Medications Associated with Lower Mortality in a SARS-CoV-2 Positive Cohort of 26,508 Veterans
et al., Journal of General Internal Medicine, doi:10.1007/s11606-022-07701-3, Jun 2022
Colchicine for COVID-19
5th treatment shown to reduce risk in
September 2020, now with p = 0.0000049 from 54 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
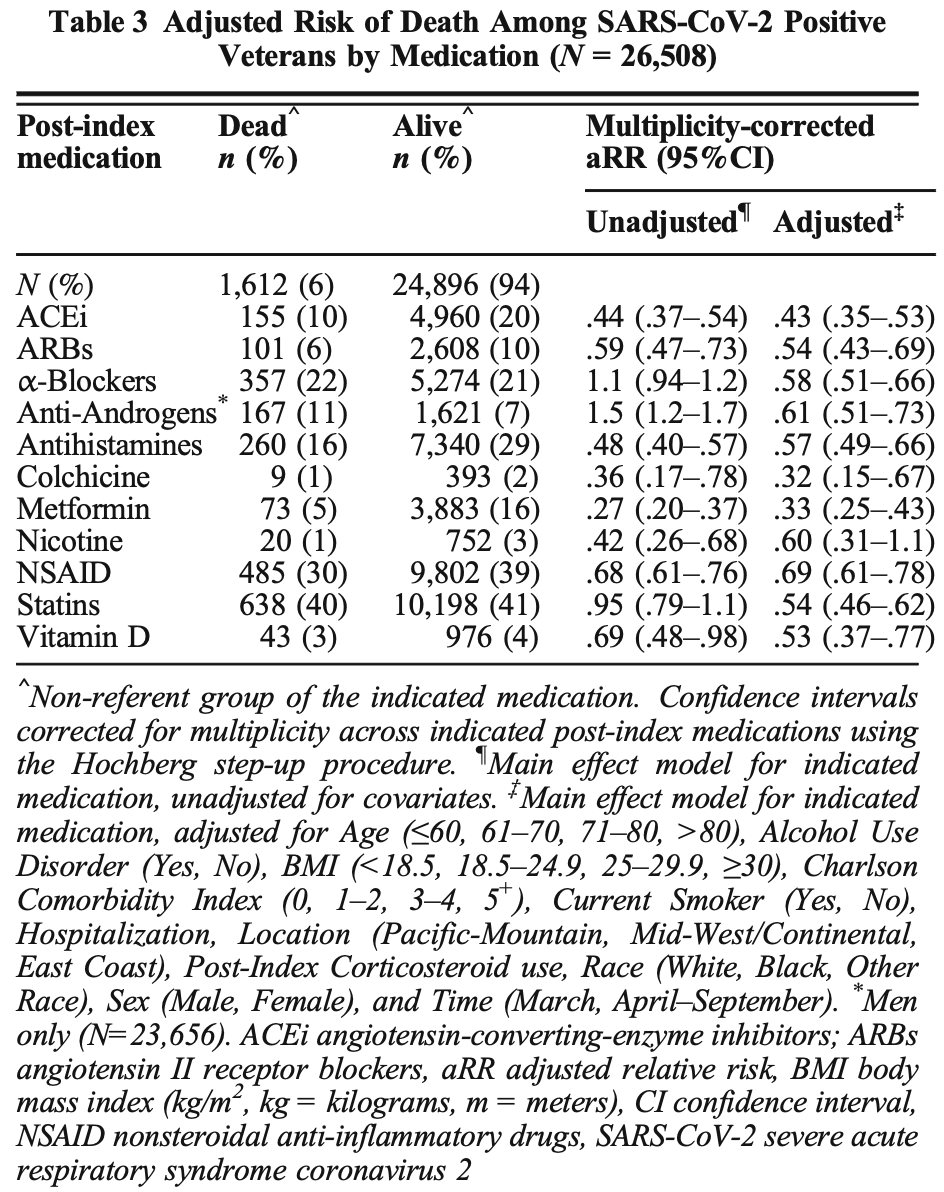
Retrospective 26,508 consecutive COVID+ veterans in the USA, showing lower mortality with multiple treatments including colchicine. Treatment was defined as drugs administered ≥50% of the time within 2 weeks post-COVID+, and may be a continuation of prophylactic treatment in some cases, and may be early or late treatment in other cases. Further reduction in mortality was seen with combinations of treatments.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
risk of death, 68.0% lower, RR 0.32, p = 0.003, treatment 9 of 402 (2.2%), control 1,603 of 26,106 (6.1%), NNT 26, adjusted per study, day 30.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Hunt et al., 29 Jun 2022, retrospective, USA, peer-reviewed, 8 authors, study period 1 March, 2020 - 10 September, 2020, dosage not specified.
Medications Associated with Lower Mortality in a SARS-CoV-2 Positive Cohort of 26,508 Veterans
Journal of General Internal Medicine, doi:10.1007/s11606-022-07701-3
BACKGROUND: Many severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) positive patients take commonly prescribed medications with properties which may affect mortality. OBJECTIVE: Assess if common medications postulated to affect clinical outcomes are associated with mortality in SARS-CoV-2 positive patients in the Veterans Health Administration (VHA). DESIGN: Observational national cohort analysis. PARTICIPANTS: Consecutive 26,508 SARS-CoV-2 positive Veterans (7% of 399,290 tested from March 1 to September 10, 2020) constitute the study cohort. MAIN MEASURES: The primary outcome was 30-day mortality from the first positive SARS-CoV-2 test date. In patients receiving medications or drug pairs within 2 weeks post-SARS-CoV-2 positive test, 30-day mortality was estimated as relative risk (RR) on the log-binomial scale or using multinomial models with and without adjusting for covariates. KEY RESULTS: The 26,508 SARS-CoV-2 positive patients were predominantly male (89%) and White (59%), and 82% were overweight/obese. Medications associated with decreased 30-day mortality risk included the following: metformin (aRR, 0.33; 95% CI, 0.25-0.43), colchicine, angiotensinconverting-enzyme inhibitors (ACEi), angiotensin II receptor blockers, statins, vitamin D, antihistamines, alpha-blockers, anti-androgens, and nonsteroidal anti-inflammatory drugs (aRR, 0.69; 95% CI, 0.61-0.78). The effect of co-prescribed medications on 30-day mortality risk revealed the lowest risk for combined statins and metformin (aRR, 0.21; 95% CI, 0.15-0.31), followed by ACEi and statins (aRR, 0.25; 95% CI, 0.18-0.35), ACEi and metformin (aRR, 0.26; 95% CI, 0.17-0.40), antihistamines and NSAIDs (aRR, 0.41; 95% CI, 0.32-0.52), and in men, combined alpha-blockers and antiandrogens (aRR, 0.51; 95% CI, 0.42-0.64). CONCLUSIONS: In this large national cohort, treatment of SARS-CoV-2 positive patients with individual or coprescribed metformin and statins, ACEi and statins (or metformin) and other medications was associated with a markedly decreased 30-day mortality and can likely be continued safely. Clinical trials may assess their therapeutic benefit.
Supplementary Information The online version contains supplementary material available at https://doi.org/10.1007/s11606-022-07701-3. Conflict of Interest: Dr. Hunt is a consultant to Akebia Therapeutics, Inc. Dr. Hostler is co-owner of Infection Control Education for Major Sports, LLC, and consultant for OneBeacon Insurance and Prime Education, LLC. Publisher's Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Baral, Tsampasian, Debski, Moran, Garg et al., Association between renin-angiotensin-aldosterone system inhibitors and clinical outcomes in patients with COVID-19: a systematic review and meta-analysis, JAMA Netw Open
Benjamini, Hochberg, Controlling the false discovery rate: a practical and powerful approach to multiple testing, J R Stat Soc Ser B Methodol
Benjamini, Yekutieli, False Discovery rate-adjusted multiple confidence intervals for selected parameters, J Am Stat Assoc
Bikdeli, Madhavan, Gupta, Jimenez, Burton et al., Pharmacological agents targeting thromboinflammation in COVID-19: review and implications for future research, Thromb Haemost
Bilaloglu, Aphinyanaphongs, Jones, Iturrate, Hochman et al., Thrombosis in Hospitalized Patients With COVID-19 in a New York City Health System, JAMA
Blanco, Bonilla, Homma, Suzuki, Smith et al., Antihistamines and azithromycin as a treatment for COVID-19 on primary health care -a retrospective observational study in elderly patients, Pulm Pharmacol Ther
Breslow, Day, Statistical methods in cancer research. Volume I -The analysis of case-control studies, IARC Sci Publ
Burton, Fort, Seoane, Hospitalization and mortality among Black patients and White patients with Covid-19, N Engl J Med
Cadegiani, Zimerman, Fonseca, Correia, Muller et al., Efficacy of proxalutamide in hospitalized COVID-19 patients: a randomized, double-blind, placebo-controlled, parallel-design clinical trial, Cureus
Cariou, Hadjadj, Wargny, Pichelin, Gourdy et al., Clinical characteristics and outcomes of patients with diabetes and COVID-19 in association with glucose-lowering medication, Diabetes Care
Chow, Khanna, Kethireddy, Yamane, Levine et al., Aspirin use is associated with decreased mechanical ventilation, ICU admission, and in-hospital mortality in hospitalized patients with COVID-19, Anesth Analg
Crouse, Grimes, Li, Might, Ovalle et al., Metformin use is associated with reduced mortality in a diverse population with COVID-19 and diabetes, Front Endocrinol
Deftereos, Siasos, Giannopoulos, Vrachatis, Angelidis et al., The Greek study in the effects of colchicine in COvid-19 complications prevention (GRECCO-19 study): Rationale and study design, Hell J Cardiol
Diabetes, Cardiovascular disease and risk management: standards of medical care in diabetes-2018, Diabetes Care
Diabetes, Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes-2018, Diabetes Care
Donnelly, Wang, Iwashyna, Prescott, Readmission and death after hospital discharge among patients with COVID-19 in a large multihospital system, JAMA
Efird, Goldilocks Rounding: achieving balance between accuracy and parsimony in the reporting of relative effect estimates, Cancer Informat
Efird, Nielsen, A method to compute multiplicity corrected confidence intervals for odds ratios and other relative effect estimates, Int J Environ Res Public Health
Farsalinos, Niaura, Houezec, Barbouni, Tsatsakis et al., Editorial: Nicotine and SARS-CoV-2: COVID-19 may be a disease of the nicotinic cholinergic system, Toxicol Rep
Gauthier, Lin, Wu, Kennedy, Daley et al., From nicotine to the cholinergic anti-inflammatory reflex -Can nicotine alleviate the dysregulated inflammation in COVID-19?, J Immunotoxicol
Gordon, Hiatt, Bouhaddou, Rezelj, Ulferts et al., Comparative host-coronavirus protein interaction networks reveal panviral disease mechanisms, Science
Group, Dexamethasone in hospitalized patients with Covid-19, N Engl J Med
Gupta, Madhavan, Poterucha, Defilippis, Hennessey et al., Association between antecedent statin use and decreased mortality in hospitalized patients with COVID-19, Nat Commun
Hochberg, A sharper Bonferroni procedure for multiple tests of significance, Biometrika
Ibrahim, Lowe, Bramante, Shah, Klatt et al., Metformin and Covid-19: focused review of mechanisms and current literature suggesting benefit, Front Endocrinol
Imam, Odish, Gill, Connor, Armstrong et al., Older age and comorbidity are independent mortality predictors in a large cohort of 1305 COVID-19 patients in Michigan, United States J Intern Med
Ioannou, Hare, Berry, Fan, Crothers et al., Trends over time in the risk of adverse outcomes among patients with SARS-CoV-2 infection, Clin Infect Dis, doi:10.1093/cid/ciab419
Ioannou, Locke, Green, Berry, Hare et al., Risk factors for hospitalization, mechanical ventilation, or death among 10 131 US Veterans with SARS-CoV-2 infection, JAMA Network Open
Jalili, Characteristics and Mortality of Hospitalized Patients With COVID-19 in Iran: A National Retrospective Cohort Study, Ann Intern Med
Karaca-Mandic, Georgiou, Sen, Assessment of COVID-19 hospitalizations by race/ethnicity in 12 states, JAMA Intern Med
Khunti, Knighton, Zaccardi, Bakhai, Barron et al., Prescription of glucose-lowering therapies and risk of COVID-19 mortality in people with type 2 diabetes: a nationwide observational study in England, Lancet Diabetes Endocrinol
Kong, Ye, Lin, Cai, Huang et al., Atorvastatin suppresses NLRP3 inflammasome activation via TLR4/MyD88/NF-κB signaling in PMA-stimulated THP-1 monocytes, Biomed Pharmacother
Konig, Powell, Staedtke, Bai, Thomas et al., Preventing cytokine storm syndrome in COVID-19 using α-1 adrenergic receptor antagonists, J Clin Invest
Kruskal, Historical notes on the wilcoxon unpaired two-sample test, J Am Stat Assoc
Luo, Qiu, Liu, Liu, Zheng et al., Metformin treatment was associated with decreased mortality in COVID-19 patients with diabetes in a retrospective analysis, Am J Trop Med Hyg
Moin, Damschroder, Youles, Makki, Billington, Implementation of a prediabetes identification algorithm for overweight and obese Veterans, J Rehabil Res Dev
Montopoli, Zumerle, Vettor, Rugge, Zorzi et al., Androgen-deprivation therapies for prostate cancer and risk of infection by SARS-CoV-2: a population-based study (N = 4532), Ann Oncol
Oran, Prevalence of asymptomatic SARS-CoV-2 infection, Ann Intern Med
Pal, Banerjee, Bhadada, Shetty, Singh et al., Vitamin D supplementation and clinical outcomes in COVID-19: a systematic review and meta-analysis, J Endocrinol Investig
Petrilli, Jones, Yang, Rajagopalan, Donnell et al., Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study, BMJ
Piazza, Morrow, Diagnosis, management, and pathophysiology of arterial and venous thrombosis in COVID-19, JAMA
Reznikov, Norris, Vashisht, Bluhm, Liao, Identification of antiviral antihistamines for COVID-19 repurposing, Biochem Biophys Res Commun
Rose, Graham, Koenecke, Powell, Xiong et al., The association between Alpha-1 adrenergic receptor antagonists and inhospital mortality from COVID-19, Front Med
Rosenthal, Cao, Gundrum, Sianis, Safo, Risk factors associated with in-hospital mortality in a US national sample of patients with COVID-19, JAMA Network Open
Rossotti, Travi, Ughi, Corradin, Baiguera et al., Safety and efficacy of anti-il6-receptor tocilizumab use in severe and critical patients affected by coronavirus disease 2019: a comparative analysis, J Infect
Scheen, Metformin and COVID-19: from cellular mechanisms to reduced mortality, Diabetes Metab
Sharma, Ray, Sadasivam, Metformin in COVID-19: a possible role beyond diabetes, Diabetes Res Clin Pract
Sohn, Maynard, Hynes, Accuracy and completeness of mortality data in the Department of Veterans Affairs, Popul Health Metrics
Suzuki, Efird, Tst, Thompson, Press et al., COVID-19-associated mortality in US Veterans with and without SARS-CoV-2 infection, Int J Environ Res Public Health
Tardif, Bouabdallaoui, Allier, Gaudet, Shah et al., Colchicine for community-treated patients with COVID-19 (COLCORONA): a phase 3, randomised, double-blinded, adaptive, placebo-controlled, multicentre trial, Lancet Respir Med
Thomsen, Christiansen, Heide-Jørgensen, Vogelstein, Vogelstein et al., Association of α1-blocker receipt with 30-day mortality and risk of intensive care unit admission among adults hospitalized with influenza or pneumonia in Denmark, JAMA Netw Open
Weidenbacher, Beadles, Maciejewski, Reeve, Voils, Extent and reasons for nonadherence to antihypertensive, cholesterol, and diabetes medications: the association with depressive symptom burden in a sample of American veterans, Patient Prefer Adherence
Williamson, Walker, Bhaskaran, Bacon, Bates et al., Factors associated with COVID-19-related death using OpenSAFELY, Nature
Wong, Mackenna, Morton, Schultze, Walker et al., Use of non-steroidal anti-inflammatory drugs and risk of death from COVID-19: an OpenSAFELY cohort analysis based on two cohorts, Ann Rheum Dis
Woolf, Chapman, Lee, COVID-19 as the leading cause of death in the United States, JAMA
Zhang, Qin, Cheng, Shen, Zhao et al., In-hospital use of statins is associated with a reduced risk of mortality among individuals with COVID-19, Cell Meta
DOI record:
{
"DOI": "10.1007/s11606-022-07701-3",
"ISSN": [
"0884-8734",
"1525-1497"
],
"URL": "http://dx.doi.org/10.1007/s11606-022-07701-3",
"alternative-id": [
"7701"
],
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "12 October 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "15 June 2022"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "29 June 2022"
},
{
"group": {
"label": "Declarations",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1
},
{
"group": {
"label": "Conflict of Interest",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "Dr. Hunt is a consultant to Akebia Therapeutics, Inc. Dr. Hostler is co-owner of Infection Control Education for Major Sports, LLC, and consultant for OneBeacon Insurance and Prime Education, LLC."
},
{
"label": "Free to read",
"name": "free",
"value": "This content has been made available to all."
}
],
"author": [
{
"affiliation": [],
"family": "Hunt",
"given": "Christine M.",
"sequence": "first"
},
{
"affiliation": [],
"family": "Efird",
"given": "Jimmy T.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Redding",
"given": "Thomas S.",
"sequence": "additional",
"suffix": "IV"
},
{
"affiliation": [],
"family": "Thompson",
"given": "Andrew D.",
"sequence": "additional",
"suffix": "Jr"
},
{
"affiliation": [],
"family": "Press",
"given": "Ashlyn M.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Williams",
"given": "Christina D.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hostler",
"given": "Christopher J.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1824-1067",
"affiliation": [],
"authenticated-orcid": false,
"family": "Suzuki",
"given": "Ayako",
"sequence": "additional"
}
],
"container-title": "Journal of General Internal Medicine",
"container-title-short": "J GEN INTERN MED",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2022,
6,
29
]
],
"date-time": "2022-06-29T19:02:47Z",
"timestamp": 1656529367000
},
"deposited": {
"date-parts": [
[
2022,
6,
30
]
],
"date-time": "2022-06-30T11:03:08Z",
"timestamp": 1656586988000
},
"funder": [
{
"DOI": "10.13039/100000738",
"doi-asserted-by": "publisher",
"name": "U.S. Department of Veterans Affairs"
}
],
"indexed": {
"date-parts": [
[
2022,
7,
1
]
],
"date-time": "2022-07-01T17:13:54Z",
"timestamp": 1656695634004
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
6,
29
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.springer.com/tdm",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
6,
29
]
],
"date-time": "2022-06-29T00:00:00Z",
"timestamp": 1656460800000
}
},
{
"URL": "https://www.springer.com/tdm",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
6,
29
]
],
"date-time": "2022-06-29T00:00:00Z",
"timestamp": 1656460800000
}
}
],
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1007/s11606-022-07701-3.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/article/10.1007/s11606-022-07701-3/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/content/pdf/10.1007/s11606-022-07701-3.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1007",
"published": {
"date-parts": [
[
2022,
6,
29
]
]
},
"published-online": {
"date-parts": [
[
2022,
6,
29
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1001/jama.2020.24865",
"author": "SH Woolf",
"doi-asserted-by": "publisher",
"first-page": "123",
"issue": "2",
"journal-title": "JAMA",
"key": "7701_CR1",
"unstructured": "Woolf SH, Chapman DA, Lee JH. COVID-19 as the leading cause of death in the United States. JAMA 2021;325(2):123-4.",
"volume": "325",
"year": "2021"
},
{
"DOI": "10.7326/M20-3012",
"author": "DP Oran",
"doi-asserted-by": "publisher",
"first-page": "362",
"issue": "5",
"journal-title": "Ann Intern Med",
"key": "7701_CR2",
"unstructured": "Oran DP. Prevalence of asymptomatic SARS-CoV-2 infection. Ann Intern Med 2020;173(5):362-7.",
"volume": "173",
"year": "2020"
},
{
"DOI": "10.1001/jamanetworkopen.2020.22310",
"author": "GN Ioannou",
"doi-asserted-by": "publisher",
"first-page": "e2022310-e",
"issue": "9",
"journal-title": "JAMA Network Open",
"key": "7701_CR3",
"unstructured": "Ioannou GN, Locke E, Green P, Berry K, O’Hare AM, Shah JA, et al. Risk factors for hospitalization, mechanical ventilation, or death among 10 131 US Veterans with SARS-CoV-2 infection. JAMA Network Open. 2020;3(9):e2022310-e.",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1056/NEJMsa2011686",
"doi-asserted-by": "crossref",
"key": "7701_CR4",
"unstructured": "Price-Haywood EG, Burton J, Fort D, Seoane L. Hospitalization and mortality among Black patients and White patients with Covid-19. N Engl J Med 2020;382(26):2534-43."
},
{
"DOI": "10.1001/jamainternmed.2020.3857",
"author": "P Karaca-Mandic",
"doi-asserted-by": "publisher",
"first-page": "131",
"issue": "1",
"journal-title": "JAMA Intern Med",
"key": "7701_CR5",
"unstructured": "Karaca-Mandic P, Georgiou A, Sen S. Assessment of COVID-19 hospitalizations by race/ethnicity in 12 states. JAMA Intern Med 2021;181(1):131-4.",
"volume": "181",
"year": "2021"
},
{
"author": "Group RC",
"first-page": "693",
"issue": "8",
"journal-title": "N Engl J Med",
"key": "7701_CR6",
"unstructured": "Group RC. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med 2020;384(8):693-704.",
"volume": "384",
"year": "2020"
},
{
"DOI": "10.1093/cid/ciab419",
"doi-asserted-by": "publisher",
"key": "7701_CR7",
"unstructured": "Ioannou GN, O'Hare AM, Berry K, Fan VS, Crothers K, Eastment MC, et al. Trends over time in the risk of adverse outcomes among patients with SARS-CoV-2 infection. Clin Infect Dis. 2021;ciab419. https://doi.org/10.1093/cid/ciab419."
},
{
"DOI": "10.1001/jama.2020.21465",
"author": "JP Donnelly",
"doi-asserted-by": "publisher",
"first-page": "304",
"issue": "3",
"journal-title": "JAMA.",
"key": "7701_CR8",
"unstructured": "Donnelly JP, Wang XQ, Iwashyna TJ, Prescott HC. Readmission and death after initial hospital discharge among patients with COVID-19 in a large multihospital system. JAMA. 2021;325(3):304-6.",
"volume": "325",
"year": "2021"
},
{
"DOI": "10.1001/jama.2020.23422",
"author": "G Piazza",
"doi-asserted-by": "publisher",
"first-page": "2548",
"issue": "24",
"journal-title": "JAMA.",
"key": "7701_CR9",
"unstructured": "Piazza G, Morrow DA. Diagnosis, management, and pathophysiology of arterial and venous thrombosis in COVID-19. JAMA. 2020;324(24):2548-9.",
"volume": "324",
"year": "2020"
},
{
"DOI": "10.1016/j.cmet.2020.06.015",
"author": "X-J Zhang",
"doi-asserted-by": "publisher",
"first-page": "176",
"issue": "2",
"journal-title": "Cell Meta",
"key": "7701_CR10",
"unstructured": "Zhang X-J, Qin J-J, Cheng X, Shen L, Zhao Y-C, Yuan Y, et al. In-hospital use of statins is associated with a reduced risk of mortality among individuals with COVID-19. Cell Meta. 2020;32(2):176-87.e4.",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.1001/jamanetworkopen.2020.29058",
"doi-asserted-by": "crossref",
"key": "7701_CR11",
"unstructured": "Rosenthal N, Cao Z, Gundrum J, Sianis J, Safo S. Risk factors associated with in-hospital mortality in a US national sample of patients with COVID-19. JAMA Network Open. 2020;3(12):e2029058-e."
},
{
"DOI": "10.1016/j.jinf.2020.07.008",
"author": "R Rossotti",
"doi-asserted-by": "publisher",
"first-page": "e11",
"issue": "4",
"journal-title": "J Infect",
"key": "7701_CR12",
"unstructured": "Rossotti R, Travi G, Ughi N, Corradin M, Baiguera C, Fumagalli R, et al. Safety and efficacy of anti-il6-receptor tocilizumab use in severe and critical patients affected by coronavirus disease 2019: a comparative analysis. J Infect 2020;81(4):e11-e7.",
"volume": "81",
"year": "2020"
},
{
"DOI": "10.1172/JCI139642",
"author": "MF Konig",
"doi-asserted-by": "publisher",
"first-page": "3345",
"issue": "7",
"journal-title": "J Clin Invest",
"key": "7701_CR13",
"unstructured": "Konig MF, Powell M, Staedtke V, Bai R-Y, Thomas DL, Fischer N, et al. Preventing cytokine storm syndrome in COVID-19 using α-1 adrenergic receptor antagonists. J Clin Invest 2020;130(7):3345-3347.",
"volume": "130",
"year": "2020"
},
{
"DOI": "10.1001/jamanetworkopen.2020.37053",
"author": "RW Thomsen",
"doi-asserted-by": "publisher",
"first-page": "e2037053",
"issue": "2",
"journal-title": "JAMA Netw Open",
"key": "7701_CR14",
"unstructured": "Thomsen RW, Christiansen CF, Heide-Jørgensen U, Vogelstein JT, Vogelstein B, Bettegowda C, et al. Association of α1-blocker receipt with 30-day mortality and risk of intensive care unit admission among adults hospitalized with influenza or pneumonia in Denmark. JAMA Netw Open 2021;4(2):e2037053.",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1001/jama.2020.13372",
"author": "S Bilaloglu",
"doi-asserted-by": "publisher",
"first-page": "799",
"issue": "8",
"journal-title": "JAMA.",
"key": "7701_CR15",
"unstructured": "Bilaloglu S, Aphinyanaphongs Y, Jones S, Iturrate E, Hochman J, Berger JS. Thrombosis in Hospitalized Patients With COVID-19 in a New York City Health System. JAMA. 2020: 324(8):799-801.",
"volume": "324",
"year": "2020"
},
{
"DOI": "10.1213/ANE.0000000000005292",
"author": "JH Chow",
"doi-asserted-by": "publisher",
"first-page": "930",
"issue": "4",
"journal-title": "Anesth Analg",
"key": "7701_CR16",
"unstructured": "Chow JH, Khanna AK, Kethireddy S, Yamane D, Levine A, Jackson AM, et al. Aspirin use is associated with decreased mechanical ventilation, ICU admission, and in-hospital mortality in hospitalized patients with COVID-19. Anesth Analg 2021;132(4):930-941.",
"volume": "132",
"year": "2021"
},
{
"DOI": "10.1001/jamanetworkopen.2021.3594",
"author": "R Baral",
"doi-asserted-by": "publisher",
"first-page": "e213594",
"issue": "3",
"journal-title": "JAMA Netw Open",
"key": "7701_CR17",
"unstructured": "Baral R, Tsampasian V, Debski M, Moran B, Garg P, Clark A, et al. Association between renin-angiotensin-aldosterone system inhibitors and clinical outcomes in patients with COVID-19: a systematic review and meta-analysis. JAMA Netw Open 2021;4(3):e213594.",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1038/s41467-021-21553-1",
"author": "A Gupta",
"doi-asserted-by": "publisher",
"first-page": "1325",
"issue": "1",
"journal-title": "Nat Commun",
"key": "7701_CR18",
"unstructured": "Gupta A, Madhavan MV, Poterucha TJ, DeFilippis EM, Hennessey JA, Redfors B, et al. Association between antecedent statin use and decreased mortality in hospitalized patients with COVID-19. Nat Commun 2021;12(1):1325.",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1126/science.abe9403",
"author": "DE Gordon",
"doi-asserted-by": "publisher",
"first-page": "eabe9403",
"issue": "6521",
"journal-title": "Science",
"key": "7701_CR19",
"unstructured": "Gordon DE, Hiatt J, Bouhaddou M, Rezelj VV, Ulferts S, Braberg H, et al. Comparative host-coronavirus protein interaction networks reveal pan-viral disease mechanisms. Science. 2020:370(6521):eabe9403.",
"volume": "370",
"year": "2020"
},
{
"DOI": "10.1136/annrheumdis-2020-219517",
"author": "AY Wong",
"doi-asserted-by": "publisher",
"first-page": "943",
"issue": "7",
"journal-title": "Ann Rheum Dis",
"key": "7701_CR20",
"unstructured": "Wong AY, MacKenna B, Morton CE, Schultze A, Walker AJ, Bhaskaran K, et al. Use of non-steroidal anti-inflammatory drugs and risk of death from COVID-19: an OpenSAFELY cohort analysis based on two cohorts. Ann Rheum Dis 2021;80(7):943-51.",
"volume": "80",
"year": "2021"
},
{
"author": "Z Imam",
"first-page": "469",
"issue": "4",
"journal-title": "United States J Intern Med",
"key": "7701_CR21",
"unstructured": "Imam Z, Odish F, Gill I, O'Connor D, Armstrong J, Vanood A, et al. Older age and comorbidity are independent mortality predictors in a large cohort of 1305 COVID-19 patients in Michigan, United States J Intern Med 2020;288(4):469-76.",
"volume": "288",
"year": "2020"
},
{
"DOI": "10.1016/S2213-8587(21)00050-4",
"author": "K Khunti",
"doi-asserted-by": "publisher",
"first-page": "293",
"issue": "5",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "7701_CR22",
"unstructured": "Khunti K, Knighton P, Zaccardi F, Bakhai C, Barron E, Holman N, et al. Prescription of glucose-lowering therapies and risk of COVID-19 mortality in people with type 2 diabetes: a nationwide observational study in England. Lancet Diabetes Endocrinol 2021;9(5):293-303.",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1016/j.diabres.2020.108183",
"author": "S Sharma",
"doi-asserted-by": "publisher",
"first-page": "108183",
"journal-title": "Diabetes Res Clin Pract",
"key": "7701_CR23",
"unstructured": "Sharma S, Ray A, Sadasivam B. Metformin in COVID-19: a possible role beyond diabetes. Diabetes Res Clin Pract 2020;164:108183.",
"volume": "164",
"year": "2020"
},
{
"DOI": "10.1007/s40618-021-01614-4",
"author": "R Pal",
"doi-asserted-by": "publisher",
"first-page": "53",
"issue": "1",
"journal-title": "J Endocrinol Investig",
"key": "7701_CR24",
"unstructured": "Pal R, Banerjee M, Bhadada SK, Shetty AJ, Singh B, Vyas A. Vitamin D supplementation and clinical outcomes in COVID-19: a systematic review and meta-analysis. J Endocrinol Investig 2021;45(1):53-68.",
"volume": "45",
"year": "2021"
},
{
"DOI": "10.1016/j.annonc.2020.04.479",
"author": "M Montopoli",
"doi-asserted-by": "publisher",
"first-page": "1040",
"issue": "8",
"journal-title": "Ann Oncol",
"key": "7701_CR25",
"unstructured": "Montopoli M, Zumerle S, Vettor R, Rugge M, Zorzi M, Catapano CV, et al. Androgen-deprivation therapies for prostate cancer and risk of infection by SARS-CoV-2: a population-based study (N = 4532). Ann Oncol 2020;31(8):1040-5.",
"volume": "31",
"year": "2020"
},
{
"DOI": "10.1016/j.hjc.2020.03.002",
"author": "SG Deftereos",
"doi-asserted-by": "publisher",
"first-page": "42",
"issue": "1",
"journal-title": "Hell J Cardiol",
"key": "7701_CR26",
"unstructured": "Deftereos SG, Siasos G, Giannopoulos G, Vrachatis DA, Angelidis C, Giotaki SG, et al. The Greek study in the effects of colchicine in COvid-19 complications prevention (GRECCO-19 study): Rationale and study design. Hell J Cardiol 2020;61(1):42-5.",
"volume": "61",
"year": "2020"
},
{
"DOI": "10.1016/j.pupt.2021.101989",
"author": "JI Morán Blanco",
"doi-asserted-by": "publisher",
"first-page": "101989",
"journal-title": "Pulm Pharmacol Ther",
"key": "7701_CR27",
"unstructured": "Morán Blanco JI, Alvarenga Bonilla JA, Homma S, Suzuki K, Fremont-Smith P, Villar Gómez de Las Heras K. Antihistamines and azithromycin as a treatment for COVID-19 on primary health care - a retrospective observational study in elderly patients. Pulm Pharmacol Ther 2021;67:101989.",
"volume": "67",
"year": "2021"
},
{
"DOI": "10.3390/ijerph18168486",
"author": "A Suzuki",
"doi-asserted-by": "publisher",
"first-page": "8486",
"issue": "16",
"journal-title": "Int J Environ Res Public Health",
"key": "7701_CR28",
"unstructured": "Suzuki A, Efird JT, Redding TSt, Thompson AD, Jr., Press AM, Williams CD, et al. COVID-19-associated mortality in US Veterans with and without SARS-CoV-2 infection. Int J Environ Res Public Health 2021;18(16):8486.",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.1186/1478-7954-4-2",
"author": "M-W Sohn",
"doi-asserted-by": "publisher",
"first-page": "2",
"issue": "1",
"journal-title": "Popul Health Metrics",
"key": "7701_CR29",
"unstructured": "Sohn M-W, Arnold N, Maynard C, Hynes DM. Accuracy and completeness of mortality data in the Department of Veterans Affairs. Popul Health Metrics 2006;4(1):2.",
"volume": "4",
"year": "2006"
},
{
"DOI": "10.1080/01621459.1957.10501395",
"author": "WH Kruskal",
"doi-asserted-by": "publisher",
"first-page": "356",
"issue": "279",
"journal-title": "J Am Stat Assoc",
"key": "7701_CR30",
"unstructured": "Kruskal WH. Historical notes on the wilcoxon unpaired two-sample test. J Am Stat Assoc 1957;52(279):356-60.",
"volume": "52",
"year": "1957"
},
{
"author": "NE Breslow",
"first-page": "5",
"journal-title": "IARC Sci Publ.",
"key": "7701_CR31",
"unstructured": "Breslow NE, Day NE. Statistical methods in cancer research. Volume I - The analysis of case-control studies. IARC Sci Publ. 1980(32):5-338.",
"volume": "32",
"year": "1980"
},
{
"DOI": "10.1093/biomet/75.4.800",
"author": "Y Hochberg",
"doi-asserted-by": "publisher",
"first-page": "800",
"issue": "4",
"journal-title": "Biometrika",
"key": "7701_CR32",
"unstructured": "Hochberg Y. A sharper Bonferroni procedure for multiple tests of significance. Biometrika. 1988;75(4):800-2.",
"volume": "75",
"year": "1988"
},
{
"author": "Y Benjamini",
"first-page": "289",
"issue": "1",
"journal-title": "J R Stat Soc Ser B Methodol",
"key": "7701_CR33",
"unstructured": "Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B Methodol 1995;57(1):289-300.",
"volume": "57",
"year": "1995"
},
{
"DOI": "10.1198/016214504000001907",
"author": "Y Benjamini",
"doi-asserted-by": "publisher",
"first-page": "71",
"issue": "469",
"journal-title": "J Am Stat Assoc",
"key": "7701_CR34",
"unstructured": "Benjamini Y, Yekutieli D. False Discovery rate–adjusted multiple confidence intervals for selected parameters. J Am Stat Assoc 2005;100(469):71-81.",
"volume": "100",
"year": "2005"
},
{
"DOI": "10.3390/ijerph5050394",
"author": "JT Efird",
"doi-asserted-by": "publisher",
"first-page": "394",
"issue": "5",
"journal-title": "Int J Environ Res Public Health",
"key": "7701_CR35",
"unstructured": "Efird JT, Nielsen SS. A method to compute multiplicity corrected confidence intervals for odds ratios and other relative effect estimates. Int J Environ Res Public Health 2008;5(5):394-8.",
"volume": "5",
"year": "2008"
},
{
"DOI": "10.1177/1176935120985132",
"author": "JT Efird",
"doi-asserted-by": "publisher",
"first-page": "117693512098513",
"journal-title": "Cancer Informat",
"key": "7701_CR36",
"unstructured": "Efird JT. Goldilocks Rounding: achieving balance between accuracy and parsimony in the reporting of relative effect estimates. Cancer Informat 2021;20:1176935120985132.",
"volume": "20",
"year": "2021"
},
{
"DOI": "10.7326/M20-2911",
"author": "M Jalili",
"doi-asserted-by": "publisher",
"first-page": "125",
"issue": "1",
"journal-title": "Ann Intern Med",
"key": "7701_CR37",
"unstructured": "Jalili M, et al. Characteristics and Mortality of Hospitalized Patients With COVID-19 in Iran: A National Retrospective Cohort Study. Ann Intern Med 2021;174(1):125-7.",
"volume": "174",
"year": "2021"
},
{
"DOI": "10.1136/bmj.m1966",
"author": "CM Petrilli",
"doi-asserted-by": "publisher",
"first-page": "m1966",
"journal-title": "BMJ.",
"key": "7701_CR38",
"unstructured": "Petrilli CM, Jones SA, Yang J, Rajagopalan H, O’Donnell L, Chernyak Y, et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ. 2020;369:m1966.",
"volume": "369",
"year": "2020"
},
{
"DOI": "10.1038/s41586-020-2521-4",
"author": "EJ Williamson",
"doi-asserted-by": "publisher",
"first-page": "430",
"issue": "7821",
"journal-title": "Nature.",
"key": "7701_CR39",
"unstructured": "Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584(7821):430-6.",
"volume": "584",
"year": "2020"
},
{
"DOI": "10.1682/JRRD.2015.06.0104",
"author": "T Moin",
"doi-asserted-by": "publisher",
"first-page": "853",
"issue": "6",
"journal-title": "J Rehabil Res Dev",
"key": "7701_CR40",
"unstructured": "Moin T, Damschroder LJ, Youles B, Makki F, Billington C, Yancy W, et al. Implementation of a prediabetes identification algorithm for overweight and obese Veterans. J Rehabil Res Dev 2016;53(6):853-62.",
"volume": "53",
"year": "2016"
},
{
"DOI": "10.2337/dc18-S009",
"author": "American Diabetes Association",
"doi-asserted-by": "publisher",
"first-page": "S86",
"issue": "Suppl 1",
"journal-title": "Diabetes Care",
"key": "7701_CR41",
"unstructured": "American Diabetes Association. Cardiovascular disease and risk management: standards of medical care in diabetes-2018. Diabetes Care 2018;41(Suppl 1):S86-s104.",
"volume": "41",
"year": "2018"
},
{
"DOI": "10.2337/dc18-S008",
"author": "American Diabetes Association",
"doi-asserted-by": "publisher",
"first-page": "S73",
"issue": "Suppl 1",
"journal-title": "Diabetes Care",
"key": "7701_CR42",
"unstructured": "American Diabetes Association. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes-2018. Diabetes Care 2018;41(Suppl 1):S73-s85.",
"volume": "41",
"year": "2018"
},
{
"DOI": "10.1016/j.biopha.2016.04.043",
"author": "F Kong",
"doi-asserted-by": "publisher",
"first-page": "167",
"journal-title": "Biomed Pharmacother",
"key": "7701_CR43",
"unstructured": "Kong F, Ye B, Lin L, Cai X, Huang W, Huang Z. Atorvastatin suppresses NLRP3 inflammasome activation via TLR4/MyD88/NF-κB signaling in PMA-stimulated THP-1 monocytes. Biomed Pharmacother 2016;82:167-72.",
"volume": "82",
"year": "2016"
},
{
"DOI": "10.1055/s-0040-1713152",
"author": "B Bikdeli",
"doi-asserted-by": "publisher",
"first-page": "1004",
"issue": "7",
"journal-title": "Thromb Haemost",
"key": "7701_CR44",
"unstructured": "Bikdeli B, Madhavan MV, Gupta A, Jimenez D, Burton JR, Der Nigoghossian C, et al. Pharmacological agents targeting thromboinflammation in COVID-19: review and implications for future research. Thromb Haemost 2020;120(7):1004-24.",
"volume": "120",
"year": "2020"
},
{
"DOI": "10.1016/j.diabet.2020.07.006",
"author": "AJ Scheen",
"doi-asserted-by": "publisher",
"first-page": "423",
"issue": "6",
"journal-title": "Diabetes Metab",
"key": "7701_CR45",
"unstructured": "Scheen AJ. Metformin and COVID-19: from cellular mechanisms to reduced mortality. Diabetes Metab 2020;46(6):423-6.",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.2337/dc20-1205",
"author": "B Cariou",
"doi-asserted-by": "publisher",
"first-page": "e163",
"issue": "10",
"journal-title": "Diabetes Care",
"key": "7701_CR46",
"unstructured": "Cariou B, Hadjadj S, Wargny M, Pichelin M, Gourdy P. Comment on Chen et al. Clinical characteristics and outcomes of patients with diabetes and COVID-19 in association with glucose-lowering medication. Diabetes Care 2020;43:1399-1407. Diabetes Care 2020;43(10):e163-e164.",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.4269/ajtmh.20-0375",
"author": "P Luo",
"doi-asserted-by": "publisher",
"first-page": "69",
"issue": "1",
"journal-title": "Am J Trop Med Hyg",
"key": "7701_CR47",
"unstructured": "Luo P, Qiu L, Liu Y, Liu XL, Zheng JL, Xue HY, et al. Metformin treatment was associated with decreased mortality in COVID-19 patients with diabetes in a retrospective analysis. Am J Trop Med Hyg 2020;103(1):69-72.",
"volume": "103",
"year": "2020"
},
{
"DOI": "10.3389/fendo.2020.600439",
"author": "AB Crouse",
"doi-asserted-by": "publisher",
"first-page": "600439",
"issue": "1081",
"journal-title": "Front Endocrinol",
"key": "7701_CR48",
"unstructured": "Crouse AB, Grimes T, Li P, Might M, Ovalle F, Shalev A. Metformin use is associated with reduced mortality in a diverse population with COVID-19 and diabetes. Front Endocrinol 2021;11(1081):600439.",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.3389/fendo.2021.587801",
"author": "S Ibrahim",
"doi-asserted-by": "publisher",
"first-page": "587801",
"issue": "625",
"journal-title": "Front Endocrinol",
"key": "7701_CR49",
"unstructured": "Ibrahim S, Lowe JR, Bramante CT, Shah S, Klatt NR, Sherwood N, et al. Metformin and Covid-19: focused review of mechanisms and current literature suggesting benefit. Front Endocrinol 2021;12(625):587801.",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.3389/fmed.2021.637647",
"doi-asserted-by": "crossref",
"key": "7701_CR50",
"unstructured": "Rose L, Graham L, Koenecke A, Powell M, Xiong R, Shen Z, et al. The association between Alpha-1 adrenergic receptor antagonists and in-hospital mortality from COVID-19. Front Med. 2021;8(304)."
},
{
"author": "FA Cadegiani",
"first-page": "e20691",
"issue": "12",
"journal-title": "Cureus.",
"key": "7701_CR51",
"unstructured": "Cadegiani FA, Zimerman RA, Fonseca DN, Correia MN, Muller MP, Bet DL, et al. Efficacy of proxalutamide in hospitalized COVID-19 patients: a randomized, double-blind, placebo-controlled, parallel-design clinical trial. Cureus. 2021;13(12):e20691.",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1016/S2213-2600(21)00222-8",
"author": "JC Tardif",
"doi-asserted-by": "publisher",
"first-page": "924",
"issue": "8",
"journal-title": "Lancet Respir Med",
"key": "7701_CR52",
"unstructured": "Tardif JC, Bouabdallaoui N, L'Allier PL, Gaudet D, Shah B, Pillinger MH, et al. Colchicine for community-treated patients with COVID-19 (COLCORONA): a phase 3, randomised, double-blinded, adaptive, placebo-controlled, multicentre trial. Lancet Respir Med 2021;9(8):924–932.",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1016/j.bbrc.2020.11.095",
"author": "LR Reznikov",
"doi-asserted-by": "publisher",
"first-page": "173",
"journal-title": "Biochem Biophys Res Commun",
"key": "7701_CR53",
"unstructured": "Reznikov LR, Norris MH, Vashisht R, Bluhm AP, Li D, Liao YJ, et al. Identification of antiviral antihistamines for COVID-19 repurposing. Biochem Biophys Res Commun 2021;538:173-9.",
"volume": "538",
"year": "2021"
},
{
"key": "7701_CR54",
"unstructured": "NCT04583410. Efficacy of Nicotine in Preventing COVID-19 Infection (NICOVID-PREV). Available at: https://clinicaltrials.gov/ct2/show/NCT04583410 Accessed on March 12 2021."
},
{
"DOI": "10.1016/j.toxrep.2020.04.012",
"author": "K Farsalinos",
"doi-asserted-by": "publisher",
"first-page": "658",
"journal-title": "Toxicol Rep",
"key": "7701_CR55",
"unstructured": "Farsalinos K, Niaura R, Le Houezec J, Barbouni A, Tsatsakis A, Kouretas D, et al. Editorial: Nicotine and SARS-CoV-2: COVID-19 may be a disease of the nicotinic cholinergic system. Toxicol Rep 2020;7:658-63.",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1080/1547691X.2021.1875085",
"author": "AG Gauthier",
"doi-asserted-by": "publisher",
"first-page": "23",
"issue": "1",
"journal-title": "J Immunotoxicol",
"key": "7701_CR56",
"unstructured": "Gauthier AG, Lin M, Wu J, Kennedy TP, Daley L-A, Ashby CR, et al. From nicotine to the cholinergic anti-inflammatory reflex – Can nicotine alleviate the dysregulated inflammation in COVID-19? J Immunotoxicol 2021;18(1):23-9.",
"volume": "18",
"year": "2021"
},
{
"key": "7701_CR57",
"unstructured": "US Department of Veterans Affairs. Available at https://www.va.gov/health/docs/VA_COVID_Response.pdf Accessed on July 20 2021."
},
{
"DOI": "10.2147/PPA.S74531",
"author": "HJ Weidenbacher",
"doi-asserted-by": "publisher",
"first-page": "327",
"journal-title": "Patient Prefer Adherence",
"key": "7701_CR58",
"unstructured": "Weidenbacher HJ, Beadles CA, Maciejewski ML, Reeve BB, Voils CI. Extent and reasons for nonadherence to antihypertensive, cholesterol, and diabetes medications: the association with depressive symptom burden in a sample of American veterans. Patient Prefer Adherence 2015;9:327-36.",
"volume": "9",
"year": "2015"
}
],
"reference-count": 58,
"references-count": 58,
"relation": {},
"resource": {
"primary": {
"URL": "https://link.springer.com/10.1007/s11606-022-07701-3"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Internal Medicine"
],
"subtitle": [],
"title": "Medications Associated with Lower Mortality in a SARS-CoV-2 Positive Cohort of 26,508 Veterans",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy"
}
hunt
