Clinical outcomes of patients hospitalized for COVID-19 and evidence-based on the pharmacological management reduce mortality in a region of the Colombian Caribbean
et al., Journal of Infection and Public Health, doi:10.1016/j.jiph.2021.02.013, Mar 2021
Colchicine for COVID-19
5th treatment shown to reduce risk in
September 2020, now with p = 0.0000049 from 54 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
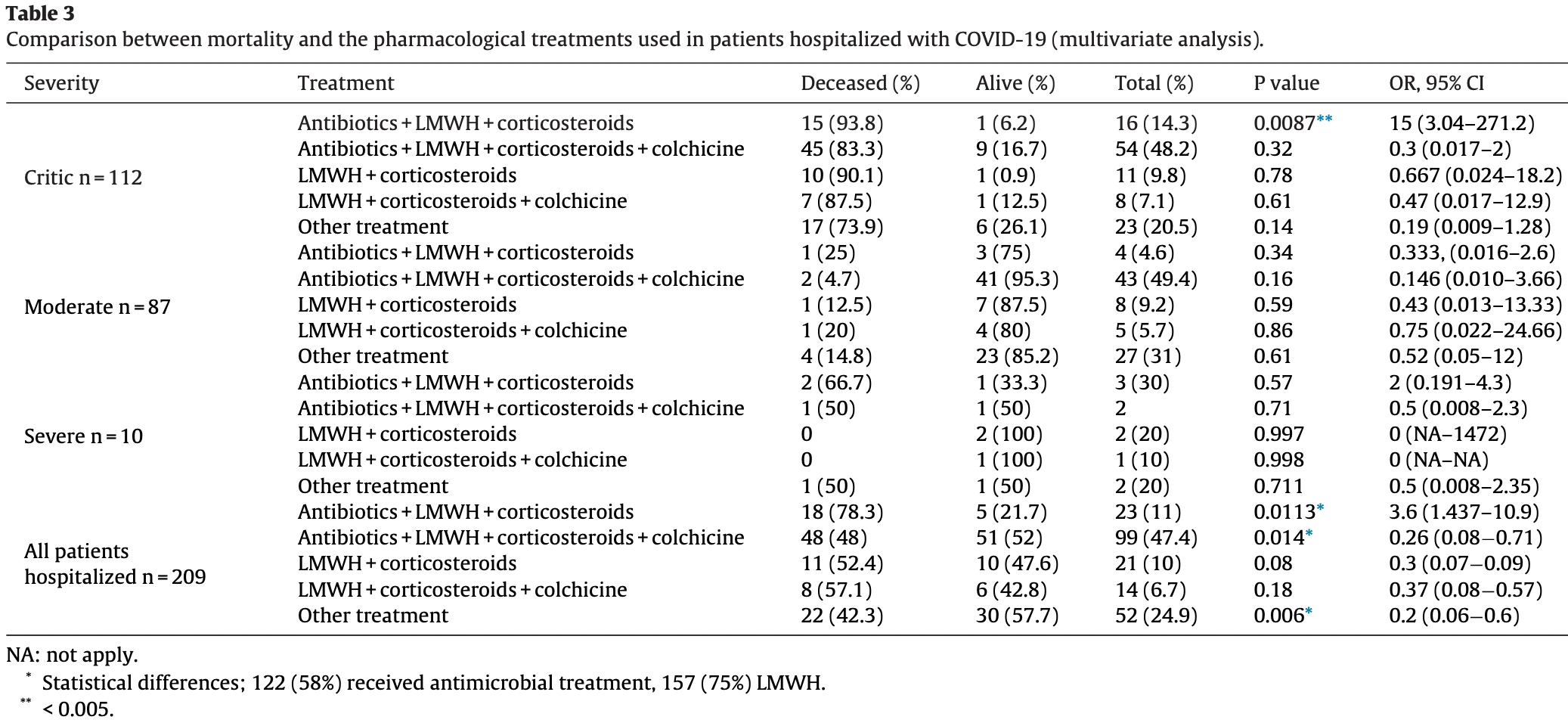
Retrospective 209 hospitalized patients in Colombia, showing lower mortality with antibiotics + LMWH + corticosteroids + colchicine in multivariable analysis.
This study is excluded in meta-analysis:
combined treatments may contribute more to the effect seen.
|
risk of death, 56.9% lower, RR 0.43, p = 0.01, treatment 48 of 99 (48.5%), control 59 of 110 (53.6%), adjusted per study, odds ratio converted to relative risk, multivariable.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
García-Posada et al., 6 Mar 2021, retrospective, Colombia, peer-reviewed, 8 authors, dosage not specified, this trial uses multiple treatments in the treatment arm (combined with antibiotics, LMWH, and corticosteroidsPERIOD:5/20-8/20) - results of individual treatments may vary.
Clinical outcomes of patients hospitalized for COVID-19 and evidence-based on the pharmacological management reduce mortality in a region of the Colombian Caribbean
Journal of Infection and Public Health, doi:10.1016/j.jiph.2021.02.013
Introduction: Despite the high volume of infections, some clinical aspects of this disease are still unknown. There are currently no studies in Colombia that describe the disease's clinical and treatment aspects in detail. Objective: Describe the characteristics and clinical management of a group of admitted patients with SARS-CoV-2 infection in a private clinic in Montería, Córdoba-Colombia. Patients and methods: A descriptive observational study was carried out between May and August 2020 in 209 hospitalized patients with a confirmed diagnosis of COVID-19. Upon admittance, clinical, sociodemographic characteristics, comorbidities, and complications were analyzed. Additionally, the effect of the following medications was described: 1-antibiotics (cefepime, piperacillin, tazobactam, meropenem, vancomycin) + low molecular weight heparin (LMWH) + corticosteroids (dexamethasone-methylprednisolone) + colchicine. 2-Antibiotic + LMWH + corticosteroids. 3-LMWH + corticosteroids. 4-LMWH + corticosteroids + colchicine. 5-Other treatments (Tocilizumab). Results: 107 (51%) of the 209 patients with a confirmed diagnosis of COVID-19 passed away. The main comorbidities related to mortality of these hospitalized patients with COVID-19 were obesity and kidney disease (P < 0.05). The main complications associated with fatal outcomes in this group of patients were Acute Respiratory Distress Syndrome (ARDS) and sepsis (P < 0.05). Furthermore, it was evidenced that the colchicine combination showed a significant difference in reducing mortality in hospitalized patients compared to the other therapeutic regimens (P < 0.05). Conclusion: A mortality rate of 51% was found attributable to several factors such as advanced age, obesity, kidney disease, and an average time in days of late consultation. The implementation of the colchicine combination could reduce the mortality rate in this disease.
Competing interests None declared.
Ethical approval This research was approved by the ethics and research committee of Oncomedica S.A.
References
Ayerbe, Risco, Ayis, The association between treatment with heparin and survival in patients with Covid-19, J Thromb Thrombolysis
Carlson, Nelveg-Kristensen, Ballegaard, Feldt-Rasmussen, Hornum et al., Increased vulnerability to Covid-19 in chronic kidney disease, J Intern Med
Chang, Chan, Underestimation of co-infections in COVID-19 due to non-discriminatory use of antibiotics, J Infect
Chen, Zhou, Dong, Qu, Gong et al., Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study, Lancet
Cui, Chen, Li, Liu, Wang, Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia, J Thromb Haemost
De Souza, Buss, Da S Candido, Carrera, Li et al., Epidemiological and clinical characteristics of the COVID-19 epidemic in Brazil, Nat Hum Behav
Deftereos, Giannopoulos, Vrachatis, Siasos, Giotaki et al., Effect of colchicine vs standard care on cardiac and inflammatory biomarkers and clinical outcomes in patients hospitalized with coronavirus disease 2019: the GRECCO-19 randomized clinical trial, JAMA Netw Open
Galvão, COVID-19: the deadly threat of misinformation, doi:10.1016/S1473-3099
Goyal, Choi, Pinheiro, Schenck, Chen et al., Clinical characteristics of covid-19 in New York City, N Engl J Med
Guan, Ni, Hu, Liang, Ou et al., Clinical characteristics of coronavirus disease 2019 in China, N Engl J Med
Han, Shi, Xie, Zhang, Huang et al., Analysis of factors affecting the prognosis of COVID-19 patients and viral shedding duration, Epidemiol Infect
Ins, Covid, -19 en Colombia
Jiménez, Vela, Valencia, Fernandez-Jimenez, Álvaro-Alonso et al., Characteristics, complications and outcomes among 1549 patients hospitalised with COVID-19 in a secondary hospital in Madrid, Spain: a retrospective case series study, BMJ Open
Klok, Kruip, Van Der Meer, Arbous, Gommers et al., Incidence of thrombotic complications in critically ill ICU patients with COVID-19, Thromb Res
Lansbury, Lim, Baskaran, Lim, Co-infections in people with COVID-19: a systematic review and meta-analysis, J Infect, doi:10.1093/cid/ciaa530
Middeldorp, Coppens, Van Haaps, Foppen, Vlaar et al., Incidence of venous thromboembolism in hospitalized patients with COVID-19, J Thromb Haemost
Mohamed, Benn, Astha, Okhawere, Korn et al., Association between chronic kidney disease and COVID-19-related mortality in New York, World J Urol, doi:10.1007/s00345-020-03567-4
Ortiz-Brizuela, Villanueva-Reza, González-Lara, Tamez-Torres, Montes et al., Clinical and epidemiological characteristics of patients diagnosed with covid-19 in a tertiary care center in Mexico City: a prospective cohort study, Rev Investig Clin organo del Hosp Enfermedades la Nutr
Ozturk, Turgutalp, Arici, Odabas, Altiparmak et al., Mortality analysis of COVID-19 infection in chronic kidney disease, haemodialysis and renal transplant patients compared with patients without kidney disease: a nationwide analysis from Turkey, Nephrol Dial Transplant
Panigada, Bottino, Tagliabue, Grasselli, Novembrino et al., Hypercoagulability of COVID-19 patients in intensive care unit: a report of thromboelastography findings and other parameters of hemostasis, J Thromb Haemost
Parra-Bracamonte, Parra-Bracamonte, Lopez-Villalobos, Al, Chronic kidney disease is a very significant comorbidity for high risk of death in patients with COVID-19 in Mexico, Nephrology, doi:10.1007/s00345-020-03567-4
Ranucci, Ballotta, Dedda, Bayshnikova, Poli et al., The procoagulant pattern of patients with COVID-19 acute respiratory distress syndrome, J Thromb Haemost
Rawson, Moore, Zhu, Ranganathan, Skolimowska et al., Bacterial and fungal coinfection in individuals with coronavirus: a rapid review to support COVID-19 antimicrobial prescribing, Clin Infect Dis, doi:10.1093/cid/ciaa530
Richardson, Hirsch, Narasimhan, Crawford, Mcginn et al., Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area, JAMA, doi:10.1001/jama.2020.6775
Rodriguez-Nava, Yanez-Bello, Garcia, Chung, Chaudry et al., Clinical characteristics and risk factors for mortality of hospitalized patients with COVID-19 in a community hospital: a retrospective cohort study, Mayo Clin Proc Innov Qual Outcomes
Roozenbeek, Schneider, Dryhurst, Kerr, Freeman et al., Susceptibility to misinformation about COVID-19 around the world, R Soc Open Sci, doi:10.1016/S1473-3099
Sattar, Mcinnes, Mcmurray, Obesity is a risk factor for severe COVID-19 infection: multiple potential mechanisms, Circulation
Sharma, Garg, Rout, Lavie, Association of obesity with more critical illness in COVID-19, Mayo Clinic Proc
Tamara, Tahapary, Obesity as a predictor for a poor prognosis of COVID-19: a systematic review, Diabetes Metab Syndr
Tang, Bai, Chen, Gong, Li et al., Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy, J Thromb Haemost
Trujillo, Consenso colombiano de atención, diagnóstico y manejo de la infección por SARS-COV-2/COVID-19 en establecimientos de atención de la salud Recomendaciones basadas en consenso de expertos e informadas en la evidencia
Tzotzos, Fischer, Fischer, Zeitlinger, Incidence of ARDS and outcomes in hospitalized patients with COVID-19: a global literature survey, Crit Care
Wang, Du, Zhu, Cao, An et al., Comorbidities and multi-organ injuries in the treatment of COVID-19, Lancet
Wang, Hu, Hu, Zhu, Liu et al., Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China, JAMA
Wu, Chen, Cai, Xia, Zhou et al., Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China, JAMA Intern Med, doi:10.1001/jamainternmed.2020.0994
Xiong, Liu, Lin, Shi, Han et al., Clinical characteristics of 116 hospitalized patients with COVID-19 in Wuhan, China: a single-centered, retrospective, observational study, BMC Infect Dis
Yang, Sheng, Huang, Jin, Xiong et al., Clinical characteristics, outcomes, and risk factors for mortality in patients with cancer and COVID-19 in Hubei, China: a multicentre, retrospective, cohort study, Lancet Oncol
Zangrillo, Beretta, Scandroglio, Monti, Fominskiy et al., Characteristics, treatment, outcomes and cause of death of invasively ventilated patients with COVID-19 ARDS in Milan, Italy, Crit care Resusc J Australas Acad Crit Care Med
Zhou, Yu, Du, Fan, Liu et al., Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet
DOI record:
{
"DOI": "10.1016/j.jiph.2021.02.013",
"ISSN": [
"1876-0341"
],
"URL": "http://dx.doi.org/10.1016/j.jiph.2021.02.013",
"alternative-id": [
"S1876034121000575"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Clinical outcomes of patients hospitalized for COVID-19 and evidence-based on the pharmacological management reduce mortality in a region of the Colombian Caribbean"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Journal of Infection and Public Health"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.jiph.2021.02.013"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2021 The Author(s). Published by Elsevier Ltd on behalf of King Saud Bin Abdulaziz University for Health Sciences."
}
],
"author": [
{
"affiliation": [],
"family": "García-Posada",
"given": "Mara",
"sequence": "first"
},
{
"affiliation": [],
"family": "Aruachan-Vesga",
"given": "Sandra",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mestra",
"given": "Danis",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Humánez",
"given": "Katherine",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Serrano-Coll",
"given": "Héctor",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6120-9436",
"affiliation": [],
"authenticated-orcid": false,
"family": "Cabrales",
"given": "Heriberto",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Faccini",
"given": "Álvaro",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mattar",
"given": "Salim",
"sequence": "additional"
}
],
"container-title": [
"Journal of Infection and Public Health"
],
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.jp",
"clinicalkey.com",
"clinicalkey.es",
"clinicalkey.fr",
"clinicalkey.com.au",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2021,
3,
7
]
],
"date-time": "2021-03-07T15:29:30Z",
"timestamp": 1615130970000
},
"deposited": {
"date-parts": [
[
2021,
5,
18
]
],
"date-time": "2021-05-18T22:43:18Z",
"timestamp": 1621377798000
},
"indexed": {
"date-parts": [
[
2022,
2,
3
]
],
"date-time": "2022-02-03T03:27:15Z",
"timestamp": 1643858835089
},
"is-referenced-by-count": 8,
"issn-type": [
{
"type": "print",
"value": "1876-0341"
}
],
"issue": "6",
"issued": {
"date-parts": [
[
2021,
6
]
]
},
"journal-issue": {
"issue": "6",
"published-print": {
"date-parts": [
[
2021,
6
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
6,
1
]
],
"date-time": "2021-06-01T00:00:00Z",
"timestamp": 1622505600000
}
},
{
"URL": "http://creativecommons.org/licenses/by-nc-nd/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
3,
3
]
],
"date-time": "2021-03-03T00:00:00Z",
"timestamp": 1614729600000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S1876034121000575?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S1876034121000575?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "696-701",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2021,
6
]
]
},
"published-print": {
"date-parts": [
[
2021,
6
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"first-page": "26",
"key": "10.1016/j.jiph.2021.02.013_bib0005",
"series-title": "A world at risk: annual report on global preparedness for health emergencies",
"year": "2019"
},
{
"key": "10.1016/j.jiph.2021.02.013_bib0010",
"unstructured": "https://www.worldometers.info/coronavirus/ [Internet]. Available from: https://www.worldometers.info/coronavirus/. [cited 12 August 2020]."
},
{
"author": "INS",
"key": "10.1016/j.jiph.2021.02.013_bib0015",
"series-title": "COVID-19 en Colombia",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2002032",
"article-title": "Clinical characteristics of coronavirus disease 2019 in China",
"author": "Guan",
"doi-asserted-by": "crossref",
"first-page": "1708",
"issue": "April (18)",
"journal-title": "N Engl J Med",
"key": "10.1016/j.jiph.2021.02.013_bib0020",
"volume": "382",
"year": "2020"
},
{
"article-title": "Dexamethasone in hospitalized patients with covid-19 — preliminary report",
"issue": "July",
"journal-title": "N Engl J Med",
"key": "10.1016/j.jiph.2021.02.013_bib0025",
"year": "2020"
},
{
"article-title": "Effect of colchicine vs standard care on cardiac and inflammatory biomarkers and clinical outcomes in patients hospitalized with coronavirus disease 2019: the GRECCO-19 randomized clinical trial",
"author": "Deftereos",
"issue": "June (6)",
"journal-title": "JAMA Netw Open",
"key": "10.1016/j.jiph.2021.02.013_bib0030",
"volume": "3",
"year": "2020"
},
{
"author": "Saavedra Trujillo",
"first-page": "36",
"key": "10.1016/j.jiph.2021.02.013_bib0035",
"series-title": "Consenso colombiano de atención, diagnóstico y manejo de la infección por SARS-COV-2/COVID-19 en establecimientos de atención de la salud Recomendaciones basadas en consenso de expertos e informadas en la evidencia. Vol. 24, Infectio. scieloco",
"year": "2020"
},
{
"key": "10.1016/j.jiph.2021.02.013_bib0040",
"unstructured": "Clinical management of COVID-19 [Internet]. Available from: https://www.who.int/publications/i/item/clinical-management-of-covid-19 [cited 6 Dec 2020]."
},
{
"DOI": "10.1001/jama.2020.1585",
"article-title": "Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "1061",
"issue": "March (11)",
"journal-title": "JAMA",
"key": "10.1016/j.jiph.2021.02.013_bib0045",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30211-7",
"article-title": "Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "507",
"issue": "February (10223)",
"journal-title": "Lancet (London, England)",
"key": "10.1016/j.jiph.2021.02.013_bib0050",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1056/NEJMc2010419",
"article-title": "Clinical characteristics of covid-19 in New York City",
"author": "Goyal",
"doi-asserted-by": "crossref",
"first-page": "2372",
"journal-title": "N Engl J Med",
"key": "10.1016/j.jiph.2021.02.013_bib0055",
"volume": "382",
"year": "2020"
},
{
"article-title": "Clinical and epidemiological characteristics of patients diagnosed with covid-19 in a tertiary care center in Mexico City: a prospective cohort study",
"author": "Ortiz-Brizuela",
"first-page": "165",
"issue": "3",
"journal-title": "Rev Investig Clin organo del Hosp Enfermedades la Nutr",
"key": "10.1016/j.jiph.2021.02.013_bib0060",
"volume": "72",
"year": "2020"
},
{
"DOI": "10.1038/s41562-020-0928-4",
"article-title": "Epidemiological and clinical characteristics of the COVID-19 epidemic in Brazil",
"author": "de Souza",
"doi-asserted-by": "crossref",
"first-page": "856",
"issue": "August (8)",
"journal-title": "Nat Hum Behav",
"key": "10.1016/j.jiph.2021.02.013_bib0065",
"volume": "4",
"year": "2020"
},
{
"article-title": "Characteristics, complications and outcomes among 1549 patients hospitalised with COVID-19 in a secondary hospital in Madrid, Spain: a retrospective case series study",
"author": "Jiménez",
"issue": "November (11)",
"journal-title": "BMJ Open",
"key": "10.1016/j.jiph.2021.02.013_bib0070",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1186/s12879-020-05452-2",
"article-title": "Clinical characteristics of 116 hospitalized patients with COVID-19 in Wuhan, China: a single-centered, retrospective, observational study",
"author": "Xiong",
"doi-asserted-by": "crossref",
"first-page": "787",
"issue": "October (1)",
"journal-title": "BMC Infect Dis",
"key": "10.1016/j.jiph.2021.02.013_bib0075",
"volume": "20",
"year": "2020"
},
{
"article-title": "Clinical characteristics and risk factors for mortality of hospitalized patients with COVID-19 in a community hospital: a retrospective cohort study",
"author": "Rodriguez-Nava",
"first-page": "1",
"journal-title": "Mayo Clin Proc Innov Qual Outcomes",
"key": "10.1016/j.jiph.2021.02.013_bib0080",
"volume": "5",
"year": "2020"
},
{
"article-title": "Analysis of factors affecting the prognosis of COVID-19 patients and viral shedding duration",
"author": "Han",
"issue": "June",
"journal-title": "Epidemiol Infect",
"key": "10.1016/j.jiph.2021.02.013_bib0085",
"volume": "148",
"year": "2020"
},
{
"key": "10.1016/j.jiph.2021.02.013_bib0090",
"unstructured": "COVID Misinformation Is Killing People – Scientific American [Internet]. Available from: https://www.scientificamerican.com/article/covid-misinformation-is-killing-people1/ [cited 30 November 2020]."
},
{
"key": "10.1016/j.jiph.2021.02.013_bib0095",
"unstructured": "Where Are All the Patients? Addressing Covid-19 Fear to Encourage Sick Patients to Seek Emergency Care | Catalyst non-issue content [Internet]. Available from: https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0193 [cited 30 November 2020]."
},
{
"author": "Galvão",
"key": "10.1016/j.jiph.2021.02.013_bib0100",
"series-title": "COVID-19: the deadly threat of misinformation. Vol. 0, the lancet infectious diseases",
"year": "2020"
},
{
"article-title": "Susceptibility to misinformation about COVID-19 around the world",
"author": "Roozenbeek",
"issue": "October (10)",
"journal-title": "R Soc Open Sci",
"key": "10.1016/j.jiph.2021.02.013_bib0105",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.6775",
"article-title": "Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area",
"author": "Richardson",
"doi-asserted-by": "crossref",
"first-page": "2052",
"issue": "May (20)",
"journal-title": "JAMA",
"key": "10.1016/j.jiph.2021.02.013_bib0110",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30558-4",
"article-title": "Comorbidities and multi-organ injuries in the treatment of COVID-19",
"author": "Wang",
"doi-asserted-by": "crossref",
"journal-title": "Lancet (London, England)",
"key": "10.1016/j.jiph.2021.02.013_bib0115",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1016/S1470-2045(20)30310-7",
"article-title": "Clinical characteristics, outcomes, and risk factors for mortality in patients with cancer and COVID-19 in Hubei, China: a multicentre, retrospective, cohort study",
"author": "Yang",
"doi-asserted-by": "crossref",
"first-page": "904",
"issue": "July (7)",
"journal-title": "Lancet Oncol",
"key": "10.1016/j.jiph.2021.02.013_bib0120",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.1016/j.dsx.2020.05.020",
"article-title": "Obesity as a predictor for a poor prognosis of COVID-19: a systematic review",
"author": "Tamara",
"doi-asserted-by": "crossref",
"first-page": "655",
"issue": "4",
"journal-title": "Diabetes Metab Syndr",
"key": "10.1016/j.jiph.2021.02.013_bib0125",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1016/j.mayocp.2020.06.046",
"article-title": "Association of obesity with more critical illness in COVID-19",
"author": "Sharma",
"doi-asserted-by": "crossref",
"first-page": "2040",
"journal-title": "Mayo Clinic Proc",
"key": "10.1016/j.jiph.2021.02.013_bib0130",
"volume": "95",
"year": "2020"
},
{
"DOI": "10.1161/CIRCULATIONAHA.120.047659",
"article-title": "Obesity is a risk factor for severe COVID-19 infection: multiple potential mechanisms",
"author": "Sattar",
"doi-asserted-by": "crossref",
"first-page": "4",
"issue": "July (1)",
"journal-title": "Circulation",
"key": "10.1016/j.jiph.2021.02.013_bib0135",
"volume": "142",
"year": "2020"
},
{
"article-title": "Increased vulnerability to Covid‐19 in chronic kidney disease",
"author": "Carlson",
"issue": "January",
"journal-title": "J Intern Med",
"key": "10.1016/j.jiph.2021.02.013_bib0140",
"year": "2021"
},
{
"DOI": "10.1093/ndt/gfaa271",
"article-title": "Mortality analysis of COVID-19 infection in chronic kidney disease, haemodialysis and renal transplant patients compared with patients without kidney disease: a nationwide analysis from Turkey",
"author": "Ozturk",
"doi-asserted-by": "crossref",
"first-page": "2083",
"issue": "December (12)",
"journal-title": "Nephrol Dial Transplant",
"key": "10.1016/j.jiph.2021.02.013_bib0145",
"volume": "35",
"year": "2020"
},
{
"article-title": "Association between chronic kidney disease and COVID-19-related mortality in New York",
"author": "Mohamed",
"issue": "January",
"journal-title": "World J Urol",
"key": "10.1016/j.jiph.2021.02.013_bib0150",
"year": "2021"
},
{
"article-title": "Chronic kidney disease is a very significant comorbidity for high risk of death in patients with COVID-19 in Mexico",
"author": "Parra-Bracamonte",
"journal-title": "Nephrology",
"key": "10.1016/j.jiph.2021.02.013_bib0155",
"year": "2020"
},
{
"DOI": "10.1001/jamainternmed.2020.0994",
"article-title": "Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China",
"author": "Wu",
"doi-asserted-by": "crossref",
"first-page": "934",
"issue": "July (7)",
"journal-title": "JAMA Intern Med",
"key": "10.1016/j.jiph.2021.02.013_bib0160",
"volume": "180",
"year": "2020"
},
{
"article-title": "Characteristics, treatment, outcomes and cause of death of invasively ventilated patients with COVID-19 ARDS in Milan, Italy",
"author": "Zangrillo",
"first-page": "200",
"issue": "September (3)",
"journal-title": "Crit care Resusc J Australas Acad Crit Care Med",
"key": "10.1016/j.jiph.2021.02.013_bib0165",
"volume": "22",
"year": "2020"
},
{
"DOI": "10.1186/s13054-020-03240-7",
"article-title": "Incidence of ARDS and outcomes in hospitalized patients with COVID-19: a global literature survey",
"author": "Tzotzos",
"doi-asserted-by": "crossref",
"first-page": "516",
"issue": "August (1)",
"journal-title": "Crit Care",
"key": "10.1016/j.jiph.2021.02.013_bib0170",
"volume": "24",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"article-title": "Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study",
"author": "Zhou",
"doi-asserted-by": "crossref",
"first-page": "1054",
"issue": "March (10229)",
"journal-title": "Lancet",
"key": "10.1016/j.jiph.2021.02.013_bib0175",
"volume": "395",
"year": "2020"
},
{
"article-title": "Bacterial and fungal coinfection in individuals with coronavirus: a rapid review to support COVID-19 antimicrobial prescribing",
"author": "Rawson",
"issue": "May",
"journal-title": "Clin Infect Dis",
"key": "10.1016/j.jiph.2021.02.013_bib0180",
"year": "2020"
},
{
"DOI": "10.1016/j.jinf.2020.05.046",
"article-title": "Co-infections in people with COVID-19: a systematic review and meta-analysis",
"author": "Lansbury",
"doi-asserted-by": "crossref",
"first-page": "266",
"issue": "2",
"journal-title": "J Infect",
"key": "10.1016/j.jiph.2021.02.013_bib0185",
"volume": "81",
"year": "2020"
},
{
"DOI": "10.1016/j.jinf.2020.06.077",
"article-title": "Underestimation of co-infections in COVID-19 due to non-discriminatory use of antibiotics",
"author": "Chang",
"doi-asserted-by": "crossref",
"first-page": "e29",
"issue": "September (3)",
"journal-title": "J Infect",
"key": "10.1016/j.jiph.2021.02.013_bib0190",
"volume": "81",
"year": "2020"
},
{
"DOI": "10.1111/jth.14854",
"article-title": "The procoagulant pattern of patients with COVID-19 acute respiratory distress syndrome",
"author": "Ranucci",
"doi-asserted-by": "crossref",
"first-page": "1747",
"issue": "July (7)",
"journal-title": "J Thromb Haemost",
"key": "10.1016/j.jiph.2021.02.013_bib0195",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.1111/jth.14850",
"article-title": "Hypercoagulability of COVID-19 patients in intensive care unit: a report of thromboelastography findings and other parameters of hemostasis",
"author": "Panigada",
"doi-asserted-by": "crossref",
"first-page": "1738",
"issue": "July (7)",
"journal-title": "J Thromb Haemost",
"key": "10.1016/j.jiph.2021.02.013_bib0200",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.1111/jth.14888",
"article-title": "Incidence of venous thromboembolism in hospitalized patients with COVID-19",
"author": "Middeldorp",
"doi-asserted-by": "crossref",
"first-page": "1995",
"issue": "August (8)",
"journal-title": "J Thromb Haemost",
"key": "10.1016/j.jiph.2021.02.013_bib0205",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.1016/j.thromres.2020.04.013",
"article-title": "Incidence of thrombotic complications in critically ill ICU patients with COVID-19",
"author": "Klok",
"doi-asserted-by": "crossref",
"first-page": "145",
"issue": "July",
"journal-title": "Thromb Res",
"key": "10.1016/j.jiph.2021.02.013_bib0210",
"volume": "191",
"year": "2020"
},
{
"DOI": "10.1111/jth.14830",
"article-title": "Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia",
"author": "Cui",
"doi-asserted-by": "crossref",
"first-page": "1421",
"issue": "June (6)",
"journal-title": "J Thromb Haemost",
"key": "10.1016/j.jiph.2021.02.013_bib0215",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.1007/s11239-020-02162-z",
"article-title": "The association between treatment with heparin and survival in patients with Covid-19",
"author": "Ayerbe",
"doi-asserted-by": "crossref",
"first-page": "298",
"issue": "August (2)",
"journal-title": "J Thromb Thrombolysis",
"key": "10.1016/j.jiph.2021.02.013_bib0220",
"volume": "50",
"year": "2020"
},
{
"DOI": "10.1111/jth.14817",
"article-title": "Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy",
"author": "Tang",
"doi-asserted-by": "crossref",
"first-page": "1094",
"issue": "May (5)",
"journal-title": "J Thromb Haemost",
"key": "10.1016/j.jiph.2021.02.013_bib0225",
"volume": "18",
"year": "2020"
}
],
"reference-count": 45,
"references-count": 45,
"relation": {},
"score": 1,
"short-container-title": [
"Journal of Infection and Public Health"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Infectious Diseases",
"Public Health, Environmental and Occupational Health",
"General Medicine"
],
"subtitle": [],
"title": [
"Clinical outcomes of patients hospitalized for COVID-19 and evidence-based on the pharmacological management reduce mortality in a region of the Colombian Caribbean"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "14"
}
