Influence of colchicine prescription in COVID-19-related hospital admissions: a survival analysis
et al., Therapeutic Advances in Musculoskeletal Disease, doi:10.1177/1759720x211002684, Jan 2021
Colchicine for COVID-19
5th treatment shown to reduce risk in
September 2020, now with p = 0.0000049 from 54 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 9,379 patients attending a rheumatology outpatient clinic in Spain, showing higher mortality and hospitalization with colchicine use, without statistical significance.
|
risk of death, 37.1% higher, HR 1.37, p = 0.57.
|
|
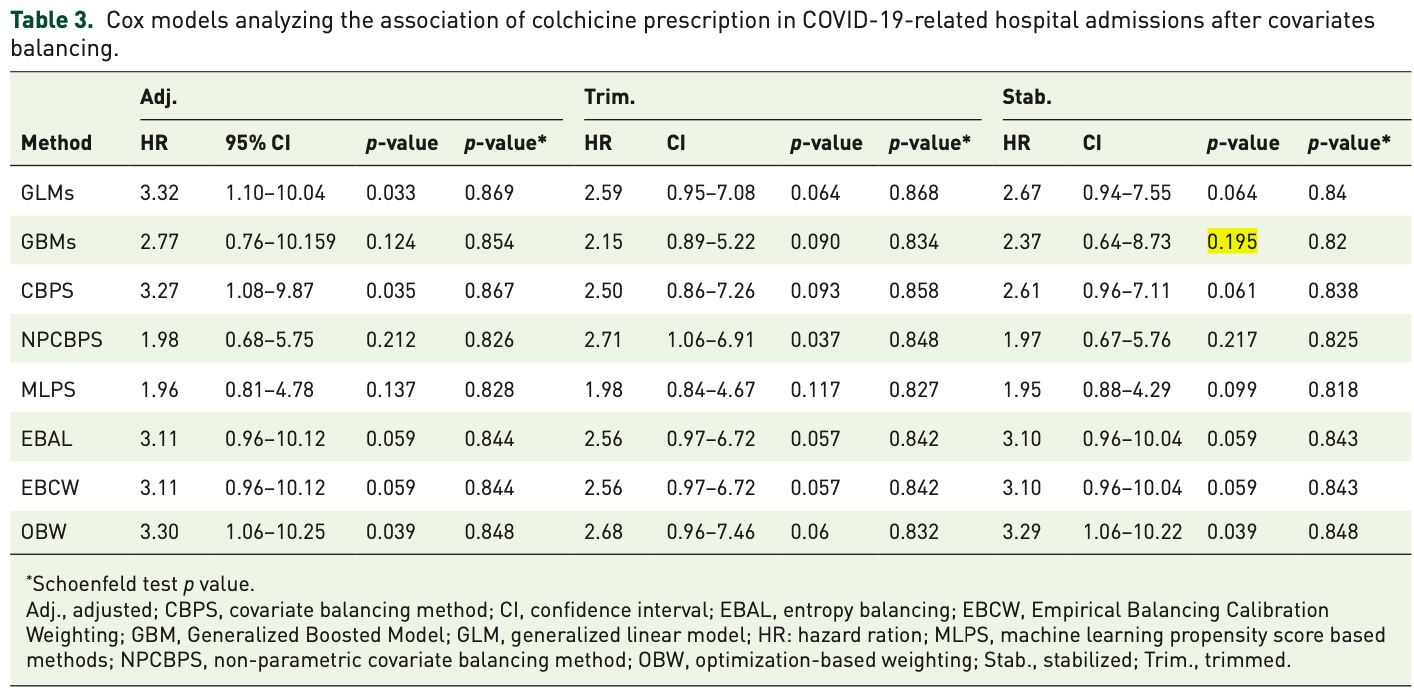
risk of hospitalization, 137.0% higher, HR 2.37, p = 0.20, GBM.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Madrid-García et al., 31 Jan 2021, retrospective, Spain, peer-reviewed, 8 authors, study period 1 March, 2020 - 20 May, 2020.
Influence of colchicine prescription in COVID-19-related hospital admissions: a survival analysis
Therapeutic Advances in Musculoskeletal Disease, doi:10.1177/1759720x211002684
Aims: To analyze the association between colchicine prescription and COVID-19-related hospital admissions in patients with rheumatic and musculoskeletal diseases (RMDs). Methods: Patients attending a rheumatology outpatient clinic from a tertiary care center in Madrid, Spain, from 1 September 2019 to 29 February 2020 were included. Patients were assigned as exposed or unexposed based on whether they were prescribed with colchicine in their last visit to the clinic during the 6 months before the start of the observation period. Treatment changes during the observation period were also considered. The primary outcome was COVID-19-related hospital admissions between 1 March and 20 May 2020. Secondary outcome included COVID-19-related mortality. Several weighting techniques for data balancing, based and non-based on the propensity score, followed by Cox regressions were performed to estimate the association of colchicine prescription on both outcomes. Discussion: The number of patients entered in the study was 9379, with 406 and 9002 exposed and unexposed follow-up periods, respectively. Generalized Boosted Models (GBMs) and Empirical Balancing Calibration Weighting (EBCW) methods showed the best balance for COVID-19-related hospital admissions. Colchicine prescription did not show a statistically significant association after covariable balancing (p-value = 0.195 and 0.059 for GBM and EBCW, respectively). Regarding mortality, the low number of events prevented a success variable balancing and analysis. Conclusion: Colchicine prescription does not play a significant protective or risk role in RMD patients regarding COVID-19-related hospital admissions. Our observations could support the maintenance of colchicine prescription in those patients already being treated, as it is not associated with a worse prognosis.
Author contributions LRR and LAA conceived and designed the study. IP, JIC, LLM, JAJ, and BFG collected data. AMG, LAA, and LRR performed the data analysis and interpreted the data. All of the authors were involved in the drafting and/or revising of the manuscript.
Conflict of interest statement The authors declare that there is no conflict of interest.
Funding The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Instituto de Salud Carlos III (ISCIII), Ministry of Health, Spain (CPII17/00014; PI18/01188; CP16/00916; and RD16/0012/0014) and cofounded by el Fondo
Ethics statement The study was approved by the Hospital Clínico San Carlos Ethics Committee (approval number 20/268-E-BS). This study was conducted according to the principles of the Declaration of Helsinki.
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Patient consent for publication Not required.
ORCID iDs
References
Bourguiba, Delplanque, Vinit, Clinical course of COVID-19 in a cohort of 342 familial Mediterranean fever patients with a long-term treatment by colchicine in a French endemic area, Ann Rheum Dis. Epub ahead of print, doi:10.1136/annrheumdis-2020-218707
Brunetti, Diawara, Tsai, Colchicine to weather the cytokine storm in hospitalized patients with COVID-19, J Clin Med. Epub ahead of print, doi:10.3390/jcm9092961
Clerkin, Fried, Raikhelkar, COVID-19 and cardiovascular disease, Circulation
Concato, Peduzzi, Holford, Importance of events per independent variable in proportional hazards analysis. I. Background, goals, and general strategy, J Clin Epidemiol
Coperchini, Chiovato, Croce, The cytokine storm in COVID-19: an overview of the involvement of the chemokine/chemokinereceptor system, Cytokine Growth Factor Rev
Della-Torre, Della-Torre, Kusanovic, Treating COVID-19 with colchicine in community healthcare setting, Clin Immunol
Fernandez-Gutierrez, COVID-19 with pulmonary involvement. An autoimmune disease of known cause, Reumatol Clin
Fernandez-Gutierrez, Leon, Madrid, Hospital admissions in inflammatory rheumatic diseases during the COVID-19 pandemic: incidence and role of disease modifying agents, medRxiv
Geleris, Sun, Platt, Observational study of hydroxychloroquine in hospitalized patients with Covid-19, N Engl J Med
Greifer, WeightIt: weighting for covariate balance in observational studies
Greifer, cobalt: covariate balance tables and plots
Hemkens, Ewald, Gloy, Colchicine for prevention of cardiovascular events, Cochrane database Syst Rev
Lopes, Bonjorno, Giannini, Beneficial effects of colchicine for moderate to severe COVID-19: an interim analysis of a randomized, double-blinded, placebo controlled clinical trial, medRxiv
López-Medina, Ladehesa-Pineda, Gómez-García, Treatment adherence during the COVID-19 pandemic and the impact of confinement on disease activity and emotional status: a survey in 644 rheumatic patients, Joint Bone Spine
López-Otero, López-Pais, Antúnez-Muiños, Asociación entre el daño miocárdico y el pronóstico de pacientes hospitalizados por COVID-19 con y sin cardiopatía. Registro CARDIOVID, Rev Española Cardiol. Epub ahead of print, doi:10.1016/j.recesp.2020.08.003
Mikuls, Johnson, Fraenkel, American College of Rheumatology guidance for the management of rheumatic disease in adult patients during the COVID-19 pandemic: Version 2, Arthritis Rheumatol, doi:10.1002/art.41437
Montealegre-Gómez, Garavito, Gómez-López, Colchicine: a potential therapeutic tool against COVID-19
Nuñez, Leon, Mucientes, Risk factors for hospital admissions related to COVID-19 in patients with autoimmune inflammatory rheumatic diseases, Ann Rheum Dis
Peduzzi, Concato, Feinstein, Importance of events per independent variable in proportional hazards regression analysis. II. Accuracy and precision of regression estimates, J Clin Epidemiol
Peduzzi, Concato, Kemper, A simulation study of the number of events per variable in logistic regression analysis, J Clin Epidemiol
Sandhu, Tieng, Chilimuri, A case control study to evaluate the impact of colchicine on patients admitted to the hospital with moderate to severe COVID-19 infection, Can J Infect Dis Med Microbiol
Scarsi, Piantoni, Colombo, Association between treatment with colchicine and improved survival in a single-centre cohort of adult hospitalised patients with COVID-19 pneumonia and acute respiratory distress syndrome, Ann Rheum Dis
Schneeweiss, Sensitivity analysis and external adjustment for unmeasured confounders in epidemiologic database studies of therapeutics, Pharmacoepidemiol Drug Saf
Shaffer, 15 drugs being tested to treat COVID-19 and how they would work, Nat Med. Epub ahead of print, doi:10.1038/d41591-020-00019-9
Stürmer, Schneeweiss, Avorn, Adjusting effect estimates for unmeasured confounding with validation data using propensity score calibration, Am J Epidemiol
Terkeltaub, Colchicine update: 2008, Semin Arthritis Rheum
Varshney, Wang, Bhatt, Characteristics of clinical trials evaluating cardiovascular therapies for coronavirus disease 2019 registered on ClinicalTrials.gov: a cross sectional analysis, Am Heart J. Epub ahead of print, doi:10.1016/j.ahj.2020.10.065
Xu, Han, Li, Effective treatment of severe COVID-19 patients with tocilizumab, Proc Natl Acad Sci U S A
Zheng, Ma, Zhang, COVID-19 and the cardiovascular system, Nat Rev Cardiol
DOI record:
{
"DOI": "10.1177/1759720x211002684",
"ISSN": [
"1759-720X",
"1759-7218"
],
"URL": "http://dx.doi.org/10.1177/1759720x211002684",
"abstract": "<jats:sec><jats:title>Aims:</jats:title><jats:p> To analyze the association between colchicine prescription and COVID-19-related hospital admissions in patients with rheumatic and musculoskeletal diseases (RMDs). </jats:p></jats:sec><jats:sec><jats:title>Methods:</jats:title><jats:p> Patients attending a rheumatology outpatient clinic from a tertiary care center in Madrid, Spain, from 1 September 2019 to 29 February 2020 were included. Patients were assigned as exposed or unexposed based on whether they were prescribed with colchicine in their last visit to the clinic during the 6 months before the start of the observation period. Treatment changes during the observation period were also considered. The primary outcome was COVID-19-related hospital admissions between 1 March and 20 May 2020. Secondary outcome included COVID-19-related mortality. Several weighting techniques for data balancing, based and non-based on the propensity score, followed by Cox regressions were performed to estimate the association of colchicine prescription on both outcomes. </jats:p></jats:sec><jats:sec><jats:title>Discussion:</jats:title><jats:p> The number of patients entered in the study was 9379, with 406 and 9002 exposed and unexposed follow-up periods, respectively. Generalized Boosted Models (GBMs) and Empirical Balancing Calibration Weighting (EBCW) methods showed the best balance for COVID-19-related hospital admissions. Colchicine prescription did not show a statistically significant association after covariable balancing ( p-value = 0.195 and 0.059 for GBM and EBCW, respectively). Regarding mortality, the low number of events prevented a success variable balancing and analysis. </jats:p></jats:sec><jats:sec><jats:title>Conclusion:</jats:title><jats:p> Colchicine prescription does not play a significant protective or risk role in RMD patients regarding COVID-19-related hospital admissions. Our observations could support the maintenance of colchicine prescription in those patients already being treated, as it is not associated with a worse prognosis. </jats:p></jats:sec><jats:sec><jats:title>Plain language title:</jats:title><jats:p> Colchicine influence in COVID-19-related hospital admissions </jats:p></jats:sec>",
"alternative-id": [
"10.1177/1759720X211002684"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-1591-0467",
"affiliation": [
{
"name": "Rheumatology Department, and Health Research Institute (IdISSC), Hospital Clínico San Carlos, Madrid, Spain"
},
{
"name": "Escuela Técnica Superior de Ingenieros de Telecomunicación (ETSIT), Universidad Politécnica de Madrid, Madrid, Spain"
}
],
"authenticated-orcid": false,
"family": "Madrid-García",
"given": "Alfredo",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Rheumatology Department, and Health Research Institute (IdISSC), Hospital Clínico San Carlos, Madrid, Spain"
}
],
"family": "Pérez",
"given": "Inés",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Rheumatology Department, and Health Research Institute (IdISSC), Hospital Clínico San Carlos, Madrid, Spain"
}
],
"family": "Colomer",
"given": "José Ignacio",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Rheumatology Department, and Health Research Institute (IdISSC), Hospital Clínico San Carlos, Madrid, Spain"
}
],
"family": "León-Mateos",
"given": "Leticia",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6126-8786",
"affiliation": [
{
"name": "Rheumatology Department, and Health Research Institute (IdISSC), Hospital Clínico San Carlos, Madrid, Spain"
}
],
"authenticated-orcid": false,
"family": "Jover",
"given": "Juan A",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Rheumatology Department, and Health Research Institute (IdISSC), Hospital Clínico San Carlos, Madrid, Spain"
}
],
"family": "Fernández-Gutiérrez",
"given": "Benjamín",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Rheumatology Department, and Health Research Institute (IdISSC), Hospital Clínico San Carlos, Madrid, Spain"
}
],
"family": "Abásolo-Alcazar",
"given": "Lydia",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2869-7861",
"affiliation": [
{
"name": "Rheumatology Department, and Health Research Institute (IdISSC), Hospital Clínico San Carlos, c\\ Prof. Martin Lagos s/n, Madrid, 28040, Spain"
}
],
"authenticated-orcid": false,
"family": "Rodríguez-Rodríguez",
"given": "Luis",
"sequence": "additional"
}
],
"container-title": "Therapeutic Advances in Musculoskeletal Disease",
"container-title-short": "Therapeutic Advances in Musculoskeletal",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"journals.sagepub.com"
]
},
"created": {
"date-parts": [
[
2021,
3,
26
]
],
"date-time": "2021-03-26T10:39:44Z",
"timestamp": 1616755184000
},
"deposited": {
"date-parts": [
[
2021,
6,
11
]
],
"date-time": "2021-06-11T01:10:18Z",
"timestamp": 1623373818000
},
"indexed": {
"date-parts": [
[
2023,
2,
24
]
],
"date-time": "2023-02-24T15:29:53Z",
"timestamp": 1677252593994
},
"is-referenced-by-count": 6,
"issued": {
"date-parts": [
[
2021,
1
]
]
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by-nc/4.0/",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
1,
1
]
],
"date-time": "2021-01-01T00:00:00Z",
"timestamp": 1609459200000
}
}
],
"link": [
{
"URL": "http://journals.sagepub.com/doi/pdf/10.1177/1759720X211002684",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "http://journals.sagepub.com/doi/full-xml/10.1177/1759720X211002684",
"content-type": "application/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "http://journals.sagepub.com/doi/pdf/10.1177/1759720X211002684",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "179",
"original-title": [],
"page": "1759720X2110026",
"prefix": "10.1177",
"published": {
"date-parts": [
[
2021,
1
]
]
},
"published-online": {
"date-parts": [
[
2021,
3,
26
]
]
},
"published-print": {
"date-parts": [
[
2021,
1
]
]
},
"publisher": "SAGE Publications",
"reference": [
{
"DOI": "10.1016/j.reuma.2020.04.001",
"doi-asserted-by": "publisher",
"key": "bibr1-1759720X211002684"
},
{
"DOI": "10.1016/j.cytogfr.2020.05.003",
"doi-asserted-by": "publisher",
"key": "bibr2-1759720X211002684"
},
{
"DOI": "10.1038/d41591-020-00019-9",
"doi-asserted-by": "publisher",
"key": "bibr3-1759720X211002684"
},
{
"DOI": "10.1056/NEJMoa2012410",
"doi-asserted-by": "publisher",
"key": "bibr4-1759720X211002684"
},
{
"DOI": "10.1073/pnas.2005615117",
"doi-asserted-by": "publisher",
"key": "bibr5-1759720X211002684"
},
{
"DOI": "10.1016/j.semarthrit.2008.08.006",
"doi-asserted-by": "publisher",
"key": "bibr6-1759720X211002684"
},
{
"author": "Hemkens LG",
"journal-title": "Cochrane database Syst Rev",
"key": "bibr7-1759720X211002684",
"volume": "1",
"year": "2016"
},
{
"author": "Fernandez-Gutierrez B",
"journal-title": "medRxiv",
"key": "bibr9-1759720X211002684",
"year": "2020"
},
{
"DOI": "10.1136/annrheumdis-2020-217984",
"doi-asserted-by": "publisher",
"key": "bibr10-1759720X211002684"
},
{
"DOI": "10.1016/0895-4356(95)00510-2",
"doi-asserted-by": "publisher",
"key": "bibr11-1759720X211002684"
},
{
"DOI": "10.1016/0895-4356(95)00048-8",
"doi-asserted-by": "publisher",
"key": "bibr12-1759720X211002684"
},
{
"DOI": "10.1016/S0895-4356(96)00236-3",
"doi-asserted-by": "publisher",
"key": "bibr13-1759720X211002684"
},
{
"DOI": "10.1155/2020/8865954",
"doi-asserted-by": "publisher",
"key": "bibr18-1759720X211002684"
},
{
"DOI": "10.1136/annrheumdis-2020-217712",
"doi-asserted-by": "publisher",
"key": "bibr19-1759720X211002684"
},
{
"DOI": "10.3390/jcm9092961",
"doi-asserted-by": "publisher",
"key": "bibr20-1759720X211002684"
},
{
"DOI": "10.1016/j.clim.2020.108490",
"doi-asserted-by": "publisher",
"key": "bibr21-1759720X211002684"
},
{
"author": "Lopes MIF",
"journal-title": "medRxiv",
"key": "bibr22-1759720X211002684",
"year": "2020"
},
{
"DOI": "10.1136/annrheumdis-2020-218707",
"doi-asserted-by": "publisher",
"key": "bibr23-1759720X211002684"
},
{
"DOI": "10.1016/j.reuma.2020.05.001",
"doi-asserted-by": "publisher",
"key": "bibr24-1759720X211002684"
},
{
"DOI": "10.1002/art.41437",
"doi-asserted-by": "publisher",
"key": "bibr25-1759720X211002684"
},
{
"DOI": "10.1038/s41569-020-0360-5",
"doi-asserted-by": "publisher",
"key": "bibr26-1759720X211002684"
},
{
"DOI": "10.1161/CIRCULATIONAHA.120.046941",
"doi-asserted-by": "publisher",
"key": "bibr27-1759720X211002684"
},
{
"DOI": "10.1016/j.recesp.2020.08.003",
"doi-asserted-by": "publisher",
"key": "bibr28-1759720X211002684"
},
{
"DOI": "10.1016/j.jbspin.2020.105085",
"doi-asserted-by": "publisher",
"key": "bibr29-1759720X211002684"
},
{
"DOI": "10.1093/aje/kwi192",
"doi-asserted-by": "publisher",
"key": "bibr30-1759720X211002684"
},
{
"DOI": "10.1002/pds.1200",
"doi-asserted-by": "publisher",
"key": "bibr31-1759720X211002684"
}
],
"reference-count": 26,
"references-count": 26,
"relation": {},
"resource": {
"primary": {
"URL": "http://journals.sagepub.com/doi/10.1177/1759720X211002684"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Orthopedics and Sports Medicine",
"Rheumatology"
],
"subtitle": [],
"title": "Influence of colchicine prescription in COVID-19-related hospital admissions: a survival analysis",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1177/sage-journals-update-policy",
"volume": "13"
}
