Safety and efficacy of Favipiravir in moderate to severe SARS-CoV-2 pneumonia
et al., International Immunopharmacology, doi:10.1016/j.intimp.2021.107522, Mar 2021
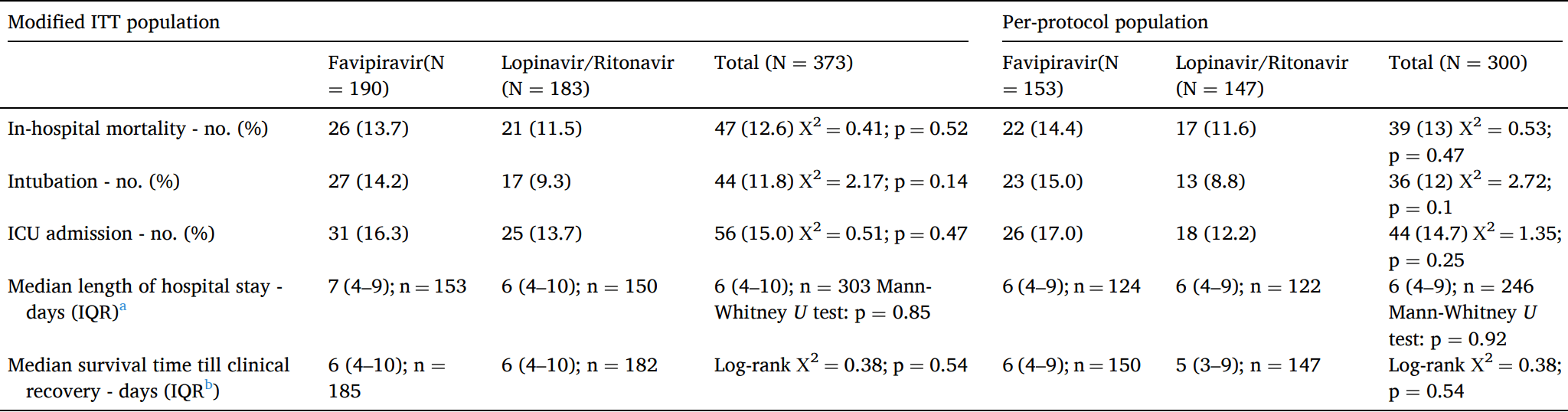
RCT late stage patients (median SpO2 89), 193 treated with favipiravir, 187 with lopinavir/ritonavir, showing no significant differences in mortality, intubation, or ICU admission.
Potential risks of favipiravir include kidney injury1-3, liver injury2-5, cardiovascular events5,6, pulmonary toxicity6,7, and mutagenicity, carcinogenicity, teratogenicity, embryotoxicity, and the creation of dangerous variants8-14.
|
risk of death, 19.2% higher, RR 1.19, p = 0.54, treatment 26 of 190 (13.7%), control 21 of 183 (11.5%).
|
|
risk of mechanical ventilation, 53.0% higher, RR 1.53, p = 0.15, treatment 27 of 190 (14.2%), control 17 of 183 (9.3%).
|
|
risk of ICU admission, 19.4% higher, RR 1.19, p = 0.56, treatment 31 of 190 (16.3%), control 25 of 183 (13.7%).
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Abdulaziz et al., Clinical Features and Prognosis of Acute Kidney Injury in Hospital-Admitted Patients with COVID-19 in Egypt: A Single-Center Experience, Mansoura Medical Journal, doi:10.58775/2735-3990.1433.
2.
Ülger et al., Experimental evaluation of favipiravir (T-705)-induced liver and kidney toxicity in rats, Food and Chemical Toxicology, doi:10.1016/j.fct.2025.115472.
3.
El-Fetouh et al., Experimental Studies on Some Drugs Used in Covid-19 Treatment (Favipiravir and Dexamethasone) in Albino Rats, Journal of Advanced Veterinary Research, 13:10, www.advetresearch.com/index.php/AVR/article/view/1635.
4.
Almutairi et al., Liver Injury in Favipiravir-Treated COVID-19 Patients: Retrospective Single-Center Cohort Study, Tropical Medicine and Infectious Disease, doi:10.3390/tropicalmed8020129.
5.
Siby et al., Temporal Trends in Serious Adverse Events Associated with Oral Antivirals During the COVID-19 Pandemic: Insights from the FAERS Database (2020–2023), Open Forum Infectious Diseases, doi:10.1093/ofid/ofaf695.1825.
6.
Ozhan et al., Evaluation of the cardiopulmonary effects of repurposed COVID-19 therapeutics in healthy rats, Scientific Reports, doi:10.1038/s41598-025-31048-4.
7.
Ülger (B) et al., Evaluation of the effects of favipiravir (T-705) on the lung tissue of healty rats: An experimental study, Food and Chemical Toxicology, doi:10.1016/j.fct.2025.115235.
8.
Zhirnov et al., Favipiravir: the hidden threat of mutagenic action, Journal of microbiology, epidemiology and immunobiology, doi:10.36233/0372-9311-114.
9.
Waters et al., Human genetic risk of treatment with antiviral nucleoside analog drugs that induce lethal mutagenesis: the special case of molnupiravir, Environmental and Molecular Mutagenesis, doi:10.1002/em.22471.
10.
Hadj Hassine et al., Lethal Mutagenesis of RNA Viruses and Approved Drugs with Antiviral Mutagenic Activity, Viruses, doi:10.3390/v14040841.
11.
Shum, C., An investigational study into the drug-associated mutational signature in SARS-CoV-2 viruses, The University of Hong Kong, PhD Thesis, hub.hku.hk/handle/10722/344396.
12.
Shiraki et al., Convenient screening of the reproductive toxicity of favipiravir and antiviral drugs in Caenorhabditis elegans, Heliyon, doi:10.1016/j.heliyon.2024.e35331.
Solaymani-Dodaran et al., 11 Mar 2021, Randomized Controlled Trial, Iran, peer-reviewed, 44 authors, study period 4 February, 2020 - 8 March, 2020, this trial compares with another treatment - results may be better when compared to placebo.
Safety and efficacy of Favipiravir in moderate to severe SARS-CoV-2 pneumonia
International Immunopharmacology, doi:10.1016/j.intimp.2021.107522
Background: We examined the safety and efficacy of a treatment protocol containing Favipiravir for the treatment of SARS-CoV-2. Methods: We did a multicenter randomized open-labeled clinical trial on moderate to severe cases infections of SARS-CoV-2. Patients with typical ground glass appearance on chest computerized tomography scan (CT scan) and oxygen saturation (SpO 2 ) of less than 93% were enrolled. They were randomly allocated into Favipiravir (1.6 gr loading, 1.8 gr daily) and Lopinavir/Ritonavir (800/200 mg daily) treatment regimens in addition to standard care. In-hospital mortality, ICU admission, intubation, time to clinical recovery, changes in daily SpO 2 after min discontinuation of supplemental oxygen, and length of hospital stay were quantified and compared in the two groups. Results: 380 patients were randomly allocated into Favipiravir (1 9 3) and Lopinavir/Ritonavir (1 8 7) groups in centers. The number of deaths, intubations, and ICU admissions were not significantly different (26, 27, 31 and 21, 17, 25 respectively). Mean hospital stay was also not different (7.9 days [SD = 6] in the Favipiravir and 8.1 [SD = 6.5] days in Lopinavir/Ritonavir groups) (p = 0.61). Time to clinical recovery in the Favipiravir group was similar to Lopinavir/Ritonavir group (HR = 0.94, 95% CI 0.75 -1.17) and likewise the changes in the daily SpO after discontinuation of supplemental oxygen (p = 0.46) Conclusion: Adding Favipiravir to the treatment protocol did not reduce the number of ICU admissions or intubations or In-hospital mortality compared to Lopinavir/Ritonavir regimen. It also did not shorten time to clinical recovery and length of hospital stay.
Authors' contributionsRole of the funding source All authors drafted and drafted the manuscript, revised the manuscript, supervised the treatment and the and wrote the manuscript; and all authors approved the manuscript.
References
Bolarin, Oluwatoyosi, Orege, Therapeutic drugs for SARS-CoV-2 treatment: Current state and perspective, International Immunopharmacology
Cai, Yang, Liu, Experimental Treatment with Favipiravir for COVID-19: An Open-Label Control Study
Cao, Wang, Wen, A Trial of Lopinavir-Ritonavir in Adults Hospitalized with Severe Covid-19, The New England journal of medicine
Catanzaro, Fagiani, Racchi, Corsini, Govoni et al., Immune response in COVID-19: addressing a pharmacological challenge by targeting pathways triggered by SARS-CoV-2, Signal Transduct Target Ther
Dabbous, Abd-Elsalam, El-Sayed, Efficacy of favipiravir in COVID-19 treatment: a multi-center randomized study, Arch Virol
Doi, Hibino, Hase, A prospective, randomized, open-label trial of early versus late favipiravir in hospitalized patients with COVID-19, Antimicrob Agents Chemother
Du, Chen, Favipiravir: Pharmacokinetics and Concerns About Clinical Trials for 2019-nCoV Infection, Clinical pharmacology and therapeutics
Fu, Cao, Zhao, Li, Zhong et al., Oral favipiravir for patients with delayed SARS-CoV-2 viral RNA clearance: a case series, Crit Care
Furuta, Komeno, Nakamura, Favipiravir (T-705), a broad spectrum inhibitor of viral RNA polymerase, Proceedings of the Japan Academy Series B, Physical and biological sciences
Furuta, Takahashi, Fukuda, In Vitro and In Vivo Activities of Anti-Influenza Virus Compound T-705, Antimicrobial Agents and Chemotherapy
Geleris, Sun, Platt, Observational Study of Hydroxychloroquine in Hospitalized Patients with Covid-19, New England Journal of Medicine
Giammaria, Pajewski, Can early treatment of patients with risk factors contribute to managing the COVID-19 pandemic?, Journal of global health
Ivashchenko, Dmitriev, Vostokova, AVIFAVIR for Treatment of Patients with Moderate COVID-19: Interim Results of a Phase II/III Multicenter Randomized Clinical Trial, Clinical
Jin, Cai, Cheng, A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version), Military Medical Research
Kivrak, Ulas, Kivrak, A comparative analysis for anti-viral drugs: Their efficiency against SARS-CoV-2, International immunopharmacology
Mason, Pathogenesis of COVID-19 from a cell biology perspective, European Respiratory Journal
Mccullough, Favipiravir and the Need for Early Ambulatory Treatment of SARS-CoV2 Infection (COVID-19), Antimicrobial Agents and Chemotherapy
Meini, Pagotto, Longo, Vendramin, Pecori et al., Role of Lopinavir/Ritonavir in the Treatment of Covid-19: A Review of Current Evidence, Guideline Recommendations, and Perspectives, Journal of, Clinical Medicine
Moschini, Loffi, Regazzoni, Di Tano, Gherbesi et al., Effects on QT interval of hydroxychloroquine associated with ritonavir/darunavir or azithromycin in patients with SARS-CoV-2 infection
Sanders, Monogue, Jodlowski, Cutrell, Pharmacologic Treatments for Coronavirus Disease 2019 (COVID-19): A Review, Jama
Shannon, Selisko, Le, Favipiravir strikes the SARS-CoV-2 at its Achilles heel, the RNA polymerase, bioRxiv
Siddiqi, Mehra, COVID-19 illness in native and immunosuppressed states: A clinical-therapeutic staging proposal, J Heart Lung Transplant
Sissoko, Laouenan, Folkesson, Experimental Treatment with Favipiravir for Ebola Virus Disease (the JIKI Trial): A Historically Controlled, Single-Arm Proof-of-Concept Trial in Guinea, PLoS medicine
Tang, Cao, Han, Hydroxychloroquine in patients with mainly mild to moderate coronavirus disease 2019: open label, randomised controlled trial, BMJ (Clinical research ed
Tuccori, Convertino, Ferraro, The Impact of the COVID-19 "Infodemic" on Drug-Utilization Behaviors: Implications for Pharmacovigilance
Venkatasubbaiah, Reddy, Satyanarayana, Literaturebased review of the drugs used for the treatment of COVID-19, Curr Med Res Pract
Vijayvargiya, Esquer Garrigos, Castillo Almeida, Gurram, Stevens et al., Treatment Considerations for COVID-19: A Critical Review of the Evidence (or Lack Thereof), Mayo Clinic proceedings
Wu, Li, Shi, Early antiviral treatment contributes to alleviate the severity and improve the prognosis of patients with novel coronavirus disease (COVID-19), J Intern Med
Yavuz, Antiviral treatment of COVID-19. Turk, J Med Sci
DOI record:
{
"DOI": "10.1016/j.intimp.2021.107522",
"ISSN": [
"1567-5769"
],
"URL": "http://dx.doi.org/10.1016/j.intimp.2021.107522",
"alternative-id": [
"S1567576921001582"
],
"article-number": "107522",
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Safety and efficacy of Favipiravir in moderate to severe SARS-CoV-2 pneumonia"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "International Immunopharmacology"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.intimp.2021.107522"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2021 Elsevier B.V. All rights reserved."
}
],
"author": [
{
"affiliation": [],
"family": "Solaymani-Dodaran",
"given": "Masoud",
"sequence": "first"
},
{
"affiliation": [],
"family": "Ghanei",
"given": "Mostafa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bagheri",
"given": "Mehdi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Qazvini",
"given": "Ali",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Vahedi",
"given": "Ensieh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hassan Saadat",
"given": "Seyed",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Amin Setarehdan",
"given": "Seyed",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ansarifar",
"given": "Akram",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Biganeh",
"given": "Hossein",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mohazzab",
"given": "Arash",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Khalili",
"given": "Davood",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hosein Ghazale",
"given": "Amir",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Reza Heidari",
"given": "Mohammad",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Taheri",
"given": "Ali",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Khoramdad",
"given": "Maliheh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mahdi Asadi",
"given": "Mohammad",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nazemieh",
"given": "Masoud",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Varshochi",
"given": "Mojtaba",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Abbasian",
"given": "Samaneh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bakhtiari",
"given": "Ali",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mosaed",
"given": "Reza",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hosseini-shokouh",
"given": "Seyyed-Javad",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Shahrokhi",
"given": "Masoume",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yassin",
"given": "Zeynab",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ali Zohal",
"given": "Mohammad",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Qaraati",
"given": "Maryam",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rastgoo",
"given": "Nafiseh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sami",
"given": "Ramin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Javad Eslami",
"given": "Mohammad",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Asghari",
"given": "Akram",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Namazi",
"given": "Mansoor",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ziaie",
"given": "Shadi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jafari-Moghaddam",
"given": "Raana",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kalantari",
"given": "Saeid",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Memarian",
"given": "Mohammad",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Khodadadi",
"given": "Javad",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hossein Afshari",
"given": "Mohammad",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Momen-Heravi",
"given": "Mansooreh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Behzadseresht",
"given": "Niusha",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Reza Mobayen",
"given": "Ahmad",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mozafari",
"given": "Abolfazl",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Movasaghi",
"given": "Fatemeh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Haddadzadeh Shoushtari",
"given": "Maryam",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Moazen",
"given": "Javad",
"sequence": "additional"
}
],
"container-title": "International Immunopharmacology",
"container-title-short": "International Immunopharmacology",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2021,
3,
12
]
],
"date-time": "2021-03-12T10:23:15Z",
"timestamp": 1615544595000
},
"deposited": {
"date-parts": [
[
2023,
4,
15
]
],
"date-time": "2023-04-15T09:09:37Z",
"timestamp": 1681549777000
},
"funder": [
{
"DOI": "10.13039/501100005849",
"award": [
"IRCT20200318046812N1"
],
"doi-asserted-by": "publisher",
"name": "Baqiyatallah University of Medical Sciences"
},
{
"DOI": "10.13039/100012021",
"award": [
"IRCT20200318046812N1"
],
"doi-asserted-by": "publisher",
"name": "Iran University of Medical Sciences"
}
],
"indexed": {
"date-parts": [
[
2024,
3,
28
]
],
"date-time": "2024-03-28T04:37:57Z",
"timestamp": 1711600677178
},
"is-referenced-by-count": 45,
"issued": {
"date-parts": [
[
2021,
6
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
6,
1
]
],
"date-time": "2021-06-01T00:00:00Z",
"timestamp": 1622505600000
}
},
{
"URL": "https://doi.org/10.15223/policy-017",
"content-version": "stm-asf",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
6,
1
]
],
"date-time": "2021-06-01T00:00:00Z",
"timestamp": 1622505600000
}
},
{
"URL": "https://doi.org/10.15223/policy-037",
"content-version": "stm-asf",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
6,
1
]
],
"date-time": "2021-06-01T00:00:00Z",
"timestamp": 1622505600000
}
},
{
"URL": "https://doi.org/10.15223/policy-012",
"content-version": "stm-asf",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
6,
1
]
],
"date-time": "2021-06-01T00:00:00Z",
"timestamp": 1622505600000
}
},
{
"URL": "https://doi.org/10.15223/policy-029",
"content-version": "stm-asf",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
6,
1
]
],
"date-time": "2021-06-01T00:00:00Z",
"timestamp": 1622505600000
}
},
{
"URL": "https://doi.org/10.15223/policy-004",
"content-version": "stm-asf",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
6,
1
]
],
"date-time": "2021-06-01T00:00:00Z",
"timestamp": 1622505600000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S1567576921001582?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S1567576921001582?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "107522",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2021,
6
]
]
},
"published-print": {
"date-parts": [
[
2021,
6
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1016/j.cmrp.2020.05.013",
"article-title": "Literature-based review of the drugs used for the treatment of COVID-19",
"author": "Venkatasubbaiah",
"doi-asserted-by": "crossref",
"first-page": "100",
"issue": "3",
"journal-title": "Curr Med Res Pract",
"key": "10.1016/j.intimp.2021.107522_b0005",
"volume": "10",
"year": "2020"
},
{
"article-title": "Antiviral treatment of COVID-19. Turk",
"author": "Şimşek Yavuz",
"first-page": "611",
"issue": "SI-1",
"journal-title": "J Med Sci",
"key": "10.1016/j.intimp.2021.107522_b0010",
"volume": "50",
"year": "2020"
},
{
"DOI": "10.1007/s40264-020-00965-w",
"article-title": "The Impact of the COVID-19 “Infodemic” on Drug-Utilization Behaviors: Implications for Pharmacovigilance",
"author": "Tuccori",
"doi-asserted-by": "crossref",
"journal-title": "Drug Safety",
"key": "10.1016/j.intimp.2021.107522_b0015",
"year": "2020"
},
{
"DOI": "10.1128/AAC.46.4.977-981.2002",
"article-title": "In Vitro and In Vivo Activities of Anti-Influenza Virus Compound T-705",
"author": "Furuta",
"doi-asserted-by": "crossref",
"first-page": "977",
"issue": "4",
"journal-title": "Antimicrobial Agents and Chemotherapy",
"key": "10.1016/j.intimp.2021.107522_b0020",
"volume": "46",
"year": "2002"
},
{
"DOI": "10.2183/pjab.93.027",
"article-title": "Favipiravir (T-705), a broad spectrum inhibitor of viral RNA polymerase",
"author": "Furuta",
"doi-asserted-by": "crossref",
"first-page": "449",
"issue": "7",
"journal-title": "Proceedings of the Japan Academy Series B, Physical and biological sciences",
"key": "10.1016/j.intimp.2021.107522_b0025",
"volume": "93",
"year": "2017"
},
{
"DOI": "10.1101/2020.05.15.098731",
"doi-asserted-by": "crossref",
"key": "10.1016/j.intimp.2021.107522_b0030",
"unstructured": "Shannon A, Selisko B, Le N, et al. Favipiravir strikes the SARS-CoV-2 at its Achilles heel, the RNA polymerase. bioRxiv 2020: 2020.05.15.098731."
},
{
"DOI": "10.1002/cpt.1844",
"article-title": "Favipiravir: Pharmacokinetics and Concerns About Clinical Trials for 2019-nCoV Infection",
"author": "Du",
"doi-asserted-by": "crossref",
"journal-title": "Clinical pharmacology and therapeutics",
"key": "10.1016/j.intimp.2021.107522_b0035",
"year": "2020"
},
{
"DOI": "10.1371/journal.pmed.1001967",
"article-title": "Experimental Treatment with Favipiravir for Ebola Virus Disease (the JIKI Trial): A Historically Controlled, Single-Arm Proof-of-Concept Trial in Guinea",
"author": "Sissoko",
"doi-asserted-by": "crossref",
"issue": "3",
"journal-title": "PLoS medicine",
"key": "10.1016/j.intimp.2021.107522_b0040",
"volume": "13",
"year": "2016"
},
{
"article-title": "Pharmacologic Treatments for Coronavirus Disease 2019 (COVID-19): A Review",
"author": "Sanders",
"first-page": "1824",
"issue": "18",
"journal-title": "Jama",
"key": "10.1016/j.intimp.2021.107522_b0045",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1016/j.mayocp.2020.04.027",
"article-title": "Treatment Considerations for COVID-19: A Critical Review of the Evidence (or Lack Thereof)",
"author": "Vijayvargiya",
"doi-asserted-by": "crossref",
"first-page": "1454",
"issue": "7",
"journal-title": "Mayo Clinic proceedings",
"key": "10.1016/j.intimp.2021.107522_b0050",
"volume": "95",
"year": "2020"
},
{
"DOI": "10.1016/j.intimp.2020.107228",
"article-title": "Therapeutic drugs for SARS-CoV-2 treatment: Current state and perspective",
"author": "Bolarin",
"doi-asserted-by": "crossref",
"journal-title": "International Immunopharmacology",
"key": "10.1016/j.intimp.2021.107522_b0055",
"volume": "90",
"year": "2021"
},
{
"DOI": "10.1016/j.intimp.2020.107232",
"article-title": "A comparative analysis for anti-viral drugs: Their efficiency against SARS-CoV-2",
"author": "Kivrak",
"doi-asserted-by": "crossref",
"first-page": "107232-",
"journal-title": "International immunopharmacology",
"key": "10.1016/j.intimp.2021.107522_b0060",
"volume": "90",
"year": "2021"
},
{
"DOI": "10.1186/s40779-020-0233-6",
"article-title": "A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version)",
"author": "Jin",
"doi-asserted-by": "crossref",
"first-page": "4",
"issue": "1",
"journal-title": "Military Medical Research",
"key": "10.1016/j.intimp.2021.107522_b0065",
"volume": "7",
"year": "2020"
},
{
"article-title": "Role of Lopinavir/Ritonavir in the Treatment of Covid-19: A Review of Current Evidence, Guideline Recommendations, and Perspectives. Journal of",
"author": "Meini",
"issue": "7",
"journal-title": "Clinical Medicine",
"key": "10.1016/j.intimp.2021.107522_b0070",
"volume": "9",
"year": "2020"
},
{
"key": "10.1016/j.intimp.2021.107522_b0075",
"unstructured": "Scientific Bureau of National COVID-19 Management Committee. Iranian National Guideline for dignosis and treatment of COVID-19. MOHME, Ministry of Health and Medical Education 2020. p. 13-4."
},
{
"DOI": "10.1056/NEJMoa2001282",
"article-title": "A Trial of Lopinavir-Ritonavir in Adults Hospitalized with Severe Covid-19",
"author": "Cao",
"doi-asserted-by": "crossref",
"first-page": "1787",
"issue": "19",
"journal-title": "The New England journal of medicine",
"key": "10.1016/j.intimp.2021.107522_b0080",
"volume": "382",
"year": "2020"
},
{
"article-title": "Hydroxychloroquine in patients with mainly mild to moderate coronavirus disease 2019: open label, randomised controlled trial",
"author": "Tang",
"journal-title": "BMJ (Clinical research ed)",
"key": "10.1016/j.intimp.2021.107522_b0085",
"volume": "369",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2012410",
"article-title": "Observational Study of Hydroxychloroquine in Hospitalized Patients with Covid-19",
"author": "Geleris",
"doi-asserted-by": "crossref",
"first-page": "2411",
"issue": "25",
"journal-title": "New England Journal of Medicine",
"key": "10.1016/j.intimp.2021.107522_b0090",
"volume": "382",
"year": "2020"
},
{
"author": "Moschini",
"first-page": "1",
"journal-title": "Effects on QT interval of hydroxychloroquine associated with ritonavir/darunavir or azithromycin in patients with SARS-CoV-2 infection.",
"key": "10.1016/j.intimp.2021.107522_b0095",
"year": "2020"
},
{
"DOI": "10.1038/s41392-020-0191-1",
"article-title": "Immune response in COVID-19: addressing a pharmacological challenge by targeting pathways triggered by SARS-CoV-2",
"author": "Catanzaro",
"doi-asserted-by": "crossref",
"first-page": "84-",
"issue": "1",
"journal-title": "Signal Transduct Target Ther",
"key": "10.1016/j.intimp.2021.107522_b0100",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1016/j.healun.2020.03.012",
"article-title": "COVID-19 illness in native and immunosuppressed states: A clinical-therapeutic staging proposal",
"author": "Siddiqi",
"doi-asserted-by": "crossref",
"first-page": "405",
"issue": "5",
"journal-title": "J Heart Lung Transplant",
"key": "10.1016/j.intimp.2021.107522_b0105",
"volume": "39",
"year": "2020"
},
{
"DOI": "10.1111/joim.13063",
"article-title": "Early antiviral treatment contributes to alleviate the severity and improve the prognosis of patients with novel coronavirus disease (COVID-19)",
"author": "Wu",
"doi-asserted-by": "crossref",
"first-page": "128",
"issue": "1",
"journal-title": "J Intern Med",
"key": "10.1016/j.intimp.2021.107522_b0110",
"volume": "288",
"year": "2020"
},
{
"DOI": "10.1183/13993003.00607-2020",
"article-title": "Pathogenesis of COVID-19 from a cell biology perspective",
"author": "Mason",
"doi-asserted-by": "crossref",
"first-page": "2000607",
"issue": "4",
"journal-title": "European Respiratory Journal",
"key": "10.1016/j.intimp.2021.107522_b0115",
"volume": "55",
"year": "2020"
},
{
"DOI": "10.7189/jogh.10.010377",
"article-title": "Can early treatment of patients with risk factors contribute to managing the COVID-19 pandemic?",
"author": "Giammaria",
"doi-asserted-by": "crossref",
"issue": "1",
"journal-title": "Journal of global health",
"key": "10.1016/j.intimp.2021.107522_b0120",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1186/s13054-020-03288-5",
"article-title": "Oral favipiravir for patients with delayed SARS-CoV-2 viral RNA clearance: a case series",
"author": "Fu",
"doi-asserted-by": "crossref",
"first-page": "578-",
"issue": "1",
"journal-title": "Crit Care",
"key": "10.1016/j.intimp.2021.107522_b0125",
"volume": "24",
"year": "2020"
},
{
"DOI": "10.1128/AAC.02017-20",
"doi-asserted-by": "crossref",
"key": "10.1016/j.intimp.2021.107522_b0130",
"unstructured": "McCullough PA. Favipiravir and the Need for Early Ambulatory Treatment of SARS-CoV2 Infection (COVID-19). Antimicrobial Agents and Chemotherapy 2020: AAC.02017-20."
},
{
"article-title": "Efficacy of favipiravir in COVID-19 treatment: a multi-center randomized study",
"author": "Dabbous",
"first-page": "1",
"journal-title": "Arch Virol",
"key": "10.1016/j.intimp.2021.107522_b0135",
"year": "2021"
},
{
"DOI": "10.1128/AAC.01897-20",
"article-title": "A prospective, randomized, open-label trial of early versus late favipiravir in hospitalized patients with COVID-19",
"author": "Doi",
"doi-asserted-by": "crossref",
"journal-title": "Antimicrob Agents Chemother",
"key": "10.1016/j.intimp.2021.107522_b0140",
"year": "2020"
},
{
"DOI": "10.1016/j.eng.2020.03.007",
"doi-asserted-by": "crossref",
"key": "10.1016/j.intimp.2021.107522_b0145",
"unstructured": "Cai Q, Yang M, Liu D, et al. Experimental Treatment with Favipiravir for COVID-19: An Open-Label Control Study. Engineering (Beijing, China) 2020."
},
{
"DOI": "10.1093/cid/ciaa1176",
"doi-asserted-by": "crossref",
"key": "10.1016/j.intimp.2021.107522_b0150",
"unstructured": "Ivashchenko AA, Dmitriev KA, Vostokova NV, et al. AVIFAVIR for Treatment of Patients with Moderate COVID-19: Interim Results of a Phase II/III Multicenter Randomized Clinical Trial. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America 2020."
},
{
"key": "10.1016/j.intimp.2021.107522_b0155",
"unstructured": "Dexamethasone in Hospitalized Patients with Covid-19 — Preliminary Report. New England Journal of Medicine 2020."
}
],
"reference-count": 31,
"references-count": 31,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S1567576921001582"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Pharmacology",
"Immunology",
"Immunology and Allergy"
],
"subtitle": [],
"title": "Safety and efficacy of Favipiravir in moderate to severe SARS-CoV-2 pneumonia",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "95"
}