., Dwivedi, A. K., Goyal, H. Prehospitalization proton pump inhibitor (PPI) use and clinical outcomes in COVID-19. medRxiv (2020)"
},
{
"DOI": "10.1111/joim.13121",
"author": "H Luxenburger",
"doi-asserted-by": "publisher",
"first-page": "121",
"journal-title": "J. Intern. Med.",
"key": "11680_CR29",
"unstructured": "Luxenburger, H. et al. Treatment with proton pump inhibitors increases the risk of secondary infections and ARDS in hospitalized patients with COVID-19: coincidence or underestimated risk factor?. J. Intern. Med. 289, 121–124. https://doi.org/10.1111/joim.13121 (2021).",
"volume": "289",
"year": "2021"
},
{
"DOI": "10.1136/gutjnl-2020-323668",
"author": "J Zhou",
"doi-asserted-by": "publisher",
"journal-title": "Gut",
"key": "11680_CR30",
"unstructured": "Zhou, J. et al. Proton pump inhibitor or famotidine use and severe COVID-19 disease: a propensity score-matched territory-wide study. Gut https://doi.org/10.1136/gutjnl-2020-323668 (2020).",
"year": "2020"
},
{
"DOI": "10.14309/ajg.0000000000000798",
"author": "CV Almario",
"doi-asserted-by": "publisher",
"first-page": "1707",
"journal-title": "Am. J. Gastroenterol.",
"key": "11680_CR31",
"unstructured": "Almario, C. V., Chey, W. D. & Spiegel, B. M. Increased risk of COVID-19 among users of proton pump inhibitors. Am. J. Gastroenterol. 115, 1707–1715 (2020).",
"volume": "115",
"year": "2020"
},
{
"DOI": "10.14309/ajg.0000000000000933",
"author": "B Tarlow",
"doi-asserted-by": "publisher",
"first-page": "1920",
"journal-title": "Am. J. Gastroenterol.",
"key": "11680_CR32",
"unstructured": "Tarlow, B., Gubatan, J., Khan, M. A. & Cholankeril, G. Are proton pump inhibitors contributing to SARS-COV-2 infection?. Am. J. Gastroenterol. 115, 1920–1921 (2020).",
"volume": "115",
"year": "2020"
},
{
"DOI": "10.15585/mmwr.mm6912e2",
"author": "S Bialek",
"doi-asserted-by": "publisher",
"first-page": "343",
"issue": "12",
"journal-title": "Morb. Mortal. Wkly. Rep.",
"key": "11680_CR33",
"unstructured": "CDC COVID-19 Response Team et al. (2020) Severe outcomes among patients with coronavirus disease 2019 (COVID-19)—United States 15 February 12–March 16. Morb. Mortal. Wkly. Rep. 69(12), 343–346 (2020).",
"volume": "69",
"year": "2020"
}
],
"reference-count": 33,
"references-count": 33,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.nature.com/articles/s41598-022-11680-0"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Proton pump inhibitor therapy usage and associated hospitalization rates and critical care outcomes of COVID-19 patients",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "12"
}