Favipiravir: the hidden threat of mutagenic action
et al., Journal of microbiology, epidemiology and immunobiology, doi:10.36233/0372-9311-114, May 2021
Review of the mutagenic effect of favipiravir and associated concerns.
1.
Shen et al., Carboxylesterase Factors Influencing the Therapeutic Activity of Common Antiviral Medications Used for SARS-CoV-2 Infection, Pharmaceutics, doi:10.3390/pharmaceutics17070832.
2.
Saha et al., Inhaled Dry Powder of Antiviral Agents: A Promising Approach to Treating Respiratory Viral Pathogens, Viruses, doi:10.3390/v17020252.
3.
Lopez et al., SARS-CoV-2 Resistance to Small Molecule Inhibitors, Current Clinical Microbiology Reports, doi:10.1007/s40588-024-00229-6.
4.
Bacigalupo et al., Unveiling patenting strategies of therapeutics and vaccines: evergreening in the context of COVID-19 pandemic, Frontiers in Medicine, doi:10.3389/fmed.2023.1287542.
5.
Hadj Hassine et al., Lethal Mutagenesis of RNA Viruses and Approved Drugs with Antiviral Mutagenic Activity, Viruses, doi:10.3390/v14040841.
Zhirnov et al., 5 May 2021, Russia, peer-reviewed, 2 authors.
Favipiravir: the hidden threat of mutagenic action
Journal of microbiology, epidemiology and immunobiology, doi:10.36233/0372-9311-114
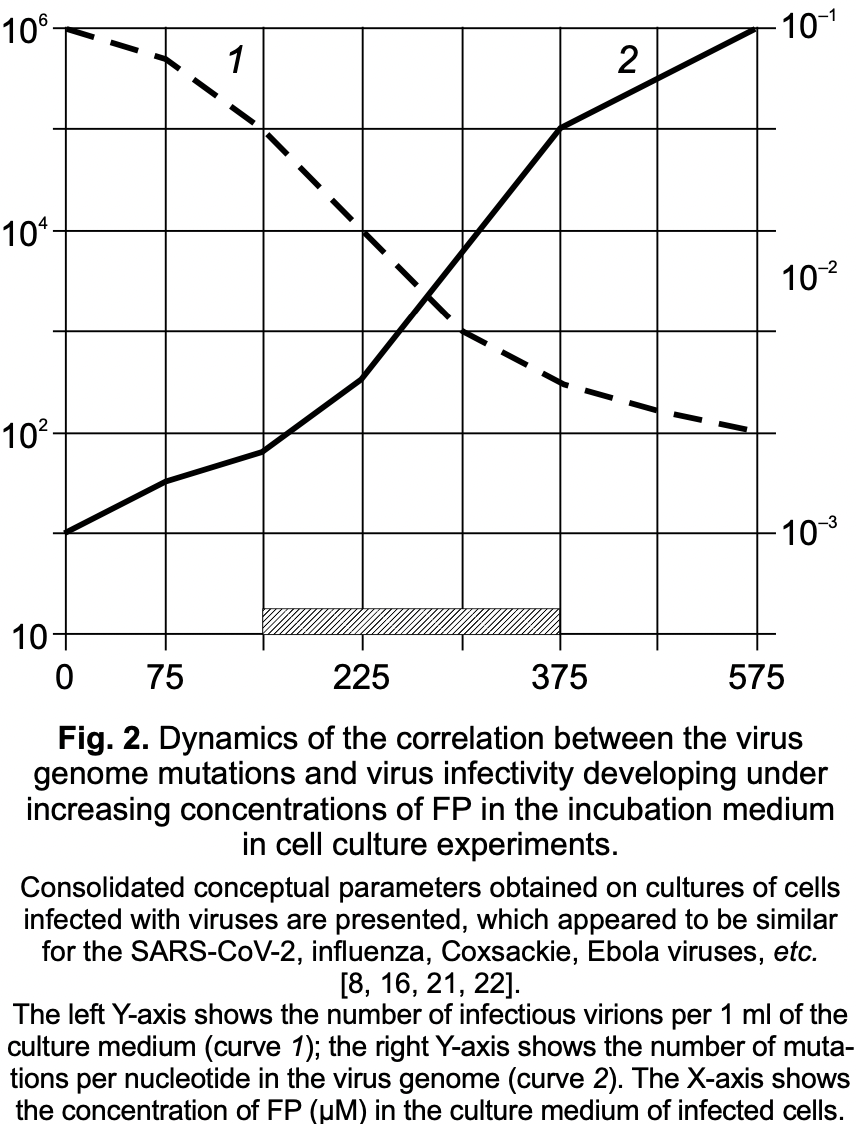
The antiviral drug favipiravir (FPV), which is a structural analogue of guanosine, undergoes chemical transformation in infected cells by cellular enzymes into a nucleotide form -favipiravir ribose triphosphate (FPV-RTP). FPV-RTP is able to bind to viral RNA-dependent RNA polymerase and integrate into the viral RNA chain, causing a significant mutagenic effect through G→A and G→U transitions in the viral RNA genome. Besides the virus inhibiting effect, the increased synthesis of mutant virions under the action of FP possess a threat of the emergence of novel threatening viral strains with high pathogenicity for humans and animals and acquired resistance to chemotherapeutic compound. There are three ways to minimize this mutagenic effect of FP. (1) Synthesis of new FPV modifications lacking the ability to integrate into the synthesized viral RNA molecule. (2) The combined use of FPV with antiviral chemotherapeutic drugs of a different mechanism of action directed at various viral and/or host cell targets. (3) Permanent application of high therapeutic doses of FPV under the strict medical control to enhance the lethal mutagenic effect on an infectious virus in the recipient organism to prevent the multiplication of its mutant forms.
Author contribution. Аll authors made a substantial contribution to the conception of the work, acquisition, analysis, interpretation of data for the work, drafting and revising the work, final approval of the version to be published.
References
Abdelnabi, Morais, Leyssen, Imbert, Beaucourt et al., Understanding the Mechanism of the Broad-Spectrum Antiviral Activity of Favipiravir (T-705): Key Role of the F1 Motif of the Viral Polymerase, J. Virol, doi:10.1128/jvi.00487-17
Alyona, Chernyshova -Junior, Researcher, None
Arias, Thorne, Goodfellow, Favipiravir elicit antiviral mutagenesis during virus replication in vivo, eLife, doi:10.7554/elife.03679
Baranovich, Wong, Armstrong, Marjuki, Webby et al., T-705 (favipiravir) induces lethal mutagenesis in influenza A H1N1 viruses in vitro, J. Virol, doi:10.1128/jvi.02346-12
Baz, Carbonneau, Rhéaume, Cavanagh, Boivin, Combination therapy with Oseltamivir and Favipiravir delays mortality but does not prevent Oseltamivir resistance in immunodeficient mice infected with pandemic A(H1N1) influenza virus, Viruses, doi:10.3390/v10110610
Beigel, Bao, Beeler, Manosuthi, Slandzicki et al., A randomized double-blind phase 2 study of combination antivirals for the treatment of influenza, Lancet, doi:10.1016/S1473-3099(17)30476-0
Bixler, Bocan, Wells, Wetzel, Van Tongeren et al., Intracellular conversion and in vivo dose response of favipiravir (T-705) in rodents infected with Ebola virus, Antiviral Res, doi:10.1016/j.antiviral.2017.12.020
Cai, Yang, Liu, Chen, Shu et al., Experimental treatment with Favipiravir for COVID-19: An open-label control study, Engineering, doi:10.1016/j.eng.2020.03.007
De Ávila, Gallego, Soria, Gregori, Quer et al., Lethal mutagenesis of hepatitis C virus induced by Favipiravir, PLoS One, doi:10.1371/journal.pone.0164691
Delang, Abdelnabi, Neyts, Favipiravir as a potential countermeasure against neglected and emerging RNA viruses, Antiviral Res, doi:10.1016/j.anti-viral.2018.03.003
Du, Chen, Response to "Dose rationale for Favipiravir use in patients infected with SARS-CoV-2, Clin. Pharmacol. Ther, doi:10.1002/cpt.1878
Dunning, Baillie, Cao, Hayden, Antiviral combinations for severe influenza, Lancet Infect. Dis, doi:10.1016/S1473-3099
Eloy, Solas, Touret, Mentré, Malvy et al., Dose rationale for Favipiravir use in patients infected with SARS-CoV-2, Clin. Pharmacol. Ther, doi:10.1002/cpt.1877
Ferron, Structural and molecular basis of mismatch correction and ribavirin excision from coronavirus RNA, Proc. Natl. Acad. Sci, doi:10.1073/pnas.1718806115
Furuta, Egawa, Nitrogenous heterocyclic carboxamide derivatives or salts thereof and antiviral agents containing both, European Patent Office WO
Furuta, Gowen, Takahashi, Shiraki, Smee et al., Favipiravir (T-705), a novel viral RNA polymerase inhibitor, Antiviral Res, doi:10.1016/j.antiviral.2013.09.015
Furuta, Komeno, Nakamura, Favipiravir (T-705), a broad spectrum inhibitor of viral RNA polymerase, Proc. Jpn Acad. Ser. B Phys. Biol. Sci, doi:10.2183/pjab.93.027
Furuta, Takahashi, Kuno-Maekawa, Sangawa, Uehara et al., Mechanism of action of T-705 against influenza virus, Antimicrob. Agents Chemother, doi:10.1128/AAC.49.3.981-986.2005
Goldhill, Velthuis, Fletcher, Langat, Zambon et al., The mechanism of resistance to Favipiravir in influenza, Proc. Natl Acad. Sci, doi:10.1073/pnas.1811345115
Grande-Pérez, Lazaro, Lowenstein, Domingo, Manrubia, Suppression of viral infectivity through lethal defection, Proc. Natl Acad. Sci, doi:10.1073/pnas.0408871102
Guedj, Piorkowski, Jacquot, Madelain, Nguyen et al., Antiviral efficacy of Favipiravir against Ebo la virus: A translational study in cynomolgus macaques, PLoS Med, doi:10.1371/journal.pmed.1002535
Hurt, Ison, Hayden, Hay, Second isirv antiviral group conference: overview. Influenza Other, Respir. Viru ses, doi:10.1111/irv.12207
Ilyushina, Bovin, Webster, Govorkova, Combination chemotherapy, a potential strategy for reducing the emergence of drug-resistant influenza A variants, Antiviral Res, doi:10.1016/j.antiviral.2006.01.012
Ivashchenko, Dmitriev, Vostokova, Azarova, Blinow et al., AVIFAVIR for treatment of patients with moderate COVID-19: Interim results of a phase II/III multicenter randomized clinical trial, Clin. Infect. Dis, doi:10.1093/cid/ciaa1176
Jordan, Stevens, Deval, Nucleosides for the treatment of respiratory RNA virus infections, Antivir. Chem. Chemother, doi:10.1177/2040206618764483
Joshi, Parkar, Ansari, Vora, Talwar et al., Role of Favipiravir in the treatment of COVID-19, Int. J. Infect. Dis, doi:10.1016/j.ijid.2020.10.069
Li, De Clercq, Therapeutic options for the 2019 novel coronavirus (2019-nCoV), Nat. Rev. Drug Discov, doi:10.1038/d41573-020-00016-0
Li, Yang, Liu, Yang, Zhao et al., Effect of combination antiviral therapy on hematological profiles in 151 adults hospitalized with severe coronavirus disease 2019, Pharmacol. Res, doi:10.1016/j.phrs.2020.105036
Lu, Hardes, Dahms, Böttcher-Friebertshäuser, Steinmetzer et al., Peptidomimetic furin inhibitor MI-701 in combination with oseltamivir and ribavirin efficiently blocks propagation of highly pathogenic avian influenza viruses and delays high level oseltamivir resistance in MDCK cells, Antiviral Res, doi:10.1016/j.antiviral.2015.05.006
Naesens, Guddat, Keough, Van Kuilenburg, Meijer et al., Role of human hypoxanthine guanine phosphoribosyltransferase in activation of the antiviral agent T-705 (favipiravir), Mol. Pharmacol, doi:10.1124/mol.113.087247
Neogi, Hill, Ambikan, Heng, Quinn et al., Feasibility of known RNA polymerase inhibitors as anti-SARS-CoV-2 drugs, Pathogens, doi:10.3390/pathogens9050320
Ortega, Zambrano, Jastrzebska, Liprandi, Rangel et al., Understanding severe acute respiratory syndrome coronavirus 2 replication to design efficient drug combination therapies, Intervirology, doi:10.1159/000512141
Perales, Gallego, De Ávila, Soria, Gregori et al., The increasing impact of lethal mutagenesis of viruses, Future Med. Chem, doi:10.4155/fmc-2018-0457
Perales, Mateo, Mateu, Domingo, Insights into RNA virus mutant spectrum and lethal mutagenesis events: replicative interference and complementation by multiple point mutants, J. Mol. Biol, doi:10.1016/j.jmb.2007.03.074
Pilkington, Pepperrell, Hill, A review of the safety of favipiravir -a potential treatment in the COVID-19 pandemic?, J. Virus Erad, doi:10.1016/s2055-6640(20)30016-9
Sada, Saraya, Ishii, Okayama, Hayashi et al., Detailed molecular interactions of Favipiravir with SARS-CoV-2, SARS-CoV, MERS-CoV, and influenza virus polymerases in silico, Microorganisms, doi:10.3390/microorganisms8101610
Sangawa, Komeno, Nishikawa, Yoshida, Takahashi et al., Mechanism of action of T-705 ribosyl triphosphate against influenza virus RNA polymerase, Antimicrob. Agents Chemother, doi:10.1128/aac.00649-13
Shannon, Selisko, Le, Huchting, Touret et al., Rapid incorporation of Favipiravir by the fast and permissive viral RNA polymerase complex results in ЖУРНАЛ МИКРОБИОЛОГИИ
Shiraki, Daikoku, Favipiravir, an anti-influenza drug against life-threatening RNA virus infections, Pharmacol Ther, doi:10.1016/j.pharmthera.2020.107512
Smee, Hurst, Egawa, Takahashi, Kadota et al., Intracellular metabolism of favipiravir (T-705) in uninfected and influenza A (H5N1) virus-infected cells. J. Antimicrob, Chemother, doi:10.1093/jac/dkp274
Smith, Rajwanshi, Kim, Deval, The ambiguous base-pairing and high substrate efficiency of T-705 (Favipiravir) ribofuranosyl 5'-triphosphate towards influenza A virus polymerase, PLoS One, doi:10.1371/journal.pone.0068347
Tsai, Lu, Bau, Chiu, Yen et al., Approaches towards fighting the COVID-19 pandemic (Review), Int. J. Mol. Med, doi:10.3892/ijmm.2020.4794
Wang, Cao, Zhang, Yang, Liu et al., Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro, Cell. Res, doi:10.1038/s41422-020-0282-0
Zhirnov -D. Sci ; Prof, Corr, Information about the authors Oleg
Zhirnov, High protection of animals lethally infected with influenza virus by aprotinin-rimantadine combination, J. Med. Virol, doi:10.1002/jmv.1890210208
Zhirnov, Molecular targets in the chemotherapy of coronavirus infection, Biochemistry (Mosc), doi:10.1134/S0006297920050016
Авторов, Все авторы внесли существенный вклад в проведение поисково-аналитической работы и подготовку статьи, прочли и одобрили финальную версию до публикации, Статья поступила в редакцию
Алёна Игоревна -М, Русско-немецкой академии медико-социальных и биотехнологических наук
DOI record:
{
"DOI": "10.36233/0372-9311-114",
"ISSN": [
"2686-7613",
"0372-9311"
],
"URL": "http://dx.doi.org/10.36233/0372-9311-114",
"abstract": "<jats:p> </jats:p><jats:p>The antiviral drug favipiravir (FVP), which is a structural analogue of guanosine, undergoes chemical transformation in infected cells by cellular enzymes into a nucleotide form — favipiravir ribose triphosphate (FVPRTP). FVP-RTP is able to bind to viral RNA-dependent RNA polymerase and integrate into the viral RNA chain, causing a significant mutagenic effect through G→A and С→U transitions in the viral RNA genome. Besides the virus inhibiting effect, the increased synthesis of mutant virions under the action of FPV possess a threat of the emergence of novel threatening viral strains with high pathogenicity for humans and animals and acquired resistance to chemotherapeutic compound. There are three ways to minimize this mutagenic effect of FP. (1) Synthesis of new FPV modifications lacking the ability to integrate into the synthesized viral RNA molecule. (2) The combined use of FPV with antiviral chemotherapeutic drugs of a different mechanism of action directed at various viral and/or host cell targets. (3) Permanent application of high therapeutic doses of FPV under the strict medical control to enhance the lethal mutagenic effect on an infectious virus in the recipient organism to prevent the multiplication of its mutant forms.</jats:p>",
"author": [
{
"ORCID": "http://orcid.org/0000-0002-3192-8405",
"affiliation": [
{
"name": "The Russian-German Academy of Medico-Social and Biotechnological Sciences;\r\nThe D.I. Ivanovsky Institute of Virology, The N.F. Gamaleya National Research Center of Epidemiology and Microbiology"
}
],
"authenticated-orcid": true,
"family": "Zhirnov",
"given": "O. P.",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0003-1290-4042",
"affiliation": [
{
"name": "The D.I. Ivanovsky Institute of Virology, The N.F. Gamaleya National Research Center of Epidemiology and Microbiology;\r\nThe I.M. Sechenov First Moscow State Medical University (Sechenov University)"
}
],
"authenticated-orcid": true,
"family": "Chernyshova",
"given": "A. I.",
"sequence": "additional"
}
],
"container-title": "Journal of microbiology, epidemiology and immunobiology",
"container-title-short": "Zhurnal mikrobiologii, èpidemiologii i immunobiologii",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"microbiol.elpub.ru"
]
},
"created": {
"date-parts": [
[
2021,
5,
5
]
],
"date-time": "2021-05-05T07:44:12Z",
"timestamp": 1620200652000
},
"deposited": {
"date-parts": [
[
2021,
5,
5
]
],
"date-time": "2021-05-05T07:45:22Z",
"timestamp": 1620200722000
},
"indexed": {
"date-parts": [
[
2022,
3,
31
]
],
"date-time": "2022-03-31T14:51:34Z",
"timestamp": 1648738294054
},
"is-referenced-by-count": 3,
"issue": "2",
"issued": {
"date-parts": [
[
2021,
5,
5
]
]
},
"journal-issue": {
"issue": "2",
"published-online": {
"date-parts": [
[
2021,
5,
5
]
]
}
},
"license": [
{
"URL": "https://microbiol.elpub.ru/jour/about/editorialPolicies#openAccessPolicy",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
5,
5
]
],
"date-time": "2021-05-05T00:00:00Z",
"timestamp": 1620172800000
}
}
],
"link": [
{
"URL": "https://microbiol.elpub.ru/jour/article/viewFile/1005/590",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://microbiol.elpub.ru/jour/article/viewFile/1005/598",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "22004",
"original-title": [],
"page": "213-220",
"prefix": "10.36233",
"published": {
"date-parts": [
[
2021,
5,
5
]
]
},
"published-online": {
"date-parts": [
[
2021,
5,
5
]
]
},
"publisher": "Central Research Institute for Epidemiology",
"reference": [
{
"DOI": "10.1134/S0006297920050016",
"doi-asserted-by": "crossref",
"key": "ref1",
"unstructured": "Zhirnov O.P. Molecular targets in the chemotherapy of coronavirus infection. Biochemistry (Mosc). 2020; 85(5): 523–30. https://doi.org/10.1134/S0006297920050016"
},
{
"DOI": "10.3892/ijmm.2020.4794",
"doi-asserted-by": "crossref",
"key": "ref2",
"unstructured": "Tsai S.C., Lu C.C., Bau D.T., Chiu Y.J., Yen Y.T., Hsu Y.M., et al. Approaches towards fighting the COVID 19 pandemic (Review). Int. J. Mol. Med. 2020; 47(1): 3–22. https://doi.org/10.3892/ijmm.2020.4794"
},
{
"DOI": "10.1016/j.antiviral.2013.09.015",
"doi-asserted-by": "crossref",
"key": "ref3",
"unstructured": "Furuta Y., Gowen B.B., Takahashi K., Shiraki K., Smee D.F., Barnard D.L. Favipiravir (T-705), a novel viral RNA polymerase inhibitor. Antiviral Res. 2013; 100(2): 446–54. https://doi.org/10.1016/j.antiviral.2013.09.015"
},
{
"DOI": "10.2183/pjab.93.027",
"doi-asserted-by": "crossref",
"key": "ref4",
"unstructured": "Furuta Y., Komeno T., Nakamura T. Favipiravir (T-705), a broad spectrum inhibitor of viral RNA polymerase. Proc. Jpn Acad. Ser. B Phys. Biol. Sci. 2017; 93(7): 449–63. https://doi.org/10.2183/pjab.93.027"
},
{
"key": "ref5",
"unstructured": "Furuta Y., Egawa H. Nitrogenous heterocyclic carboxamide derivatives or salts thereof and antiviral agents containing both. European Patent Office WO, 00/10569 (JP25044198 application 20.08.1998). WO2000010569A1; 2000."
},
{
"DOI": "10.1016/j.pharmthera.2020.107512",
"doi-asserted-by": "crossref",
"key": "ref6",
"unstructured": "Shiraki K., Daikoku T. Favipiravir, an anti-influenza drug against life-threatening RNA virus infections. Pharmacol Ther. 2020; 209: 107512. https://doi.org/10.1016/j.pharmthera.2020.107512"
},
{
"DOI": "10.1016/S2055-6640(20)30016-9",
"doi-asserted-by": "crossref",
"key": "ref7",
"unstructured": "Pilkington V., Pepperrell T., Hill A. A review of the safety of favipiravir – a potential treatment in the COVID-19 pandemic? J. Virus Erad. 2020; 6(2): 45–51. https://doi.org/10.1016/s2055-6640(20)30016-9"
},
{
"DOI": "10.1128/JVI.00487-17",
"doi-asserted-by": "crossref",
"key": "ref8",
"unstructured": "Abdelnabi R., Morais A.T.S., Leyssen P., Imbert I., Beaucourt S., Blanc H., et al. Understanding the Mechanism of the Broad-Spectrum Antiviral Activity of Favipiravir (T-705): Key Role of the F1 Motif of the Viral Polymerase. J. Virol. 2017; 91(12): e00487–17. https://doi.org/10.1128/jvi.00487-17"
},
{
"DOI": "10.1177/2040206618764483",
"doi-asserted-by": "crossref",
"key": "ref9",
"unstructured": "Jordan P.C., Stevens S.K., Deval J. Nucleosides for the treatment of respiratory RNA virus infections. Antivir. Chem. Chemother. 2018; 26: 2040206618764483. https://doi.org/10.1177/2040206618764483"
},
{
"DOI": "10.3390/pathogens9050320",
"doi-asserted-by": "crossref",
"key": "ref10",
"unstructured": "Neogi U., Hill K.J., Ambikan A.T., Heng X., Quinn T.P., Byrareddy S.N., et al. Feasibility of Known RNA Polymerase Inhibitors as Anti-SARS-CoV-2 Drugs. Pathogens. 2020; 9(5): 320. https://doi.org/10.3390/pathogens9050320"
},
{
"DOI": "10.1016/j.antiviral.2018.03.003",
"doi-asserted-by": "crossref",
"key": "ref11",
"unstructured": "Delang L., Abdelnabi R., Neyts J. Favipiravir as a potential countermeasure against neglected and emerging RNA viruses. Antiviral Res. 2018; 153: 85–94. https://doi.org/10.1016/j.antiviral.2018.03.003"
},
{
"DOI": "10.3390/microorganisms8101610",
"doi-asserted-by": "crossref",
"key": "ref12",
"unstructured": "Sada M., Saraya T., Ishii H., Okayama K., Hayashi Y., Tsugawa T., et al. Detailed molecular interactions of Favipiravir with SARS-CoV-2, SARS-CoV, MERS-CoV, and influenza virus polymerases in silico. Microorganisms. 2020; 8(10): 1610. https://doi.org/10.3390/microorganisms8101610"
},
{
"DOI": "10.1124/mol.113.087247",
"doi-asserted-by": "crossref",
"key": "ref13",
"unstructured": "Naesens L., Guddat L.W., Keough D.T., van Kuilenburg A.B., Meijer J., Vande Voorde J., et al. Role of human hypoxanthine guanine phosphoribosyltransferase in activation of the antiviral agent T-705 (favipiravir). Mol. Pharmacol. 2013; 84(4): 615–29. https://doi.org/10.1124/mol.113.087247"
},
{
"DOI": "10.1093/jac/dkp274",
"doi-asserted-by": "crossref",
"key": "ref14",
"unstructured": "Smee D.F., Hurst B.L., Egawa H., Takahashi K., Kadota T., Furuta Y. Intracellular metabolism of favipiravir (T-705) in uninfected and influenza A (H5N1) virus-infected cells. J. Antimicrob. Chemother. 2009; 64(4): 741–6. https://doi.org/10.1093/jac/dkp274"
},
{
"DOI": "10.1016/j.antiviral.2017.12.020",
"doi-asserted-by": "crossref",
"key": "ref15",
"unstructured": "Bixler S.L., Bocan T.M., Wells J., Wetzel K.S., Van Tongeren S.A., Garza N.L., et al. Intracellular conversion and in vivo dose response of favipiravir (T-705) in rodents infected with Ebola virus. Antiviral Res. 2018; 151: 50–4. https://doi.org/10.1016/j.antiviral.2017.12.020"
},
{
"DOI": "10.1128/JVI.02346-12",
"doi-asserted-by": "crossref",
"key": "ref16",
"unstructured": "Baranovich T., Wong S.S., Armstrong J., Marjuki H., Webby R.J., Webster R.G., et al. T-705 (favipiravir) induces lethal mutagenesis in influenza A H1N1 viruses in vitro. J. Virol. 2013; 87(7): 3741–51. https://doi.org/10.1128/jvi.02346-12"
},
{
"DOI": "10.7554/eLife.03679",
"doi-asserted-by": "crossref",
"key": "ref17",
"unstructured": "Arias A., Thorne L., Goodfellow I. Favipiravir elicit antiviral mutagenesis during virus replication in vivo. eLife. 2014; 3: e03679. https://doi.org/10.7554/elife.03679"
},
{
"DOI": "10.1128/AAC.00649-13",
"doi-asserted-by": "crossref",
"key": "ref18",
"unstructured": "Sangawa H., Komeno T., Nishikawa H., Yoshida A., Takahashi K., Nomura N., et al. Mechanism of action of T-705 ribosyl triphosphate against influenza virus RNA polymerase. Antimicrob. Agents Chemother. 2013; 57(11): 5202–8. https://doi.org/10.1128/aac.00649-13"
},
{
"DOI": "10.1371/journal.pone.0068347",
"doi-asserted-by": "crossref",
"key": "ref19",
"unstructured": "Jin Z., Smith L.K., Rajwanshi V.K., Kim B., Deval J. The ambiguous base-pairing and high substrate efficiency of T-705 (Favipiravir) ribofuranosyl 5’-triphosphate towards influenza A virus polymerase. PLoS One. 2013; 8(7): e68347. https://doi.org/10.1371/journal.pone.0068347"
},
{
"DOI": "10.1371/journal.pone.0164691",
"doi-asserted-by": "crossref",
"key": "ref20",
"unstructured": "de Ávila A.I., Gallego I., Soria M.E., Gregori J., Quer J., Esteban J.I., et al. Lethal mutagenesis of hepatitis C virus induced by Favipiravir. PLoS One. 2016; 11(10): e0164691. https://doi.org/10.1371/journal.pone.0164691"
},
{
"DOI": "10.1371/journal.pmed.1002535",
"doi-asserted-by": "crossref",
"key": "ref21",
"unstructured": "Guedj J., Piorkowski G., Jacquot F., Madelain V., Nguyen T.H.T., Rodallec A., et al. Antiviral efficacy of Favipiravir against Ebola virus: A translational study in cynomolgus macaques. PLoS Med. 2018; 15(3): e1002535. https://doi.org/10.1371/journal.pmed.1002535"
},
{
"DOI": "10.1073/pnas.1811345115",
"doi-asserted-by": "crossref",
"key": "ref22",
"unstructured": "Goldhill D.H., te Velthuis A.J.W., Fletcher R.A., Langat P., Zambon M., Lackenby A., et al. The mechanism of resistance to Favipiravir in influenza. Proc. Natl Acad. Sci. USA. 2018; 115(45): 11613–8. https://doi.org/10.1073/pnas.1811345115"
},
{
"DOI": "10.1038/s41467-020-18463-z",
"doi-asserted-by": "crossref",
"key": "ref23",
"unstructured": "Shannon A., Selisko B., Le N.T., Huchting J., Touret F., Piorkowski G., et al. Rapid incorporation of Favipiravir by the fast and permissive viral RNA polymerase complex results in SARS-CoV-2 lethal mutagenesis. Nat. Commun. 2020; 11(1): 4682. https://doi.org/10.1038/s41467-020-18463-z"
},
{
"DOI": "10.1073/pnas.0408871102",
"doi-asserted-by": "crossref",
"key": "ref24",
"unstructured": "Grande-Pérez A., Lazaro E., Lowenstein P., Domingo E., Manrubia S.C. Suppression of viral infectivity through lethal defection. Proc. Natl Acad. Sci. USA. 2005; 102(12): 4448–52. https://doi.org/10.1073/pnas.0408871102"
},
{
"DOI": "10.1016/j.jmb.2007.03.074",
"doi-asserted-by": "crossref",
"key": "ref25",
"unstructured": "Perales C., Mateo R., Mateu M.G., Domingo E. Insights into RNA virus mutant spectrum and lethal mutagenesis events: replicative interference and complementation by multiple point mutants. J. Mol. Biol. 2007; 369(4): 985–1000. https://doi.org/10.1016/j.jmb.2007.03.074"
},
{
"DOI": "10.1038/s41422-020-0282-0",
"doi-asserted-by": "crossref",
"key": "ref26",
"unstructured": "Wang M., Cao R., Zhang L., Yang X., Liu J., Xu M., et al. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell. Res. 2020; 30: 269–71. https://doi.org/10.1038/s41422-020-0282-0"
},
{
"DOI": "10.1016/j.eng.2020.03.007",
"doi-asserted-by": "crossref",
"key": "ref27",
"unstructured": "Cai Q., Yang M., Liu D., Chen J., Shu D., Xia J., et al. Experimental treatment with Favipiravir for COVID-19: An open-label control study. Engineering (Beijing). 2020; 6(10): 1192–8. https://doi.org/10.1016/j.eng.2020.03.007"
},
{
"DOI": "10.1016/j.ijid.2020.10.069",
"doi-asserted-by": "crossref",
"key": "ref28",
"unstructured": "Joshi S., Parkar J., Ansari A., Vora A., Talwar D., Tiwaskar M., et al. Role of Favipiravir in the treatment of COVID-19. Int. J. Infect. Dis. 2020; 102: 501–8. https://doi.org/10.1016/j.ijid.2020.10.069"
},
{
"DOI": "10.1093/cid/ciaa1176",
"doi-asserted-by": "crossref",
"key": "ref29",
"unstructured": "Ivashchenko A.A., Dmitriev K.A., Vostokova N.V., Azarova V.N., Blinow A.A., Egorova A.N., et al. AVIFAVIR for treatment of patients with moderate COVID-19: Interim results of a phase II/III multicenter randomized clinical trial. Clin. Infect. Dis. 2020; ciaa1176. https://doi.org/10.1093/cid/ciaa1176"
},
{
"DOI": "10.1002/cpt.1877",
"doi-asserted-by": "crossref",
"key": "ref30",
"unstructured": "Eloy P., Solas C., Touret F., Mentré F., Malvy D., de Lamballerie X., et al. Dose rationale for Favipiravir use in patients infected with SARS-CoV-2. Clin. Pharmacol. Ther. 2020; 108(2): 188. https://doi.org/10.1002/cpt.1877"
},
{
"DOI": "10.4155/fmc-2018-0457",
"doi-asserted-by": "crossref",
"key": "ref31",
"unstructured": "Perales C., Gallego I., de ́Avila A.I., Soria M.E., Gregori J., Quer J., et al. The increasing impact of lethal mutagenesis of viruses. Future Med. Chem. 2019; 11(13): 1645–57. https://doi.org/10.4155/fmc-2018-0457"
},
{
"DOI": "10.1038/d41573-020-00016-0",
"doi-asserted-by": "crossref",
"key": "ref32",
"unstructured": "Li G., De Clercq E. Therapeutic options for the 2019 novel coronavirus (2019-nCoV). Nat. Rev. Drug Discov. 2020; 19(3): 149–50. https://doi.org/10.1038/d41573-020-00016-0"
},
{
"DOI": "10.1073/pnas.1718806115",
"doi-asserted-by": "crossref",
"key": "ref33",
"unstructured": "Ferron F. Structural and molecular basis of mismatch correction and ribavirin excision from coronavirus RNA. Proc. Natl. Acad. Sci. USA. 2018; 115(2): E162–71. https://doi.org/10.1073/pnas.1718806115"
},
{
"DOI": "10.1016/j.antiviral.2006.01.012",
"doi-asserted-by": "crossref",
"key": "ref34",
"unstructured": "Ilyushina N.A., Bovin N.V., Webster R.G., Govorkova E.A. Combination chemotherapy, a potential strategy for reducing the emergence of drug-resistant influenza A variants. Antiviral Res. 2006; 70(3): 121–31. https://doi.org/10.1016/j.antiviral.2006.01.012"
},
{
"DOI": "10.1016/j.antiviral.2015.05.006",
"doi-asserted-by": "crossref",
"key": "ref35",
"unstructured": "Lu Y., Hardes K., Dahms S.O., Böttcher-Friebertshäuser E., Steinmetzer T., Than M.E., et al. Peptidomimetic furin inhibitor MI-701 in combination with oseltamivir and ribavirin efficiently blocks propagation of highly pathogenic avian influenza viruses and delays high level oseltamivir resistance in MDCK cells. Antiviral Res. 2015; 120: 89–100. https://doi.org/10.1016/j.antiviral.2015.05.006"
},
{
"DOI": "10.3390/v10110610",
"doi-asserted-by": "crossref",
"key": "ref36",
"unstructured": "Baz M., Carbonneau J., Rhéaume C., Cavanagh M.H., Boivin G. Combination therapy with Oseltamivir and Favipiravir delays mortality but does not prevent Oseltamivir resistance in immunodeficient mice infected with pandemic A(H1N1) influenza virus. Viruses. 2018; 10(11): 610. https://doi.org/10.3390/v10110610"
},
{
"DOI": "10.1016/S1473-3099(17)30476-0",
"doi-asserted-by": "crossref",
"key": "ref37",
"unstructured": "Beigel J.H., Bao Y., Beeler J., Manosuthi W., Slandzicki A., Dar S.M., et al. A randomized double-blind phase 2 study of combination antivirals for the treatment of influenza. Lancet Infect. Dis. 2017; 17: 1255–65. https://doi.org/10.1016/S1473-3099(17)30476-0"
},
{
"DOI": "10.1111/irv.12207",
"doi-asserted-by": "crossref",
"key": "ref38",
"unstructured": "Hurt A.C., Ison M.G., Hayden F.G., Hay A.J. Second isirv antiviral group conference: overview. Influenza Other Respir. Viruses. 2013; 7(Suppl. 3): 1–7. https://doi.org/10.1111/irv.12207"
},
{
"DOI": "10.1016/S1473-3099(14)70821-7",
"doi-asserted-by": "crossref",
"key": "ref39",
"unstructured": "Dunning J., Baillie J.K., Cao B., Hayden F.G. Antiviral combinations for severe influenza. Lancet Infect. Dis. 2014; 14(12): 1259–70. https://doi.org/10.1016/S1473-3099(14)70821-7"
},
{
"DOI": "10.1016/j.phrs.2020.105036",
"doi-asserted-by": "crossref",
"key": "ref40",
"unstructured": "Li X., Yang Y., Liu L., Yang X., Zhao X., Li Y., et al. Effect of combination antiviral therapy on hematological profiles in 151 adults hospitalized with severe coronavirus disease 2019. Pharmacol. Res. 2020; 160: 105036. https://doi.org/10.1016/j.phrs.2020.105036"
},
{
"DOI": "10.1159/000512141",
"doi-asserted-by": "crossref",
"key": "ref41",
"unstructured": "Ortega J.T., Zambrano J.L., Jastrzebska B., Liprandi F., Rangel H.R., Pujol F.H. Understanding severe acute respiratory syndrome coronavirus 2 replication to design efficient drug combination therapies. Intervirology. 2020; 63(1-6): 2–9. https://doi.org/10.1159/000512141"
},
{
"DOI": "10.1002/jmv.1890210208",
"doi-asserted-by": "crossref",
"key": "ref42",
"unstructured": "Zhirnov O.P. High protection of animals lethally infected with influenza virus by aprotinin-rimantadine combination. J. Med. Virol. 1987; 21(2): 161–7. https://doi.org/10.1002/jmv.1890210208"
},
{
"DOI": "10.1128/AAC.49.3.981-986.2005",
"doi-asserted-by": "crossref",
"key": "ref43",
"unstructured": "Furuta Y., Takahashi K., Kuno-Maekawa M., Sangawa H., Uehara S., Kozaki K., et al. Mechanism of action of T-705 against influenza virus. Antimicrob. Agents Chemother. 2005; 49(3): 981–6. https://doi.org/10.1128/AAC.49.3.981-986.2005"
},
{
"DOI": "10.1002/cpt.1878",
"doi-asserted-by": "crossref",
"key": "ref44",
"unstructured": "Du Y.X., Chen X.P. Response to “Dose rationale for Favipiravir use in patients infected with SARS-CoV-2”. Clin. Pharmacol. Ther. 2020; 108(2): 190. https://doi.org/10.1002/cpt.1878"
}
],
"reference-count": 44,
"references-count": 44,
"relation": {},
"resource": {
"primary": {
"URL": "https://microbiol.elpub.ru/jour/article/view/1005"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Favipiravir: the hidden threat of mutagenic action",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.36233/0372-9311-crossmark",
"volume": "98"
}