Tixagevimab-cilgavimab (AZD7442) for the treatment of patients hospitalized with COVID-19 (DisCoVeRy): a phase 3, randomized, double-blind, placebo-controlled trial
et al., Journal of Infection, doi:10.1016/j.jinf.2024.106120, DisCoVeRy, NCT04315948, Feb 2024
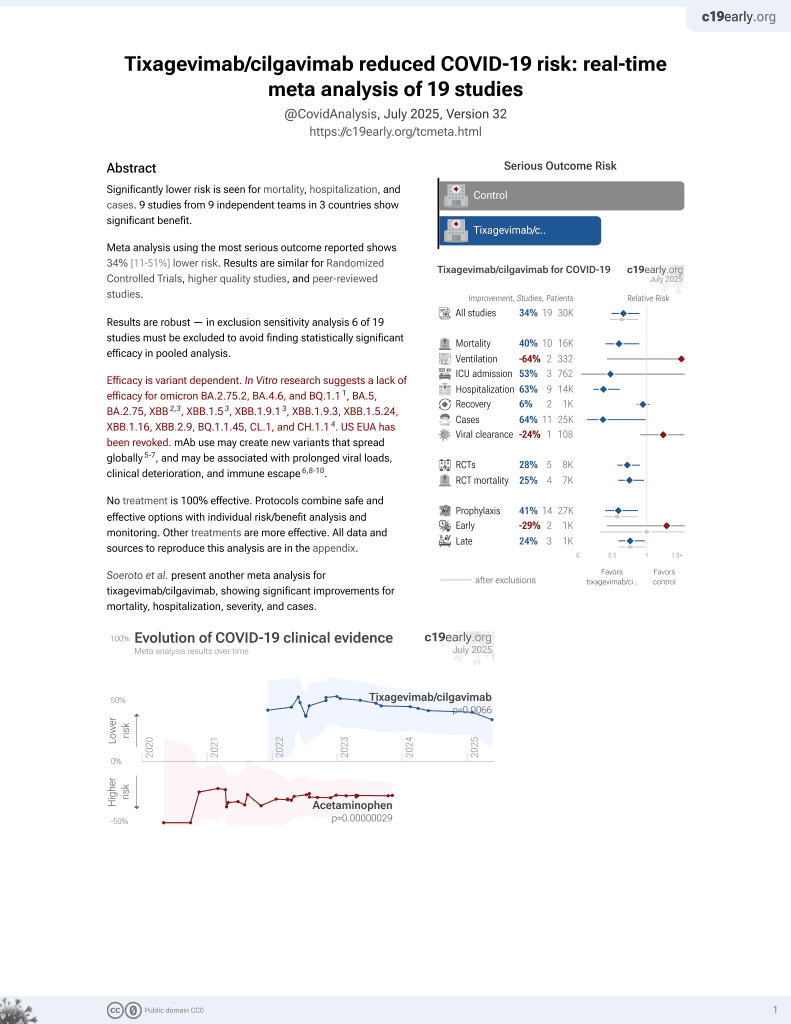
42nd treatment shown to reduce risk in
May 2022, now with p = 0.0066 from 19 studies, recognized in 33 countries.
Efficacy is variant dependent.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
RCT 173 hospitalized COVID-19 patients showing no significant difference in clinical status, time to recovery, viral clearance, or mortality with tixagevimab/cilgavimab. Mortality was lower, without statistical significance. The trial was terminated early due to concerns about reduced efficacy against circulating variants.
Efficacy is variant dependent. In Vitro research suggests a lack of efficacy for omicron BA.2.75.2, BA.4.6, BQ.1.11, BA.5, BA.2.75, XBB2,3, XBB.1.53, ХВВ.1.9.13, XBB.1.9.3, XBB.1.5.24, XBB.1.16, XBB.2.9, BQ.1.1.45, CL.1, and CH.1.14.
Although the 40% lower mortality is not statistically significant, it is consistent with the significant 40% lower mortality [11‑60%] from meta-analysis of the 10 mortality results to date.
|
risk of death, 39.9% lower, RR 0.60, p = 0.17, treatment 12 of 123 (9.8%), control 16 of 103 (15.5%), NNT 17, odds ratio converted to relative risk, day 90.
|
|
risk of 7-point scale, 17.6% higher, OR 1.18, p = 0.52, treatment 123, control 103, inverted to make OR<1 favor treatment, day 15, primary outcome, RR approximated with OR.
|
|
recovery time, 1.0% lower, relative time 0.99, p = 0.93, treatment 123, control 103, inverted to make RR<1 favor treatment.
|
|
time to discharge, 9.1% lower, relative time 0.91, p = 0.49, treatment 123, control 103, inverted to make RR<1 favor treatment.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Planas et al., Resistance of Omicron subvariants BA.2.75.2, BA.4.6 and BQ.1.1 to neutralizing antibodies, bioRxiv, doi:10.1101/2022.11.17.516888.
2.
Haars et al., Prevalence of SARS-CoV-2 Omicron Sublineages and Spike Protein Mutations Conferring Resistance against Monoclonal Antibodies in a Swedish Cohort during 2022–2023, Microorganisms, doi:10.3390/microorganisms11102417.
Hites et al., 16 Feb 2024, Double Blind Randomized Controlled Trial, placebo-controlled, France, peer-reviewed, 86 authors, trial NCT04315948 (history) (DisCoVeRy).
Contact: maya.hites@hubruxelles.be.
Abstract: Journal Pre-proof
Tixagevimab-cilgavimab (AZD7442) for the
treatment of patients hospitalized with COVID-19
(DisCoVeRy): a phase 3, randomized, doubleblind, placebo-controlled trial
Maya Hites
Clément R. Massonnaud
Simon Jamard
François Goehringer
François Danion
Jean Reignier
Nathalie de Castro
Denis Garot
Eva Larranaga Lapique
Karine Lacombe
Violaine Tolsma
Emmanuel Faure
Denis Malvy
Thérèse Staub
Johan Courjon
France Cazenave-Roblot
Anne Ma Dyrhol Riise
Paul Leturnier
Guillaume Martin-Blondel
Claire Roger
Karolina Akinosoglou
Vincent Le Moing
Lionel Piroth
Pierre Sellier
Xavier Lescure
Marius Trøseid
Philippe Clevenbergh
Olav Dalgard
Sébastien Gallien
Marie Gousseff
Paul Loubet
Fanny Vardon-Bounes
Clotilde Visée
Leila Belkhir
Élisabeth Botelho-Nevers
André Cabié
Anastasia Kotanidou
Fanny Lanternier
Elisabeth Rouveix-Nordon
Susana Silva
Guillaume Thiery
Pascal Poignard
Guislaine Carcelain
Alpha Diallo, Noémie Mercier, Vida Terzic
Maude
Bouscambert-Duchamp,
Alexandre
Gaymard
Mary-Anne Trabaud
Grégory Destras, Laurence Josset
Drifa Belhadi
Nicolas Billard
Jérémie Guedj
Thi-Hong-Lien Han
Sandrine Couffin-Cadiergues
Aline Dechanet
Christelle Delmas, Hélène Esperou
Claire Fougerou-Leurent
Soizic Le Mestre
Anabelle Métois
Marion Noret
Isabelle Bally, Sebastián Dergan-Dylon
Sarah Tubiana
Ouifiya Kalif
Nathalie Bergaud, Benjamin Leveau
Joe Eustace
Richard Greil
Edit Hajdu
Monika Halanova
Jose-Artur Paiva
Anna Piekarska
Jesus Rodriguez Baño
Kristian Tonby
Milan Trojánek
Sotirios Tsiodras
Serhat Unal
Charles Burdet
Dominique Costagliola
Yazdan Yazdanpanah
Nathan Peiffer-Smadja
France Mentré
Florence Ader
PII:
S0163-4453(24)00054-9
DOI:
https://doi.org/10.1016/j.jinf.2024.106120
Reference:
YJINF106120
To appear in: Journal of Infection
Accepted date: 8
Please cite this article as: Maya Hites, Clément R. Massonnaud, Simon Jamard,
François Goehringer, François Danion, Jean Reignier, Nathalie de Castro, Denis
Garot, Eva Larranaga Lapique, Karine Lacombe, Violaine Tolsma, Emmanuel
Faure, Denis Malvy, Thérèse Staub, Johan Courjon, France Cazenave-Roblot,
Anne Ma Dyrhol Riise, Paul Leturnier, Guillaume Martin-Blondel, Claire Roger,
Karolina Akinosoglou, Vincent Le Moing, Lionel Piroth, Pierre Sellier, Xavier
Lescure, Marius Trøseid, Philippe Clevenbergh, Olav Dalgard, Sébastien Gallien,
Marie Gousseff, Paul Loubet, Fanny Vardon-Bounes, Clotilde Visée, Leila
Belkhir, Élisabeth Botelho-Nevers, André Cabié, Anastasia Kotanidou, Fanny
Lanternier, Elisabeth Rouveix-Nordon, Susana Silva, Guillaume Thiery, Pascal
Poignard, Guislaine Carcelain, Alpha Diallo, Noémie Mercier, Vida Terzic,
Maude Bouscambert-Duchamp, Alexandre Gaymard, Mary-Anne Trabaud,
Grégory Destras, Laurence Josset, Drifa Belhadi, Nicolas Billard, Jérémie Guedj,
Thi-Hong-Lien Han, Sandrine Couffin-Cadiergues, Aline Dechanet, Christelle
Delmas, Hélène Esperou, Claire Fougerou-Leurent, Soizic Le Mestre, Anabelle
Métois, Marion Noret, Isabelle Bally, Sebastián Dergan-Dylon, Sarah Tubiana,
Ouifiya Kalif, Nathalie Bergaud, Benjamin Leveau, Joe Eustace, Richard Greil,
Edit Hajdu, Monika Halanova, Jose-Artur Paiva, Anna Piekarska, Jesus
Rodriguez Baño, Kristian Tonby, Milan Trojánek, Sotirios Tsiodras, Serhat
Unal, Charles Burdet, Dominique Costagliola, Yazdan Yazdanpanah, Nathan
Peiffer-Smadja, France Mentré and Florence Ader, Tixagevimab-cilgavimab
(AZD7442) for the treatment of patients hospitalized with COVID-19
(DisCoVeRy): a phase 3, randomized, double-blind, placebo-controlled..
DOI record:
{
"DOI": "10.1016/j.jinf.2024.106120",
"ISSN": [
"0163-4453"
],
"URL": "http://dx.doi.org/10.1016/j.jinf.2024.106120",
"alternative-id": [
"S0163445324000549"
],
"article-number": "106120",
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Tixagevimab-cilgavimab (AZD7442) for the treatment of patients hospitalized with COVID-19 (DisCoVeRy): a phase 3, randomized, double-blind, placebo-controlled trial"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Journal of Infection"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.jinf.2024.106120"
},
{
"label": "Content Type",
"name": "content_type",
"value": "simple-article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2024 Published by Elsevier Ltd on behalf of The British Infection Association."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0001-6961-6039",
"affiliation": [],
"authenticated-orcid": false,
"family": "Hites",
"given": "Maya",
"sequence": "first"
},
{
"affiliation": [],
"family": "Massonnaud",
"given": "Clément R.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jamard",
"given": "Simon",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Goehringer",
"given": "François",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3907-0658",
"affiliation": [],
"authenticated-orcid": false,
"family": "Danion",
"given": "François",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Reignier",
"given": "Jean",
"sequence": "additional"
},
{
"affiliation": [],
"family": "de Castro",
"given": "Nathalie",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Garot",
"given": "Denis",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lapique",
"given": "Eva Larranaga",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lacombe",
"given": "Karine",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tolsma",
"given": "Violaine",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Faure",
"given": "Emmanuel",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1948-9355",
"affiliation": [],
"authenticated-orcid": false,
"family": "Malvy",
"given": "Denis",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Staub",
"given": "Thérèse",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Courjon",
"given": "Johan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cazenave-Roblot",
"given": "France",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Riise",
"given": "Anne Ma Dyrhol",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Leturnier",
"given": "Paul",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Martin-Blondel",
"given": "Guillaume",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Roger",
"given": "Claire",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Akinosoglou",
"given": "Karolina",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Moing",
"given": "Vincent Le",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Piroth",
"given": "Lionel",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sellier",
"given": "Pierre",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lescure",
"given": "Xavier",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Trøseid",
"given": "Marius",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Clevenbergh",
"given": "Philippe",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4470-3181",
"affiliation": [],
"authenticated-orcid": false,
"family": "Dalgard",
"given": "Olav",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gallien",
"given": "Sébastien",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gousseff",
"given": "Marie",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Loubet",
"given": "Paul",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Vardon-Bounes",
"given": "Fanny",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Visée",
"given": "Clotilde",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1701-7584",
"affiliation": [],
"authenticated-orcid": false,
"family": "Belkhir",
"given": "Leila",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Botelho-Nevers",
"given": "Élisabeth",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cabié",
"given": "André",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kotanidou",
"given": "Anastasia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lanternier",
"given": "Fanny",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rouveix-Nordon",
"given": "Elisabeth",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Silva",
"given": "Susana",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Thiery",
"given": "Guillaume",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0021-7192",
"affiliation": [],
"authenticated-orcid": false,
"family": "Poignard",
"given": "Pascal",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Carcelain",
"given": "Guislaine",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Diallo",
"given": "Alpha",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mercier",
"given": "Noémie",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Terzic",
"given": "Vida",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bouscambert-Duchamp",
"given": "Maude",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8194-6126",
"affiliation": [],
"authenticated-orcid": false,
"family": "Gaymard",
"given": "Alexandre",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8614-1071",
"affiliation": [],
"authenticated-orcid": false,
"family": "Trabaud",
"given": "Mary-Anne",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Destras",
"given": "Grégory",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Josset",
"given": "Laurence",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Belhadi",
"given": "Drifa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Billard",
"given": "Nicolas",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Guedj",
"given": "Jérémie",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Han",
"given": "Thi-Hong-Lien",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Couffin-Cadiergues",
"given": "Sandrine",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dechanet",
"given": "Aline",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Delmas",
"given": "Christelle",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1654-4868",
"affiliation": [],
"authenticated-orcid": false,
"family": "Esperou",
"given": "Hélène",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-2736-6769",
"affiliation": [],
"authenticated-orcid": false,
"family": "Fougerou-Leurent",
"given": "Claire",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mestre",
"given": "Soizic Le",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Métois",
"given": "Anabelle",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Noret",
"given": "Marion",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8315-6080",
"affiliation": [],
"authenticated-orcid": false,
"family": "Bally",
"given": "Isabelle",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dergan-Dylon",
"given": "Sebastián",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tubiana",
"given": "Sarah",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kalif",
"given": "Ouifiya",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bergaud",
"given": "Nathalie",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Leveau",
"given": "Benjamin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Eustace",
"given": "Joe",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Greil",
"given": "Richard",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hajdu",
"given": "Edit",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9011-2238",
"affiliation": [],
"authenticated-orcid": false,
"family": "Halanova",
"given": "Monika",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Paiva",
"given": "Jose-Artur",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Piekarska",
"given": "Anna",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Baño",
"given": "Jesus Rodriguez",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tonby",
"given": "Kristian",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Trojánek",
"given": "Milan",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0463-4321",
"affiliation": [],
"authenticated-orcid": false,
"family": "Tsiodras",
"given": "Sotirios",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Unal",
"given": "Serhat",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Burdet",
"given": "Charles",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0765-0869",
"affiliation": [],
"authenticated-orcid": false,
"family": "Costagliola",
"given": "Dominique",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yazdanpanah",
"given": "Yazdan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Peiffer-Smadja",
"given": "Nathan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mentré",
"given": "France",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ader",
"given": "Florence",
"sequence": "additional"
}
],
"container-title": "Journal of Infection",
"container-title-short": "Journal of Infection",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.fr",
"clinicalkey.jp",
"clinicalkey.es",
"clinicalkey.com.au",
"clinicalkey.com",
"journalofinfection.com",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2024,
2,
16
]
],
"date-time": "2024-02-16T13:49:08Z",
"timestamp": 1708091348000
},
"deposited": {
"date-parts": [
[
2024,
2,
16
]
],
"date-time": "2024-02-16T13:49:15Z",
"timestamp": 1708091355000
},
"indexed": {
"date-parts": [
[
2024,
2,
17
]
],
"date-time": "2024-02-17T00:25:26Z",
"timestamp": 1708129526685
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2024,
2
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
2,
1
]
],
"date-time": "2024-02-01T00:00:00Z",
"timestamp": 1706745600000
}
},
{
"URL": "http://creativecommons.org/licenses/by-nc-nd/4.0/",
"content-version": "vor",
"delay-in-days": 8,
"start": {
"date-parts": [
[
2024,
2,
9
]
],
"date-time": "2024-02-09T00:00:00Z",
"timestamp": 1707436800000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S0163445324000549?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S0163445324000549?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "106120",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2024,
2
]
]
},
"published-print": {
"date-parts": [
[
2024,
2
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1016/j.jinf.2023.06.024",
"author": "Kamboj",
"doi-asserted-by": "crossref",
"first-page": "282",
"journal-title": "J Infection",
"key": "10.1016/j.jinf.2024.106120_bib1",
"volume": "87",
"year": "2023"
},
{
"DOI": "10.1016/S2213-2600(22)00180-1",
"article-title": "Efficacy and safety of intramuscular administration of tixagevimab–cilgavimab for early outpatient treatment of COVID-19 (TACKLE): a phase 3, randomised, double-blind, placebo-controlled trial",
"author": "Montgomery",
"doi-asserted-by": "crossref",
"first-page": "985",
"issue": "10",
"journal-title": "Lancet Respir Med",
"key": "10.1016/j.jinf.2024.106120_bib2",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.1016/S2213-2600(22)00215-6",
"article-title": "Tixagevimab–cilgavimab for treatment of patients hospitalised with COVID-19: a randomised, doubleblind, phase 3 trial",
"author": "Holland",
"doi-asserted-by": "crossref",
"first-page": "972",
"issue": "10",
"journal-title": "Lancet Respir Med",
"key": "10.1016/j.jinf.2024.106120_bib3",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.1038/s41579-022-00841-7",
"article-title": "SARS-CoV-2 variant biology: immune escape, transmission and fitness",
"author": "Carabelli",
"doi-asserted-by": "crossref",
"journal-title": "Nat Rev Microbiol [Internet]",
"key": "10.1016/j.jinf.2024.106120_bib4",
"year": "2023"
},
{
"DOI": "10.1016/j.isci.2023.106413",
"article-title": "Enhanced neutralization escape to therapeutic monoclonal antibodies by SARS-CoV-2 omicron sublineages",
"author": "Touret",
"doi-asserted-by": "crossref",
"issue": "4",
"journal-title": "iScience",
"key": "10.1016/j.jinf.2024.106120_bib5",
"volume": "26",
"year": "2023"
},
{
"DOI": "10.1056/NEJMc2207519",
"article-title": "Efficacy of Antibodies and Antiviral Drugs against Omicron BA.2.12.1, BA.4, and BA.5 Subvariants",
"author": "Takashita",
"doi-asserted-by": "crossref",
"first-page": "468",
"issue": "5",
"journal-title": "NEngl J Med",
"key": "10.1016/j.jinf.2024.106120_bib6",
"volume": "387",
"year": "2022"
},
{
"DOI": "10.1038/s41392-022-00997-x",
"article-title": "SARS-CoV-2 Omicron variant: recent progress and future perspectives",
"author": "Fan",
"doi-asserted-by": "crossref",
"first-page": "141",
"issue": "1",
"journal-title": "Signal Transduct Target Ther",
"key": "10.1016/j.jinf.2024.106120_bib7",
"volume": "7",
"year": "2022"
},
{
"key": "10.1016/j.jinf.2024.106120_bib8",
"unstructured": "European Medical Agency. Summary report of the Joint EMA-FDA workshop on the efficacy of monoclonal antibodies in the context of rapidly evolving SARS-CoV-2 variants [Internet]. [cited 2023 Nov 3]. Available from: 〈https://www.ema.europa.eu/en/documents/report/summary-report-joint-ema-fdaworkshop-efficacy-monoclonal-antibodies-context-rapidly-evolving-sars_en.pdf〉"
},
{
"key": "10.1016/j.jinf.2024.106120_bib9",
"unstructured": "European Centre for Disease Prevention and Control. SARS-CoV-2 variant mutations conferring reduced susceptibility to antiviral drugs and monoclonal antibodies: a non systematic literature review for surveillance purposes. [Internet]. LU: Publications Office; 2023 [cited 2023 Nov 3]. Available from: 〈https://data.europa.eu/doi/10.2900/192733〉"
},
{
"DOI": "10.1093/jac/dkac048",
"article-title": "Effect of remdesivir on viral dynamics in COVID-19 hospitalized patients: a modelling analysis of the randomized, controlled, open-label DisCoVeRy trial",
"author": "Lingas",
"doi-asserted-by": "crossref",
"first-page": "1404",
"issue": "5",
"journal-title": "J Antimicrob Chemother",
"key": "10.1016/j.jinf.2024.106120_bib10",
"volume": "77",
"year": "2022"
}
],
"reference-count": 10,
"references-count": 10,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S0163445324000549"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Infectious Diseases",
"Microbiology (medical)"
],
"subtitle": [],
"title": "Tixagevimab-cilgavimab (AZD7442) for the treatment of patients hospitalized with COVID-19 (DisCoVeRy): a phase 3, randomized, double-blind, placebo-controlled trial",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy"
}