Comparison of Favipiravir to Hydroxychloroquine Plus Azithromycin in the Treatment of Patients with Non-critical COVID-19: A Single-center, Retrospective, Propensity Score-matched Study
et al., Acta Medica, doi:10.32552/2022.ActaMedica.719, Mar 2022
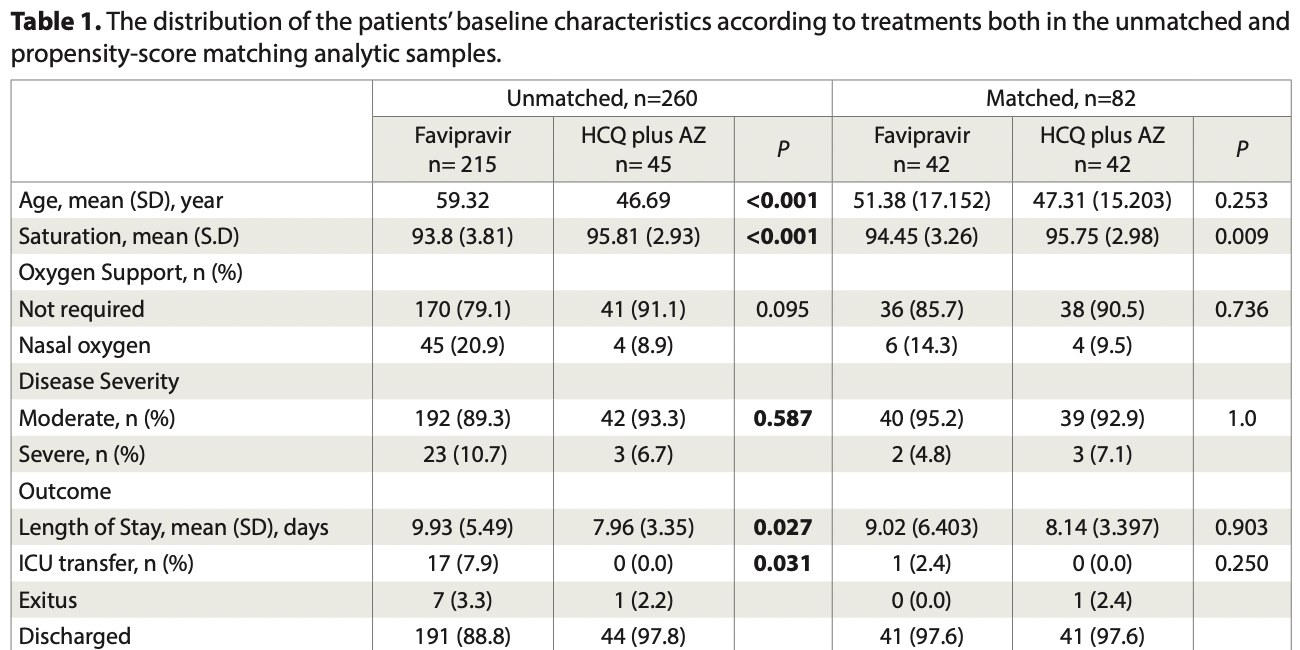
PSM retrospective 260 late stage hospitalized COVID-19 pneumonia patients in Turkey, showing no significant difference between favipiravir and HCQ.
Potential risks of favipiravir include kidney injury1-3, liver injury2-5, cardiovascular events5,6, pulmonary toxicity6,7, and mutagenicity, carcinogenicity, teratogenicity, embryotoxicity, and the creation of dangerous variants8-14.
Study covers HCQ and favipiravir.
|
risk of death, 66.7% lower, RR 0.33, p = 1.00, treatment 0 of 42 (0.0%), control 1 of 42 (2.4%), NNT 42, relative risk is not 0 because of continuity correction due to zero events (with reciprocal of the contrasting arm).
|
|
risk of ICU admission, 200.0% higher, RR 3.00, p = 1.00, treatment 1 of 42 (2.4%), control 0 of 42 (0.0%), continuity correction due to zero event (with reciprocal of the contrasting arm).
|
|
hospitalization time, 10.8% higher, relative time 1.11, p = 0.90, treatment 42, control 42.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Abdulaziz et al., Clinical Features and Prognosis of Acute Kidney Injury in Hospital-Admitted Patients with COVID-19 in Egypt: A Single-Center Experience, Mansoura Medical Journal, doi:10.58775/2735-3990.1433.
2.
Ülger et al., Experimental evaluation of favipiravir (T-705)-induced liver and kidney toxicity in rats, Food and Chemical Toxicology, doi:10.1016/j.fct.2025.115472.
3.
El-Fetouh et al., Experimental Studies on Some Drugs Used in Covid-19 Treatment (Favipiravir and Dexamethasone) in Albino Rats, Journal of Advanced Veterinary Research, 13:10, www.advetresearch.com/index.php/AVR/article/view/1635.
4.
Almutairi et al., Liver Injury in Favipiravir-Treated COVID-19 Patients: Retrospective Single-Center Cohort Study, Tropical Medicine and Infectious Disease, doi:10.3390/tropicalmed8020129.
5.
Siby et al., Temporal Trends in Serious Adverse Events Associated with Oral Antivirals During the COVID-19 Pandemic: Insights from the FAERS Database (2020–2023), Open Forum Infectious Diseases, doi:10.1093/ofid/ofaf695.1825.
6.
Ozhan et al., Evaluation of the cardiopulmonary effects of repurposed COVID-19 therapeutics in healthy rats, Scientific Reports, doi:10.1038/s41598-025-31048-4.
7.
Ülger (B) et al., Evaluation of the effects of favipiravir (T-705) on the lung tissue of healty rats: An experimental study, Food and Chemical Toxicology, doi:10.1016/j.fct.2025.115235.
8.
Zhirnov et al., Favipiravir: the hidden threat of mutagenic action, Journal of microbiology, epidemiology and immunobiology, doi:10.36233/0372-9311-114.
9.
Waters et al., Human genetic risk of treatment with antiviral nucleoside analog drugs that induce lethal mutagenesis: the special case of molnupiravir, Environmental and Molecular Mutagenesis, doi:10.1002/em.22471.
10.
Hadj Hassine et al., Lethal Mutagenesis of RNA Viruses and Approved Drugs with Antiviral Mutagenic Activity, Viruses, doi:10.3390/v14040841.
11.
Shum, C., An investigational study into the drug-associated mutational signature in SARS-CoV-2 viruses, The University of Hong Kong, PhD Thesis, hub.hku.hk/handle/10722/344396.
12.
Shiraki et al., Convenient screening of the reproductive toxicity of favipiravir and antiviral drugs in Caenorhabditis elegans, Heliyon, doi:10.1016/j.heliyon.2024.e35331.
Uyaroğlu et al., 17 Mar 2022, retrospective, propensity score matching, Turkey, peer-reviewed, 6 authors, study period 20 March, 2020 - 30 September, 2020, this trial compares with another treatment - results may be better when compared to placebo.
Contact: oguzuyaroglu@hotmail.com.
Comparison of Favipiravir to Hydroxychloroquine Plus Azithromycin in the Treatment of Patients with Non-critical COVID-19: A Singlecenter, Retrospective, Propensity Score-matched Study
In this study, we compared the clinical outcomes and effects of the treatments on laboratory parameters between patients who were treated with favipiravir (FAV) or hydroxychloroquine plus azithromycin (HCQ/AZ) for COVID-19 pneumonia in non-Intensive Care Unit (non-ICU) patients. Methods: We collected data of 260 moderate or severe COVID-19 patients hospitalized in COVID-19 wards between March 20, 2020, and September 30, 2020 retrospectively. We used propensity score matching to evaluate treatment effect on laboratory parameters of COVID-19 infection. Results: We compared 42 patients using FAV and 42 HCQ/AZ after propensity score matching. While there were statistical differences between the therapy groups in terms of transfer to ICU and/or exitus before matching (p=0.031), this was not significant after propensity analysis (p=0.250). Patients treated with FAV stayed in the hospital nearly one more day than HCQ/AZ group but the difference was not statistically significant (9.02 days vs 8.14 days, p=0.903). The levels of AST,ALT, and LDH increased at discharge in both groups, especially in the FAV group. Conclusions: FAV is not superior to HCQ/AZ in the treatment of COVID-19 infection in hospitalized patients with pneumonia.
Author contribution Study conception and design: ÖU, OAU, and NÇB; data collection: OAU, MÇS, and GTD; analysis and interpretation of results: OAU, MÇS, GTD, NÇB, SK, ÖU; draft manuscript preparation OAU, and ÖU. All authors reviewed the results and approved the final version of the manuscript.
Ethical approval The study was approved by the Hacettepe University Non-interventional Clinical Research Ethics Board (Protocol no. GO 20/353/31/03/2020).
Funding The authors declare that the study received no funding.
Conflict of interest The authors declare that there is no conflict of interest.
References
Bouazza, Treluyer, Foissac, Favipiravir for children with Ebola, Lancet
Cai, Yang, Liu, Experimental treatment with favipiravir for COVID-19: An open-label control study, Engineering
Chen, Zhang, Huang, Favipiravir versus arbidol for COVID-19: a randomized clinical trial
Dabbous, Abd-Elsalam, El-Sayed, Efficacy of favipiravir in COVID-19 treatment: a multi-center randomized study, Archives of Virology
Dabbous, El-Sayed, Assal, Safety and efficacy of favipiravir versus hydroxychloroquine in management of COVID-19: A randomised controlled trial, Scientific Reports
Doi, Hibino, Hase, A prospective, randomized, open-label trial of early versus late favipiravir therapy in hospitalized patients with COVID-19, Antimicrobial agents and chemotherapy
Doi, Ikeda, Hayase, Nafa mostat mesylate treatment in combination with favipiravir for patients critically ill with Covid-19: a case series, Crital Care
Fu, Cao, Zhao, Oral favipiravir for patients with delayed SARS-CoV-2 viral RNA clearance: a case series, Crital Care
Furuta, Gowen, Takahashi, Favipiravir (T-705), a novel viral RNA polymerase inhibitor, Antiviral Research
Gautret, Lagier, Parola, Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial, International journal of antimicrobial agents
Geleris, Sun, Platt, Observational study of hydroxychloroquine in hospitalized patients with Covid-19, New England Journal of Medicine
Inkaya, Kara, Başaran, Pretreatment serum uric acid level is not a surrogate marker for the outcome of favipiravir treatment in COVID-19 patients, Turk J Med Sci
Ivashchenko, Dmitriev, Vostokova, AVIFAVIR for treatment of patients with moderate COVID-19: Interim results of a pha se II/III multicenter randomized clinical trial, Clinical Infectious Disease
Joshi, Parkar, Ansari, Role of favipiravir in the treatment of COVID-19, International Journal of Infectious Diseases
Kocayiğit, Süner, Tomak, Observational study of the effects of Favipiravir vs Lopinavir/Ritonavir on clinical outcomes in critically Ill patients with COVID-19, Journal of Clinical Pharmacy and Therapeutics
Li, Clercq, Therapeutic options for the 2019 novel coronavirus (2019-nCoV), Nature Reviews Drug Discovery
Lou, Liu, Yao, Clinical outcomes and plasma concentrations of Baloxavir Marboxil and Favipiravir in COVID-19 patients: An exploratory randomized, controlled trial, European Journal of Pharmaceutical Sciences
Piszczatoski, Powell, Emergency authorization of chloroquine and hydroxychloroquine for treatment of COVID-19, Annals of Pharmacotherapy
Recovery Collaborative, Effect of hydroxychloroquine in hospitalized patients with Covid-19, New England Journal of Medicine
Simmering, Polgreen, Polgreen, Teske, Comellas et al., The Cardiovascular Effects of Treatment with Hydroxychloroquine and Azithromycin, Pharmacotherapy, doi:10.1002/phar.2445
Tang, Cao, Han, Hydroxychloroquine in patients with mainly mild to moderate coronavirus disease 2019: open label, randomised controlled trial
Victoria, Pepperrell, Hill, A review of the safety of favipiravir-a potential treatment in the COVID-19 pandemic?, Journal of virus eradication
Wang, Cao, Zhang, Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro, Cell Research
Yamamura, Matsuura, Nakagawa, Effect of favipiravir and an anti-inflammatory strategy for COVID-19, Critical Care
Yuki, Sadako, Kazuhiro, Evaluation of risk factors for uric acid elevation in COVID-19 patients treated with favipiravir, Diagn. Microbiol. Infect. Dis
Çalık Başaran, Uyaroğlu, Dizman, Outcome of noncritical COVID-19 patients with early hospitalization and early antiviral treatment outside the ICU, Turk J Med Sci
Çilingir, Sunnetcioglu, Yildiz, What Is The Case of More Accessible Treatment Options in COVID 19: Comparison of Hydroxychloroquine and Favipiravir Based on Laboratory Values, Eastern Journal of Medicine
Özlüşen, Kozan, Akcan, Effectiveness of favipiravir in COVID-19: a live systematic review, Eur J Clin Microbiol Infect Dis
DOI record:
{
"DOI": "10.32552/2022.actamedica.719",
"ISSN": [
"2147-9488"
],
"URL": "http://dx.doi.org/10.32552/2022.ActaMedica.719",
"abstract": "<jats:p>Objectives: In this study, we compared the clinical outcomes and effects of the treatments on laboratory parameters between patients who were treated with favipiravir (FAV) or hydroxychloroquine plus azithromycin (HCQ/AZ) for COVID-19 pneumonia in non-Intensive Care Unit (non-ICU) patients.
\nMethods: We collected data of 260 moderate or severe COVID-19 patients hospitalized in COVID-19 wards between March 20, 2020, and September 30, 2020 retrospectively. We used propensity score matching to evaluate treatment effect on laboratory parameters of COVID-19 infection.
\nResults: We compared 42 patients using FAV and 42 HCQ/AZ after propensity score matching. While there were statistical differences between the therapy groups in terms of transfer to ICU and/or exitus before matching (p=0.031), this was not significant after propensity analysis (p=0.250). Patients treated with FAV stayed in the hospital nearly one more day than HCQ/AZ group but the difference was not statistically significant (9.02 days vs 8.14 days, p=0.903). The levels of AST,ALT, and LDH increased at discharge in both groups, especially in the FAV group.
\nConclusions: FAV is not superior to HCQ/AZ in the treatment of COVID-19 infection in hospitalized patients with pneumonia.</jats:p>",
"author": [
{
"ORCID": "http://orcid.org/0000-0003-0440-2026",
"affiliation": [],
"authenticated-orcid": false,
"family": "Uyaroğlu",
"given": "Oğuz Abdullah",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0001-6529-5282",
"affiliation": [],
"authenticated-orcid": false,
"family": "Sönmezer",
"given": "Meliha Çağla",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0001-8195-3345",
"affiliation": [],
"authenticated-orcid": false,
"family": "Telli Dizman",
"given": "Gülçin",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-1290-6905",
"affiliation": [],
"authenticated-orcid": false,
"family": "Çalık Başaran",
"given": "Nursel",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-8692-7266",
"affiliation": [],
"authenticated-orcid": false,
"family": "Karahan",
"given": "Sevilay",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0003-4721-0139",
"affiliation": [],
"authenticated-orcid": false,
"family": "Uzun",
"given": "Ömrüm",
"sequence": "first"
}
],
"container-title": "Acta Medica",
"container-title-short": "Acta Medica",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
3,
26
]
],
"date-time": "2022-03-26T13:55:42Z",
"timestamp": 1648302942000
},
"deposited": {
"date-parts": [
[
2022,
3,
26
]
],
"date-time": "2022-03-26T13:55:47Z",
"timestamp": 1648302947000
},
"indexed": {
"date-parts": [
[
2022,
4,
1
]
],
"date-time": "2022-04-01T05:03:31Z",
"timestamp": 1648789411476
},
"is-referenced-by-count": 0,
"issue": "1",
"issued": {
"date-parts": [
[
2022,
3,
17
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2022,
3,
26
]
]
}
},
"license": [
{
"URL": "http://creativecommons.org/licenses/by/4.0",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
3,
17
]
],
"date-time": "2022-03-17T00:00:00Z",
"timestamp": 1647475200000
}
}
],
"link": [
{
"URL": "https://actamedica.org/index.php/actamedica/article/download/719/558",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://actamedica.org/index.php/actamedica/article/download/719/558",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "17016",
"original-title": [],
"page": "73-82",
"prefix": "10.32552",
"published": {
"date-parts": [
[
2022,
3,
17
]
]
},
"published-online": {
"date-parts": [
[
2022,
3,
17
]
]
},
"publisher": "Hacettepe University - Medical School",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://actamedica.org/index.php/actamedica/article/view/719"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subtitle": [],
"title": "Comparison of Favipiravir to Hydroxychloroquine Plus Azithromycin in the Treatment of Patients with Non-critical COVID-19: A Single-center, Retrospective, Propensity Score-matched Study",
"type": "journal-article",
"volume": "53"
}
uyaroglu