Colchicine in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial
Prof Peter W Horby, Martin J Landray, Collaborative Group, Mark Campbell, Enti Spata, Jonathan R Emberson, Natalie Staplin, Guilherme Pessoa-Amorim, Leon Peto, Martin Wiselka, Laura Wiffen, Simon Tiberi, Ben Caplin, Caroline Wroe, Christopher Green, Paul Hine, Benjamin Prudon, Tina George, Andrew J Wight, Kenneth Baillie, Buddha Basnyat, Maya Buch, Lucy C Chappell, Jeremy Day, Saul N Faust, Raph L Hamers, Thomas Jaki, Edmund Juszczak, Katie Jeffery, Wei Shen Lim, Alan Montgomery, Andrew Mumford, Kathryn Rowan, Guy Thwaites, Marion Mafham, Richard Haynes, W Peter, Mark Horby, Enti Campbell, Marion Spata, Richard Mafham, Martin J Haynes, Landray, Peter Sandercock, Janet Darbyshire, David Demets, Robert Fowler
The Lancet Respiratory Medicine, doi:10.1016/s2213-2600(21)00435-5
Background Colchicine has been proposed as a treatment for COVID-19 based on its anti-inflammatory actions. We aimed to evaluate the efficacy and safety of colchicine in patients admitted to hospital with COVID-19.
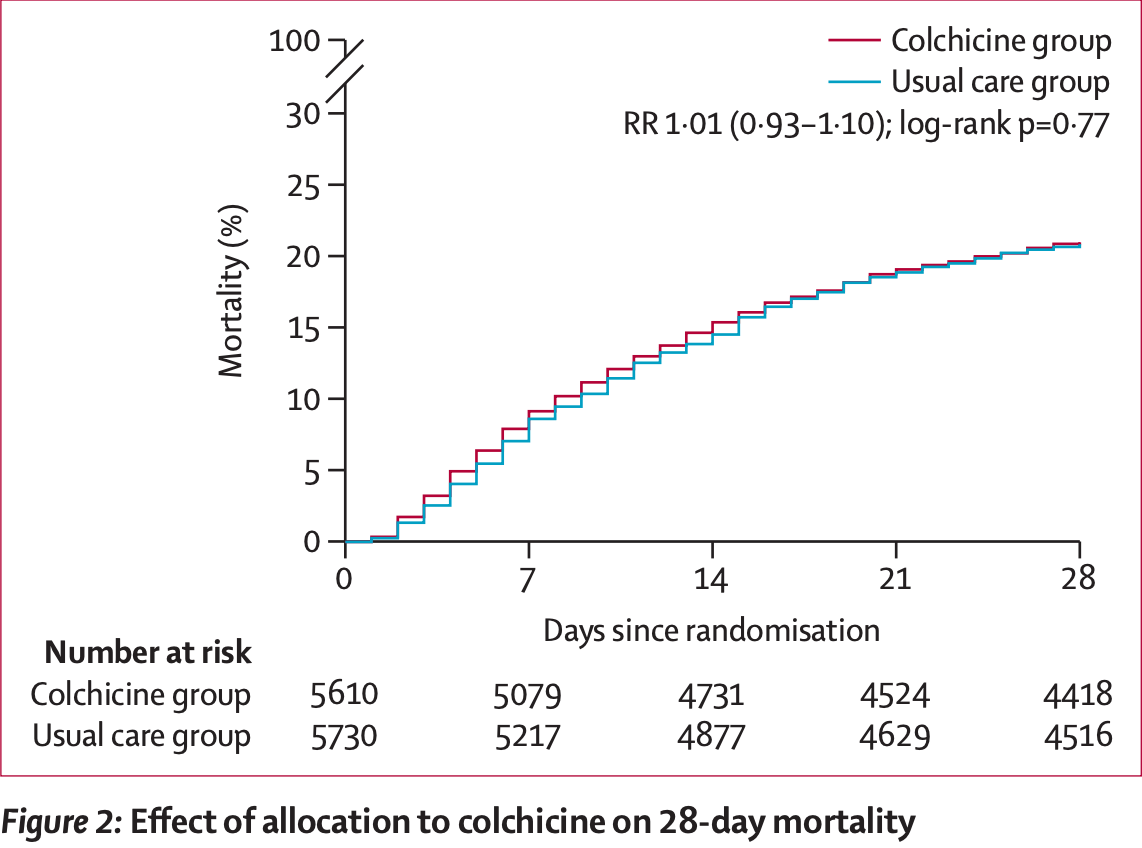
Methods In this streamlined, randomised, controlled, open-label trial, underway at 177 hospitals in the UK, two hospitals in Indonesia, and two hospitals in Nepal, several possible treatments were compared with usual care in patients hospitalised with COVID-19. Patients were eligible for inclusion in the study if they were admitted to hospital with clinically suspected or laboratory confirmed SARS-CoV-2 infection and had no medical history that might, in the opinion of the attending clinician, put the patient at significant risk if they were to participate in the trial. Eligible and consenting adults were randomly assigned (1:1) to receive either usual standard of care alone (usual care group) or usual standard of care plus colchicine (colchicine group) using web-based simple (unstratified) randomisation with allocation concealment. Participants received colchicine 1 mg after randomisation followed by 500 µg 12 h later and then 500 µg twice a day by mouth or nasogastric tube for 10 days in total or until discharge. Dose frequency was halved for patients receiving a moderate CYP3A4 inhibitor (eg, diltiazem), patients with an estimated glomerular filtration rate of less than 30 mL/min per 1•73m², and those with an estimated bodyweight of less than 70 kg. The primary outcome was 28-day mortality, secondary endpoints included time to discharge, the proportion of patients discharged from hospital within 28 days, and, in patients not on invasive mechanical ventilation at randomisation, a composite endpoint of invasive mechanical ventilation or death. All analyses were by intention-to-treat. The trial is registered with ISRCTN, 50189673, and ClinicalTrials.gov, NCT04381936.
References
Broz, Dixit, Inflammasomes: mechanism of assembly, regulation and signalling, Nat Rev Immunol
Dalbeth, Lauterio, Wolfe, Mechanism of action of colchicine in the treatment of gout, Clin Ther
Deftereos, Giannopoulos, Vrachatis, Effect of colchicine vs standard care on cardiac and inflammatory biomarkers and clinical outcomes in patients hospitalized with coronavirus disease 2019: the GRECCO-19 randomized clinical trial, JAMA Netw Open
Deftereos, Siasos, Giannopoulos, The Greek study in the effects of colchicine in COvid-19 complications prevention (GRECCO-19 study): rationale and study design, Hellenic J Cardiol
Dorward, Russell, Um, Tissue-specific immunopathology in fatal COVID-19, Am J Respir Crit Care Med
Fiolet, Opstal, Mosterd, Efficacy and safety of lowdose colchicine in patients with coronary disease: a systematic review and meta-analysis of randomized trials, Eur Heart J
Horby, Lim, Dexamethasone in hospitalized patients with Covid-19, N Engl J Med
Horby, Mafham, Effect of hydroxychloroquine in hospitalized patients with Covid-19, N Engl J Med
Huang, Wang, Li, Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet
Imazio, Brucato, Cemin, A randomized trial of colchicine for acute pericarditis, N Engl J Med
Kalil, Patterson, Mehta, Baricitinib plus remdesivir for hospitalized adults with Covid-19, N Engl J Med
Lopes, Bonjorno, Giannini, Beneficial effects of colchicine for moderate to severe COVID-19: a randomised, doubleblinded, placebo-controlled clinical trial, RMD Open
Martinez, Celermajer, Patel, The NLRP3 inflammasome and the emerging role of colchicine to inhibit atherosclerosisassociated inflammation, Atherosclerosis
Mcelvaney, Mcevoy, Mcelvaney, Characterization of the inflammatory response to severe COVID-19 illness, Am J Respir Crit Care Med
Rodrigues, De Sa, Ishimoto, Inflammasomes are activated in response to SARS-CoV-2 infection and are associated with COVID-19 severity in patients, J Exp Med
Ruan, Yang, Wang, Jiang, Song, Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China, Intensive Care Med
Sterne, Murthy, Diaz, Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19: a meta-analysis, JAMA
Tardif, Bouabdallaoui, Allier, Colchicine for community-treated patients with COVID-19 (COLCORONA): a phase 3, randomised, double-blinded, adaptive, placebo-controlled, multicentre trial, Lancet Respir Med
Tardif, Kouz, Waters, Efficacy and safety of low-dose colchicine after myocardial infarction, N Engl J Med
Thwaites, Sevilla Uruchurtu, Siggins, Inflammatory profiles across the spectrum of disease reveal a distinct role for GM-CSF in severe COVID-19, Sci Immunol
Wang, Chen, Yang, Inflammation-associated factors for predicting in-hospital mortality in patients with COVID-19, J Med Virol
DOI record:
{
"DOI": "10.1016/s2213-2600(21)00435-5",
"ISSN": [
"2213-2600"
],
"URL": "http://dx.doi.org/10.1016/S2213-2600(21)00435-5",
"alternative-id": [
"S2213260021004355"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Colchicine in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "The Lancet Respiratory Medicine"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/S2213-2600(21)00435-5"
},
{
"label": "CrossRef DOI link to the associated document",
"name": "associatedlink",
"value": "https://doi.org/10.1016/S2213-2600(21)00462-8"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2021 The Author(s). Published by Elsevier Ltd."
}
],
"container-title": "The Lancet Respiratory Medicine",
"container-title-short": "The Lancet Respiratory Medicine",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.fr",
"clinicalkey.jp",
"clinicalkey.com.au",
"clinicalkey.es",
"clinicalkey.com",
"thelancet.com",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2021,
10,
19
]
],
"date-time": "2021-10-19T18:14:33Z",
"timestamp": 1634667273000
},
"deposited": {
"date-parts": [
[
2022,
3,
25
]
],
"date-time": "2022-03-25T21:36:39Z",
"timestamp": 1648244199000
},
"funder": [
{
"DOI": "10.13039/100010269",
"doi-asserted-by": "publisher",
"name": "Wellcome Trust"
},
{
"DOI": "10.13039/501100000265",
"doi-asserted-by": "publisher",
"name": "Medical Research Council"
},
{
"DOI": "10.13039/501100000272",
"doi-asserted-by": "publisher",
"name": "National Institute for Health Research"
}
],
"indexed": {
"date-parts": [
[
2024,
3,
23
]
],
"date-time": "2024-03-23T05:20:09Z",
"timestamp": 1711171209957
},
"is-referenced-by-count": 99,
"issue": "12",
"issued": {
"date-parts": [
[
2021,
12
]
]
},
"journal-issue": {
"issue": "12",
"published-print": {
"date-parts": [
[
2021,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
12,
1
]
],
"date-time": "2021-12-01T00:00:00Z",
"timestamp": 1638316800000
}
},
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
9,
21
]
],
"date-time": "2021-09-21T00:00:00Z",
"timestamp": 1632182400000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S2213260021004355?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S2213260021004355?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "1419-1426",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2021,
12
]
]
},
"published-print": {
"date-parts": [
[
2021,
12
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"article-title": "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "497",
"journal-title": "Lancet",
"key": "10.1016/S2213-2600(21)00435-5_bib1",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1007/s00134-020-05991-x",
"article-title": "Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China",
"author": "Ruan",
"doi-asserted-by": "crossref",
"first-page": "846",
"journal-title": "Intensive Care Med",
"key": "10.1016/S2213-2600(21)00435-5_bib2",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.1002/jmv.26771",
"article-title": "Inflammation-associated factors for predicting in-hospital mortality in patients with COVID-19",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "2908",
"journal-title": "J Med Virol",
"key": "10.1016/S2213-2600(21)00435-5_bib3",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1126/sciimmunol.abg9873",
"article-title": "Inflammatory profiles across the spectrum of disease reveal a distinct role for GM-CSF in severe COVID-19",
"author": "Thwaites",
"doi-asserted-by": "crossref",
"first-page": "eabg9873",
"journal-title": "Sci Immunol",
"key": "10.1016/S2213-2600(21)00435-5_bib4",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.1164/rccm.202005-1583OC",
"article-title": "Characterization of the inflammatory response to severe COVID-19 illness",
"author": "McElvaney",
"doi-asserted-by": "crossref",
"first-page": "812",
"journal-title": "Am J Respir Crit Care Med",
"key": "10.1016/S2213-2600(21)00435-5_bib5",
"volume": "202",
"year": "2020"
},
{
"DOI": "10.1164/rccm.202008-3265OC",
"article-title": "Tissue-specific immunopathology in fatal COVID-19",
"author": "Dorward",
"doi-asserted-by": "crossref",
"first-page": "192",
"journal-title": "Am J Respir Crit Care Med",
"key": "10.1016/S2213-2600(21)00435-5_bib6",
"volume": "203",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2021436",
"article-title": "Dexamethasone in hospitalized patients with Covid-19",
"author": "Horby",
"doi-asserted-by": "crossref",
"first-page": "693",
"journal-title": "N Engl J Med",
"key": "10.1016/S2213-2600(21)00435-5_bib7",
"volume": "384",
"year": "2021"
},
{
"DOI": "10.1001/jama.2020.17023",
"article-title": "Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19: a meta-analysis",
"author": "Sterne",
"doi-asserted-by": "crossref",
"first-page": "1330",
"journal-title": "JAMA",
"key": "10.1016/S2213-2600(21)00435-5_bib8",
"volume": "324",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(21)00676-0",
"article-title": "Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial",
"doi-asserted-by": "crossref",
"first-page": "1637",
"journal-title": "Lancet",
"key": "10.1016/S2213-2600(21)00435-5_bib9",
"volume": "397",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2031994",
"article-title": "Baricitinib plus remdesivir for hospitalized adults with Covid-19",
"author": "Kalil",
"doi-asserted-by": "crossref",
"first-page": "795",
"journal-title": "N Engl J Med",
"key": "10.1016/S2213-2600(21)00435-5_bib10",
"volume": "384",
"year": "2020"
},
{
"DOI": "10.1038/nri.2016.58",
"article-title": "Inflammasomes: mechanism of assembly, regulation and signalling",
"author": "Broz",
"doi-asserted-by": "crossref",
"first-page": "407",
"journal-title": "Nat Rev Immunol",
"key": "10.1016/S2213-2600(21)00435-5_bib11",
"volume": "16",
"year": "2016"
},
{
"DOI": "10.1084/jem.20201707",
"article-title": "Inflammasomes are activated in response to SARS-CoV-2 infection and are associated with COVID-19 severity in patients",
"author": "Rodrigues",
"doi-asserted-by": "crossref",
"first-page": "e20201707",
"journal-title": "J Exp Med",
"key": "10.1016/S2213-2600(21)00435-5_bib12",
"volume": "218",
"year": "2021"
},
{
"DOI": "10.1016/j.clinthera.2014.07.017",
"article-title": "Mechanism of action of colchicine in the treatment of gout",
"author": "Dalbeth",
"doi-asserted-by": "crossref",
"first-page": "1465",
"journal-title": "Clin Ther",
"key": "10.1016/S2213-2600(21)00435-5_bib13",
"volume": "36",
"year": "2014"
},
{
"DOI": "10.1093/eurheartj/ehab115",
"article-title": "Efficacy and safety of low-dose colchicine in patients with coronary disease: a systematic review and meta-analysis of randomized trials",
"author": "Fiolet",
"doi-asserted-by": "crossref",
"first-page": "2765",
"journal-title": "Eur Heart J",
"key": "10.1016/S2213-2600(21)00435-5_bib14",
"volume": "42",
"year": "2021"
},
{
"DOI": "10.1016/j.atherosclerosis.2017.12.027",
"article-title": "The NLRP3 inflammasome and the emerging role of colchicine to inhibit atherosclerosis-associated inflammation",
"author": "Martinez",
"doi-asserted-by": "crossref",
"first-page": "262",
"journal-title": "Atherosclerosis",
"key": "10.1016/S2213-2600(21)00435-5_bib15",
"volume": "269",
"year": "2018"
},
{
"DOI": "10.1056/NEJMoa1208536",
"article-title": "A randomized trial of colchicine for acute pericarditis",
"author": "Imazio",
"doi-asserted-by": "crossref",
"first-page": "1522",
"journal-title": "N Engl J Med",
"key": "10.1016/S2213-2600(21)00435-5_bib16",
"volume": "369",
"year": "2013"
},
{
"DOI": "10.1056/NEJMoa1912388",
"article-title": "Efficacy and safety of low-dose colchicine after myocardial infarction",
"author": "Tardif",
"doi-asserted-by": "crossref",
"first-page": "2497",
"journal-title": "N Engl J Med",
"key": "10.1016/S2213-2600(21)00435-5_bib17",
"volume": "381",
"year": "2019"
},
{
"article-title": "The impact of colchicine on the COVID-19 patients; a clinical trial study",
"author": "Salehzadeh",
"journal-title": "Research Square",
"key": "10.1016/S2213-2600(21)00435-5_bib18",
"year": "2020"
},
{
"DOI": "10.1136/rmdopen-2020-001455",
"article-title": "Beneficial effects of colchicine for moderate to severe COVID-19: a randomised, double-blinded, placebo-controlled clinical trial",
"author": "Lopes",
"doi-asserted-by": "crossref",
"first-page": "e001455",
"journal-title": "RMD Open",
"key": "10.1016/S2213-2600(21)00435-5_bib19",
"volume": "7",
"year": "2021"
},
{
"DOI": "10.1001/jamanetworkopen.2020.13136",
"article-title": "Effect of colchicine vs standard care on cardiac and inflammatory biomarkers and clinical outcomes in patients hospitalized with coronavirus disease 2019: the GRECCO-19 randomized clinical trial",
"author": "Deftereos",
"doi-asserted-by": "crossref",
"first-page": "e2013136",
"journal-title": "JAMA Netw Open",
"key": "10.1016/S2213-2600(21)00435-5_bib20",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2022926",
"article-title": "Effect of hydroxychloroquine in hospitalized patients with Covid-19",
"author": "Horby",
"doi-asserted-by": "crossref",
"first-page": "2030",
"journal-title": "N Engl J Med",
"key": "10.1016/S2213-2600(21)00435-5_bib21",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)32013-4",
"article-title": "Lopinavir-ritonavir in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial",
"doi-asserted-by": "crossref",
"first-page": "1345",
"journal-title": "Lancet",
"key": "10.1016/S2213-2600(21)00435-5_bib22",
"volume": "396",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(21)00149-5",
"article-title": "Azithromycin in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial",
"doi-asserted-by": "crossref",
"first-page": "605",
"journal-title": "Lancet",
"key": "10.1016/S2213-2600(21)00435-5_bib23",
"volume": "397",
"year": "2021"
},
{
"DOI": "10.1016/S0140-6736(21)00897-7",
"article-title": "Convalescent plasma in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial",
"doi-asserted-by": "crossref",
"first-page": "2049",
"journal-title": "Lancet",
"key": "10.1016/S2213-2600(21)00435-5_bib24",
"volume": "397",
"year": "2021"
},
{
"DOI": "10.1016/j.hjc.2020.03.002",
"article-title": "The Greek study in the effects of colchicine in COvid-19 complications prevention (GRECCO-19 study): rationale and study design",
"author": "Deftereos",
"doi-asserted-by": "crossref",
"first-page": "42",
"journal-title": "Hellenic J Cardiol",
"key": "10.1016/S2213-2600(21)00435-5_bib25",
"volume": "61",
"year": "2020"
},
{
"DOI": "10.1016/S2213-2600(21)00222-8",
"article-title": "Colchicine for community-treated patients with COVID-19 (COLCORONA): a phase 3, randomised, double-blinded, adaptive, placebo-controlled, multicentre trial",
"author": "Tardif",
"doi-asserted-by": "crossref",
"first-page": "924",
"journal-title": "Lancet Respir Med",
"key": "10.1016/S2213-2600(21)00435-5_bib26",
"volume": "9",
"year": "2021"
}
],
"reference-count": 26,
"references-count": 26,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S2213260021004355"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Pulmonary and Respiratory Medicine"
],
"subtitle": [],
"title": "Colchicine in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "9"
}