Randomized controlled trial of favipiravir, hydroxychloroquine, and standard care in patients with mild/moderate COVID-19 disease
et al., Scientific Reports, doi:10.1038/s41598-022-08794-w, NCT04387760, Mar 2022
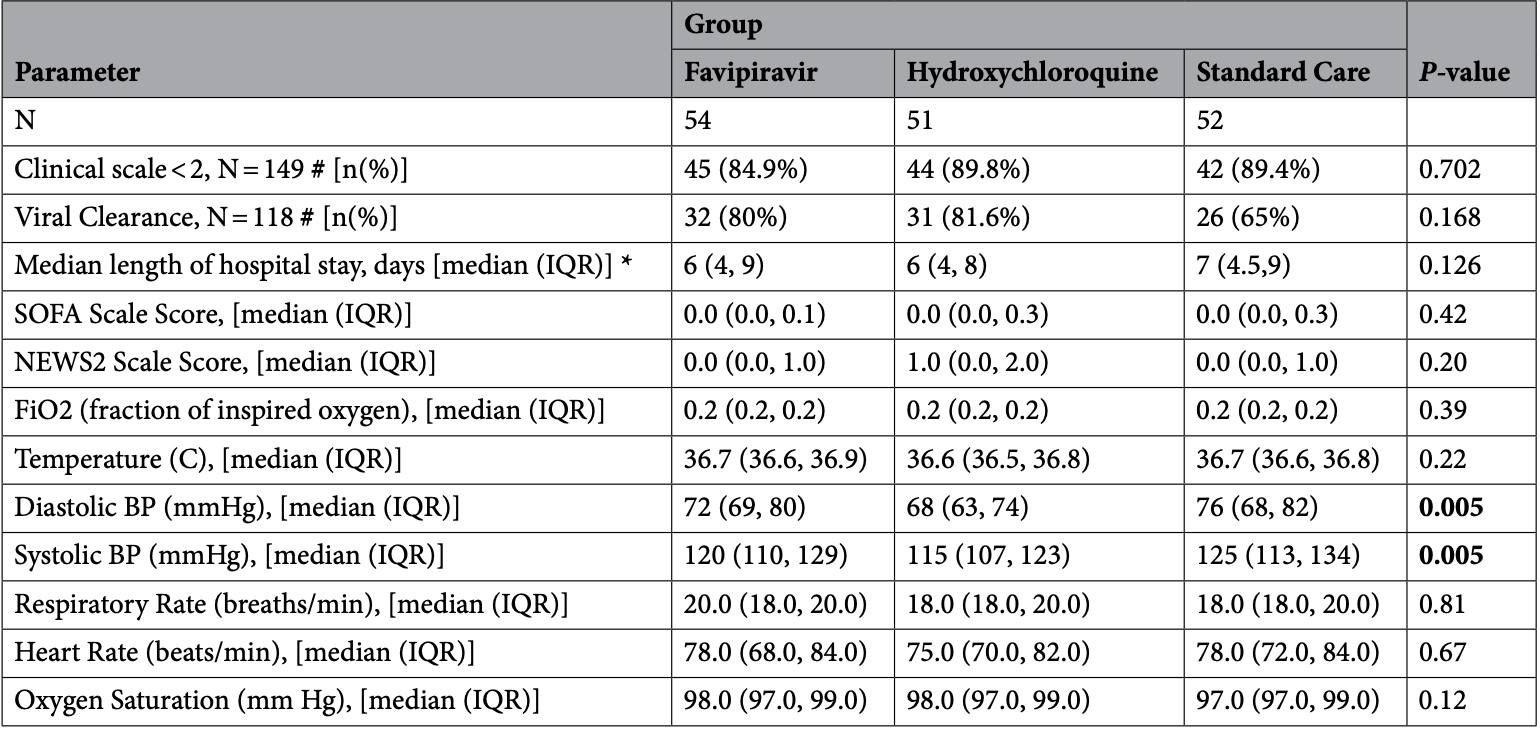
RCT with 54 favipiravir, 51 HCQ, and 52 SOC hospitalized patients in Bahrain, showing no significant differences. Viral clearance improved with both treatments, but did not reach statistical significance with the small sample size.
Potential risks of favipiravir include kidney injury1-3, liver injury2-5, cardiovascular events5,6, pulmonary toxicity6,7, and mutagenicity, carcinogenicity, teratogenicity, embryotoxicity, and the creation of dangerous variants8-14.
Study covers HCQ and favipiravir.
|
risk of death, 196.3% higher, RR 2.96, p = 1.00, treatment 1 of 54 (1.9%), control 0 of 52 (0.0%), continuity correction due to zero event (with reciprocal of the contrasting arm), day 30.
|
|
risk of ICU admission, 75.9% lower, RR 0.24, p = 0.20, treatment 1 of 54 (1.9%), control 4 of 52 (7.7%), NNT 17.
|
|
risk of no recovery, 41.9% higher, RR 1.42, p = 0.51, treatment 8 of 53 (15.1%), control 5 of 47 (10.6%).
|
|
risk of no viral clearance, 42.9% lower, RR 0.57, p = 0.21, treatment 8 of 40 (20.0%), control 14 of 40 (35.0%), NNT 6.7.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Abdulaziz et al., Clinical Features and Prognosis of Acute Kidney Injury in Hospital-Admitted Patients with COVID-19 in Egypt: A Single-Center Experience, Mansoura Medical Journal, doi:10.58775/2735-3990.1433.
2.
Ülger et al., Experimental evaluation of favipiravir (T-705)-induced liver and kidney toxicity in rats, Food and Chemical Toxicology, doi:10.1016/j.fct.2025.115472.
3.
El-Fetouh et al., Experimental Studies on Some Drugs Used in Covid-19 Treatment (Favipiravir and Dexamethasone) in Albino Rats, Journal of Advanced Veterinary Research, 13:10, www.advetresearch.com/index.php/AVR/article/view/1635.
4.
Almutairi et al., Liver Injury in Favipiravir-Treated COVID-19 Patients: Retrospective Single-Center Cohort Study, Tropical Medicine and Infectious Disease, doi:10.3390/tropicalmed8020129.
5.
Siby et al., Temporal Trends in Serious Adverse Events Associated with Oral Antivirals During the COVID-19 Pandemic: Insights from the FAERS Database (2020–2023), Open Forum Infectious Diseases, doi:10.1093/ofid/ofaf695.1825.
6.
Ozhan et al., Evaluation of the cardiopulmonary effects of repurposed COVID-19 therapeutics in healthy rats, Scientific Reports, doi:10.1038/s41598-025-31048-4.
7.
Ülger (B) et al., Evaluation of the effects of favipiravir (T-705) on the lung tissue of healty rats: An experimental study, Food and Chemical Toxicology, doi:10.1016/j.fct.2025.115235.
8.
Zhirnov et al., Favipiravir: the hidden threat of mutagenic action, Journal of microbiology, epidemiology and immunobiology, doi:10.36233/0372-9311-114.
9.
Waters et al., Human genetic risk of treatment with antiviral nucleoside analog drugs that induce lethal mutagenesis: the special case of molnupiravir, Environmental and Molecular Mutagenesis, doi:10.1002/em.22471.
10.
Hadj Hassine et al., Lethal Mutagenesis of RNA Viruses and Approved Drugs with Antiviral Mutagenic Activity, Viruses, doi:10.3390/v14040841.
11.
Shum, C., An investigational study into the drug-associated mutational signature in SARS-CoV-2 viruses, The University of Hong Kong, PhD Thesis, hub.hku.hk/handle/10722/344396.
12.
Shiraki et al., Convenient screening of the reproductive toxicity of favipiravir and antiviral drugs in Caenorhabditis elegans, Heliyon, doi:10.1016/j.heliyon.2024.e35331.
AlQahtani et al., 23 Mar 2022, Randomized Controlled Trial, Bahrain, peer-reviewed, 14 authors, study period August 2020 - March 2021, trial NCT04387760 (history).
Randomized controlled trial of favipiravir, hydroxychloroquine, and standard care in patients with mild/moderate COVID-19 disease
Scientific Reports, doi:10.1038/s41598-022-08794-w
Favipiravir has antiviral activity against influenza, West Nile virus, and yellow fever virus and against flaviviruses. The objective of this pilot study was to compare three arms: favipiravir; hydroxychloroquine; standard care (no specific SARS-CoV-2 treatment) only, in symptomatic patients infected by SARS-CoV-2 in an open-labelled randomized clinical trial. The trial was registered with Bahrain National Taskforce for Combatting COVID-19 on the 7th of May 2020 (registration code: NCT04387760). 150 symptomatic patients with COVID-19 disease were randomized into one of three arms: favipiravir, hydroxychloroquine, or standard care only. The primary outcome was the clinical scale at the end of study follow up (day 14 or on discharge/death) based on a points scale. The secondary outcomes were viral clearance, biochemical parameter changes and mortality at 30-days. Baseline characteristics did not differ between groups. The proportion of patients who achieved a clinical scale < 2 did not differ between groups. The favipiravir-treated and hydroxychloroquine-treated group showed increased viral clearance (OR, 95%CI 2.38, 0.83-6.78, OR, 95%CI 2.15, 0.78-5.92, respectively) compared to standard care, but this was not significant. The biochemical profile did not differ between groups, except for the platelet count (P < 0.03) and uric acid (P < 0.004) that were higher with favipiravir-treatment. Primary or secondary outcome measures did not differ between favipiravir, hydroxychloroquine, and standard therapy for mild to moderate COVID-19 disease; therefore, whilst favipiravir therapy appeared safe with a trend to increased viral clearance, there was no superior therapeutic utility. Clinical trials registration. NCT04387760. Registration date: 07/05/2020.
Coronavirus disease 2019 (COVID-19 ) is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and has developed into a pandemic with serious global public health and economic sequelae. As of May 30th, 2021, more than 170,695,962 million cases have been confirmed worldwide, leading to over 3,550,234 deaths 1 . Several vaccines have been shown to prevent or ameliorate COVID-19 disease, and several are currently developing 2 . However, for those that establish COVID-19 disease, there is a need for effective therapeutic agents to prevent the progressive deterioration that may be seen. There have been several reports of medications, such as remdesivir, with antiviral properties that have shown efficacy with shorter time-to-recovery against SARS-CoV-2 3 . It has been suggested that corticosteroids should be used cautiously unless there is evidence of refractory septic shock, acute respiratory distress syndrome (ARDS), or another compelling indication for their Use 4 . Hydroxychloroquine was thought to show great promise at the time that this study was initiated 5 but, in a large observational study, showed no differences in rates of intubation or death 6 , and a randomized trial..
Author contributions N.K.: data analysis, interpretation and preparation of the manuscript; D.A., A.A., F.A., M.A.F., F.A., F.A., S.S., A.A., Z.A., S.O. & S.A.: conception and design, data collection, manuscript review; S.S., N.K. & S.L.A.: writing and manuscript review; M.A.Q.: conception and design of the study and manuscript review.
Competing interests The authors declare no competing interests.
Additional information
Supplementary Information The online version contains supplementary material available at https:// doi. org/ 10. 1038/ s41598-022-08794-w. Correspondence and requests for materials should be addressed to M.A. Reprints and permissions information is available at www.nature.com/reprints. Publisher's note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Alqahtani, Randomized controlled trial of convalescent plasma therapy against standard therapy in patients with severe COVID-19 disease, Sci. Rep, doi:10.1038/s41598-021-89444-5
Beigel, Remdesivir for the treatment of Covid-19-preliminary report, N. Engl. J. Med, doi:10.1056/NEJMoa2007764
Birkett, Day, Internal pilot studies for estimating sample size, Stat. Med
Cai, Experimental treatment with favipiravir for COVID-19: An open-label control study, Engineering, doi:10.1016/j.eng.2020.03.007
Corman, Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR, Euro Surveill, doi:10.2807/1560-7917.Es.2020.25.3.2000045
Delang, Abdelnabi, Neyts, Favipiravir as a potential countermeasure against neglected and emerging RNA viruses, Antiviral Res, doi:10.1016/j.antiviral.2018.03.003
Diastolic, None, median (IQR)
Dong, Hu, Gao, Discovering drugs to treat coronavirus disease 2019 (COVID-19), Drug Discover. Therap, doi:10.5582/ddt.2020.01012
Echeverría-Esnal, Azithromycin in the treatment of COVID-19: A review, Expert Rev. Anti Infect. Ther, doi:10.1080/14787210.2020.1813024
Gautret, Clinical and microbiological effect of a combination of hydroxychloroquine and azithromycin in 80 COVID-19 patients with at least a six-day follow up: A pilot observational study, Travel Med. Infect. Dis, doi:10.1016/j.tmaid.2020.101663
Gautret, Hydroxychloroquine and azithromycin as a treatment of COVID-19: Results of an open-label non-randomized clinical trial, Int. J. Antimicrob. Agents, doi:10.1016/j.ijantimicag.2020.105949
Gavriatopoulou, Emerging treatment strategies for COVID-19 infection, Clin. Exp. Med, doi:10.1007/s10238-020-00671-y
Geleris, Observational study of hydroxychloroquine in hospitalized patients with Covid-19, N. Engl. J. Med
Geleris, Observational study of hydroxychloroquine in hospitalized patients with Covid-19, N. Engl. J. Med, doi:10.1056/NEJMoa2012410
Ghazy, A systematic review and meta-analysis on chloroquine and hydroxychloroquine as monotherapy or combined with azithromycin in COVID-19 treatment, Sci. Rep
Hassanipour, The efficacy and safety of Favipiravir in treatment of COVID-19: A systematic review and meta-analysis of clinical trials, Sci. Rep
Mehrotra, Clinical endpoints for evaluating efficacy in COVID-19 vaccine trials, Ann. Intern. Med, doi:10.7326/m20-6169
Mehta, Mazer-Amirshahi, Alkindi, Pourmand, Pharmacotherapy in COVID-19; A narrative review for emergency providers, Am. J. Emerg. Med, doi:10.1016/j.ajem.2020.04.035
Mishima, Anzai, Miyazaki, Abe, Uric acid elevation by favipiravir, an antiviral drug, Tohoku J. Exp. Med, doi:10.1620/tjem.251.87
Mitjà, A cluster-randomized trial of hydroxychloroquine for prevention of Covid-19, N. Engl. J. Med, doi:10.1056/NEJMoa2021801
Murohashi, Outcome of early-stage combination treatment with favipiravir and methylprednisolone for severe COVID-19 pneumonia: A report of 11 cases, Respir. Investig, doi:10.1016/j.resinv.2020.08.001
Néant, Modeling SARS-CoV-2 viral kinetics and association with mortality in hospitalized patients from the French COVID cohort, Proc. Natl. Acad. Sci, doi:10.1073/pnas.2017962118
Rao, Manissero, Steele, Pareja, A systematic review of the clinical utility of cycle threshold values in the context of COVID-19, Infect. Dis. Ther, doi:10.1007/s40121-020-00324-3
Shah, Safety and efficacy of ozone therapy in mild to moderate COVID-19 patients: A phase 1/11 randomized control trial (SEOT study), Int. Immunopharmacol, doi:10.1016/j.intimp.2020.107301
Sreekanth, Lai, Tackling COVID-19 using remdesivir and favipiravir as therapeutic options, Chembiochem Eur. J. Chem. Biol, doi:10.1002/cbic.202000595
Systolic, None, median (IQR
Tang, Hydroxychloroquine in patients with mainly mild to moderate coronavirus disease 2019: Open label, randomised controlled trial, BMJ, doi:10.1136/bmj.m1849
Udwadia, Efficacy and safety of favipiravir, an oral RNA-dependent RNA polymerase inhibitor, in mild-to-moderate COVID-19: A randomized, comparative, open-label, multicenter, phase 3 clinical trial, Int. J. Infect. Dis
Vicenzi, The liaison between respiratory failure and high blood pressure: Evidence from COVID-19 patients, Eur. Respir. J, doi:10.1183/13993003.01157-2020
Vincent, Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: Results of a multicenter, prospective study. Working group on "sepsis-related problems" of the European Society of Intensive Care Medicine, Crit. Care Med, doi:10.1097/00003246-199811000-00016
Yao, Vitro antiviral activity and projection of optimized dosing design of hydroxychloroquine for the treatment of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), Clin. Infect. Dis, doi:10.1093/cid/ciaa237
Yaylaci, The effects of favipiravir on hematological parameters of covıd-19 patients, Rev. Assoc Med. Bras, doi:10.1590/1806-9282.66.S2.65
DOI record:
{
"DOI": "10.1038/s41598-022-08794-w",
"ISSN": [
"2045-2322"
],
"URL": "http://dx.doi.org/10.1038/s41598-022-08794-w",
"abstract": "<jats:title>Abstract</jats:title><jats:p>Favipiravir has antiviral activity against influenza, West Nile virus, and yellow fever virus and against flaviviruses. The objective of this pilot study was to compare three arms: favipiravir; hydroxychloroquine; standard care (no specific SARS-CoV-2 treatment) only, in symptomatic patients infected by SARS-CoV-2 in an open-labelled randomized clinical trial. The trial was registered with Bahrain National Taskforce for Combatting COVID-19 on the 7th of May 2020 (registration code: NCT04387760). 150 symptomatic patients with COVID-19 disease were randomized into one of three arms: favipiravir, hydroxychloroquine, or standard care only. The primary outcome was the clinical scale at the end of study follow up (day 14 or on discharge/death) based on a points scale. The secondary outcomes were viral clearance, biochemical parameter changes and mortality at 30-days. Baseline characteristics did not differ between groups. The proportion of patients who achieved a clinical scale < 2 did not differ between groups. The favipiravir-treated and hydroxychloroquine-treated group showed increased viral clearance (OR, 95%CI 2.38, 0.83–6.78, OR, 95%CI 2.15, 0.78–5.92, respectively) compared to standard care, but this was not significant. The biochemical profile did not differ between groups, except for the platelet count (<jats:italic>P</jats:italic> < 0.03) and uric acid (<jats:italic>P</jats:italic> < 0.004) that were higher with favipiravir-treatment. Primary or secondary outcome measures did not differ between favipiravir, hydroxychloroquine, and standard therapy for mild to moderate COVID-19 disease; therefore, whilst favipiravir therapy appeared safe with a trend to increased viral clearance, there was no superior therapeutic utility.</jats:p><jats:p>Clinical trials registration. NCT04387760. Registration date: 07/05/2020.</jats:p>",
"alternative-id": [
"8794"
],
"article-number": "4925",
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "12 July 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "7 February 2022"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "23 March 2022"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Change Date",
"name": "change_date",
"order": 4,
"value": "26 September 2022"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Change Type",
"name": "change_type",
"order": 5,
"value": "Correction"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Change Details",
"name": "change_details",
"order": 6,
"value": "A Correction to this paper has been published:"
},
{
"URL": "https://doi.org/10.1038/s41598-022-20899-w",
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Change Details",
"name": "change_details",
"order": 7,
"value": "https://doi.org/10.1038/s41598-022-20899-w"
},
{
"group": {
"label": "Competing interests",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1,
"value": "The authors declare no competing interests."
}
],
"author": [
{
"affiliation": [],
"family": "AlQahtani",
"given": "Manaf",
"sequence": "first"
},
{
"affiliation": [],
"family": "Kumar",
"given": "Nitya",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Aljawder",
"given": "Dhuha",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Abdulrahman",
"given": "Abdulkarim",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mohamed",
"given": "Mohammed Wael",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alnashaba",
"given": "Fatema",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fayyad",
"given": "Mohammed Abu",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alshaikh",
"given": "Faisal",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alsahaf",
"given": "Fatima",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Saeed",
"given": "Sawsan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Almahroos",
"given": "Amal",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Abdulrahim",
"given": "Zainab",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Otoom",
"given": "Sameer",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Atkin",
"given": "Stephen L.",
"sequence": "additional"
}
],
"clinical-trial-number": [
{
"clinical-trial-number": "nct04387760",
"registry": "10.18810/clinical-trials-gov"
}
],
"container-title": "Scientific Reports",
"container-title-short": "Sci Rep",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2022,
3,
23
]
],
"date-time": "2022-03-23T11:04:41Z",
"timestamp": 1648033481000
},
"deposited": {
"date-parts": [
[
2022,
11,
25
]
],
"date-time": "2022-11-25T01:03:03Z",
"timestamp": 1669338183000
},
"indexed": {
"date-parts": [
[
2024,
3,
28
]
],
"date-time": "2024-03-28T04:36:24Z",
"timestamp": 1711600584424
},
"is-referenced-by-count": 20,
"issue": "1",
"issued": {
"date-parts": [
[
2022,
3,
23
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2022,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
3,
23
]
],
"date-time": "2022-03-23T00:00:00Z",
"timestamp": 1647993600000
}
},
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
3,
23
]
],
"date-time": "2022-03-23T00:00:00Z",
"timestamp": 1647993600000
}
}
],
"link": [
{
"URL": "https://www.nature.com/articles/s41598-022-08794-w.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.nature.com/articles/s41598-022-08794-w",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.nature.com/articles/s41598-022-08794-w.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1038",
"published": {
"date-parts": [
[
2022,
3,
23
]
]
},
"published-online": {
"date-parts": [
[
2022,
3,
23
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"key": "8794_CR1",
"unstructured": "Coronavirus Update (Live): 46,432,714 Cases and 1,200,927 Deaths from COVID-19 Virus Pandemic-Worldometer, https://www.worldometers.info/coronavirus/."
},
{
"DOI": "10.7326/m20-6169",
"author": "DV Mehrotra",
"doi-asserted-by": "publisher",
"first-page": "221",
"journal-title": "Ann. Intern. Med.",
"key": "8794_CR2",
"unstructured": "Mehrotra, D. V. et al. Clinical endpoints for evaluating efficacy in COVID-19 vaccine trials. Ann. Intern. Med. 174, 221–228. https://doi.org/10.7326/m20-6169 (2021).",
"volume": "174",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2007764",
"author": "JH Beigel",
"doi-asserted-by": "publisher",
"journal-title": "N. Engl. J. Med.",
"key": "8794_CR3",
"unstructured": "Beigel, J. H. et al. Remdesivir for the treatment of Covid-19-preliminary report. N. Engl. J. Med. https://doi.org/10.1056/NEJMoa2007764 (2020).",
"year": "2020"
},
{
"DOI": "10.1016/j.ajem.2020.04.035",
"author": "N Mehta",
"doi-asserted-by": "publisher",
"first-page": "1488",
"journal-title": "Am. J. Emerg. Med.",
"key": "8794_CR4",
"unstructured": "Mehta, N., Mazer-Amirshahi, M., Alkindi, N. & Pourmand, A. Pharmacotherapy in COVID-19; A narrative review for emergency providers. Am. J. Emerg. Med. 38, 1488–1493. https://doi.org/10.1016/j.ajem.2020.04.035 (2020).",
"volume": "38",
"year": "2020"
},
{
"DOI": "10.1016/j.ijantimicag.2020.105949",
"author": "P Gautret",
"doi-asserted-by": "publisher",
"journal-title": "Int. J. Antimicrob. Agents",
"key": "8794_CR5",
"unstructured": "Gautret, P. et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: Results of an open-label non-randomized clinical trial. Int. J. Antimicrob. Agents 56, 105949. https://doi.org/10.1016/j.ijantimicag.2020.105949 (2020).",
"volume": "56",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2012410",
"author": "J Geleris",
"doi-asserted-by": "publisher",
"first-page": "2411",
"journal-title": "N. Engl. J. Med.",
"key": "8794_CR6",
"unstructured": "Geleris, J. et al. Observational study of hydroxychloroquine in hospitalized patients with Covid-19. N. Engl. J. Med. 382, 2411–2418. https://doi.org/10.1056/NEJMoa2012410 (2020).",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1136/bmj.m1849",
"author": "W Tang",
"doi-asserted-by": "publisher",
"journal-title": "BMJ",
"key": "8794_CR7",
"unstructured": "Tang, W. et al. Hydroxychloroquine in patients with mainly mild to moderate coronavirus disease 2019: Open label, randomised controlled trial. BMJ 369, m1849. https://doi.org/10.1136/bmj.m1849 (2020).",
"volume": "369",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2021801",
"author": "O Mitjà",
"doi-asserted-by": "publisher",
"first-page": "417",
"journal-title": "N. Engl. J. Med.",
"key": "8794_CR8",
"unstructured": "Mitjà, O. et al. A cluster-randomized trial of hydroxychloroquine for prevention of Covid-19. N. Engl. J. Med. 384, 417–427. https://doi.org/10.1056/NEJMoa2021801 (2021).",
"volume": "384",
"year": "2021"
},
{
"DOI": "10.1080/14787210.2020.1813024",
"author": "D Echeverría-Esnal",
"doi-asserted-by": "publisher",
"first-page": "147",
"journal-title": "Expert Rev. Anti Infect. Ther.",
"key": "8794_CR9",
"unstructured": "Echeverría-Esnal, D. et al. Azithromycin in the treatment of COVID-19: A review. Expert Rev. Anti Infect. Ther. 19, 147–163. https://doi.org/10.1080/14787210.2020.1813024 (2021).",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.1038/s41598-021-89444-5",
"author": "M AlQahtani",
"doi-asserted-by": "publisher",
"first-page": "9927",
"journal-title": "Sci. Rep.",
"key": "8794_CR10",
"unstructured": "AlQahtani, M. et al. Randomized controlled trial of convalescent plasma therapy against standard therapy in patients with severe COVID-19 disease. Sci. Rep. 11, 9927. https://doi.org/10.1038/s41598-021-89444-5 (2021).",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1007/s10238-020-00671-y",
"author": "M Gavriatopoulou",
"doi-asserted-by": "publisher",
"first-page": "167",
"journal-title": "Clin. Exp. Med.",
"key": "8794_CR11",
"unstructured": "Gavriatopoulou, M. et al. Emerging treatment strategies for COVID-19 infection. Clin. Exp. Med. 21, 167–179. https://doi.org/10.1007/s10238-020-00671-y (2021).",
"volume": "21",
"year": "2021"
},
{
"DOI": "10.1002/cbic.202000595",
"author": "RO Sreekanth",
"doi-asserted-by": "publisher",
"first-page": "939",
"journal-title": "Chembiochem Eur. J. Chem. Biol.",
"key": "8794_CR12",
"unstructured": "Sreekanth, R. O. & Lai, W.-F. Tackling COVID-19 using remdesivir and favipiravir as therapeutic options. Chembiochem Eur. J. Chem. Biol. 22, 939–948. https://doi.org/10.1002/cbic.202000595 (2021).",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1016/j.antiviral.2018.03.003",
"author": "L Delang",
"doi-asserted-by": "publisher",
"first-page": "85",
"journal-title": "Antiviral Res.",
"key": "8794_CR13",
"unstructured": "Delang, L., Abdelnabi, R. & Neyts, J. Favipiravir as a potential countermeasure against neglected and emerging RNA viruses. Antiviral Res. 153, 85–94. https://doi.org/10.1016/j.antiviral.2018.03.003 (2018).",
"volume": "153",
"year": "2018"
},
{
"DOI": "10.5582/ddt.2020.01012",
"author": "L Dong",
"doi-asserted-by": "publisher",
"first-page": "58",
"journal-title": "Drug Discover. Therap.",
"key": "8794_CR14",
"unstructured": "Dong, L., Hu, S. & Gao, J. Discovering drugs to treat coronavirus disease 2019 (COVID-19). Drug Discover. Therap. 14, 58–60. https://doi.org/10.5582/ddt.2020.01012 (2020).",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1016/j.eng.2020.03.007",
"author": "Q Cai",
"doi-asserted-by": "publisher",
"first-page": "1192",
"journal-title": "Engineering (Beijing)",
"key": "8794_CR15",
"unstructured": "Cai, Q. et al. Experimental treatment with favipiravir for COVID-19: An open-label control study. Engineering (Beijing) 6, 1192–1198. https://doi.org/10.1016/j.eng.2020.03.007 (2020).",
"volume": "6",
"year": "2020"
},
{
"DOI": "10.2807/1560-7917.Es.2020.25.3.2000045",
"author": "VM Corman",
"doi-asserted-by": "publisher",
"journal-title": "Euro Surveill",
"key": "8794_CR16",
"unstructured": "Corman, V. M. et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill https://doi.org/10.2807/1560-7917.Es.2020.25.3.2000045 (2020).",
"year": "2020"
},
{
"DOI": "10.1097/00003246-199811000-00016",
"author": "JL Vincent",
"doi-asserted-by": "publisher",
"first-page": "1793",
"journal-title": "Crit. Care Med.",
"key": "8794_CR17",
"unstructured": "Vincent, J. L. et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: Results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit. Care Med. 26, 1793–1800. https://doi.org/10.1097/00003246-199811000-00016 (1998).",
"volume": "26",
"year": "1998"
},
{
"DOI": "10.1016/j.intimp.2020.107301",
"author": "M Shah",
"doi-asserted-by": "publisher",
"journal-title": "Int. Immunopharmacol.",
"key": "8794_CR18",
"unstructured": "Shah, M. et al. Safety and efficacy of ozone therapy in mild to moderate COVID-19 patients: A phase 1/11 randomized control trial (SEOT study). Int. Immunopharmacol. 91, 107301. https://doi.org/10.1016/j.intimp.2020.107301 (2021).",
"volume": "91",
"year": "2021"
},
{
"DOI": "10.1016/j.tmaid.2020.101663",
"author": "P Gautret",
"doi-asserted-by": "publisher",
"journal-title": "Travel Med. Infect. Dis.",
"key": "8794_CR19",
"unstructured": "Gautret, P. et al. Clinical and microbiological effect of a combination of hydroxychloroquine and azithromycin in 80 COVID-19 patients with at least a six-day follow up: A pilot observational study. Travel Med. Infect. Dis. 34, 101663. https://doi.org/10.1016/j.tmaid.2020.101663 (2020).",
"volume": "34",
"year": "2020"
},
{
"DOI": "10.1002/sim.4780132309",
"author": "MA Birkett",
"doi-asserted-by": "publisher",
"first-page": "2455",
"journal-title": "Stat. Med.",
"key": "8794_CR20",
"unstructured": "Birkett, M. A. & Day, S. J. Internal pilot studies for estimating sample size. Stat. Med. 13, 2455–2463 (1994).",
"volume": "13",
"year": "1994"
},
{
"DOI": "10.1016/j.ijid.2020.11.142",
"author": "ZF Udwadia",
"doi-asserted-by": "publisher",
"first-page": "62",
"journal-title": "Int. J. Infect. Dis.",
"key": "8794_CR21",
"unstructured": "Udwadia, Z. F. et al. Efficacy and safety of favipiravir, an oral RNA-dependent RNA polymerase inhibitor, in mild-to-moderate COVID-19: A randomized, comparative, open-label, multicenter, phase 3 clinical trial. Int. J. Infect. Dis. 103, 62–71 (2021).",
"volume": "103",
"year": "2021"
},
{
"DOI": "10.1038/s41598-021-90551-6",
"author": "S Hassanipour",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Sci. Rep.",
"key": "8794_CR22",
"unstructured": "Hassanipour, S. et al. The efficacy and safety of Favipiravir in treatment of COVID-19: A systematic review and meta-analysis of clinical trials. Sci. Rep. 11, 1–11 (2021).",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1183/13993003.01157-2020",
"author": "M Vicenzi",
"doi-asserted-by": "publisher",
"journal-title": "Eur. Respir. J.",
"key": "8794_CR23",
"unstructured": "Vicenzi, M. et al. The liaison between respiratory failure and high blood pressure: Evidence from COVID-19 patients. Eur. Respir. J. https://doi.org/10.1183/13993003.01157-2020 (2020).",
"year": "2020"
},
{
"DOI": "10.1590/1806-9282.66.S2.65",
"author": "S Yaylaci",
"doi-asserted-by": "publisher",
"first-page": "65",
"issue": "2",
"journal-title": "Rev. Assoc Med. Bras (1992)",
"key": "8794_CR24",
"unstructured": "Yaylaci, S. et al. The effects of favipiravir on hematological parameters of covıd-19 patients. Rev. Assoc Med. Bras (1992) 66(2), 65–70. https://doi.org/10.1590/1806-9282.66.S2.65 (2020).",
"volume": "66",
"year": "2020"
},
{
"DOI": "10.1620/tjem.251.87",
"author": "E Mishima",
"doi-asserted-by": "publisher",
"first-page": "87",
"journal-title": "Tohoku J. Exp. Med.",
"key": "8794_CR25",
"unstructured": "Mishima, E., Anzai, N., Miyazaki, M. & Abe, T. Uric acid elevation by favipiravir, an antiviral drug. Tohoku J. Exp. Med. 251, 87–90. https://doi.org/10.1620/tjem.251.87 (2020).",
"volume": "251",
"year": "2020"
},
{
"DOI": "10.1016/j.resinv.2020.08.001",
"author": "K Murohashi",
"doi-asserted-by": "publisher",
"first-page": "430",
"journal-title": "Respir. Investig.",
"key": "8794_CR26",
"unstructured": "Murohashi, K. et al. Outcome of early-stage combination treatment with favipiravir and methylprednisolone for severe COVID-19 pneumonia: A report of 11 cases. Respir. Investig. 58, 430–434. https://doi.org/10.1016/j.resinv.2020.08.001 (2020).",
"volume": "58",
"year": "2020"
},
{
"DOI": "10.1093/cid/ciaa237",
"author": "X Yao",
"doi-asserted-by": "publisher",
"first-page": "732",
"journal-title": "Clin. Infect. Dis.",
"key": "8794_CR27",
"unstructured": "Yao, X. et al. In Vitro antiviral activity and projection of optimized dosing design of hydroxychloroquine for the treatment of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Clin. Infect. Dis. 71, 732–739. https://doi.org/10.1093/cid/ciaa237 (2020).",
"volume": "71",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2012410",
"author": "J Geleris",
"doi-asserted-by": "publisher",
"first-page": "2411",
"journal-title": "N. Engl. J. Med.",
"key": "8794_CR28",
"unstructured": "Geleris, J. et al. Observational study of hydroxychloroquine in hospitalized patients with Covid-19. N. Engl. J. Med. 382, 2411–2418 (2020).",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1038/s41598-020-77748-x",
"author": "RM Ghazy",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Sci. Rep.",
"key": "8794_CR29",
"unstructured": "Ghazy, R. M. et al. A systematic review and meta-analysis on chloroquine and hydroxychloroquine as monotherapy or combined with azithromycin in COVID-19 treatment. Sci. Rep. 10, 1–18 (2020).",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1007/s40121-020-00324-3",
"author": "SN Rao",
"doi-asserted-by": "publisher",
"first-page": "573",
"journal-title": "Infect. Dis. Ther.",
"key": "8794_CR30",
"unstructured": "Rao, S. N., Manissero, D., Steele, V. R. & Pareja, J. A systematic review of the clinical utility of cycle threshold values in the context of COVID-19. Infect. Dis. Ther. 9, 573–586. https://doi.org/10.1007/s40121-020-00324-3 (2020).",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1073/pnas.2017962118",
"author": "N Néant",
"doi-asserted-by": "publisher",
"first-page": "1008",
"journal-title": "Proc. Natl. Acad. Sci. USA",
"key": "8794_CR31",
"unstructured": "Néant, N. et al. (2021) Modeling SARS-CoV-2 viral kinetics and association with mortality in hospitalized patients from the French COVID cohort. Proc. Natl. Acad. Sci. USA 118, 1008. https://doi.org/10.1073/pnas.2017962118 (2021).",
"volume": "118",
"year": "2021"
}
],
"reference-count": 31,
"references-count": 31,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.nature.com/articles/s41598-022-08794-w"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Multidisciplinary"
],
"subtitle": [],
"title": "Randomized controlled trial of favipiravir, hydroxychloroquine, and standard care in patients with mild/moderate COVID-19 disease",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "12"
}
alqahtani2