Remdesivir for the Treatment of Covid-19 — Final Report
et al., NEJM, doi:10.1056/NEJMoa2007764, ACTT-1, NCT04280705, Oct 2020
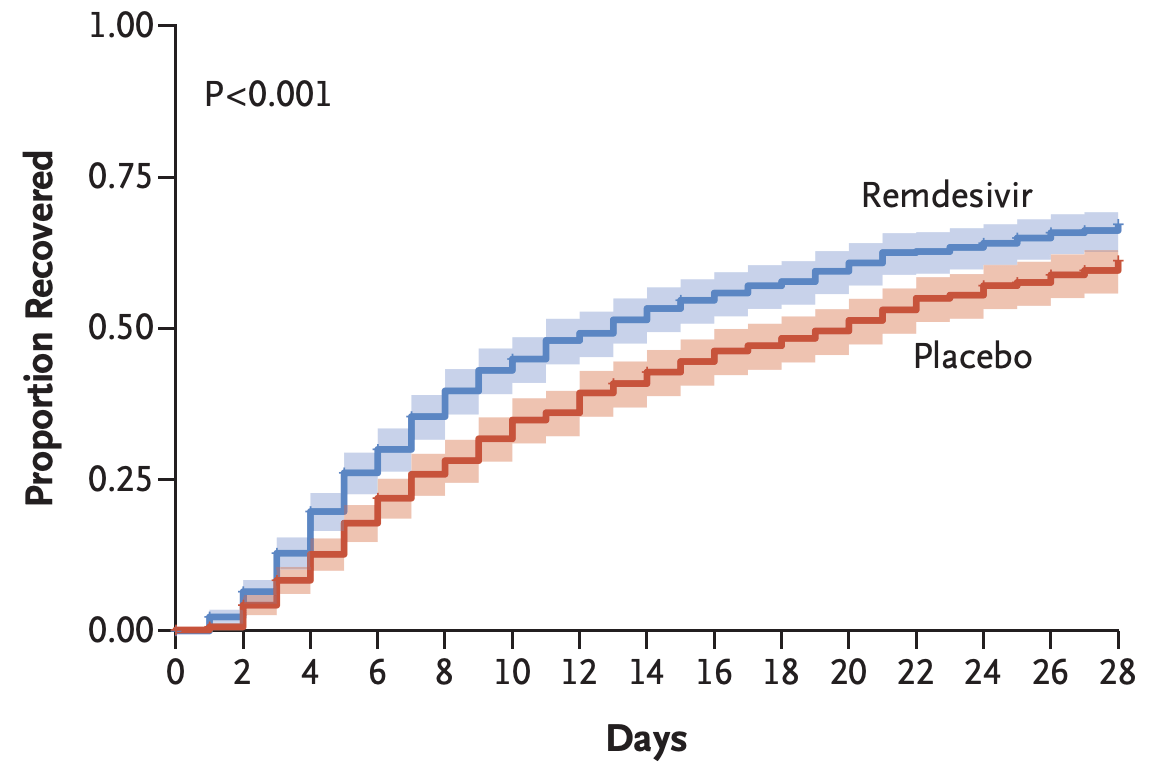
RCT 1,062 hospitalized patients showing faster recovery time with treatment, median 10 days vs. 15 days for placebo, rate ratio for recovery 1.29, p<0.001. Day 29 mortality was 11.4% with remdesivir and 15.2% with placebo, hazard ratio HR 0.73 [0.52-1.03].
Gérard, Zhou, Wu, Kamo, Choi, Kim show increased risk of acute kidney injury, Leo, Briciu, Muntean, Petrov show increased risk of liver injury, and Negru, Cheng, Mohammed, Kwok show increased risk of cardiac disorders with remdesivir.
Remdesivir efficacy disappears with longer
followup. Mixed-effects meta-regression of efficacy as a function of
followup duration across all remdesivir studies shows decreasing efficacy with
longer followup15. This may reflect
antiviral efficacy being offset by serious adverse effects of treatment.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments16.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
risk of death, 27.0% lower, HR 0.73, p = 0.07, treatment 541, control 521, day 29.
|
|
risk of death, 45.0% lower, HR 0.55, p = 0.005, treatment 541, control 521, day 15.
|
|
risk of no recovery, 22.5% lower, RR 0.78, p < 0.001, treatment 541, control 521, inverted to make RR<1 favor treatment.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Gérard et al., Remdesivir and Acute Renal Failure: A Potential Safety Signal From Disproportionality Analysis of the WHO Safety Database, Clinical Pharmacology & Therapeutics, doi:10.1002/cpt.2145.
2.
Zhou et al., Acute Kidney Injury and Drugs Prescribed for COVID-19 in Diabetes Patients: A Real-World Disproportionality Analysis, Frontiers in Pharmacology, doi:10.3389/fphar.2022.833679.
3.
Wu et al., Acute Kidney Injury Associated With Remdesivir: A Comprehensive Pharmacovigilance Analysis of COVID-19 Reports in FAERS, Frontiers in Pharmacology, doi:10.3389/fphar.2022.692828.
4.
Kamo et al., Association of Antiviral Drugs for the Treatment of COVID-19 With Acute Renal Failure, In Vivo, doi:10.21873/invivo.13637.
5.
Choi et al., Comparative effectiveness of combination therapy with nirmatrelvir–ritonavir and remdesivir versus monotherapy with remdesivir or nirmatrelvir–ritonavir in patients hospitalised with COVID-19: a target trial emulation study, The Lancet Infectious Diseases, doi:10.1016/S1473-3099(24)00353-0.
6.
Kim et al., Investigating the Safety Profile of Fast‐Track COVID‐19 Drugs Using the FDA Adverse Event Reporting System Database: A Comparative Observational Study, Pharmacoepidemiology and Drug Safety, doi:10.1002/pds.70043.
7.
Leo et al., Hepatocellular liver injury in hospitalized patients affected by COVID-19: Presence of different risk factors at different time points, Digestive and Liver Disease, doi:10.1016/j.dld.2021.12.014.
8.
Briciu et al., Evolving Clinical Manifestations and Outcomes in COVID-19 Patients: A Comparative Analysis of SARS-CoV-2 Variant Waves in a Romanian Hospital Setting, Pathogens, doi:10.3390/pathogens12121453.
9.
Muntean et al., Effects of COVID-19 on the Liver and Mortality in Patients with SARS-CoV-2 Pneumonia Caused by Delta and Non-Delta Variants: An Analysis in a Single Centre, Pharmaceuticals, doi:10.3390/ph17010003.
10.
Petrov et al., The Effect of Potentially Hepatotoxic Medicinal Products on Alanine Transaminase Levels in COVID-19 Patients: A Case–Control Study, Safety and Risk of Pharmacotherapy, doi:10.30895/2312-7821-2025-458.
11.
Negru et al., Comparative Pharmacovigilance Analysis of Approved and Repurposed Antivirals for COVID-19: Insights from EudraVigilance Data, Biomedicines, doi:10.3390/biomedicines13061387.
12.
Cheng et al., Cardiovascular Safety of COVID-19 Treatments: A Disproportionality Analysis of Adverse Event Reports from the WHO VigiBase, Infectious Diseases and Therapy, doi:10.1007/s40121-025-01225-z.
13.
Mohammed et al., Bradycardia associated with remdesivir treatment in coronavirus disease 2019 patients: A propensity score-matched analysis, Medicine, doi:10.1097/MD.0000000000044501.
Beigel et al., 8 Oct 2020, Randomized Controlled Trial, USA, peer-reviewed, 40 authors, average treatment delay 9.0 days, trial NCT04280705 (history) (ACTT-1).
Remdesivir for the Treatment of Covid-19 — Final Report
New England Journal of Medicine, doi:10.1056/nejmoa2007764
BACKGROUND Although several therapeutic agents have been evaluated for the treatment of coronavirus disease 2019 (Covid-19), no antiviral agents have yet been shown to be efficacious.
METHODS We conducted a double-blind, randomized, placebo-controlled trial of intravenous remdesivir in adults who were hospitalized with Covid-19 and had evidence of lower respiratory tract infection. Patients were randomly assigned to receive either remdesivir (200 mg loading dose on day 1, followed by 100 mg daily for up to 9 additional days) or placebo for up to 10 days. The primary outcome was the time to recovery, defined by either discharge from the hospital or hospitalization for infection-control purposes only.
RESULTS A total of 1062 patients underwent randomization (with 541 assigned to remdesivir and 521 to placebo). Those who received remdesivir had a median recovery time of 10 days (95% confidence interval [CI], 9 to 11), as compared with 15 days (95% CI, 13 to 18) among those who received placebo (rate ratio for recovery, 1.29; 95% CI, 1.12 to 1.49; P<0.001, by a log-rank test). In an analysis that used a proportional-odds model with an eight-category ordinal scale, the patients who received remdesivir were found to be more likely than those who received placebo to have clinical improvement at day 15 (odds ratio, 1.5; 95% CI, 1.2 to 1.9, after adjustment for actual disease severity). The Kaplan-Meier estimates of mortality were 6.7% with remdesivir and 11.9% with placebo by day 15 and 11.4% with remdesivir and 15.2% with placebo by day 29 (hazard ratio, 0.73; 95% CI, 0.52 to 1.03). Serious adverse events were reported in 131 of the 532 patients who received remdesivir (24.6%) and in 163 of the 516 patients who received placebo (31.6%).
CONCLUSIONS Our data show that remdesivir was superior to placebo in shortening the time to recovery in adults who were hospitalized with Covid-19 and had evidence of lower respiratory tract infection. (Funded by the National Institute of Allergy and Infectious Diseases and others; ACTT-1 ClinicalTrials.gov number, NCT04280705.
T h e ne w e ngl a nd jou r na l o f m e dicine The amendment was proposed on March 22, 2020, by trial statisticians who were unaware of treatment assignment and had no knowledge of outcome data; when this change was proposed 72 patients had been enrolled. Although changes in the primary outcome are not common in trials for diseases that are well understood, it is recognized that in some trials, such as those involving poorly understood diseases, circumstances may require a change in the way an outcome is assessed or may necessitate a different outcome. 16 The original primary outcome became the key secondary end point. In the end, findings for both primary and key secondary end points were significantly different between the remdesivir and placebo groups. Copyright © 2020 Massachusetts Medical Society. All rights reserved.
References
Agostini, Andres, Sims, Coronavirus susceptibility to the antiviral remdesivir (GS-5734) is mediated by the viral polymerase and the proofreading exoribonuclease, mBio
Borba, Val, Sampaio, Effect of high vs low doses of chloroquine diphosphate as adjunctive therapy for patients hospitalized with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection: a randomized clinical trial, JAMA Netw Open
Brown, Won, Graham, Broad spectrum antiviral remdesivir inhibits human endemic and zoonotic deltacoronaviruses with a highly divergent RNA dependent RNA polymerase, Antiviral Res
Cao, Wang, Wen, A trial of lopinavir-ritonavir in adults hospitalized with severe Covid-19, N Engl J Med
De Wit, Feldmann, Cronin, Prophylactic and therapeutic remdesivir (GS-5734) treatment in the rhesus macaque model of MERS-CoV infection, Proc Natl Acad Sci U S A
De Wit, Rasmussen, Falzarano, Middle East respiratory syndrome coronavirus (MERS-CoV) causes transient lower respiratory tract infection in rhesus macaques, Proc Natl Acad Sci U S A
Helmy, Fawzy, Elaswad, Sobieh, Kenney et al., The COVID-19 pandemic: a comprehensive review of taxonomy, genetics, epidemiology, diagnosis, treatment, and control, J Clin Med
King, Beigel, Ison, Clinical development of therapeutic agents for hospitalized patients with influenza: challenges and innovations, Open Forum Infect Dis
Loo, School, Medicine, National Center for Infectious Diseases-Tan Tock Seng Hospital-Lee Kong Chian School of Medicine
Massachusetts, Hospital, Boston, and the South Texas Veterans Health Care System
Neaton, Timothy, Burgess, Tyler Bonnett, Green et al., The authors' affiliations are as follows: the National Institute of Allergy and Infectious Diseases
Sheahan, Sims, Graham, Broad-spectrum antiviral GS-5734 inhibits both epidemic and zoonotic coronaviruses, Sci Transl Med
Sheahan, Sims, Leist, Comparative therapeutic efficacy of remdesivir and combination lopinavir, ritonavir, and interferon beta against MERS-CoV, Nat Commun
Spinner, Gottlieb, Criner, Effect of remdesivir vs standard care on clinical status at 11 days in patients with moderate COVID-19: a randomized clinical trial, JAMA
The, Group, Changes to trial design
The, Group, Dexamethasone in hospitalized patients with Covid-19 -preliminary report, N Engl J Med, doi:10.1056/NEJMoa2021436
Wang, Cao, Zhang, Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro, Cell Res
Wang, Zhang, Du, Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial, Lancet
DOI record:
{
"DOI": "10.1056/nejmoa2007764",
"ISSN": [
"0028-4793",
"1533-4406"
],
"URL": "http://dx.doi.org/10.1056/NEJMoa2007764",
"alternative-id": [
"10.1056/NEJMoa2007764"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-4879-4941",
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"authenticated-orcid": false,
"family": "Beigel",
"given": "John H.",
"sequence": "first"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Tomashek",
"given": "Kay M.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Dodd",
"given": "Lori E.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Mehta",
"given": "Aneesh K.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Zingman",
"given": "Barry S.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6489-6294",
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"authenticated-orcid": false,
"family": "Kalil",
"given": "Andre C.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Hohmann",
"given": "Elizabeth",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Chu",
"given": "Helen Y.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Luetkemeyer",
"given": "Annie",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Kline",
"given": "Susan",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Lopez de Castilla",
"given": "Diego",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Finberg",
"given": "Robert W.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Dierberg",
"given": "Kerry",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Tapson",
"given": "Victor",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Hsieh",
"given": "Lanny",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Patterson",
"given": "Thomas F.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Paredes",
"given": "Roger",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Sweeney",
"given": "Daniel A.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Short",
"given": "William R.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Touloumi",
"given": "Giota",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0324-0205",
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"authenticated-orcid": false,
"family": "Lye",
"given": "David Chien",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Ohmagari",
"given": "Norio",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Oh",
"given": "Myoung-don",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Ruiz-Palacios",
"given": "Guillermo M.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Benfield",
"given": "Thomas",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Fätkenheuer",
"given": "Gerd",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Kortepeter",
"given": "Mark G.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Atmar",
"given": "Robert L.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Creech",
"given": "C. Buddy",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Lundgren",
"given": "Jens",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Babiker",
"given": "Abdel G.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Pett",
"given": "Sarah",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Neaton",
"given": "James D.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Burgess",
"given": "Timothy H.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Bonnett",
"given": "Tyler",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Green",
"given": "Michelle",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Makowski",
"given": "Mat",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Osinusi",
"given": "Anu",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"family": "Nayak",
"given": "Seema",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9509-1045",
"affiliation": [
{
"name": "From the National Institute of Allergy and Infectious Diseases, National Institutes of Health (J.H.B., K.M.T., L.E.D., S.N., H.C.L.), and the Infectious Disease Clinical Research Program, Uniformed Services University of the Health Sciences (T.H.B.), Bethesda, the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick (T. Bonnett), and Emmes, Rockville (M.G., M.M.) — all in Maryland; Emory University, Atlanta (A.K.M.); Montefiore Medical..."
}
],
"authenticated-orcid": false,
"family": "Lane",
"given": "H. Clifford",
"sequence": "additional"
}
],
"container-title": "New England Journal of Medicine",
"container-title-short": "N Engl J Med",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2020,
5,
22
]
],
"date-time": "2020-05-22T21:45:22Z",
"timestamp": 1590183922000
},
"deposited": {
"date-parts": [
[
2022,
8,
18
]
],
"date-time": "2022-08-18T13:38:25Z",
"timestamp": 1660829905000
},
"funder": [
{
"DOI": "10.13039/100006492",
"doi-asserted-by": "publisher",
"name": "Division of Intramural Research, National Institute of Allergy and Infectious Diseases"
},
{
"DOI": "10.13039/100000054",
"award": [
"HHSN261200800001E",
"HHSN261201500003I"
],
"doi-asserted-by": "publisher",
"name": "National Cancer Institute"
},
{
"DOI": "10.13039/100000060",
"award": [
"UM1AI148450",
"UM1AI148452",
"UM1AI148573",
"UM1AI148575",
"UM1AI148576",
"UM1AI148684",
"UM1AI148685",
"UM1AI148689"
],
"doi-asserted-by": "publisher",
"name": "National Institute of Allergy and Infectious Diseases"
}
],
"indexed": {
"date-parts": [
[
2024,
4,
9
]
],
"date-time": "2024-04-09T17:54:50Z",
"timestamp": 1712685290202
},
"is-referenced-by-count": 5244,
"issue": "19",
"issued": {
"date-parts": [
[
2020,
11,
5
]
]
},
"journal-issue": {
"issue": "19",
"published-print": {
"date-parts": [
[
2020,
11,
5
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://www.nejmgroup.org/legal/terms-of-use.htm",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2020,
11,
5
]
],
"date-time": "2020-11-05T00:00:00Z",
"timestamp": 1604534400000
}
}
],
"link": [
{
"URL": "http://www.nejm.org/doi/pdf/10.1056/NEJMoa2007764",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "150",
"original-title": [],
"page": "1813-1826",
"prefix": "10.1056",
"published": {
"date-parts": [
[
2020,
11,
5
]
]
},
"published-print": {
"date-parts": [
[
2020,
11,
5
]
]
},
"publisher": "Massachusetts Medical Society",
"reference": [
{
"DOI": "10.3390/jcm9041225",
"doi-asserted-by": "publisher",
"key": "r1"
},
{
"DOI": "10.1056/NEJMoa2001282",
"doi-asserted-by": "publisher",
"key": "r2"
},
{
"DOI": "10.1001/jamanetworkopen.2020.8857",
"doi-asserted-by": "publisher",
"key": "r3"
},
{
"DOI": "10.1056/NEJMoa2021436",
"doi-asserted-by": "publisher",
"key": "r4"
},
{
"DOI": "10.1038/s41467-019-13940-6",
"doi-asserted-by": "publisher",
"key": "r5"
},
{
"DOI": "10.1128/mBio.00221-18",
"doi-asserted-by": "publisher",
"key": "r6"
},
{
"DOI": "10.1016/j.antiviral.2019.104541",
"doi-asserted-by": "publisher",
"key": "r7"
},
{
"DOI": "10.1126/scitranslmed.aal3653",
"doi-asserted-by": "publisher",
"key": "r8"
},
{
"DOI": "10.1038/s41422-020-0282-0",
"doi-asserted-by": "publisher",
"key": "r9"
},
{
"DOI": "10.1073/pnas.1310744110",
"doi-asserted-by": "publisher",
"key": "r10"
},
{
"DOI": "10.1073/pnas.1922083117",
"doi-asserted-by": "publisher",
"key": "r11"
},
{
"DOI": "10.1093/ofid/ofz137",
"doi-asserted-by": "publisher",
"key": "r13"
},
{
"DOI": "10.1016/S0140-6736(20)31022-9",
"doi-asserted-by": "publisher",
"key": "r14"
},
{
"DOI": "10.1001/jama.2020.16349",
"doi-asserted-by": "publisher",
"key": "r15"
}
],
"reference-count": 14,
"references-count": 14,
"relation": {
"has-review": [
{
"asserted-by": "object",
"id": "10.3410/f.737996445.793574807",
"id-type": "doi"
},
{
"asserted-by": "object",
"id": "10.3410/f.737996445.793581312",
"id-type": "doi"
}
]
},
"resource": {
"primary": {
"URL": "http://www.nejm.org/doi/10.1056/NEJMoa2007764"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Remdesivir for the Treatment of Covid-19 — Final Report",
"type": "journal-article",
"volume": "383"
}