The incidence, clinical characteristics, and outcome of COVID-19 in a prospectively followed cohort of patients with Behçet’s syndrome
et al., Rheumatology International, doi:10.1007/s00296-021-05056-2, Nov 2021
Colchicine for COVID-19
5th treatment shown to reduce risk in
September 2020, now with p = 0.0000049 from 54 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
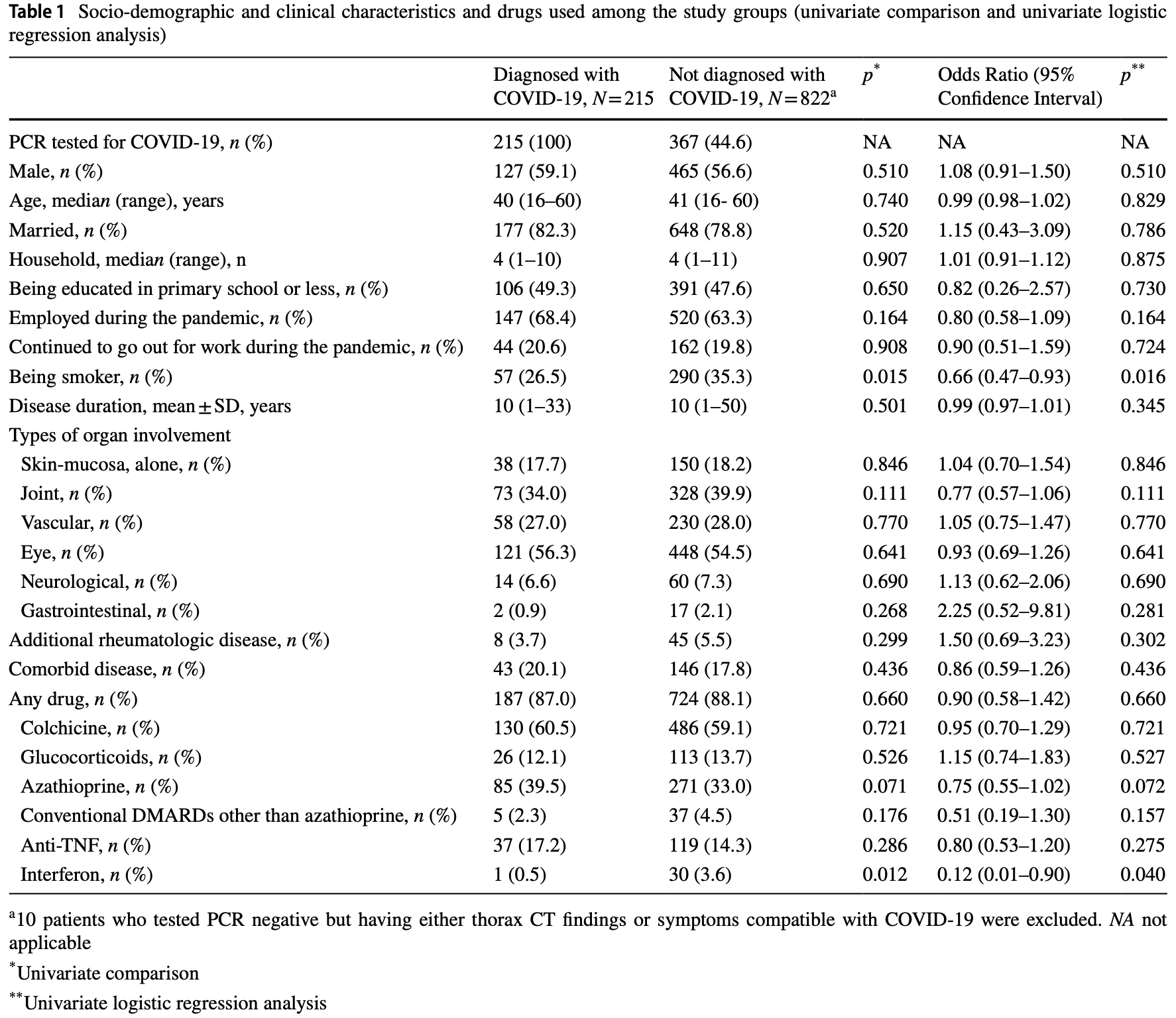
Prospective analysis of 1,047 Behçet’s syndrome patients in Turkey, showing no significant difference in cases with colchicine use.
Meta-analysis of all colchicine studies shows benefit for clinical outcomes but not for viral or case outcomes, consistent with an intervention that may have limited or no direct antiviral effect, but minimizes progression via other mechanisms (for example by aiding the immune system, minimizing immune over-activation, minizing secondary complications, or aiding recovery).
|
risk of case, 4.0% lower, RR 0.96, p = 0.72, treatment 130 of 616 (21.1%), control 85 of 421 (20.2%), odds ratio converted to relative risk.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Ozcifci et al., 25 Nov 2021, prospective, Turkey, peer-reviewed, 13 authors, study period 1 April, 2020 - 30 April, 2021.
Contact: eseyahi@yahoo.com.
The incidence, clinical characteristics, and outcome of COVID-19 in a prospectively followed cohort of patients with Behçet’s syndrome
Rheumatology International, doi:10.1007/s00296-021-05056-2
Initial case series of small number of patients at the beginning of the pandemic reported a rather guarded prognosis for Behçet's syndrome (BS) patients infected with SARS-CoV-2. In this prospective study, we describe the incidence, clinical characteristics, disease course, management, and outcome in a large cohort of BS patients with laboratory-confirmed infection of SARS-CoV-2. We defined a cohort of 1047 registered BS patients who were aged between 16 and 60 years and seen routinely before the pandemic at the multidisciplinary outpatient clinic. We followed prospectively this cohort from beginning of April 2020 until the end of April 2021. During 13 months of follow-up, of the 1047 (599 M/448 F) patients, 592 (56.5%) were tested for SARS-CoV-2 PCR at least once and 215 (20.5%; 95% CI 0.18-0.23) were tested positive. We observed 2 peaks which took place in December 2020 and April 2021. Of the 215 PCR positive patients, complete information was available in 214. Of these 214, 14 (6.5%) were asymptomatic for COVID-19. In the remaining, the most common symptoms were anosmia, fatigue, fever, arthralgia, and headache. A total of 40 (18.7%) had lung involvement, 25 (11.7%) were hospitalized, 1 was admitted to the intensive care unit while none died. Favipiravir was the most prescribed drug (74.3%), followed by colchicine (40.2%), and hydroxychloroquine (20.1%) in the treatment of COVID-19. After COVID-19, 5 patients (2.3%) were given supplemental O 2 and 31 (14.5%) antiaggregant or anticoagulants. During COVID-19, of the 214 PCR positive patients, 116 (54.2%) decreased the dose of their immunosuppressives or stopped taking completely; 36 (16.8%) experienced a BS flare which was mostly oral ulcers (10.3%). None of the patients reported a thrombotic event. A total of 93 (43.5%) patients reported BS flares after a median 45 days of COVID-19 infection and this was found to be significantly associated with immunosuppressive drug discontinuation. Multiple regression analysis adjusted for age and gender indicated that smoking and using interferon-alpha decreased the likelihood of getting COVID-19. The incidence and severity of COVID-19 did not differ between those who were using colchicine or not. The cumulative incidence of COVID-19 in this prospectively followed cohort of BS patients was almost two folds of that estimated for the general population living in Istanbul, Turkey, however, the clinical outcome of COVID-19 was not severe and there was no mortality. The protective effect of smoking and interferon deserves further investigation. On the other hand, colchicine did not have any positive or negative effect against COVID-19. Significant number of patients flared after COVID-19, however, this was significantly associated with immunosuppressive discontinuation during the infection. Contrary to our previous observations, COVID-19 did not seem to exacerbate thrombotic events during or after the infection.
Keywords Outcome • COVID-19 • Behcet's disease •..
Supplementary Information The online version contains supplementary material available at https:// doi. org/ 10. 1007/ s00296-021-05056-2. Author contributions All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by GO, TA, ZA, IIB, FT, MO, YO, SU, GH, MM, IF, VH and ES. The first draft of the manuscript was written by GO and ES and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Authors and Affiliations
Guzin
References
Akiyama, Hamdeh, Micic, Sakuraba, Prevalence and clinical outcomes of COVID-19 in patients with autoimmune diseases: a systematic and metaanalysis, Ann Rheum Dis, doi:10.1136/annrheumdis-2020-218946
Angelidis, Kotsialou, Kossyvakis, Vrettou, Zacharoulis et al., Colchicine Pharmacokinetics and Mechanism of Action, Curr Pharm Des, doi:10.2174/1381612824666180123110042
Azizlerli, Köse, Sarica, Gül, Tutkun et al., Prevalence of Behçet's disease in Istanbul, Turkey Int J Dermatol, doi:10.1046/j.1365-4362.2003.01893.x
Bourguiba, Delplanque, Vinit, Ackermann, Savey et al., Clinical course of COVID-19 in a cohort of 342 familial Mediterranean fever patients with a long-term treatment by colchicine in a French endemic area, Ann Rheum Dis, doi:10.1136/annrheumdis-2020-218707
Cocco, Chu, Pandolfi, Colchicine in clinical medicine. A guide for internists, Eur J Intern Med, doi:10.1016/j.ejim.2010.09.010
Daniel, Biostatistics: a foundation for analysis in the health sciences
Davatchi, Abdollahi, Banihashemi, Shahram, Nadji et al., Colchicine versus placebo in Behçet's disease: randomized, doubleblind, controlled crossover trial, Mod Rheumatol, doi:10.1007/s10165-009-0200-2
Deftereos, Giannopoulos, Vrachatis, Siasos, Giotaki et al., Effect of Colchicine vs Standard Care on Cardiac and Inflammatory Biomarkers and Clinical Outcomes in Patients Hospitalized With Coronavirus Disease 2019: The GRECCO-19 Randomized Clinical Trial, JAMA Netw Open, doi:10.1001/jamanetworkopen.2020.13136
Dye, Adler, Effects of cigarette smoke on epithelial cells of the respiratory tract, Thorax, doi:10.1136/thx.49.8.825
Emmi, Bettiol, Mattioli, Silvestri, Scala et al., SARS-CoV-2 infection among patients with systemic autoimmune diseases, Autoimmun Rev, doi:10.1016/j.autrev.2020.102575
Emmi, Vitale, Silvestri, Boddi, Becatti et al., Adalimumab-based treatment versus disease-modifying antirheumatic drugs for venous thrombosis in Behçet's Syndrome: a Retrospective Study of Seventy Patients With Vascular Involvement, Arthritis Rheumatol, doi:10.1002/art.40531
Esatoglu, Tascilar, Babaoğlu, Bes, Yurttas et al., Turkish Society for Rheumatology COVID-19 Registry Investigators (2021) COVID-19 among patients with inflammatory rheumatic diseases, Front Immunol, doi:10.3389/fimmu.2021.651715
Espinosa, Araujo, Amaro, Bodro, Moreno et al., COVID-19 and Behçet's disease: clinical case series, Ann Rheum Dis, doi:10.1136/annrheumdis-2020-217778
Farsalinos, Barbouni, Poulas, Polosa, Caponnetto et al., Current smoking, former smoking, and adverse outcome among hospitalized COVID-19 patients: a systematic review and meta-analysis, Ther Adv Chronic Dis, doi:10.1177/2040622320935765
Feld, Treatment indication and response to standard of care with peginterferon and ribavirin in acute and chronic HCV infection, Best Pract Res Clin Gastroenterol, doi:10.1016/j.bpg.2012.09.013
Ferri, Giuggioli, Raimondo, 'andolina, Tavoni et al., COVID-19 & ASD Italian Study Group (2020) COVID-19 and rheumatic autoimmune systemic diseases: report of a large Italian patients series, Clin Rheumatol, doi:10.1007/s10067-020-05334-7
Gendelman, Amital, Bragazzi, Watad, Chodick, Continuous hydroxychloroquine or colchicine therapy does not prevent infection with SARS-CoV-2: Insights from a large healthcare database analysis, Autoimmun Rev, doi:10.1016/j.autrev.2020.102566
González-Rubio, Navarro-López, López-Nájera, López-Nájera, Jiménez-Díaz et al., A systematic review and meta-analysis of hospitalised current smokers and COVID-19, Int J Environ Res Public Health, doi:10.3390/ijerph17207394
Hadjadj, Yatim, Barnabei, Corneau, Boussier et al., Impaired type I interferon activity and inflammatory responses in severe COVID-19 patients, Science, doi:10.1126/science.abc6027
Hyrich, Machado, Rheumatic disease and COVID-19: epidemiology and outcomes, Nat Rev Rheumatol, doi:10.1038/s41584-020-00562-2.PMID:33339986;PMCID:PMC7747184
Jain, Yuan, Predictive symptoms and comorbidities for severe COVID-19 and intensive care unit admission: a systematic review and meta-analysis, Int J Public Health, doi:10.1007/s00038-020-01390-7
Lai, Hui, Leung, Lau, Pegylated interferon alpha-2a (40 kDa) in the treatment of chronic hepatitis B, Int J Nanomedicine
Leung, Yang, Sin, Reply to: "Current smoking is not associated with COVID-19, Eur Respir J, doi:10.1183/13993003.01340-2020
Lopes, Bonjorno, Giannini, Amaral, Menezes et al., Beneficial effects of colchicine for moderate to severe COVID-19: a randomised, double-blinded, placebocontrolled clinical trial, RMD Open, doi:10.1136/rmdopen-2020-001455
Loutfy, Blatt, Siminovitch, Ward, Wolff et al., Interferon alfacon-1 plus corticosteroids in severe acute respiratory syndrome: a preliminary study, JAMA, doi:10.1001/jama.290.24.3222
Madrid-García, Pérez, Colomer, León-Mateos, Jover et al., Influence of colchicine prescription in COVID-19-related hospital admissions: a survival analysis, Ther Adv Musculoskelet Dis, doi:10.1177/1759720X211002684
Manenti, Maggiore, Fiaccadori, Meschi, Antoni et al., Reduced mortality in COVID-19 patients treated with colchicine: results from a retrospective, observational study, PLoS ONE, doi:10.1371/journal.pone.0248276
Mat, Yurdakul, Uysal, Gogus, Ozyazgan et al., A double-blind trial of depot corticosteroids in Behçet's syndrome, Rheumatology, doi:10.1093/rheumatology/kei165
Mattioli, Bettiol, Silvestri, Urban, Palermo et al., Prevalence and clinical course of SARS-CoV-2 infection in patients with Behçet's syndrome, Clin Exp Rheumatol
Mehta, Haskard, Laffan, Chambers, Hunt, Thromboses and COVID-19: reducing inflammation in addition to thromboprophylaxis, Lancet Rheumatol, doi:10.1016/S2665-9913(21)00003-5
Miesbach, Makris, COVID-19: coagulopathy, risk of thrombosis, and the rationale for anticoagulation, Clin Appl Thromb Hemost, doi:10.1177/1076029620938149
Nas, Eryilmaz, Geyik, Altaş, COVID-19 in patients with familial Mediterranean fever treated with colchicine: case based review, Rheumatol Int, doi:10.1007/s00296-021-04809-3
Pablos, Galindo, Carmona, Lledó, Retuerto et al., tors Group; RIER investigators group (2020) Clinical outcomes of hospitalised patients with COVID-19 and chronic inflammatory and autoimmune rheumatic diseases: a multicentric matched cohort study, Ann Rheum Dis, doi:10.1136/annrheumdis-2020-218296
Patanavanich, Glantz, Smoking is associated With COVID-19 progression: a meta-analysis, Nicotine Tob Res, doi:10.1093/ntr/ntaa082
Reddy, Charles, Sklavounos, Dutt, Seed et al., The effect of smoking on COVID-19 severity: a systematic review and meta-analysis, J Med Virol, doi:10.1002/jmv.26389
Rentsch, Kidwai-Khan, Tate, Park, King et al., Patterns of COVID-19 testing and mortality by race and ethnicity among United States veterans: a nationwide cohort study, PLoS Med, doi:10.1371/journal.pmed.1003379
Richter, Boldescu, Graf, Streicher, Dimoglo et al., Synthesis, biological evaluation, and molecular docking of combretastatin and colchicine derivatives and their hCE1-Activated Prodrugs as Antiviral Agents, ChemMedChem, doi:10.1002/cmdc.201800641
Russo, Bonassi, Giacconi, Malavolta, Tomino et al., COVID-19 and smoking: is nicotine the hidden link?, Eur Respir J, doi:10.1183/13993003.01116-2020
Seyahi, Poyraz, Sut, Akdogan, Hamuryudan, The psychological state and changes in the routine of the patients with rheumatic diseases during the coronavirus disease (COVID-19) outbreak in Turkey: a web-based cross-sectional survey, Rheumatol Int, doi:10.1007/s00296-020-04626-0
Shin, Moon, Jin, Kim, Yang et al., Autoimmune inflammatory rheumatic diseases and COVID-19 outcomes in South Korea: a nationwide cohort study, Lancet Rheumatol, doi:10.1016/S2665-9913(21)00151-X
Simons, Shahab, Brown, Perski, The association of smoking status with SARS-CoV-2 infection, hospitalization and mortality from COVID-19: a living rapid evidence review with Bayesian meta-analyses (version 7), Addiction, doi:10.1111/add.15276
Tardif, Bouabdallaoui, Allier, Gaudet, Shah et al., Colchicine for community-treated patients with COVID-19 (COLCORONA): a phase 3, randomised, double-blinded, adaptive, placebo-controlled, multicentre trial, Lancet Respir Med, doi:10.1016/S2213-2600(21)00222-8
Trubiano, Vogrin, Smibert, Marhoon, Alexander et al., COVID-MATCH65-A prospectively derived clinical decision rule for severe acute respiratory syndrome coronavirus 2, PLoS ONE, doi:10.1371/journal.pone.0243414
Tsigaris, Da Silva, Smoking Prevalence and COVID-19 in Europe, Nicotine Tob Res, doi:10.1093/ntr/ntaa121
Tugal-Tutkun, Mudun, Urgancioglu, Kamali, Kasapoglu et al., Efficacy of infliximab in the treatment of uveitis that is resistant to treatment with the combination of azathioprine, cyclosporine, and corticosteroids in Behçet's disease: an open-label trial, Arthritis Rheum, doi:10.1002/art.21231
Vallet, Riviere, Sanna, Deroux, Moulis et al., Efficacy of anti-TNF alpha in severe and/or refractory Behçet's disease: Multicenter study of 124 patients, J Autoimmun, doi:10.1016/j.jaut.2015.06.005
Yang, Taylor, Lightman, Interferon-alpha in the management of patients with Behçet's disease, Br J Hosp Med (Lond), doi:10.12968/hmed.2008.69.10.31317
Yazici, Pazarli, Barnes, Tüzün, Ozyazgan et al., A controlled trial of azathioprine in Behçet's syndrome, N Engl J Med, doi:10.1056/NEJM199002013220501
Yazici, Seyahi, Hatemi, Yazici, Behçet syndrome: a contemporary view, Nat Rev Rheumatol, doi:10.1038/nrrheum.2017.208
Yurdakul, Mat, Tüzün, Ozyazgan, Hamuryudan et al., A double-blind trial of colchicine in Behçet's syndrome, Arthritis Rheum, doi:10.1002/1529-0131(200111)44:11%3c2686::aid-art448%3e3.0.co;2-h
Yurttaş, Oztas, Tunc, Balkan, Tabak et al., Characteristics and outcomes of Behçet's syndrome patients with Coronavirus Disease 2019: a case series of 10 patients, Intern Emerg Med, doi:10.1007/s11739-020-02427-8
Zhang, Bastard, Liu, Inborn errors of type I IFN immunity in patients with life-threatening COVID-19, Science, doi:10.1126/science.abd4570
Zhong, Shen, Yang, Huang, Chen et al., COVID-19 in patients with rheumatic disease in Hubei province, China: a multicentre retrospective observational study, Lancet Rheumatol, doi:10.1016/S2665-9913(20)30227-7
Zhou, Chen, Shannon, Wei, Xiang et al., Corrigendum: interferon-α2b treatment for COVID-19, Front Immunol, doi:10.3389/fimmu.2020.615275.Erratumfor:FrontImmunol.2020May15;11:1061
Zouboulis, Van Laar, Schirmer, Emmi, Fortune et al., Adamantiades-Behçet's disease (Behçet's disease) and COVID-19, J Eur Acad Dermatol Venereol, doi:10.1111/jdv.17325
DOI record:
{
"DOI": "10.1007/s00296-021-05056-2",
"ISSN": [
"0172-8172",
"1437-160X"
],
"URL": "http://dx.doi.org/10.1007/s00296-021-05056-2",
"alternative-id": [
"5056"
],
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "21 October 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "13 November 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "25 November 2021"
},
{
"group": {
"label": "Declarations",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1
},
{
"group": {
"label": "Conflict of interest",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "Guzin Ozcifci, Tahacan Aydin, Zeynep Atli, Ilker Inanc Balkan, Mert Oztas, Yesim Ozguler, Melike Melikoglu, Izzet Fresko and Vedat Hamuryudan declare that they have no conflict of interest. Fehmi Tabak, has received honoraria, consulting or speaker fees from GSK, MSD, AbbVie and Gilead. Serdal Ugurlu has received honoraria, consulting or speaker fees from Novartis, Pfizer, Lilly and Celltrion. Gulen Hatemi has received research grant from Celgene, honoraria consulting or speaker fees from AbbVie, Amgen, Celgene, Lilly, Novartis and UCB Pharma. Emire Seyahi has received honoraria, consulting or speaker fees from Novartis, Pfizer, AbbVie and Gilead."
},
{
"label": "Free to read",
"name": "free",
"value": "This content has been made available to all."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-4774-9284",
"affiliation": [],
"authenticated-orcid": false,
"family": "Ozcifci",
"given": "Guzin",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-8125-4808",
"affiliation": [],
"authenticated-orcid": false,
"family": "Aydin",
"given": "Tahacan",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2959-0978",
"affiliation": [],
"authenticated-orcid": false,
"family": "Atli",
"given": "Zeynep",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8977-5931",
"affiliation": [],
"authenticated-orcid": false,
"family": "Balkan",
"given": "Ilker Inanc",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8632-2825",
"affiliation": [],
"authenticated-orcid": false,
"family": "Tabak",
"given": "Fehmi",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4077-1374",
"affiliation": [],
"authenticated-orcid": false,
"family": "Oztas",
"given": "Mert",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2082-4715",
"affiliation": [],
"authenticated-orcid": false,
"family": "Ozguler",
"given": "Yesim",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9561-2282",
"affiliation": [],
"authenticated-orcid": false,
"family": "Ugurlu",
"given": "Serdal",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1952-1135",
"affiliation": [],
"authenticated-orcid": false,
"family": "Hatemi",
"given": "Gulen",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0253-8368",
"affiliation": [],
"authenticated-orcid": false,
"family": "Melikoglu",
"given": "Melike",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8914-9690",
"affiliation": [],
"authenticated-orcid": false,
"family": "Fresko",
"given": "Izzet",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6625-1652",
"affiliation": [],
"authenticated-orcid": false,
"family": "Hamuryudan",
"given": "Vedat",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4965-2918",
"affiliation": [],
"authenticated-orcid": false,
"family": "Seyahi",
"given": "Emire",
"sequence": "additional"
}
],
"container-title": "Rheumatology International",
"container-title-short": "Rheumatol Int",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2021,
11,
25
]
],
"date-time": "2021-11-25T17:02:46Z",
"timestamp": 1637859766000
},
"deposited": {
"date-parts": [
[
2023,
1,
16
]
],
"date-time": "2023-01-16T08:33:32Z",
"timestamp": 1673858012000
},
"indexed": {
"date-parts": [
[
2023,
3,
14
]
],
"date-time": "2023-03-14T07:50:44Z",
"timestamp": 1678780244501
},
"is-referenced-by-count": 4,
"issue": "1",
"issued": {
"date-parts": [
[
2021,
11,
25
]
]
},
"journal-issue": {
"issue": "1",
"published-print": {
"date-parts": [
[
2022,
1
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.springer.com/tdm",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
11,
25
]
],
"date-time": "2021-11-25T00:00:00Z",
"timestamp": 1637798400000
}
},
{
"URL": "https://www.springer.com/tdm",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
11,
25
]
],
"date-time": "2021-11-25T00:00:00Z",
"timestamp": 1637798400000
}
}
],
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1007/s00296-021-05056-2.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/article/10.1007/s00296-021-05056-2/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/content/pdf/10.1007/s00296-021-05056-2.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"page": "101-113",
"prefix": "10.1007",
"published": {
"date-parts": [
[
2021,
11,
25
]
]
},
"published-online": {
"date-parts": [
[
2021,
11,
25
]
]
},
"published-print": {
"date-parts": [
[
2022,
1
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"key": "5056_CR1",
"unstructured": "https://www.worldometers.info/coronavirus/#countries. Accessed 7 September 2021"
},
{
"key": "5056_CR2",
"unstructured": "https://www.aa.com.tr/en/latest-on-coronavirus-outbreak/turkey-confirms-first-case-of-coronavirus/1761522. Accessed 11 March 2020"
},
{
"DOI": "10.1007/s10067-020-05334-7",
"author": "C Ferri",
"doi-asserted-by": "publisher",
"first-page": "3195",
"issue": "11",
"journal-title": "Clin Rheumatol.",
"key": "5056_CR3",
"unstructured": "Ferri C, Giuggioli D, Raimondo V, L’Andolina M, Tavoni A, Cecchetti R, Guiducci S, Ursini F, Caminiti M, Varcasia G, Gigliotti P, Pellegrini R, Olivo D, Colaci M, Murdaca G, Brittelli R, Mariano GP, Spinella A, Bellando-Randone S, Aiello V, Bilia S, Giannini D, Ferrari T, Caminiti R, Brusi V, Meliconi R, Fallahi P, Antonelli A, COVID-19 & ASD Italian Study Group (2020) COVID-19 and rheumatic autoimmune systemic diseases: report of a large Italian patients series. Clin Rheumatol. 39(11):3195–3204. https://doi.org/10.1007/s10067-020-05334-7",
"volume": "39",
"year": "2020"
},
{
"DOI": "10.1136/annrheumdis-2020-218296",
"author": "JL Pablos",
"doi-asserted-by": "publisher",
"first-page": "1544",
"issue": "12",
"journal-title": "Ann Rheum Dis.",
"key": "5056_CR4",
"unstructured": "Pablos JL, Galindo M, Carmona L, Lledó A, Retuerto M, Blanco R, Gonzalez-Gay MA, Martinez-Lopez D, Castrejón I, Alvaro-Gracia JM, Fernández Fernández D, Mera-Varela A, Manrique-Arija S, Mena Vázquez N, Fernandez-Nebro A, RIER Investigators Group; RIER investigators group (2020) Clinical outcomes of hospitalised patients with COVID-19 and chronic inflammatory and autoimmune rheumatic diseases: a multicentric matched cohort study. Ann Rheum Dis. 79(12):1544–1549. https://doi.org/10.1136/annrheumdis-2020-218296",
"volume": "79",
"year": "2020"
},
{
"DOI": "10.1046/j.1365-4362.2003.01893.x",
"author": "G Azizlerli",
"doi-asserted-by": "publisher",
"first-page": "803",
"issue": "10",
"journal-title": "Turkey Int J Dermatol",
"key": "5056_CR5",
"unstructured": "Azizlerli G, Köse AA, Sarica R, Gül A, Tutkun IT, Kulaç M, Tunç R, Urgancioğlu M, Dişçi R (2003) Prevalence of Behçet’s disease in Istanbul. Turkey Int J Dermatol 42(10):803–806. https://doi.org/10.1046/j.1365-4362.2003.01893.x",
"volume": "42",
"year": "2003"
},
{
"DOI": "10.1038/nrrheum.2017.208",
"author": "H Yazici",
"doi-asserted-by": "publisher",
"first-page": "107",
"issue": "2",
"journal-title": "Nat Rev Rheumatol.",
"key": "5056_CR6",
"unstructured": "Yazici H, Seyahi E, Hatemi G, Yazici Y (2018) Behçet syndrome: a contemporary view. Nat Rev Rheumatol. 14(2):107–119. https://doi.org/10.1038/nrrheum.2017.208 (Epub 2018 Jan 3. Erratum in: Nat Rev Rheumatol. 2018 Jan 24;14 (2):119)",
"volume": "14",
"year": "2018"
},
{
"DOI": "10.1056/NEJM199002013220501",
"author": "H Yazici",
"doi-asserted-by": "publisher",
"first-page": "281",
"issue": "5",
"journal-title": "N Engl J Med",
"key": "5056_CR7",
"unstructured": "Yazici H, Pazarli H, Barnes CG, Tüzün Y, Ozyazgan Y, Silman A, Serdaroğlu S, Oğuz V, Yurdakul S, Lovatt GE et al (1990) A controlled trial of azathioprine in Behçet’s syndrome. N Engl J Med 322(5):281–285. https://doi.org/10.1056/NEJM199002013220501 (PMID: 2404204)",
"volume": "322",
"year": "1990"
},
{
"DOI": "10.1093/rheumatology/kei165",
"author": "C Mat",
"doi-asserted-by": "publisher",
"first-page": "348",
"issue": "3",
"journal-title": "Rheumatology (Oxford)",
"key": "5056_CR8",
"unstructured": "Mat C, Yurdakul S, Uysal S, Gogus F, Ozyazgan Y, Uysal O, Fresko I, Yazici H (2006) A double-blind trial of depot corticosteroids in Behçet’s syndrome. Rheumatology (Oxford) 45(3):348–352. https://doi.org/10.1093/rheumatology/kei165 (Epub 2005 Nov 1 PMID: 16263779)",
"volume": "45",
"year": "2006"
},
{
"DOI": "10.1002/art.21231",
"author": "I Tugal-Tutkun",
"doi-asserted-by": "publisher",
"first-page": "2478",
"issue": "8",
"journal-title": "Arthritis Rheum",
"key": "5056_CR9",
"unstructured": "Tugal-Tutkun I, Mudun A, Urgancioglu M, Kamali S, Kasapoglu E, Inanc M, Gül A (2005) Efficacy of infliximab in the treatment of uveitis that is resistant to treatment with the combination of azathioprine, cyclosporine, and corticosteroids in Behçet’s disease: an open-label trial. Arthritis Rheum 52(8):2478–2484. https://doi.org/10.1002/art.21231 (PMID: 16052571)",
"volume": "52",
"year": "2005"
},
{
"DOI": "10.1002/art.40531",
"author": "G Emmi",
"doi-asserted-by": "publisher",
"first-page": "1500",
"issue": "9",
"journal-title": "Arthritis Rheumatol",
"key": "5056_CR10",
"unstructured": "Emmi G, Vitale A, Silvestri E, Boddi M, Becatti M, Fiorillo C, Fabiani C, Frediani B, Emmi L, Di Scala G, Goldoni M, Bettiol A, Vaglio A, Cantarini L, Prisco D (2018) Adalimumab-based treatment versus disease-modifying antirheumatic drugs for venous thrombosis in Behçet’s Syndrome: a Retrospective Study of Seventy Patients With Vascular Involvement. Arthritis Rheumatol 70(9):1500–1507. https://doi.org/10.1002/art.40531 (Epub 2018 Jul 19 PMID: 29676522)",
"volume": "70",
"year": "2018"
},
{
"DOI": "10.1016/j.jaut.2015.06.005",
"author": "H Vallet",
"doi-asserted-by": "publisher",
"first-page": "67",
"journal-title": "J Autoimmun",
"key": "5056_CR11",
"unstructured": "Vallet H, Riviere S, Sanna A, Deroux A, Moulis G, Addimanda O, Salvarani C, Lambert M, Bielefeld P, Seve P, Sibilia J, Pasquali J, Fraison J, Marie I, Perard L, Bouillet L, Cohen F, Sene D, Schoindre Y, Lidove O, Le Hoang P, Hachulla E, Fain O, Mariette X, Papo T, Wechsler B, Bodaghi B, Rigon MR, Cacoub P, Saadoun D, French Behçet Network (2015) Efficacy of anti-TNF alpha in severe and/or refractory Behçet’s disease: Multicenter study of 124 patients. J Autoimmun 62:67–74. https://doi.org/10.1016/j.jaut.2015.06.005",
"volume": "62",
"year": "2015"
},
{
"DOI": "10.1002/1529-0131(200111)44:11<2686::aid-art448>3.0.co;2-h",
"author": "S Yurdakul",
"doi-asserted-by": "publisher",
"first-page": "2686",
"issue": "11",
"journal-title": "Arthritis Rheum",
"key": "5056_CR12",
"unstructured": "Yurdakul S, Mat C, Tüzün Y, Ozyazgan Y, Hamuryudan V, Uysal O, Senocak M, Yazici H (2001) A double-blind trial of colchicine in Behçet’s syndrome. Arthritis Rheum 44(11):2686–2692. https://doi.org/10.1002/1529-0131(200111)44:11%3c2686::aid-art448%3e3.0.co;2-h (PMID: 11710724)",
"volume": "44",
"year": "2001"
},
{
"DOI": "10.1007/s10165-009-0200-2",
"author": "F Davatchi",
"doi-asserted-by": "publisher",
"first-page": "542",
"issue": "5",
"journal-title": "Mod Rheumatol",
"key": "5056_CR13",
"unstructured": "Davatchi F, Sadeghi Abdollahi B, Tehrani Banihashemi A, Shahram F, Nadji A, Shams H, Chams-Davatchi C (2009) Colchicine versus placebo in Behçet’s disease: randomized, double-blind, controlled crossover trial. Mod Rheumatol 19(5):542–549. https://doi.org/10.1007/s10165-009-0200-2 (Epub 2009 Jul 14 PMID: 19597921)",
"volume": "19",
"year": "2009"
},
{
"DOI": "10.1007/s11739-020-02427-8",
"author": "B Yurttaş",
"doi-asserted-by": "publisher",
"first-page": "1567",
"issue": "8",
"journal-title": "Intern Emerg Med",
"key": "5056_CR14",
"unstructured": "Yurttaş B, Oztas M, Tunc A, Balkan İİ, Tabak OF, Hamuryudan V, Seyahi E (2020) Characteristics and outcomes of Behçet’s syndrome patients with Coronavirus Disease 2019: a case series of 10 patients. Intern Emerg Med 15(8):1567–1571. https://doi.org/10.1007/s11739-020-02427-8 (Epub 2020 Jul 9)",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.3389/fimmu.2021.651715",
"author": "SN Esatoglu",
"doi-asserted-by": "publisher",
"first-page": "651715",
"journal-title": "Front Immunol.",
"key": "5056_CR15",
"unstructured": "Esatoglu SN, Tascilar K, Babaoğlu H, Bes C, Yurttas B, Akar S, Pehlivan O, Akleylek C, Tecer D, Seyahi E, Yuce-Inel T, Alpay-Kanitez N, Bodakci E, Tekgoz E, Colak S, Bolek EC, Koca SS, Kalyoncu U, Icacan OC, Ugurlu S, Oz HE, Hamuryudan V, Hatemi G, Turkish Society for Rheumatology COVID-19 Registry Investigators (2021) COVID-19 among patients with inflammatory rheumatic diseases. Front Immunol. 12:651715. https://doi.org/10.3389/fimmu.2021.651715",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.55563/clinexprheumatol/pmnqmf",
"author": "I Mattioli",
"doi-asserted-by": "crossref",
"first-page": "47",
"issue": "5",
"journal-title": "Clin Exp Rheumatol.",
"key": "5056_CR16",
"unstructured": "Mattioli I, Bettiol A, Silvestri E, Urban ML, Palermo A, Fagni F, Malandrino D, Del Bianco A, Prisco D, Emmi G (2021) Prevalence and clinical course of SARS-CoV-2 infection in patients with Behçet’s syndrome. Clin Exp Rheumatol. 132(5):47–50 (Epub 2021 Jun 9. PMID: 34128795.)",
"volume": "132",
"year": "2021"
},
{
"DOI": "10.1136/annrheumdis-2020-217778",
"author": "G Espinosa",
"doi-asserted-by": "publisher",
"journal-title": "Ann Rheum Dis",
"key": "5056_CR17",
"unstructured": "Espinosa G, Araujo O, Amaro S, Bodro M, Moreno PJ, Moreno R, Ugarte A, Cervera R (2020) COVID-19 and Behçet’s disease: clinical case series. Ann Rheum Dis. https://doi.org/10.1136/annrheumdis-2020-217778",
"year": "2020"
},
{
"DOI": "10.1111/jdv.17325",
"author": "CC Zouboulis",
"doi-asserted-by": "publisher",
"first-page": "e541",
"issue": "9",
"journal-title": "J Eur Acad Dermatol Venereol",
"key": "5056_CR18",
"unstructured": "Zouboulis CC, van Laar JAM, Schirmer M, Emmi G, Fortune F, Gül A, Kirino Y, Lee ES, Sfikakis PP, Shahram F, Wallace GR (2021) Adamantiades-Behçet’s disease (Behçet’s disease) and COVID-19. J Eur Acad Dermatol Venereol 35(9):e541–e543. https://doi.org/10.1111/jdv.17325",
"volume": "35",
"year": "2021"
},
{
"key": "5056_CR19",
"unstructured": "https://covid19asi.saglik.gov.tr/TR-77707/asi-uygulanacak-grup-siralamasi.html. Accessed 27 March 2021"
},
{
"key": "5056_CR20",
"unstructured": "https://covid19.saglik.gov.tr/TR-66301/covid-19-rehberi.html. Accessed 2020˗2021"
},
{
"DOI": "10.1016/j.autrev.2020.102575",
"author": "G Emmi",
"doi-asserted-by": "publisher",
"issue": "7",
"journal-title": "Autoimmun Rev",
"key": "5056_CR21",
"unstructured": "Emmi G, Bettiol A, Mattioli I, Silvestri E, Di Scala G, Urban ML, Vaglio A, Prisco D (2020) SARS-CoV-2 infection among patients with systemic autoimmune diseases. Autoimmun Rev 19(7):102575. https://doi.org/10.1016/j.autrev.2020.102575",
"volume": "19",
"year": "2020"
},
{
"author": "WW Daniel",
"edition": "7",
"key": "5056_CR22",
"unstructured": "Daniel WW (1999) Biostatistics: a foundation for analysis in the health sciences, 7th edn. Wiley, New York",
"volume-title": "Biostatistics: a foundation for analysis in the health sciences",
"year": "1999"
},
{
"key": "5056_CR23",
"unstructured": "https://covid19.saglik.gov.tr/TR-66935/genel-koronavirus-tablosu.html. Accessed September 2021"
},
{
"key": "5056_CR24",
"unstructured": "https://data.tuik.gov.tr/Bulten/Index?p=37210. Accessed September 2021"
},
{
"DOI": "10.1016/S2665-9913(20)30227-7",
"author": "J Zhong",
"doi-asserted-by": "publisher",
"first-page": "e557",
"issue": "9",
"journal-title": "Lancet Rheumatol",
"key": "5056_CR25",
"unstructured": "Zhong J, Shen G, Yang H, Huang A, Chen X, Dong L, Wu B, Zhang A, Su L, Hou X, Song S, Li H, Zhou W, Zhou T, Huang Q, Chu A, Braunstein Z, Rao X, Ye C, Dong L (2020) COVID-19 in patients with rheumatic disease in Hubei province, China: a multicentre retrospective observational study. Lancet Rheumatol 2(9):e557–e564. https://doi.org/10.1016/S2665-9913(20)30227-7",
"volume": "2",
"year": "2020"
},
{
"DOI": "10.1136/annrheumdis-2020-218946",
"author": "S Akiyama",
"doi-asserted-by": "publisher",
"journal-title": "Ann Rheum Dis",
"key": "5056_CR26",
"unstructured": "Akiyama S, Hamdeh S, Micic D, Sakuraba A (2020) Prevalence and clinical outcomes of COVID-19 in patients with autoimmune diseases: a systematic review and meta-analysis. Ann Rheum Dis. https://doi.org/10.1136/annrheumdis-2020-218946",
"year": "2020"
},
{
"DOI": "10.1016/S2665-9913(21)00151-X",
"author": "YH Shin",
"doi-asserted-by": "publisher",
"first-page": "e698",
"issue": "10",
"journal-title": "Lancet Rheumatol",
"key": "5056_CR27",
"unstructured": "Shin YH, Shin JI, Moon SY, Jin HY, Kim SY, Yang JM, Cho SH, Kim S, Lee M, Park Y, Kim MS, Won HH, Hong SH, Kronbichler A, Koyanagi A, Jacob L, Smith L, Lee KH, Suh DI, Lee SW, Yon DK (2021) Autoimmune inflammatory rheumatic diseases and COVID-19 outcomes in South Korea: a nationwide cohort study. Lancet Rheumatol 3(10):e698–e706. https://doi.org/10.1016/S2665-9913(21)00151-X",
"volume": "3",
"year": "2021"
},
{
"DOI": "10.1007/s00296-020-04626-0",
"author": "E Seyahi",
"doi-asserted-by": "publisher",
"first-page": "1229",
"issue": "8",
"journal-title": "Rheumatol Int",
"key": "5056_CR28",
"unstructured": "Seyahi E, Poyraz BC, Sut N, Akdogan S, Hamuryudan V (2020) The psychological state and changes in the routine of the patients with rheumatic diseases during the coronavirus disease (COVID-19) outbreak in Turkey: a web-based cross-sectional survey. Rheumatol Int 40(8):1229–1238. https://doi.org/10.1007/s00296-020-04626-0",
"volume": "40",
"year": "2020"
},
{
"DOI": "10.1177/1076029620938149",
"author": "W Miesbach",
"doi-asserted-by": "publisher",
"journal-title": "Clin Appl Thromb Hemost",
"key": "5056_CR29",
"unstructured": "Miesbach W, Makris M (2020) COVID-19: coagulopathy, risk of thrombosis, and the rationale for anticoagulation. Clin Appl Thromb Hemost. https://doi.org/10.1177/1076029620938149 (PMID: 32677459; PMCID: PMC7370334)",
"year": "2020"
},
{
"DOI": "10.1016/S2665-9913(21)00003-5",
"author": "P Mehta",
"doi-asserted-by": "publisher",
"first-page": "e171",
"issue": "3",
"journal-title": "Lancet Rheumatol.",
"key": "5056_CR30",
"unstructured": "Mehta P, Haskard DO, Laffan MA, Chambers RC, Hunt BJ (2021) Thromboses and COVID-19: reducing inflammation in addition to thromboprophylaxis. Lancet Rheumatol. 3(3):e171–e172. https://doi.org/10.1016/S2665-9913(21)00003-5 (Epub 2021 Jan 7. PMID: 33521654; PMCID: PMC7832098)",
"volume": "3",
"year": "2021"
},
{
"DOI": "10.1371/journal.pmed.1003379",
"author": "CT Rentsch",
"doi-asserted-by": "publisher",
"issue": "9",
"journal-title": "PLoS Med.",
"key": "5056_CR31",
"unstructured": "Rentsch CT, Kidwai-Khan F, Tate JP, Park LS, King JT Jr, Skanderson M, Hauser RG, Schultze A, Jarvis CI, Holodniy M, Lo RV 3rd, Akgün KM, Crothers K, Taddei TH, Freiberg MS, Justice AC (2020) Patterns of COVID-19 testing and mortality by race and ethnicity among United States veterans: a nationwide cohort study. PLoS Med. 17(9):e1003379. https://doi.org/10.1371/journal.pmed.1003379 (PMID: 32960880; PMCID: PMC7508372)",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0243414",
"author": "JA Trubiano",
"doi-asserted-by": "publisher",
"issue": "12",
"journal-title": "PLoS ONE",
"key": "5056_CR32",
"unstructured": "Trubiano JA, Vogrin S, Smibert OC, Marhoon N, Alexander AA, Chua KYL, James FL, Jones NRL, Grigg SE, Xu CLH, Moini N, Stanley SR, Birrell MT, Rose MT, Gordon CL, Kwong JC, Holmes NE (2020) COVID-MATCH65-A prospectively derived clinical decision rule for severe acute respiratory syndrome coronavirus 2. PLoS ONE 15(12):e0243414. https://doi.org/10.1371/journal.pone.0243414",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1111/add.15276",
"author": "D Simons",
"doi-asserted-by": "publisher",
"first-page": "1319",
"issue": "6",
"journal-title": "Addiction",
"key": "5056_CR33",
"unstructured": "Simons D, Shahab L, Brown J, Perski O (2021) The association of smoking status with SARS-CoV-2 infection, hospitalization and mortality from COVID-19: a living rapid evidence review with Bayesian meta-analyses (version 7). Addiction 116(6):1319–1368. https://doi.org/10.1111/add.15276",
"volume": "116",
"year": "2021"
},
{
"DOI": "10.1093/ntr/ntaa121",
"author": "P Tsigaris",
"doi-asserted-by": "publisher",
"journal-title": "Nicotine Tob Res",
"key": "5056_CR34",
"unstructured": "Tsigaris P, Teixeira da Silva JA (2020) Smoking Prevalence and COVID-19 in Europe. Nicotine Tob Res. https://doi.org/10.1093/ntr/ntaa121",
"year": "2020"
},
{
"DOI": "10.3390/ijerph17207394",
"author": "J González-Rubio",
"doi-asserted-by": "publisher",
"first-page": "7394",
"issue": "20",
"journal-title": "Int J Environ Res Public Health",
"key": "5056_CR35",
"unstructured": "González-Rubio J, Navarro-López C, López-Nájera E, López-Nájera A, Jiménez-Díaz L, Navarro-López JD, Nájera A (2020) A systematic review and meta-analysis of hospitalised current smokers and COVID-19. Int J Environ Res Public Health 17(20):7394. https://doi.org/10.3390/ijerph17207394",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.1177/2040622320935765",
"author": "K Farsalinos",
"doi-asserted-by": "publisher",
"first-page": "204062232093576",
"issue": "11",
"journal-title": "Ther Adv Chronic Dis",
"key": "5056_CR36",
"unstructured": "Farsalinos K, Barbouni A, Poulas K, Polosa R, Caponnetto P, Niaura R (2020) Current smoking, former smoking, and adverse outcome among hospitalized COVID-19 patients: a systematic review and meta-analysis. Ther Adv Chronic Dis 25(11):2040622320935765. https://doi.org/10.1177/2040622320935765",
"volume": "25",
"year": "2020"
},
{
"DOI": "10.1183/13993003.01340-2020",
"author": "JM Leung",
"doi-asserted-by": "publisher",
"first-page": "2001340",
"issue": "6",
"journal-title": "Eur Respir J",
"key": "5056_CR37",
"unstructured": "Leung JM, Yang CX, Sin DD (2020) Reply to: “Current smoking is not associated with COVID-19.” Eur Respir J 55(6):2001340. https://doi.org/10.1183/13993003.01340-2020",
"volume": "55",
"year": "2020"
},
{
"DOI": "10.1002/jmv.26389",
"author": "RK Reddy",
"doi-asserted-by": "publisher",
"first-page": "1045",
"issue": "2",
"journal-title": "J Med Virol",
"key": "5056_CR38",
"unstructured": "Reddy RK, Charles WN, Sklavounos A, Dutt A, Seed PT, Khajuria A (2021) The effect of smoking on COVID-19 severity: a systematic review and meta-analysis. J Med Virol 93(2):1045–1056. https://doi.org/10.1002/jmv.26389",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1093/ntr/ntaa082",
"author": "R Patanavanich",
"doi-asserted-by": "publisher",
"first-page": "1653",
"issue": "9",
"journal-title": "Nicotine Tob Res",
"key": "5056_CR39",
"unstructured": "Patanavanich R, Glantz SA (2020) Smoking is associated With COVID-19 progression: a meta-analysis. Nicotine Tob Res 22(9):1653–1656. https://doi.org/10.1093/ntr/ntaa082",
"volume": "22",
"year": "2020"
},
{
"DOI": "10.1136/thx.49.8.825",
"author": "JA Dye",
"doi-asserted-by": "publisher",
"first-page": "825",
"issue": "8",
"journal-title": "Thorax",
"key": "5056_CR40",
"unstructured": "Dye JA, Adler KB (1994) Effects of cigarette smoke on epithelial cells of the respiratory tract. Thorax 49(8):825–834. https://doi.org/10.1136/thx.49.8.825",
"volume": "49",
"year": "1994"
},
{
"DOI": "10.1183/13993003.01116-2020",
"author": "P Russo",
"doi-asserted-by": "publisher",
"first-page": "2001116",
"issue": "6",
"journal-title": "Eur Respir J",
"key": "5056_CR41",
"unstructured": "Russo P, Bonassi S, Giacconi R, Malavolta M, Tomino C, Maggi F (2020) COVID-19 and smoking: is nicotine the hidden link? Eur Respir J 55(6):2001116. https://doi.org/10.1183/13993003.01116-2020",
"volume": "55",
"year": "2020"
},
{
"DOI": "10.12968/hmed.2008.69.10.31317",
"author": "DS Yang",
"doi-asserted-by": "publisher",
"first-page": "575",
"issue": "10",
"journal-title": "Br J Hosp Med (Lond)",
"key": "5056_CR42",
"unstructured": "Yang DS, Taylor SR, Lightman SL (2008) Interferon-alpha in the management of patients with Behçet’s disease. Br J Hosp Med (Lond) 69(10):575–579. https://doi.org/10.12968/hmed.2008.69.10.31317",
"volume": "69",
"year": "2008"
},
{
"author": "L Lai",
"first-page": "255",
"issue": "3",
"journal-title": "Int J Nanomedicine.",
"key": "5056_CR43",
"unstructured": "Lai L, Hui CK, Leung N, Lau GK (2006) Pegylated interferon alpha-2a (40 kDa) in the treatment of chronic hepatitis B. Int J Nanomedicine. 1(3):255–62 (PMID: 17717966; PMCID: PMC2426802)",
"volume": "1",
"year": "2006"
},
{
"DOI": "10.1016/j.bpg.2012.09.013",
"author": "JJ Feld",
"doi-asserted-by": "publisher",
"first-page": "429",
"issue": "4",
"journal-title": "Best Pract Res Clin Gastroenterol",
"key": "5056_CR44",
"unstructured": "Feld JJ (2012) Treatment indication and response to standard of care with peginterferon and ribavirin in acute and chronic HCV infection. Best Pract Res Clin Gastroenterol 26(4):429–444. https://doi.org/10.1016/j.bpg.2012.09.013",
"volume": "26",
"year": "2012"
},
{
"DOI": "10.3389/fimmu.2020.615275.Erratumfor:FrontImmunol.2020May15;11:1061",
"author": "Q Zhou",
"doi-asserted-by": "publisher",
"issue": "11",
"journal-title": "Front Immunol",
"key": "5056_CR45",
"unstructured": "Zhou Q, Chen V, Shannon CP, Wei XS, Xiang X, Wang X, Wang ZH, Tebbutt SJ, Kollmann TR, Fish EN (2020) Corrigendum: interferon-α2b treatment for COVID-19. Front Immunol 27(11):615275. https://doi.org/10.3389/fimmu.2020.615275.Erratumfor:FrontImmunol.2020May15;11:1061",
"volume": "27",
"year": "2020"
},
{
"DOI": "10.1001/jama.290.24.3222",
"author": "MR Loutfy",
"doi-asserted-by": "publisher",
"first-page": "3222",
"issue": "24",
"journal-title": "JAMA",
"key": "5056_CR46",
"unstructured": "Loutfy MR, Blatt LM, Siminovitch KA, Ward S, Wolff B, Lho H, Pham DH, Deif H, LaMere EA, Chang M, Kain KC, Farcas GA, Ferguson P, Latchford M, Levy G, Dennis JW, Lai EK, Fish EN (2003) Interferon alfacon-1 plus corticosteroids in severe acute respiratory syndrome: a preliminary study. JAMA 290(24):3222–3228. https://doi.org/10.1001/jama.290.24.3222",
"volume": "290",
"year": "2003"
},
{
"DOI": "10.1126/science.abd4570",
"author": "Q Zhang",
"doi-asserted-by": "publisher",
"journal-title": "Science.",
"key": "5056_CR47",
"unstructured": "Zhang Q, Bastard P, Liu Z et al (2020) Inborn errors of type I IFN immunity in patients with life-threatening COVID-19. Science. https://doi.org/10.1126/science.abd4570",
"year": "2020"
},
{
"DOI": "10.1126/science.abc6027",
"author": "J Hadjadj",
"doi-asserted-by": "publisher",
"first-page": "718",
"issue": "6504",
"journal-title": "Science",
"key": "5056_CR48",
"unstructured": "Hadjadj J, Yatim N, Barnabei L, Corneau A, Boussier J, Smith N, Péré H, Charbit B, Bondet V, Chenevier-Gobeaux C, Breillat P, Carlier N, Gauzit R, Morbieu C, Pène F, Marin N, Roche N, Szwebel TA, Merkling SH, Treluyer JM, Veyer D, Mouthon L, Blanc C, Tharaux PL, Rozenberg F, Fischer A, Duffy D, Rieux-Laucat F, Kernéis S, Terrier B (2020) Impaired type I interferon activity and inflammatory responses in severe COVID-19 patients. Science 369(6504):718–724. https://doi.org/10.1126/science.abc6027",
"volume": "369",
"year": "2020"
},
{
"DOI": "10.2174/1381612824666180123110042",
"author": "C Angelidis",
"doi-asserted-by": "publisher",
"first-page": "659",
"issue": "6",
"journal-title": "Curr Pharm Des",
"key": "5056_CR49",
"unstructured": "Angelidis C, Kotsialou Z, Kossyvakis C, Vrettou AR, Zacharoulis A, Kolokathis F, Kekeris V, Giannopoulos G (2018) Colchicine Pharmacokinetics and Mechanism of Action. Curr Pharm Des 24(6):659–663. https://doi.org/10.2174/1381612824666180123110042",
"volume": "24",
"year": "2018"
},
{
"DOI": "10.1016/j.ejim.2010.09.010",
"author": "G Cocco",
"doi-asserted-by": "publisher",
"first-page": "503",
"issue": "6",
"journal-title": "Eur J Intern Med.",
"key": "5056_CR50",
"unstructured": "Cocco G, Chu DC, Pandolfi S (2010) Colchicine in clinical medicine. A guide for internists. Eur J Intern Med. 21(6):503–8. https://doi.org/10.1016/j.ejim.2010.09.010",
"volume": "21",
"year": "2010"
},
{
"DOI": "10.1002/cmdc.201800641",
"author": "M Richter",
"doi-asserted-by": "publisher",
"first-page": "469",
"issue": "4",
"journal-title": "ChemMedChem",
"key": "5056_CR51",
"unstructured": "Richter M, Boldescu V, Graf D, Streicher F, Dimoglo A, Bartenschlager R, Klein CD (2019) Synthesis, biological evaluation, and molecular docking of combretastatin and colchicine derivatives and their hCE1-Activated Prodrugs as Antiviral Agents. ChemMedChem 14(4):469–483. https://doi.org/10.1002/cmdc.201800641",
"volume": "14",
"year": "2019"
},
{
"DOI": "10.1001/jamanetworkopen.2020.13136",
"author": "SG Deftereos",
"doi-asserted-by": "publisher",
"first-page": "2013136",
"issue": "6",
"journal-title": "JAMA Netw Open.",
"key": "5056_CR52",
"unstructured": "Deftereos SG, Giannopoulos G, Vrachatis DA, Siasos GD, Giotaki SG, Gargalianos P, Metallidis S, Sianos G, Baltagiannis S, Panagopoulos P, Dolianitis K, Randou E, Syrigos K, Kotanidou A, Koulouris NG, Milionis H, Sipsas N, Gogos C, Tsoukalas G, Olympios CD, Tsagalou E, Migdalis I, Gerakari S, Angelidis C, Alexopoulos D, Davlouros P, Hahalis G, Kanonidis I, Katritsis D, Kolettis T, Manolis AS, Michalis L, Naka KK, Pyrgakis VN, Toutouzas KP, Triposkiadis F, Tsioufis K, Vavouranakis E, Martinèz-Dolz L, Reimers B, Stefanini GG, Cleman M, Goudevenos J, Tsiodras S, Tousoulis D, Iliodromitis E, Mehran R, Dangas G, Stefanadis C, GRECCO-19 investigators (2020) Effect of Colchicine vs Standard Care on Cardiac and Inflammatory Biomarkers and Clinical Outcomes in Patients Hospitalized With Coronavirus Disease 2019: The GRECCO-19 Randomized Clinical Trial. JAMA Netw Open. 3(6):2013136. https://doi.org/10.1001/jamanetworkopen.2020.13136",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0248276",
"author": "L Manenti",
"doi-asserted-by": "publisher",
"issue": "3",
"journal-title": "PLoS ONE",
"key": "5056_CR53",
"unstructured": "Manenti L, Maggiore U, Fiaccadori E, Meschi T, Antoni AD, Nouvenne A, Ticinesi A, Cerundolo N, Prati B, Delsante M, Gandoflini I, Donghi L, Gentile M, Farina MT, Oliva V, Zambrano C, Regolisti G, Palmisano A, Caminiti C, Cocchi E, Ferrari C, Riella LV, Cravedi P, Peruzzi L (2021) Reduced mortality in COVID-19 patients treated with colchicine: results from a retrospective, observational study. PLoS ONE 16(3):e0248276. https://doi.org/10.1371/journal.pone.0248276",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.1136/rmdopen-2020-001455",
"author": "MI Lopes",
"doi-asserted-by": "publisher",
"issue": "1",
"journal-title": "RMD Open",
"key": "5056_CR54",
"unstructured": "Lopes MI, Bonjorno LP, Giannini MC, Amaral NB, Menezes PI, Dib SM, Gigante SL, Benatti MN, Rezek UC, Emrich-Filho LL, Sousa BAA, Almeida SCL, Luppino Assad R, Veras FP, Schneider A, Rodrigues TS, Leiria LOS, Cunha LD, Alves-Filho JC, Cunha TM, Arruda E, Miranda CH, Pazin-Filho A, Auxiliadora-Martins M, Borges MC, Fonseca BAL, Bollela VR, Del-Ben CM, Cunha FQ, Zamboni DS, Santana RC, Vilar FC, Louzada-Junior P, Oliveira RDR (2021) Beneficial effects of colchicine for moderate to severe COVID-19: a randomised, double-blinded, placebo-controlled clinical trial. RMD Open 7(1):e001455. https://doi.org/10.1136/rmdopen-2020-001455",
"volume": "7",
"year": "2021"
},
{
"DOI": "10.1016/S2213-2600(21)00222-8",
"author": "JC Tardif",
"doi-asserted-by": "publisher",
"first-page": "924",
"issue": "8",
"journal-title": "Lancet Respir Med.",
"key": "5056_CR55",
"unstructured": "Tardif JC, Bouabdallaoui N, L’Allier PL, Gaudet D, Shah B, Pillinger MH, Lopez-Sendon J, da Luz P, Verret L, Audet S, Dupuis J, Denault A, Pelletier M, Tessier PA, Samson S, Fortin D, Tardif JD, Busseuil D, Goulet E, Lacoste C, Dubois A, Joshi AY, Waters DD, Hsue P, Lepor NE, Lesage F, Sainturet N, Roy-Clavel E, Bassevitch Z, Orfanos A, Stamatescu G, Grégoire JC, Busque L, Lavallée C, Hétu PO, Paquette JS, Deftereos SG, Levesque S, Cossette M, Nozza A, Chabot-Blanchet M, Dubé MP, Guertin MC, Boivin G, COLCORONA Investigators (2021) Colchicine for community-treated patients with COVID-19 (COLCORONA): a phase 3, randomised, double-blinded, adaptive, placebo-controlled, multicentre trial. Lancet Respir Med. 9(8):924–932. https://doi.org/10.1016/S2213-2600(21)00222-8",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1016/j.autrev.2020.102566",
"author": "O Gendelman",
"doi-asserted-by": "publisher",
"issue": "7",
"journal-title": "Autoimmun Rev",
"key": "5056_CR56",
"unstructured": "Gendelman O, Amital H, Bragazzi NL, Watad A, Chodick G (2020) Continuous hydroxychloroquine or colchicine therapy does not prevent infection with SARS-CoV-2: Insights from a large healthcare database analysis. Autoimmun Rev 19(7):102566. https://doi.org/10.1016/j.autrev.2020.102566",
"volume": "19",
"year": "2020"
},
{
"DOI": "10.1177/1759720X211002684",
"author": "A Madrid-García",
"doi-asserted-by": "publisher",
"journal-title": "Ther Adv Musculoskelet Dis.",
"key": "5056_CR57",
"unstructured": "Madrid-García A, Pérez I, Colomer JI, León-Mateos L, Jover JA, Fernández-Gutiérrez B, Abásolo-Alcazar L, Rodríguez-Rodríguez L (2021) Influence of colchicine prescription in COVID-19-related hospital admissions: a survival analysis. Ther Adv Musculoskelet Dis. https://doi.org/10.1177/1759720X211002684",
"year": "2021"
},
{
"DOI": "10.1007/s00296-021-04809-3",
"author": "K Nas",
"doi-asserted-by": "publisher",
"first-page": "811",
"issue": "4",
"journal-title": "Rheumatol Int",
"key": "5056_CR58",
"unstructured": "Nas K, Eryilmaz N, Geyik MF, Altaş A (2021) COVID-19 in patients with familial Mediterranean fever treated with colchicine: case based review. Rheumatol Int 41(4):811–817. https://doi.org/10.1007/s00296-021-04809-3",
"volume": "41",
"year": "2021"
},
{
"DOI": "10.1136/annrheumdis-2020-218707",
"author": "R Bourguiba",
"doi-asserted-by": "publisher",
"journal-title": "Ann Rheum Dis",
"key": "5056_CR59",
"unstructured": "Bourguiba R, Delplanque M, Vinit C, Ackermann F, Savey L, Grateau G, Hentgen V, Georgin-Lavialle S (2020) Clinical course of COVID-19 in a cohort of 342 familial Mediterranean fever patients with a long-term treatment by colchicine in a French endemic area. Ann Rheum Dis. https://doi.org/10.1136/annrheumdis-2020-218707",
"year": "2020"
},
{
"DOI": "10.1038/s41584-020-00562-2.PMID:33339986;PMCID:PMC7747184",
"author": "KL Hyrich",
"doi-asserted-by": "publisher",
"first-page": "71",
"issue": "2",
"journal-title": "Nat Rev Rheumatol",
"key": "5056_CR60",
"unstructured": "Hyrich KL, Machado PM (2021) Rheumatic disease and COVID-19: epidemiology and outcomes. Nat Rev Rheumatol 17(2):71–72. https://doi.org/10.1038/s41584-020-00562-2.PMID:33339986;PMCID:PMC7747184",
"volume": "17",
"year": "2021"
},
{
"DOI": "10.1007/s00038-020-01390-7",
"author": "V Jain",
"doi-asserted-by": "publisher",
"first-page": "533",
"issue": "5",
"journal-title": "Int J Public Health",
"key": "5056_CR61",
"unstructured": "Jain V, Yuan JM (2020) Predictive symptoms and comorbidities for severe COVID-19 and intensive care unit admission: a systematic review and meta-analysis. Int J Public Health 65(5):533–546. https://doi.org/10.1007/s00038-020-01390-7",
"volume": "65",
"year": "2020"
}
],
"reference-count": 61,
"references-count": 61,
"relation": {},
"resource": {
"primary": {
"URL": "https://link.springer.com/10.1007/s00296-021-05056-2"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Immunology",
"Immunology and Allergy",
"Rheumatology"
],
"subtitle": [],
"title": "The incidence, clinical characteristics, and outcome of COVID-19 in a prospectively followed cohort of patients with Behçet’s syndrome",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "42"
}
