Effects of COVID-19 on the Liver and Mortality in Patients with SARS-CoV-2 Pneumonia Caused by Delta and Non-Delta Variants: An Analysis in a Single Centre
et al., Pharmaceuticals, doi:10.3390/ph17010003, Dec 2023
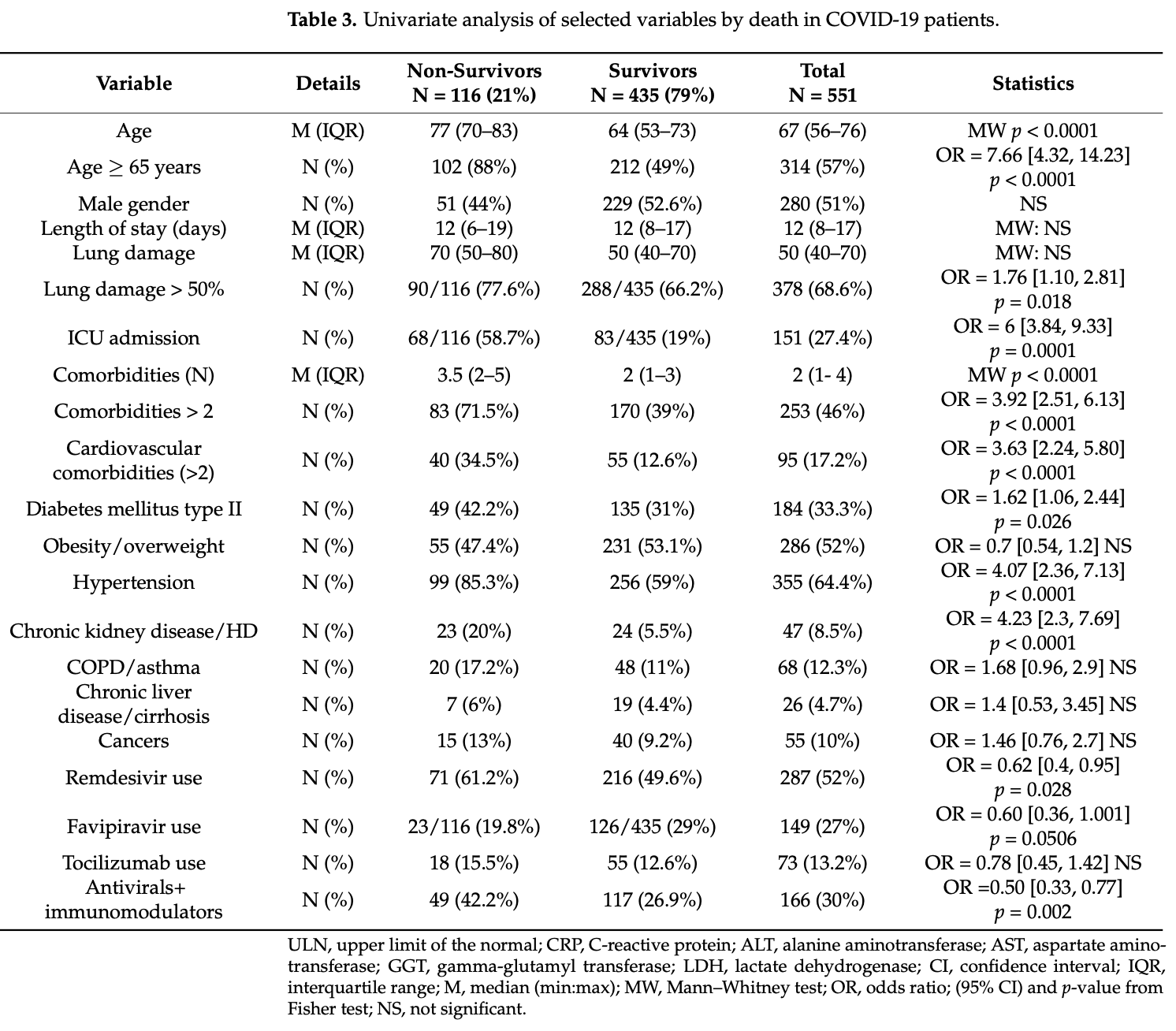
Retrospective 551 severe/critical COVID-19 patients showing higher mortality and higher risk of drug induced liver injury with remdesivir. Authors appear to have reversed the OR for remdesivir - use was more common in non-survivors (61% vs. 50%). Authors report 116 patients treated with HCQ but provide no results for HCQ.
Gérard, Zhou, Wu, Kamo, Choi, Kim show increased risk of acute kidney injury, Leo, Briciu, Muntean, Petrov show increased risk of liver injury, and Negru, Cheng, Mohammed, Kwok show increased risk of cardiac disorders with remdesivir.
|
risk of death, 45.1% higher, RR 1.45, p = 0.03, treatment 71 of 287 (24.7%), control 45 of 264 (17.0%).
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Gérard et al., Remdesivir and Acute Renal Failure: A Potential Safety Signal From Disproportionality Analysis of the WHO Safety Database, Clinical Pharmacology & Therapeutics, doi:10.1002/cpt.2145.
2.
Zhou et al., Acute Kidney Injury and Drugs Prescribed for COVID-19 in Diabetes Patients: A Real-World Disproportionality Analysis, Frontiers in Pharmacology, doi:10.3389/fphar.2022.833679.
3.
Wu et al., Acute Kidney Injury Associated With Remdesivir: A Comprehensive Pharmacovigilance Analysis of COVID-19 Reports in FAERS, Frontiers in Pharmacology, doi:10.3389/fphar.2022.692828.
4.
Kamo et al., Association of Antiviral Drugs for the Treatment of COVID-19 With Acute Renal Failure, In Vivo, doi:10.21873/invivo.13637.
5.
Choi et al., Comparative effectiveness of combination therapy with nirmatrelvir–ritonavir and remdesivir versus monotherapy with remdesivir or nirmatrelvir–ritonavir in patients hospitalised with COVID-19: a target trial emulation study, The Lancet Infectious Diseases, doi:10.1016/S1473-3099(24)00353-0.
6.
Kim et al., Investigating the Safety Profile of Fast‐Track COVID‐19 Drugs Using the FDA Adverse Event Reporting System Database: A Comparative Observational Study, Pharmacoepidemiology and Drug Safety, doi:10.1002/pds.70043.
7.
Leo et al., Hepatocellular liver injury in hospitalized patients affected by COVID-19: Presence of different risk factors at different time points, Digestive and Liver Disease, doi:10.1016/j.dld.2021.12.014.
8.
Briciu et al., Evolving Clinical Manifestations and Outcomes in COVID-19 Patients: A Comparative Analysis of SARS-CoV-2 Variant Waves in a Romanian Hospital Setting, Pathogens, doi:10.3390/pathogens12121453.
9.
Muntean et al., Effects of COVID-19 on the Liver and Mortality in Patients with SARS-CoV-2 Pneumonia Caused by Delta and Non-Delta Variants: An Analysis in a Single Centre, Pharmaceuticals, doi:10.3390/ph17010003.
10.
Petrov et al., The Effect of Potentially Hepatotoxic Medicinal Products on Alanine Transaminase Levels in COVID-19 Patients: A Case–Control Study, Safety and Risk of Pharmacotherapy, doi:10.30895/2312-7821-2025-458.
11.
Negru et al., Comparative Pharmacovigilance Analysis of Approved and Repurposed Antivirals for COVID-19: Insights from EudraVigilance Data, Biomedicines, doi:10.3390/biomedicines13061387.
12.
Cheng et al., Cardiovascular Safety of COVID-19 Treatments: A Disproportionality Analysis of Adverse Event Reports from the WHO VigiBase, Infectious Diseases and Therapy, doi:10.1007/s40121-025-01225-z.
Muntean et al., 19 Dec 2023, retrospective, Romania, peer-reviewed, 8 authors.
Contact: briciu.tincuta@umfcluj.ro (corresponding author), monica.muntean@umfcluj.ro, mihaela.lupse@yahoo.com, raulvlad.macicasan@gmail.com, csiszerdagnes@gmail.com, manole_alexandra20@yahoo.com, aradulescu@umfcluj.ro, colceardoina@gmail.com.
Effects of COVID-19 on the Liver and Mortality in Patients with SARS-CoV-2 Pneumonia Caused by Delta and Non-Delta Variants: An Analysis in a Single Centre
Pharmaceuticals, doi:10.3390/ph17010003
The aim of this study was to ascertain patient characteristics, outcomes, and liver injuries in patients infected with different SARS-CoV-2 variants. Data from consecutive adult patients with severe/critical COVID-19 admitted to our hospital during the peak month of the Delta wave were compared to the ancestral, Alpha, and Omicron waves. The dataset of 551 hospitalized patients was similar in the Delta/non-Delta waves. At admission and discharge, the median aminotransferase levels were normal or slightly increased. During the Delta wave (172 vs. 379 non-Delta patients), more patients died (OR 1.69, 95%CI 1.09-2.56) or had liver injury at discharge (alanine aminotransferase, ALT ≥ 2 ULN) (OR 1.97, 95%CI 1.08-3.54). In-hospital mortality was associated with age, lung injury, intensive care unit admission, number of and cardiovascular comorbidities, diabetes, chronic kidney disease, and all inflammatory biomarkers. Serious liver injury at admission (ALT ≥ 5 × ULN) was significantly associated with in-hospital mortality (OR = 7.9, 95%CI 2-28.9). At discharge, drug-induced liver injury (DILI) was found in patients treated with remdesivir, ALT ≥ 2 ULN (OR = 2.62, 95%CI 1.22-5.75). Treatment with dexamethasone, remdesivir, and immunomodulators showed improved survival, OR = 0.50 (95%CI 0.33-0.77). Regardless of the variant and treatment options, less than 2% of patients displayed serious liver injury, which was not found to be a death predictor in multivariable analysis.
Conflicts of Interest: The authors declare no conflict of interest.
References
Ahlstrand, Cajander, Cajander, Ingberg, Löf et al., Visual scoring of chest CT at hospital admission predicts hospitalization time and intensive care admission in COVID-19, Infect. Dis, doi:10.1080/23744235.2021.1910727
Amri, Bégin, Tessier, Vachon, Villeneuve et al., Use of Early Donated COVID-19 Convalescent Plasma Is Optimal to Preserve the Integrity of Lymphatic Endothelial Cells, Pharmaceuticals, doi:10.3390/ph15030365
Baldelli, Marjot, Barnes, Barritt, Webb et al., SARS-CoV-2 Infection and Liver Disease: A Review of Pathogenesis and Outcomes, Gut Liver, doi:10.5009/gnl220327
Batool, Vuthaluru, Hassan, Bseiso, Tehseen et al., Efficacy and Safety of Favipiravir in Treating COVID-19 Patients: A Meta-Analysis of Randomized Control Trials, Cureus, doi:10.7759/cureus.33676
Bennett, Moffitt, Hajagos, Amor, Anand et al., (N3C) Consortium. Clinical Characterization and Prediction of Clinical Severity of SARS-CoV-2 Infection among US Adults Using Data From the US National COVID Cohort Collaborative, JAMA Netw. Open, doi:10.1001/jamanetworkopen.2021.16901
Bergamaschi, Mescia, Turner, Hanson, Kotagiri et al., Longitudinal analysis reveals that delayed bystander CD8+ T cell activation and early immune pathology distinguish severe COVID-19 from mild disease, Immunity, doi:10.1016/j.immuni.2021.05.010
Bhaskaran, Bacon, Evans, Bates, Rentsch et al., Factors associated with deaths due to COVID-19 versus other causes: Population-based cohort analysis of UK primary care data and linked national death registrations within the OpenSAFELY platform, Lancet Reg. Health Eur, doi:10.1016/j.lanepe.2021.100109
Bhimraj, Morgan, Shumaker, Baden, Cheng et al., Infectious Diseases Society of America Guidelines on the Treatment and Management of Patients with COVID-19
Briciu, Leucuta, Muntean, Radulescu, Cismaru et al., Evolving Clinical Manifestations and Outcomes in COVID-19 Patients: A Comparative Analysis of SARS-CoV-2 Variant Waves in a Romanian Hospital Setting, Pathogens, doi:10.3390/pathogens12121453
Briciu, Topan, Calin, Dobrota, Leucuta et al., Comparison of COVID-19 Severity in Vaccinated and Unvaccinated Patients during the Delta and Omicron Wave of the Pandemic in a Romanian Tertiary Infectious Diseases Hospital, Healthcare, doi:10.3390/healthcare11030373
Cai, Huang, Yu, Zhu, Xia et al., COVID-19: Abnormal liver function tests, J. Hepatol, doi:10.1016/j.jhep.2020.04.006
Chaibi, Boussier, Hajj, Abitbol, Taieb et al., Liver function test abnormalities are associated with a poorer prognosis in COVID-19 patients: Results of a French cohort, Clin. Res. Hepatol. Gastroenterol, doi:10.1016/j.clinre.2020.10.002
Chew, Tang, Radcliffe, Caruana, Doilicho et al., Significant Liver Injury During Hospitalization for COVID-19 Is Not Associated with Liver Insufficiency or Death, Clin. Gastroenterol. Hepatol, doi:10.1016/j.cgh.2021.05.022
Conrozier, Lohse, Balblanc, Dussert, Royer et al., Biomarker variation in patients successfully treated with tocilizumab for severe coronavirus disease 2019 (COVID-19): Results of a multidisciplinary collaboration, Clin. Exp. Rheumatol
Core, A Language and Environment for Statistical Computing
Crisan, Avram, Grapa, Dragan, Radulescu et al., Liver Injury and Elevated FIB-4 Define a High-Risk Group in Patients with COVID-19, J. Clin. Med, doi:10.3390/jcm11010153
Danan, Teschke, RUCAM in Drug and Herb Induced Liver Injury: The Update, Int. J. Mol. Sci, doi:10.3390/ijms17010014
Deng, Lin, Mai, Liu, Chen, Clinical features and predictive factors related to liver injury in SARS-CoV-2 Delta and Omicron variant-infected patients, Eur. J. Gastroenterol. Hepatol, doi:10.1097/MEG.0000000000002381
Dufour, Marjot, Becchetti, Tilg, COVID-19 and liver disease, Gut, doi:10.1136/gutjnl-2021-326792
Ebrahimi, Simon, Hagström, Söderling, Wester et al., Risk of Severe Infection in Patients With Biopsy-proven Nonalcoholic Fatty Liver Disease-A Population-based Cohort Study, Clin. Gastroenterol. Hepatol, doi:10.1016/j.cgh.2023.05.013
Ekpanyapong, Bunchorntavakul, Reddy, COVID-19 and the liver: Lessons learnt from the EAST and the WEST, a year later, J. Viral Hepat, doi:10.1111/jvh.13590
Fu, Zhu, Bai, Han, He et al., Clinical features of patients infected with coronavirus disease 2019 with elevated liver biochemistries: A multicenter, retrospective study, Hepatology, doi:10.1002/hep.31446
Gabrielli, Franza, Esperide, Gasparrini, Gasbarrini et al., Liver Injury in Patients Hospitalized for COVID-19: Possible Role of Therapy, Vaccines, doi:10.3390/vaccines10020192
Gottlieb, Vaca, Paredes, Mera, Webb et al., GS-US-540-9012 (PINETREE) Investigators. Early Remdesivir to Prevent Progression to Severe Covid-19 in Outpatients, N. Engl. J. Med, doi:10.1056/NEJMoa2116846
Hamming, Timens, Bulthuis, Lely, Navis et al., Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis, J. Pathol, doi:10.1002/path.1570
Hermine, Mariette, Tharaux, Resche-Rigon, Porcher et al., Effect of Tocilizumab vs Usual Care in Adults Hospitalized with COVID-19 and Moderate or Severe Pneumonia: A Randomized Clinical Trial, JAMA Intern. Med, doi:10.1001/jamainternmed.2020.6820
Idalsoaga, Ayares, Arab, Díaz, COVID-19 and indirect liver injury: A narrative synthesis of the evidence, J. Clin. Transl. Hepatol, doi:10.14218/JCTH.2020.00140
Imam, Almalki, Alzahrani, Al-Ghamdi, Falemban et al., COVID-19 and severity of liver diseases: Possible crosstalk and clinical implications, Int. Immunopharmacol, doi:10.1016/j.intimp.2023.110439
Karlafti, Paramythiotis, Pantazi, Georgakopoulou, Kaiafa et al., Drug-Induced Liver Injury in Hospitalized Patients during SARS-CoV-2 Infection, Medicina, doi:10.3390/medicina58121848
Kotfis, Karolak, Lechowicz, Zegan-Bara Ńska, Pikulska et al., Mineralocorticoid Receptor Antagonist (Potassium Canrenoate) Does Not Influence Outcome in the Treatment of COVID-19-Associated Pneumonia and Fibrosis-A Randomized Placebo Controlled Clinical Trial, Pharmaceuticals, doi:10.3390/ph15020200
Kulkarni, Kumar, Tevethia, Premkumar, Arab et al., Systematic review with meta-analysis: Liver manifestations and outcomes in COVID-19, Aliment. Pharmacol. Ther, doi:10.1111/apt.15916
Laffont-Lozes, Laureillard, Loubet, Stephan, Chiaruzzi et al., Effect of Tocilizumab on Mortality in Patients with SARS-CoV-2 Pneumonia Caused by Delta or Omicron Variants: A Propensity-Matched Analysis in Nimes University Hospital, France, Antibiotics, doi:10.3390/antibiotics12010088
Lamers, Haagmans, SARS-CoV-2 pathogenesis, Nat. Rev. Microbiol, doi:10.1038/s41579-022-00713-0
Legislativ, Protocol of Treatment of SARS-CoV-2 Infection
Lei, Liu, Zhou, Qin, Zhang et al., Longitudinal Association Between Markers of Liver Injury and Mortality in COVID-19 in China, Hepatology, doi:10.1002/hep.31301
Liakina, Stundiene, Milaknyte, Bytautiene, Reivytyte et al., Effects of COVID-19 on the liver: The experience of a single center, World J. Gastroenterol, doi:10.3748/wjg.v28.i39.5735
Liatsos, SARS-CoV-2 induced liver injury: Incidence, risk factors, impact on COVID-19 severity and prognosis in different population groups, World J. Gastroenterol, doi:10.3748/wjg.v29.i16.2397
Loomba, Villarreal, Farias, Aggarwal, Aggarwal et al., Serum biomarkers for prediction of mortality in patients with COVID-19, Ann. Clin. Biochem, doi:10.1177/00045632211014244
Luxenburger, Thimme, SARS-CoV-2 and the liver: Clinical and immunological features in chronic liver disease, Gut, doi:10.1136/gutjnl-2023-329623
Malik, Patel, Mehta, Patel, Kelkar et al., Biomarkers and outcomes of COVID-19 hospitalisations: Systematic review and meta-analysis, BMJ Evid.-Based Med, doi:10.1136/bmjebm-2020-111536
Marjot, Webb, Barritt, Moon, Stamataki et al., COVID-19 and liver disease: Mechanistic and clinical perspectives, Nat. Rev. Gastroenterol. Hepatol, doi:10.1038/s41575-021-00426-4
Martínez-Sanz, Muriel, Ron, Herrera, Perez-Molina et al., Effects of tocilizumab on mortality in hospitalized patients with COVID-19: A multicentre cohort study, Clin. Microbiol. Infect, doi:10.1016/j.cmi.2020.09.021
Mihai, Tiliscan, Visan, Stratan, Ganea et al., Evaluation of Drug-Induced Liver Injury in Hospitalized Patients with SARS-CoV-2 Infection, Microorganisms, doi:10.3390/microorganisms10102045
Moga, Foncea, Bende, Popescu, Burdan et al., Impact of COVID-19 on Patients with Decompensated Liver Cirrhosis, Diagnostics, doi:10.3390/diagnostics13040600
Moreno Diaz, Amor García, Teigell Muñoz, Saldana Perez, Gonzalez et al., Does timing matter on tocilizumab administration? Clinical, analytical and radiological outcomes in COVID-19, Eur. J. Hosp. Pharm, doi:10.1136/ejhpharm-2020-002669
Nab, Parker, Andrews, Hulme, Fisher et al., Changes in COVID-19-related mortality across key demographic and clinical subgroups in England from 2020 to 2022: A retrospective cohort study using the OpenSAFELY platform, Lancet Public Health, doi:10.1016/S2468-2667(23)00079-8
Pan, Peto, Henao-Restrepo, Preziosi, Sathiyamoorthy et al., Repurposed antiviral drugs for COVID-19-Interim WHO Solidarity Trial Results, N. Engl. J. Med, doi:10.1056/NEJMoa2023184
Papagiouvanni, Kotoulas, Pataka, Spyratos, Porpodis et al., COVID-19 and liver injury: An ongoing challenge, World J. Gastroenterol, doi:10.3748/wjg.v29.i2.257
Paranga, Pavel-Tanasa, Constantinescu, Plesca, Petrovici et al., Comparison of C-reactive protein with distinct hyperinflammatory biomarkers in association with COVID-19 severity, mortality and SARS-CoV-2 variants, Front. Immunol, doi:10.3389/fimmu.2023.1213246
Phipps, Barraza, Lasota, Sobieszczyk, Pereira et al., Acute Liver Injury in COVID-19: Prevalence and Association with Clinical Outcomes in a Large U.S. Cohort, Hepatology, doi:10.1002/hep.31404
Ponziani, Del Zompo, Nesci, Santopaolo, Ianiro et al., Gemelli against COVID-19" group. Liver involvement is not associated with mortality: Results from a large cohort of SARS-CoV-2-positive patients, Aliment. Pharmacol. Ther, doi:10.1111/apt.15996
Radulescu, Istrate, Muntean, Treatment with Tocilizumab in Adult Patients with Moderate to Critical COVID-19 Pneumonia: A Single-Center Retrospective Study, Int. J. Infect. Dis, doi:10.1016/j.ijid.2022.01.048
Radulescu, Lupse, Istrate, Calin, Topan et al., Validation of Mortality Scores among High-Risk COVID-19 Patients: A Romanian Retrospective Study in the First Pandemic Year, J. Clin. Med, doi:10.3390/jcm11195630
Roca-Fernández, Dennis, Nicholls, Mcgonigle, Kelly et al., Hepatic Steatosis, Rather Than Underlying Obesity, Increases the Risk of Infection and Hospitalization for COVID-19, Front. Med, doi:10.3389/fmed.2021.636637
Salton, Confalonieri, Campisciano, Cifaldi, Rizzardi et al., Cytokine Profiles as Potential Prognostic and Therapeutic Markers in SARS-CoV-2-Induced ARDS, J. Clin. Med, doi:10.3390/jcm11112951
Shah, Orton, Grinsztejn, Donaldson, Ramírez et al., Favipiravir in patients hospitalised with COVID-19 (PIONEERtrial): A multicentre, open-label, phase 3, randomised controlled trial of early intervention versus standard care, Lancet Respir. Med, doi:10.1016/S2213-2600(22)00412-X
Shehab, Alrashed, Shuaibi, Alajmi, Barkun, Gastroenterological and hepatic manifestations of patients with COVID-19, prevalence, mortality by country, and intensive care admission rate: Systematic review and meta-analysis, BMJ Open Gastroenterol, doi:10.1136/bmjgast-2020-000571
Sun, Aghemo, Forner, Valenti, COVID-19 and liver disease, Liver Int, doi:10.1111/liv.14470
Tleyjeh, Kashour, Damlaj, Riaz, Tlayjeh et al., Efficacy and safety of tocilizumab in COVID-19 patients: A living systematic review and meta-analysis, Clin. Microbiol. Infect, doi:10.1016/j.cmi.2020.10.036
Turtle, Thorpe, Drake, Swets, Palmieri et al., Outcome of COVID-19 in hospitalised immunocompromised patients: An analysis of the WHO ISARIC CCP-UK prospective cohort study, PLoS Med, doi:10.1371/journal.pmed.1004086
Tuteja, Yu, Wilson, Chen, Wendt et al., Pharmacogenetic variants and risk of remdesivir-associated liver enzyme elevations in Million Veteran Program participants hospitalized with COVID-19, Clin. Transl. Sci, doi:10.1111/cts.13313
Vadiraj, Thareja, Raman, Karantha, Jayaraman et al., Does Raised Transaminases Predict Severity and Mortality in Patients with COVID-19?, J. Clin. Exp. Hepatol, doi:10.1016/j.jceh.2022.01.004
Veklury, Package Insert
Vijayaraghavan, Bishnu, Baruch, Citarella, Kartsonaki et al., Liver injury in hospitalized patients with COVID-19: An International observational cohort study, PLoS ONE
Vitiello, La Porta, D'aiuto, Ferrara, The risks of liver injury in COVID-19 patients and pharmacological management to reduce or prevent the damage induced. Egypt, Liver J, doi:10.1186/s43066-021-00082-y
Wang, Lei, Li, Yan, Potential effects of coronaviruses on the liver: An update, Front. Med, doi:10.3389/fmed.2021.651658
Wanner, Andrieux, Badia-I-Mompel, Edler, Pfefferle et al., Molecular consequences of SARS-CoV-2 liver tropism, Nat. Metab, doi:10.1038/s42255-022-00552-6
Weber, Hellmuth, Scherer, Muenchhoff, Mayerle et al., Liver function test abnormalities at hospital admission are associated with severe course of SARS-CoV-2 infection: A prospective cohort study, Gut, doi:10.1136/gutjnl-2020-323800
Who, Clinical Management of COVID-19, Living Guideline
Who, Working Group on the Clinical Characterisation and Management of COVID-19 infection, a minimal common outcome measure set for COVID-19 clinical research, Lancet Infect. Dis, doi:10.1016/S1473-3099(20)30483-7
Wijarnpreecha, Ungprasert, Panjawatanan, Harnois, Zaver et al., COVID-19 and liver injury: A meta-analysis, Eur. J. Gastroenterol. Hepatol, doi:10.1097/MEG.0000000000001817
Xu, Huang, Fei, Li, Chen, Dynamic Changes in Liver Function Tests and Their Correlation with Illness Severity and Mortality in Patients with COVID-19: A Retrospective Cohort Study, Clin. Interv. Aging, doi:10.2147/CIA.S303629
Yanez, Weiss, Romand, Treggiari, COVID-19 mortality risk for older men and women, BMC Public Health, doi:10.1186/s12889-020-09826-8
Zghal, Bouhamed, Mellouli, Triki, Kallel et al., Liver injury in COVID-19: Pathological findings, Pan Afr. Med. J, doi:10.11604/pamj.2022.41.56.31114
Zhang, Shi, Wang, Liver injury in COVID-19: Management and challenges, Lancet Gastroenterol. Hepatol, doi:10.1016/S2468-1253(20)30057-1
Zhao, Li, Li, Su, Liver injury in COVID-19: Clinical features, potential mechanisms, risk factors and clinical treatments, World J. Gastroenterol, doi:10.3748/wjg.v29.i2.241
DOI record:
{
"DOI": "10.3390/ph17010003",
"ISSN": [
"1424-8247"
],
"URL": "http://dx.doi.org/10.3390/ph17010003",
"abstract": "<jats:p>The aim of this study was to ascertain patient characteristics, outcomes, and liver injuries in patients infected with different SARS-CoV-2 variants. Data from consecutive adult patients with severe/critical COVID-19 admitted to our hospital during the peak month of the Delta wave were compared to the ancestral, Alpha, and Omicron waves. The dataset of 551 hospitalized patients was similar in the Delta/non-Delta waves. At admission and discharge, the median aminotransferase levels were normal or slightly increased. During the Delta wave (172 vs. 379 non-Delta patients), more patients died (OR 1.69, 95%CI 1.09–2.56) or had liver injury at discharge (alanine aminotransferase, ALT ≥ 2 ULN) (OR 1.97, 95%CI 1.08–3.54). In-hospital mortality was associated with age, lung injury, intensive care unit admission, number of and cardiovascular comorbidities, diabetes, chronic kidney disease, and all inflammatory biomarkers. Serious liver injury at admission (ALT ≥ 5 × ULN) was significantly associated with in-hospital mortality (OR = 7.9, 95%CI 2–28.9). At discharge, drug-induced liver injury (DILI) was found in patients treated with remdesivir, ALT ≥ 2 ULN (OR = 2.62, 95%CI 1.22–5.75). Treatment with dexamethasone, remdesivir, and immunomodulators showed improved survival, OR = 0.50 (95%CI 0.33–0.77). Regardless of the variant and treatment options, less than 2% of patients displayed serious liver injury, which was not found to be a death predictor in multivariable analysis.</jats:p>",
"alternative-id": [
"ph17010003"
],
"author": [
{
"affiliation": [
{
"name": "Department of Infectious Diseases and Epidemiology, The “Iuliu Hatieganu” University of Medicine and Pharmacy, 400348 Cluj-Napoca, Romania"
},
{
"name": "The Teaching Hospital of Infectious Diseases, 400348 Cluj-Napoca, Romania"
}
],
"family": "Muntean",
"given": "Monica",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Department of Infectious Diseases and Epidemiology, The “Iuliu Hatieganu” University of Medicine and Pharmacy, 400348 Cluj-Napoca, Romania"
},
{
"name": "The Teaching Hospital of Infectious Diseases, 400348 Cluj-Napoca, Romania"
}
],
"family": "Briciu",
"given": "Violeta",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4010-2901",
"affiliation": [
{
"name": "Department of Infectious Diseases and Epidemiology, The “Iuliu Hatieganu” University of Medicine and Pharmacy, 400348 Cluj-Napoca, Romania"
},
{
"name": "The Teaching Hospital of Infectious Diseases, 400348 Cluj-Napoca, Romania"
}
],
"authenticated-orcid": false,
"family": "Lupse",
"given": "Mihaela",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6067-5307",
"affiliation": [
{
"name": "The Teaching Hospital of Infectious Diseases, 400348 Cluj-Napoca, Romania"
}
],
"authenticated-orcid": false,
"family": "Colcear",
"given": "Doina",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0009-0002-9730-3333",
"affiliation": [
{
"name": "Department of Infectious Diseases and Epidemiology, The “Iuliu Hatieganu” University of Medicine and Pharmacy, 400348 Cluj-Napoca, Romania"
}
],
"authenticated-orcid": false,
"family": "Macicasan",
"given": "Raul Vlad",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Infectious Diseases and Epidemiology, The “Iuliu Hatieganu” University of Medicine and Pharmacy, 400348 Cluj-Napoca, Romania"
}
],
"family": "Csiszer",
"given": "Agnes",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Infectious Diseases and Epidemiology, The “Iuliu Hatieganu” University of Medicine and Pharmacy, 400348 Cluj-Napoca, Romania"
}
],
"family": "Manole",
"given": "Alexandra",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4154-0498",
"affiliation": [
{
"name": "Department of Infectious Diseases and Epidemiology, The “Iuliu Hatieganu” University of Medicine and Pharmacy, 400348 Cluj-Napoca, Romania"
},
{
"name": "The Teaching Hospital of Infectious Diseases, 400348 Cluj-Napoca, Romania"
}
],
"authenticated-orcid": false,
"family": "Radulescu",
"given": "Amanda",
"sequence": "additional"
}
],
"container-title": "Pharmaceuticals",
"container-title-short": "Pharmaceuticals",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
12,
19
]
],
"date-time": "2023-12-19T16:17:24Z",
"timestamp": 1703002644000
},
"deposited": {
"date-parts": [
[
2023,
12,
20
]
],
"date-time": "2023-12-20T09:22:54Z",
"timestamp": 1703064174000
},
"funder": [
{
"award": [
"PDI-PFE-CDI 2021",
"0PFE/30.12.2021"
],
"name": "Increasing the Performance of Scientific Research, Supporting Excellence in Medical Research and Innovation"
}
],
"indexed": {
"date-parts": [
[
2023,
12,
21
]
],
"date-time": "2023-12-21T00:25:58Z",
"timestamp": 1703118358241
},
"is-referenced-by-count": 0,
"issue": "1",
"issued": {
"date-parts": [
[
2023,
12,
19
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2024,
1
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
12,
19
]
],
"date-time": "2023-12-19T00:00:00Z",
"timestamp": 1702944000000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/1424-8247/17/1/3/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "3",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2023,
12,
19
]
]
},
"published-online": {
"date-parts": [
[
2023,
12,
19
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"article-title": "COVID-19 and indirect liver injury: A narrative synthesis of the evidence",
"author": "Idalsoaga",
"first-page": "760",
"journal-title": "J. Clin. Transl. Hepatol.",
"key": "ref_1",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1186/s43066-021-00082-y",
"article-title": "The risks of liver injury in COVID-19 patients and pharmacological management to reduce or prevent the damage induced",
"author": "Vitiello",
"doi-asserted-by": "crossref",
"first-page": "11",
"journal-title": "Egypt. Liver J.",
"key": "ref_2",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1002/path.1570",
"article-title": "Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis",
"author": "Hamming",
"doi-asserted-by": "crossref",
"first-page": "631",
"journal-title": "J. Pathol.",
"key": "ref_3",
"volume": "203",
"year": "2004"
},
{
"DOI": "10.3390/microorganisms10102045",
"doi-asserted-by": "crossref",
"key": "ref_4",
"unstructured": "Mihai, N., Tiliscan, C., Visan, C.A., Stratan, L., Ganea, O., Arama, S.S., Lazar, M., and Arama, V. (2022). Evaluation of Drug-Induced Liver Injury in Hospitalized Patients with SARS-CoV-2 Infection. Microorganisms, 10."
},
{
"DOI": "10.11604/pamj.2022.41.56.31114",
"article-title": "Liver injury in COVID-19: Pathological findings",
"author": "Zghal",
"doi-asserted-by": "crossref",
"first-page": "56",
"journal-title": "Pan Afr. Med. J.",
"key": "ref_5",
"volume": "41",
"year": "2022"
},
{
"DOI": "10.2147/CIA.S303629",
"article-title": "Dynamic Changes in Liver Function Tests and Their Correlation with Illness Severity and Mortality in Patients with COVID-19: A Retrospective Cohort Study",
"author": "Xu",
"doi-asserted-by": "crossref",
"first-page": "675",
"journal-title": "Clin. Interv. Aging",
"key": "ref_6",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.3389/fmed.2021.651658",
"article-title": "Potential effects of coronaviruses on the liver: An update",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "651658",
"journal-title": "Front. Med.",
"key": "ref_7",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1097/MEG.0000000000002381",
"article-title": "Clinical features and predictive factors related to liver injury in SARS-CoV-2 Delta and Omicron variant-infected patients",
"author": "Deng",
"doi-asserted-by": "crossref",
"first-page": "933",
"journal-title": "Eur. J. Gastroenterol. Hepatol.",
"key": "ref_8",
"volume": "34",
"year": "2022"
},
{
"DOI": "10.1111/liv.14470",
"article-title": "COVID-19 and liver disease",
"author": "Sun",
"doi-asserted-by": "crossref",
"first-page": "1278",
"journal-title": "Liver Int.",
"key": "ref_9",
"volume": "40",
"year": "2020"
},
{
"DOI": "10.1016/S2468-1253(20)30057-1",
"article-title": "Liver injury in COVID-19: Management and challenges",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "428",
"journal-title": "Lancet Gastroenterol. Hepatol.",
"key": "ref_10",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.3748/wjg.v29.i16.2397",
"article-title": "SARS-CoV-2 induced liver injury: Incidence, risk factors, impact on COVID-19 severity and prognosis in different population groups",
"author": "Liatsos",
"doi-asserted-by": "crossref",
"first-page": "2397",
"journal-title": "World J. Gastroenterol.",
"key": "ref_11",
"volume": "29",
"year": "2023"
},
{
"DOI": "10.1111/jvh.13590",
"article-title": "COVID-19 and the liver: Lessons learnt from the EAST and the WEST, a year later",
"author": "Ekpanyapong",
"doi-asserted-by": "crossref",
"first-page": "4",
"journal-title": "J. Viral Hepat.",
"key": "ref_12",
"volume": "29",
"year": "2022"
},
{
"DOI": "10.3390/jcm11112951",
"doi-asserted-by": "crossref",
"key": "ref_13",
"unstructured": "Salton, F., Confalonieri, P., Campisciano, G., Cifaldi, R., Rizzardi, C., Generali, D., Pozzan, R., Tavano, S., Bozzi, C., and Lapadula, G. (2022). Cytokine Profiles as Potential Prognostic and Therapeutic Markers in SARS-CoV-2-Induced ARDS. J. Clin. Med., 11."
},
{
"DOI": "10.3390/ph15030365",
"doi-asserted-by": "crossref",
"key": "ref_14",
"unstructured": "Amri, N., Bégin, R., Tessier, N., Vachon, L., Villeneuve, L., Bégin, P., Bazin, R., Loubaki, L., and Martel, C. (2022). Use of Early Donated COVID-19 Convalescent Plasma Is Optimal to Preserve the Integrity of Lymphatic Endothelial Cells. Pharmaceuticals, 15."
},
{
"DOI": "10.3390/ph15020200",
"doi-asserted-by": "crossref",
"key": "ref_15",
"unstructured": "Kotfis, K., Karolak, I., Lechowicz, K., Zegan-Barańska, M., Pikulska, A., Niedźwiedzka-Rystwej, P., Kawa, M., Sieńko, J., Szylińska, A., and Wiśniewska, M. (2022). Mineralocorticoid Receptor Antagonist (Potassium Canrenoate) Does Not Influence Outcome in the Treatment of COVID-19-Associated Pneumonia and Fibrosis-A Randomized Placebo Controlled Clinical Trial. Pharmaceuticals, 15."
},
{
"DOI": "10.1016/j.cgh.2021.05.022",
"article-title": "Significant Liver Injury During Hospitalization for COVID-19 Is Not Associated with Liver Insufficiency or Death",
"author": "Chew",
"doi-asserted-by": "crossref",
"first-page": "2182",
"journal-title": "Clin. Gastroenterol. Hepatol.",
"key": "ref_16",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.1038/s41575-021-00426-4",
"article-title": "COVID-19 and liver disease: Mechanistic and clinical perspectives",
"author": "Marjot",
"doi-asserted-by": "crossref",
"first-page": "348",
"journal-title": "Nat. Rev. Gastroenterol. Hepatol.",
"key": "ref_17",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.5009/gnl220327",
"article-title": "SARS-CoV-2 Infection and Liver Disease: A Review of Pathogenesis and Outcomes",
"author": "Baldelli",
"doi-asserted-by": "crossref",
"first-page": "12",
"journal-title": "Gut Liver",
"key": "ref_18",
"volume": "17",
"year": "2023"
},
{
"DOI": "10.1038/s42255-022-00552-6",
"article-title": "Molecular consequences of SARS-CoV-2 liver tropism",
"author": "Wanner",
"doi-asserted-by": "crossref",
"first-page": "310",
"journal-title": "Nat. Metab.",
"key": "ref_19",
"volume": "4",
"year": "2022"
},
{
"DOI": "10.1136/gutjnl-2023-329623",
"article-title": "SARS-CoV-2 and the liver: Clinical and immunological features in chronic liver disease",
"author": "Luxenburger",
"doi-asserted-by": "crossref",
"first-page": "1783",
"journal-title": "Gut",
"key": "ref_20",
"volume": "72",
"year": "2023"
},
{
"DOI": "10.1016/j.immuni.2021.05.010",
"article-title": "Longitudinal analysis reveals that delayed bystander CD8+ T cell activation and early immune pathology distinguish severe COVID-19 from mild disease",
"author": "Bergamaschi",
"doi-asserted-by": "crossref",
"first-page": "1257",
"journal-title": "Immunity",
"key": "ref_21",
"volume": "54",
"year": "2021"
},
{
"DOI": "10.3390/antibiotics12010088",
"doi-asserted-by": "crossref",
"key": "ref_22",
"unstructured": "Laffont-Lozes, P., Laureillard, D., Loubet, P., Stephan, R., Chiaruzzi, M., Clemmer, E., Martin, A., Roger, C., Muller, L., and Claret, P.G. (2023). Effect of Tocilizumab on Mortality in Patients with SARS-CoV-2 Pneumonia Caused by Delta or Omicron Variants: A Propensity-Matched Analysis in Nimes University Hospital, France. Antibiotics, 12."
},
{
"DOI": "10.1016/j.jhep.2020.04.006",
"article-title": "COVID-19: Abnormal liver function tests",
"author": "Cai",
"doi-asserted-by": "crossref",
"first-page": "566",
"journal-title": "J. Hepatol.",
"key": "ref_23",
"volume": "73",
"year": "2020"
},
{
"DOI": "10.1136/gutjnl-2020-323800",
"article-title": "Liver function test abnormalities at hospital admission are associated with severe course of SARS-CoV-2 infection: A prospective cohort study",
"author": "Weber",
"doi-asserted-by": "crossref",
"first-page": "1925",
"journal-title": "Gut",
"key": "ref_24",
"volume": "70",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0277859",
"doi-asserted-by": "crossref",
"key": "ref_25",
"unstructured": "Vijayaraghavan, B.K.T., Bishnu, S., Baruch, J., Citarella, B.W., Kartsonaki, C., Meeyai, A., Zubair, M., Ohshimo, S., Al-Fares, A., and Calvache, J.A. (2023). ISARIC Clinical Characterisation Group. Liver injury in hospitalized patients with COVID-19: An International observational cohort study. PLoS ONE, 18."
},
{
"DOI": "10.1111/apt.15996",
"article-title": "Liver involvement is not associated with mortality: Results from a large cohort of SARS-CoV-2-positive patients",
"author": "Ponziani",
"doi-asserted-by": "crossref",
"first-page": "1060",
"journal-title": "Aliment. Pharmacol. Ther.",
"key": "ref_26",
"volume": "52",
"year": "2020"
},
{
"DOI": "10.1002/hep.31446",
"article-title": "Clinical features of patients infected with coronavirus disease 2019 with elevated liver biochemistries: A multicenter, retrospective study",
"author": "Fu",
"doi-asserted-by": "crossref",
"first-page": "1509",
"journal-title": "Hepatology",
"key": "ref_27",
"volume": "73",
"year": "2021"
},
{
"DOI": "10.1097/MEG.0000000000001817",
"article-title": "COVID-19 and liver injury: A meta-analysis",
"author": "Wijarnpreecha",
"doi-asserted-by": "crossref",
"first-page": "990",
"journal-title": "Eur. J. Gastroenterol. Hepatol.",
"key": "ref_28",
"volume": "33",
"year": "2021"
},
{
"DOI": "10.1016/j.intimp.2023.110439",
"article-title": "COVID-19 and severity of liver diseases: Possible crosstalk and clinical implications",
"author": "Imam",
"doi-asserted-by": "crossref",
"first-page": "110439",
"journal-title": "Int. Immunopharmacol.",
"key": "ref_29",
"volume": "121",
"year": "2023"
},
{
"DOI": "10.1111/apt.15916",
"article-title": "Systematic review with meta-analysis: Liver manifestations and outcomes in COVID-19",
"author": "Kulkarni",
"doi-asserted-by": "crossref",
"first-page": "584",
"journal-title": "Aliment. Pharmacol. Ther.",
"key": "ref_30",
"volume": "52",
"year": "2020"
},
{
"DOI": "10.3390/healthcare11030373",
"doi-asserted-by": "crossref",
"key": "ref_31",
"unstructured": "Briciu, V., Topan, A., Calin, M., Dobrota, R., Leucuta, D.C., and Lupse, M. (2023). Comparison of COVID-19 Severity in Vaccinated and Unvaccinated Patients during the Delta and Omicron Wave of the Pandemic in a Romanian Tertiary Infectious Diseases Hospital. Healthcare, 11."
},
{
"article-title": "Hepatic Steatosis, Rather Than Underlying Obesity, Increases the Risk of Infection and Hospitalization for COVID-19",
"author": "Dennis",
"first-page": "636637",
"journal-title": "Front. Med.",
"key": "ref_32",
"volume": "29",
"year": "2021"
},
{
"DOI": "10.1016/j.cgh.2023.05.013",
"article-title": "Risk of Severe Infection in Patients With Biopsy-proven Nonalcoholic Fatty Liver Disease—A Population-based Cohort Study",
"author": "Ebrahimi",
"doi-asserted-by": "crossref",
"first-page": "3346",
"journal-title": "Clin. Gastroenterol. Hepatol.",
"key": "ref_33",
"volume": "21",
"year": "2023"
},
{
"DOI": "10.1038/s41579-022-00713-0",
"article-title": "SARS-CoV-2 pathogenesis",
"author": "Lamers",
"doi-asserted-by": "crossref",
"first-page": "270",
"journal-title": "Nat. Rev. Microbiol.",
"key": "ref_34",
"volume": "20",
"year": "2022"
},
{
"DOI": "10.1136/gutjnl-2021-326792",
"article-title": "COVID-19 and liver disease",
"author": "Dufour",
"doi-asserted-by": "crossref",
"first-page": "2350",
"journal-title": "Gut",
"key": "ref_35",
"volume": "71",
"year": "2022"
},
{
"DOI": "10.3390/diagnostics13040600",
"doi-asserted-by": "crossref",
"key": "ref_36",
"unstructured": "Moga, T.V., Foncea, C., Bende, R., Popescu, A., Burdan, A., Heredea, D., Danilă, M., Miutescu, B., Ratiu, I., and Bizerea-Moga, T.O. (2023). Impact of COVID-19 on Patients with Decompensated Liver Cirrhosis. Diagnostics, 13."
},
{
"DOI": "10.3748/wjg.v29.i2.241",
"article-title": "Liver injury in COVID-19: Clinical features, potential mechanisms, risk factors and clinical treatments",
"author": "Zhao",
"doi-asserted-by": "crossref",
"first-page": "241",
"journal-title": "World J. Gastroenterol.",
"key": "ref_37",
"volume": "29",
"year": "2023"
},
{
"DOI": "10.1016/j.lanepe.2021.100109",
"article-title": "Factors associated with deaths due to COVID-19 versus other causes: Population-based cohort analysis of UK primary care data and linked national death registrations within the OpenSAFELY platform",
"author": "Bhaskaran",
"doi-asserted-by": "crossref",
"first-page": "100109",
"journal-title": "Lancet Reg. Health Eur.",
"key": "ref_38",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.1001/jamanetworkopen.2021.16901",
"article-title": "National COVID Cohort Collaborative (N3C) Consortium. Clinical Characterization and Prediction of Clinical Severity of SARS-CoV-2 Infection among US Adults Using Data From the US National COVID Cohort Collaborative",
"author": "Bennett",
"doi-asserted-by": "crossref",
"first-page": "e2116901",
"journal-title": "JAMA Netw. Open",
"key": "ref_39",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.3390/jcm11195630",
"doi-asserted-by": "crossref",
"key": "ref_40",
"unstructured": "Radulescu, A., Lupse, M., Istrate, A., Calin, M., Topan, A., Kormos, N.F., Macicasan, R.V., and Briciu, V. (2022). Validation of Mortality Scores among High-Risk COVID-19 Patients: A Romanian Retrospective Study in the First Pandemic Year. J. Clin. Med., 11."
},
{
"DOI": "10.1016/S2468-2667(23)00079-8",
"article-title": "Changes in COVID-19-related mortality across key demographic and clinical subgroups in England from 2020 to 2022: A retrospective cohort study using the OpenSAFELY platform",
"author": "Nab",
"doi-asserted-by": "crossref",
"first-page": "e364",
"journal-title": "Lancet Public Health",
"key": "ref_41",
"volume": "8",
"year": "2023"
},
{
"DOI": "10.1056/NEJMoa2116846",
"article-title": "GS-US-540-9012 (PINETREE) Investigators. Early Remdesivir to Prevent Progression to Severe Covid-19 in Outpatients",
"author": "Gottlieb",
"doi-asserted-by": "crossref",
"first-page": "305",
"journal-title": "N. Engl. J. Med.",
"key": "ref_42",
"volume": "386",
"year": "2022"
},
{
"DOI": "10.1371/journal.pmed.1004086",
"doi-asserted-by": "crossref",
"key": "ref_43",
"unstructured": "Turtle, L., Thorpe, M., Drake, T., Swets, M., Palmieri, C., Russell, C., Ho, A., Aston, S., Wootton, D.G., and Richter, A. (2023). Outcome of COVID-19 in hospitalised immunocompromised patients: An analysis of the WHO ISARIC CCP-UK prospective cohort study. PLoS Med., 20."
},
{
"key": "ref_44",
"unstructured": "Institutul National de Sanatate Publica (INSP) (The Romanian Nationale Institute of Public Health) (2023, May 05). Informare Privind Cazurile de COVID-19 Confirmate cu Variante ale SARS-CoV-2 Care Determina Îngrijorare (VOC). Available online: https://www.cnscbt.ro/index.php/analiza-cazuri-confirmate-covid19/3437-s-13-2023-informare-cazuri-cu-variante-de-ingrijorare-voc-si-variante-de-interes-voi/file."
},
{
"DOI": "10.3748/wjg.v28.i39.5735",
"article-title": "Effects of COVID-19 on the liver: The experience of a single center",
"author": "Liakina",
"doi-asserted-by": "crossref",
"first-page": "5735",
"journal-title": "World J. Gastroenterol.",
"key": "ref_45",
"volume": "28",
"year": "2022"
},
{
"DOI": "10.1002/hep.31301",
"article-title": "Longitudinal Association Between Markers of Liver Injury and Mortality in COVID-19 in China",
"author": "Lei",
"doi-asserted-by": "crossref",
"first-page": "389",
"journal-title": "Hepatology",
"key": "ref_46",
"volume": "72",
"year": "2020"
},
{
"DOI": "10.1016/j.jceh.2022.01.004",
"article-title": "Does Raised Transaminases Predict Severity and Mortality in Patients with COVID-19?",
"author": "Vadiraj",
"doi-asserted-by": "crossref",
"first-page": "1114",
"journal-title": "J. Clin. Exp. Hepatol.",
"key": "ref_47",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1186/s12889-020-09826-8",
"doi-asserted-by": "crossref",
"key": "ref_48",
"unstructured": "Yanez, N.D., Weiss, N.S., Romand, J.A., and Treggiari, M.M. (2020). COVID-19 mortality risk for older men and women. BMC Public Health, 20."
},
{
"DOI": "10.1136/bmjgast-2020-000571",
"article-title": "Gastroenterological and hepatic manifestations of patients with COVID-19, prevalence, mortality by country, and intensive care admission rate: Systematic review and meta-analysis",
"author": "Shehab",
"doi-asserted-by": "crossref",
"first-page": "e000571",
"journal-title": "BMJ Open Gastroenterol.",
"key": "ref_49",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.3390/pathogens12121453",
"doi-asserted-by": "crossref",
"key": "ref_50",
"unstructured": "Briciu, V., Leucuta, D.-C., Muntean, M., Radulescu, A., Cismaru, C., Topan, A., Herbel, L., Horvat, M., Calin, M., and Dobrota, R. (2023). Evolving Clinical Manifestations and Outcomes in COVID-19 Patients: A Comparative Analysis of SARS-CoV-2 Variant Waves in a Romanian Hospital Setting. Pathogens, 12."
},
{
"DOI": "10.1136/bmjebm-2020-111536",
"article-title": "Biomarkers and outcomes of COVID-19 hospitalisations: Systematic review and meta-analysis",
"author": "Malik",
"doi-asserted-by": "crossref",
"first-page": "107",
"journal-title": "BMJ Evid.-Based Med.",
"key": "ref_51",
"volume": "26",
"year": "2021"
},
{
"DOI": "10.3389/fimmu.2023.1213246",
"article-title": "Comparison of C-reactive protein with distinct hyperinflammatory biomarkers in association with COVID-19 severity, mortality and SARS-CoV-2 variants",
"author": "Paranga",
"doi-asserted-by": "crossref",
"first-page": "1213246",
"journal-title": "Front. Immunol.",
"key": "ref_52",
"volume": "14",
"year": "2023"
},
{
"DOI": "10.1177/00045632211014244",
"article-title": "Serum biomarkers for prediction of mortality in patients with COVID-19",
"author": "Loomba",
"doi-asserted-by": "crossref",
"first-page": "15",
"journal-title": "Ann. Clin. Biochem.",
"key": "ref_53",
"volume": "59",
"year": "2022"
},
{
"DOI": "10.1016/j.cmi.2020.09.021",
"article-title": "Effects of tocilizumab on mortality in hospitalized patients with COVID-19: A multicentre cohort study",
"author": "Muriel",
"doi-asserted-by": "crossref",
"first-page": "238",
"journal-title": "Clin. Microbiol. Infect.",
"key": "ref_54",
"volume": "27",
"year": "2021"
},
{
"article-title": "Does timing matter on tocilizumab administration? Clinical, analytical and radiological outcomes in COVID-19",
"first-page": "340",
"journal-title": "Eur. J. Hosp. Pharm.",
"key": "ref_55",
"volume": "29",
"year": "2021"
},
{
"article-title": "Biomarker variation in patients successfully treated with tocilizumab for severe coronavirus disease 2019 (COVID-19): Results of a multidisciplinary collaboration",
"author": "Conrozier",
"first-page": "742",
"journal-title": "Clin. Exp. Rheumatol.",
"key": "ref_56",
"volume": "38",
"year": "2019"
},
{
"DOI": "10.1016/j.ijid.2022.01.048",
"article-title": "Treatment with Tocilizumab in Adult Patients with Moderate to Critical COVID-19 Pneumonia: A Single-Center Retrospective Study",
"author": "Radulescu",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Int. J. Infect. Dis.",
"key": "ref_57",
"volume": "117",
"year": "2022"
},
{
"DOI": "10.1002/hep.31404",
"article-title": "Acute Liver Injury in COVID-19: Prevalence and Association with Clinical Outcomes in a Large U.S. Cohort",
"author": "Phipps",
"doi-asserted-by": "crossref",
"first-page": "807",
"journal-title": "Hepatology",
"key": "ref_58",
"volume": "72",
"year": "2020"
},
{
"DOI": "10.3748/wjg.v29.i2.257",
"article-title": "COVID-19 and liver injury: An ongoing challenge",
"author": "Papagiouvanni",
"doi-asserted-by": "crossref",
"first-page": "257",
"journal-title": "World J. Gastroenterol.",
"key": "ref_59",
"volume": "29",
"year": "2023"
},
{
"DOI": "10.3390/vaccines10020192",
"doi-asserted-by": "crossref",
"key": "ref_60",
"unstructured": "Gabrielli, M., Franza, L., Esperide, A., Gasparrini, I., Gasbarrini, A., and Franceschi, F. (2022). On Behalf of Gemelli Against Covid. Liver Injury in Patients Hospitalized for COVID-19: Possible Role of Therapy. Vaccines, 10."
},
{
"DOI": "10.3390/jcm11010153",
"doi-asserted-by": "crossref",
"key": "ref_61",
"unstructured": "Crisan, D., Avram, L., Grapa, C., Dragan, A., Radulescu, D., Crisan, S., Grosu, A., Militaru, V., Buzdugan, E., and Stoicescu, L. (2021). Liver Injury and Elevated FIB-4 Define a High-Risk Group in Patients with COVID-19. J. Clin. Med., 11."
},
{
"DOI": "10.1016/j.clinre.2020.10.002",
"article-title": "Liver function test abnormalities are associated with a poorer prognosis in COVID-19 patients: Results of a French cohort",
"author": "Chaibi",
"doi-asserted-by": "crossref",
"first-page": "101556",
"journal-title": "Clin. Res. Hepatol. Gastroenterol.",
"key": "ref_62",
"volume": "45",
"year": "2021"
},
{
"key": "ref_63",
"unstructured": "(2023, May 10). NIH Coronavirus Disease 2019 (COVID-19) Treatment Guidelines 2023, Available online: https://files.covid19treatmentguidelines.nih.gov/guidelines/covid19treatmentguidelines.pdf."
},
{
"DOI": "10.1101/2021.02.11.21249258",
"doi-asserted-by": "crossref",
"key": "ref_64",
"unstructured": "RECOVERY Collaborative Group (2021). Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): A randomised, controlled, open-label, platform trial. Lancet, 397, 1637–1645."
},
{
"key": "ref_65",
"unstructured": "Veklury (Remdesivir) (2023, January 28). Package Insert, Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/214787Orig1s000lbl.pdf."
},
{
"key": "ref_66",
"unstructured": "Bhimraj, A., Morgan, R.L., Shumaker, A.H., Baden, L., Cheng, V.C., Edwards, K.M., Gandhi, R., Muller, W.J., O’Horo, J.C., and Shoham, S. (2023, June 10). Infectious Diseases Society of America Guidelines on the Treatment and Management of Patients with COVID-19. Available online: https://www.idsociety.org/globalassets/idsa/practice-guidelines/covid-19/treatment/idsa-covid-19-gl-tx-and-mgmt-v11.0.0.pdf."
},
{
"DOI": "10.1111/cts.13313",
"article-title": "Pharmacogenetic variants and risk of remdesivir-associated liver enzyme elevations in Million Veteran Program participants hospitalized with COVID-19",
"author": "Tuteja",
"doi-asserted-by": "crossref",
"first-page": "1880",
"journal-title": "Clin. Transl. Sci.",
"key": "ref_67",
"volume": "15",
"year": "2022"
},
{
"key": "ref_68",
"unstructured": "WHO (2023, January 30). Clinical Management of COVID-19: Living Guideline. 13 January 2023. Available online: https://iris.who.int/bitstream/handle/10665/365580/WHO-2019-nCoV-clinical-2023.1-eng.pdf."
},
{
"DOI": "10.1001/jamainternmed.2020.6820",
"article-title": "CORIMUNO-19 Collaborative Group. Effect of Tocilizumab vs Usual Care in Adults Hospitalized with COVID-19 and Moderate or Severe Pneumonia: A Randomized Clinical Trial",
"author": "Hermine",
"doi-asserted-by": "crossref",
"first-page": "32",
"journal-title": "JAMA Intern. Med.",
"key": "ref_69",
"volume": "181",
"year": "2021"
},
{
"DOI": "10.1016/j.cmi.2020.10.036",
"article-title": "Efficacy and safety of tocilizumab in COVID-19 patients: A living systematic review and meta-analysis",
"author": "Tleyjeh",
"doi-asserted-by": "crossref",
"first-page": "215",
"journal-title": "Clin. Microbiol. Infect.",
"key": "ref_70",
"volume": "27",
"year": "2021"
},
{
"article-title": "Efficacy and Safety of Favipiravir in Treating COVID-19 Patients: A Meta-Analysis of Randomized Control Trials",
"author": "Batool",
"first-page": "e33676",
"journal-title": "Cureus",
"key": "ref_71",
"volume": "15",
"year": "2023"
},
{
"DOI": "10.1016/S2213-2600(22)00412-X",
"article-title": "Favipiravir in patients hospitalised with COVID-19 (PIONEERtrial): A multicentre, open-label, phase 3, randomised controlled trial of early intervention versus standard care",
"author": "Shah",
"doi-asserted-by": "crossref",
"first-page": "415",
"journal-title": "Lancet Respir. Med.",
"key": "ref_72",
"volume": "11",
"year": "2023"
},
{
"key": "ref_73",
"unstructured": "Portal Legislativ (2023, January 30). Protocol of Treatment of SARS-CoV-2 Infection. Available online: https://legislatie.just.ro/Public/DetaliiDocumentAfis/249520."
},
{
"key": "ref_74",
"unstructured": "WHO (2020). Working Group on the Clinical Characterisation and Management of COVID-19 infection, a minimal common outcome measure set for COVID-19 clinical research. Lancet Infect. Dis., 20, e192–e197."
},
{
"key": "ref_75",
"unstructured": "National Institutes of Health (2023, May 30). COVID-19 Treatment Guidelines Panel. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines, Available online: https://www.covid19treatmentguidelines.nih.gov/."
},
{
"DOI": "10.1056/NEJMoa2023184",
"doi-asserted-by": "crossref",
"key": "ref_76",
"unstructured": "WHO Solidarity Trial Consortium, Pan, H., Peto, R., Henao-Restrepo, A.M., Preziosi, M.P., Sathiyamoorthy, V., Abdool Karim, Q., Alejandria, M.M., Hernández García, C., and Kieny, M.P. (2021). Repurposed antiviral drugs for COVID-19—Interim WHO Solidarity Trial Results. N. Engl. J. Med., 384, 497–511."
},
{
"DOI": "10.3390/ijms17010014",
"doi-asserted-by": "crossref",
"key": "ref_77",
"unstructured": "Danan, G., and Teschke, R. (2015). RUCAM in Drug and Herb Induced Liver Injury: The Update. Int. J. Mol. Sci., 17."
},
{
"DOI": "10.3390/medicina58121848",
"doi-asserted-by": "crossref",
"key": "ref_78",
"unstructured": "Karlafti, E., Paramythiotis, D., Pantazi, K., Georgakopoulou, V.E., Kaiafa, G., Papalexis, P., Protopapas, A.A., Ztriva, E., Fyntanidou, V., and Savopoulos, C. (2022). Drug-Induced Liver Injury in Hospitalized Patients during SARS-CoV-2 Infection. Medicina, 58."
},
{
"DOI": "10.1080/23744235.2021.1910727",
"article-title": "Visual scoring of chest CT at hospital admission predicts hospitalization time and intensive care admission in COVID-19",
"author": "Ahlstrand",
"doi-asserted-by": "crossref",
"first-page": "622",
"journal-title": "Infect. Dis.",
"key": "ref_79",
"volume": "53",
"year": "2021"
},
{
"key": "ref_80",
"unstructured": "R Core Team (2020). R. A Language and Environment for Statistical Computing, R Foundation for Statistical Computing. Available online: https://www.R-project.org/."
}
],
"reference-count": 80,
"references-count": 80,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/1424-8247/17/1/3"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Drug Discovery",
"Pharmaceutical Science",
"Molecular Medicine"
],
"subtitle": [],
"title": "Effects of COVID-19 on the Liver and Mortality in Patients with SARS-CoV-2 Pneumonia Caused by Delta and Non-Delta Variants: An Analysis in a Single Centre",
"type": "journal-article",
"volume": "17"
}