Factores asociados a la muerte por COVID-19 en pacientes admitidos en un hospital público en Tacna, Perú
et al., Revista Peruana de Medicina Experimental y Salud Pública, doi:10.17843/rpmesp.2021.382.7158, Jun 2021
Colchicine for COVID-19
5th treatment shown to reduce risk in
September 2020, now with p = 0.0000049 from 54 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
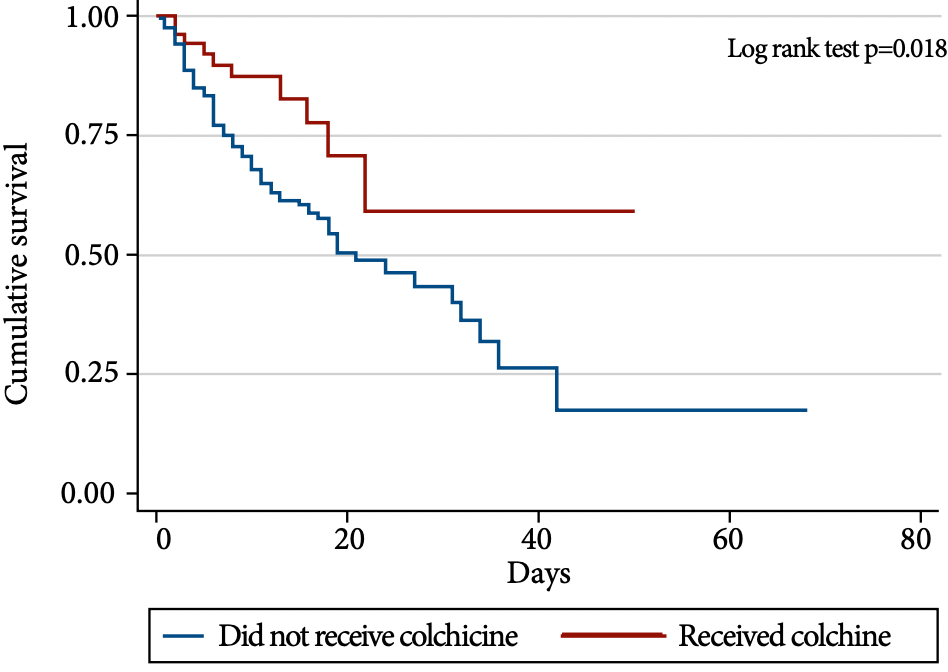
Retrospective 450 late stage (median oxygen saturation 86%) COVID+ hospitalized patients in Peru, showing lower mortality with colchicine treatment.
|
risk of death, 54.0% lower, HR 0.46, p = 0.03, treatment 10 of 50 (20.0%), control 109 of 301 (36.2%), NNT 6.2, adjusted per study, multivariable.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Hueda-Zavaleta et al., 10 Jun 2021, retrospective, Peru, peer-reviewed, 6 authors, dosage not specified.
Factores asociados a la muerte por COVID-19 en pacientes admitidos en un hospital público en Tacna, Perú
Revista Peruana de Medicina Experimental y Salud Pública, doi:10.17843/rpmesp.2021.382.7158
Objective: To describe the clinical, laboratory and treatment characteristics of COVID-19 patients and to determine the factors associated with mortality during hospital stay. Materials and Methods: Retrospective cohort study of adult COVID-19 inpatients. The clinical, laboratory and treatment data were obtained from the medical records of patients from the Hospital Nivel III Daniel Alcides Carrión in Tacna. For the survival analysis we used the Cox proportional hazards model, and we calculated crude and adjusted hazard ratios (HR) with 95% confidence intervals (95% CI). Results: We evaluated 351 patients; 74.1% of them were men. The most common comorbidities were obesity (31.6%), hypertension (27.1%) and diabetes mellitus (24.5%). The median time of hospitalization was 8 days (IQR: 4-15). From the total of patients, 32.9% died during follow-up. The multivariate analysis showed an increased risk of dying associated with the following: age ≥65 years, HR = 3.55 (95% CI: 1.70-7.40); increase in lactate dehydrogenase >720 U/L, HR = 2.08 (95% CI: 1.34-3.22); and oxygen saturation less than 90%, mainly when it was less than 80%, HR = 4.07 (95% CI: 2.10-7.88). In addition, the use of colchicine during treatment showed a protective effect, HR = 0.46 (95% CI: 0.23-0.91). Conclusions: Risk factors for mortality due to COVID-19 included being older than 65 years, having oxygen saturation less than 90%, and elevated lactate dehydrogenase >720 U/L; colchicine treatment could improve the prognosis of patients.
Author contributions: MHZ and CCC conceived the research idea, wrote the article, and carried out the data analysis and interpretation. FBS, RFP and LBR participated in data collection and wrote the article. VABZ participated in data analysis and interpretation, statistical and technical advice, and critical revision of the article. All authors approved the final version of the manuscript.
Conflict of interest: The authors deny any conflict of interest.
References
Abdullahi, Emeribe, Mustapha, Fasogbon, Ofor et al., Exploring the genetics, ecology of SARS-COV-2 and climatic factors as possible control strategies against COVID-19, Ahead Of Print1
Benites-Goñi, Vargas-Carrillo, Peña-Monge, Taype-Rondan, Arróspinde-Mormontoy et al., Características clínicas, manejo y mortalidad de pacientes hospitalizados con CO-VID-19 en un hospital de referencia en Lima, Perú
Davidson, Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area, JAMA, doi:10.1001/jama.2020.6775
Deftereos, Siasos, Giannopoulos, Vrachatis, Angelidis et al., The Greek study in the effects of colchicine in COVID-19 complications prevention (GRECCO-19 study): Rationale and study design, Hellenic J Cardiol, doi:10.1016/j.hjc.2020.03.002
Diaz, Riviello, Papali, Adhikari, Ferreira, Global Critical Care: Moving Forward in Resource-Limited Settings, Ann Glob Health, doi:10.5334/aogh.2413
Díaz-Vélez, Urrunaga-Pastor, Romero-Cerdán, Peña-Sánchez, Fernández et al., Risk factors for mortality in hospitalized patients with COVID-19 from three hospitals in Peru: a retrospective cohort study [version 1; peer review: awaiting peer review, F1000Research, doi:10.12688/f1000research.51474.1
Gianella, Iguiñiz-Romero, Romero, Good Health Indicators are Not Enough: Lessons from COVID-19 in Peru, Health Hum Rights
Giraldo, COVID-19 in Peru, Indian J Psychiatry, doi:10.4103/psychiatry.IndianJPsychiatry_1045_20
Horby, Pessoa-Amorim, Peto, Brightling, Sarkar et al., Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): preliminary results of a randomised, controlled, open-label, platform trial
Investigators, Gordon, Mouncey, Al-Beidh, Rowan et al., Interleukin-6 Receptor Antagonists in Critically Ill Patients with Covid-19, N Engl J Med, doi:10.1056/NEJMoa2100433
Mcginn, None
Medrxiv, None, doi:10.1101/2021.02.11.21249258
Mejía, Medina, Cornejo, Morello, Vásquez et al., Oxygen saturation as a predictor of mortality in hospitalized adult patients with COVID-19 in a public hospital in Lima, Peru, PLoS One, doi:10.1371/journal.pone.0244171
Richardson, Hirsch, Narasimhan, Crawford, None
Rodríguez-Zúñiga, Quintana-Aquehua, Díaz-Lajo, Charaja-Coata, Becerra-Bonilla et al., Factores de riesgo asociados a mortalidad en pacientes adultos con neumonía por SARS-CoV-2 en un hospital público de Lima, Perú, Acta Med Peru, doi:10.35663/amp.2020.374.1676
Salama, Mohan, Tocilizumab in Patients Hospitalized with Covid-19 Pneumonia. Reply, N Engl J Med, doi:10.1056/NEJMc2100217
Salomaa, Bouffler, Atkinson, Cardis, Hamada, Is there any supportive evidence for low dose radiotherapy for COVID-19 pneumonia?, Int J Radiat Biol, doi:10.1080/09553002.2020.1786609
Sandhu, Tieng, Chilimuri, Franchin, A Case Control Study to Evaluate the Impact of Colchicine on Patients Admitted to the Hospital with Moderate to Severe COVID-19 Infection, Can J Infect Dis Med Microbiol, doi:10.1155/2020/8865954
Schlesinger, Firestein, Brunetti, Colchicine in COVID-19: an Old Drug, New Use, Curr Pharmacol Rep, doi:10.1007/s40495-020-00225-6
Sousa, Garces, Cestari, Florêncio, Moreira et al., Mortality and survival of COVID-19, Epidemiol Infect, doi:10.1017/S0950268820001405
Stone, Frigault, Serling-Boyd, Fernandes, Harvey et al., Tocilizumab Trial Investigators. Efficacy of Tocilizumab in Patients Hospitalized with Covid-19, N Engl J Med, doi:10.1056/NEJMoa2028836
Suleyman, Fadel, Malette, Hammond, Abdulla et al., Clinical Characteristics and Morbidity Associated With Coronavirus Disease 2019 in a Series of Patients in Metropolitan Detroit, JAMA Netw Open, doi:10.1001/jama-networkopen.2020.12270
Vena, Giacobbe, Biagio, Mikulska, Taramasso et al., GECOVID study group. Clinical characteristics, management and in-hospital mortality of patients with coronavirus disease 2019 in Genoa, Italy, Clin Microbiol Infect, doi:10.1016/j.cmi.2020.07.049
Vrachatis, Giannopoulos, Giotaki, Raisakis, Kossyvakis et al., Impact of colchicine on mortality in patients with COVID-19. A meta-analysis, Hellenic J Cardiol, doi:10.1016/j.hjc.2020.11.012
DOI record:
{
"DOI": "10.17843/rpmesp.2021.382.7158",
"ISSN": [
"1726-4642",
"1726-4634"
],
"URL": "http://dx.doi.org/10.17843/rpmesp.2021.382.7158",
"abstract": "<jats:p>Objetivo: Describir las características demográficas, clínicas, laboratoriales y de tratamiento de pacientes hospitalizados por la COVID-19 y determinar los factores de riesgo de mortalidad hospitalaria. Materiales y métodos: Estudio de cohorte retrospectivo de pacientes adultos hospitalizados por la COVID-19. Se extrajeron datos demográficos, clínicos, laboratoriales y de tratamiento de las historias clínicas de pacientes que ingresaron al Hospital III Daniel Alcides Carrión de Tacna. Para el análisis de supervivencia se empleó el modelo de riesgos proporcionales de Cox y se calcularon los cocientes de riesgo instantáneos (HR) crudos y ajustados con sus respectivos intervalos de confianza al 95% (IC 95%). Resultados: Se evaluó a 351 pacientes, el 74,1% eran hombres; las comorbilidades más comunes fueron obesidad (31,6%), hipertensión (27,1%) y diabetes mellitus (24,5%). La mediana de tiempo de hospitalización fue 8 días (RIC: 4-15). El 32,9% falleció durante el seguimiento. El análisis multivariado mostró un aumento del riesgo de morir asociado a la edad ≥65 años, HR = 3,55 (IC 95%: 1,70-7,40); al incremento de lactato deshidrogenasa 720 U/L, HR = 2,08 (IC 95%: 1,34-3,22); y a la saturación de oxígeno por debajo del 90%, principalmente cuando fue menor al 80%, HR = 4,07 (IC 95%: 2,10-7,88). Además, el uso de colchicina en el tratamiento tuvo un efecto protector, HR = 0,46 (IC 95%: 0,23-0,91). Conclusiones: Los factores de riesgo de muerte por la COVID-19 incluyeron ser mayor de 65 años, tener saturación de oxígeno menor de 90% y elevación del lactato deshidrogenasa 720 U/L; el tratamiento con colchicina podría mejorar el pronóstico de los pacientes.</jats:p>",
"author": [
{
"ORCID": "http://orcid.org/0000-0002-8049-7787",
"affiliation": [],
"authenticated-orcid": false,
"family": "Hueda-Zavaleta",
"given": "Miguel",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-3497-0158",
"affiliation": [],
"authenticated-orcid": false,
"family": "Copaja-Corzo",
"given": "Cesar",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9020-4426",
"affiliation": [],
"authenticated-orcid": false,
"family": "Bardales-Silva",
"given": "Fabrizzio",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-5374-7915",
"affiliation": [],
"authenticated-orcid": false,
"family": "Flores-Palacios",
"given": "Rodrigo",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2851-0219",
"affiliation": [],
"authenticated-orcid": false,
"family": "Barreto-Rocchetti",
"given": "Luis",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9158-1108",
"affiliation": [],
"authenticated-orcid": false,
"family": "Benites-Zapata",
"given": "Vicente A.",
"sequence": "additional"
}
],
"container-title": [
"Revista Peruana de Medicina Experimental y Salud Pública"
],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
8,
3
]
],
"date-time": "2021-08-03T17:06:35Z",
"timestamp": 1628010395000
},
"deposited": {
"date-parts": [
[
2021,
8,
3
]
],
"date-time": "2021-08-03T17:07:07Z",
"timestamp": 1628010427000
},
"indexed": {
"date-parts": [
[
2021,
12,
11
]
],
"date-time": "2021-12-11T07:41:09Z",
"timestamp": 1639208469936
},
"is-referenced-by-count": 1,
"issn-type": [
{
"type": "electronic",
"value": "1726-4642"
},
{
"type": "print",
"value": "1726-4634"
}
],
"issue": "2",
"issued": {
"date-parts": [
[
2021,
6,
10
]
]
},
"journal-issue": {
"issue": "2",
"published-online": {
"date-parts": [
[
2021,
3,
26
]
]
}
},
"link": [
{
"URL": "https://rpmesp.ins.gob.pe/rpmesp/article/viewFile/7158/4248",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://rpmesp.ins.gob.pe/rpmesp/article/viewFile/7158/4248",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "7920",
"original-title": [],
"page": "214-23",
"prefix": "10.17843",
"published": {
"date-parts": [
[
2021,
6,
10
]
]
},
"published-online": {
"date-parts": [
[
2021,
6,
10
]
]
},
"publisher": "Instituto Nacional de Salud (Peru)",
"reference-count": 0,
"references-count": 0,
"relation": {},
"score": 1,
"short-container-title": [
"Rev Peru Med Exp Salud Publica"
],
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine",
"Public Health, Environmental and Occupational Health"
],
"subtitle": [],
"title": [
"Factores asociados a la muerte por COVID-19 en pacientes admitidos en un hospital público en Tacna, Perú"
],
"type": "journal-article",
"volume": "38"
}
