Randomized Controlled Open Label Trial on the Use of Favipiravir Combined with Inhaled Interferon beta-1b in Hospitalized Patients with Moderate to Severe COVID-19 Pneumonia
et al., International Journal of Infectious Diseases, doi:10.1016/j.ijid.2020.11.008, Nov 2020
Small 89 patient RCT comparing favipiravir and inhaled interferon with HCQ for moderate to severe COVID-19 pneumonia, not finding significant differences. There was no control group.
Potential risks of favipiravir include kidney injury1-3, liver injury2-5, cardiovascular events5,6, pulmonary toxicity6,7, and mutagenicity, carcinogenicity, teratogenicity, embryotoxicity, and the creation of dangerous variants8-14.
This study is excluded in the after exclusion results of meta-analysis:
study compares against another treatment showing significant efficacy.
Study covers HCQ and favipiravir.
|
risk of death, 14.8% lower, RR 0.85, p = 1.00, treatment 5 of 44 (11.4%), control 6 of 45 (13.3%), NNT 51, day 14.
|
|
risk of ICU admission, 2.3% higher, RR 1.02, p = 1.00, treatment 8 of 44 (18.2%), control 8 of 45 (17.8%).
|
|
risk of no recovery, 9.6% higher, RR 1.10, p = 0.82, treatment 15 of 44 (34.1%), control 14 of 45 (31.1%).
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Abdulaziz et al., Clinical Features and Prognosis of Acute Kidney Injury in Hospital-Admitted Patients with COVID-19 in Egypt: A Single-Center Experience, Mansoura Medical Journal, doi:10.58775/2735-3990.1433.
2.
Ülger et al., Experimental evaluation of favipiravir (T-705)-induced liver and kidney toxicity in rats, Food and Chemical Toxicology, doi:10.1016/j.fct.2025.115472.
3.
El-Fetouh et al., Experimental Studies on Some Drugs Used in Covid-19 Treatment (Favipiravir and Dexamethasone) in Albino Rats, Journal of Advanced Veterinary Research, 13:10, www.advetresearch.com/index.php/AVR/article/view/1635.
4.
Almutairi et al., Liver Injury in Favipiravir-Treated COVID-19 Patients: Retrospective Single-Center Cohort Study, Tropical Medicine and Infectious Disease, doi:10.3390/tropicalmed8020129.
5.
Siby et al., Temporal Trends in Serious Adverse Events Associated with Oral Antivirals During the COVID-19 Pandemic: Insights from the FAERS Database (2020–2023), Open Forum Infectious Diseases, doi:10.1093/ofid/ofaf695.1825.
6.
Ozhan et al., Evaluation of the cardiopulmonary effects of repurposed COVID-19 therapeutics in healthy rats, Scientific Reports, doi:10.1038/s41598-025-31048-4.
7.
Ülger (B) et al., Evaluation of the effects of favipiravir (T-705) on the lung tissue of healty rats: An experimental study, Food and Chemical Toxicology, doi:10.1016/j.fct.2025.115235.
8.
Zhirnov et al., Favipiravir: the hidden threat of mutagenic action, Journal of microbiology, epidemiology and immunobiology, doi:10.36233/0372-9311-114.
9.
Waters et al., Human genetic risk of treatment with antiviral nucleoside analog drugs that induce lethal mutagenesis: the special case of molnupiravir, Environmental and Molecular Mutagenesis, doi:10.1002/em.22471.
10.
Hadj Hassine et al., Lethal Mutagenesis of RNA Viruses and Approved Drugs with Antiviral Mutagenic Activity, Viruses, doi:10.3390/v14040841.
11.
Shum, C., An investigational study into the drug-associated mutational signature in SARS-CoV-2 viruses, The University of Hong Kong, PhD Thesis, hub.hku.hk/handle/10722/344396.
12.
Shiraki et al., Convenient screening of the reproductive toxicity of favipiravir and antiviral drugs in Caenorhabditis elegans, Heliyon, doi:10.1016/j.heliyon.2024.e35331.
Khamis et al., 9 Nov 2020, Randomized Controlled Trial, Oman, peer-reviewed, 11 authors, study period 22 June, 2020 - 13 August, 2020, this trial compares with another treatment - results may be better when compared to placebo, this trial uses multiple treatments in the treatment arm (combined with interferon beta-1b) - results of individual treatments may vary.
Randomized controlled open label trial on the use of favipiravir combined with inhaled interferon beta-1b in hospitalized patients with moderate to severe COVID-19 pneumonia
International Journal of Infectious Diseases, doi:10.1016/j.ijid.2020.11.008
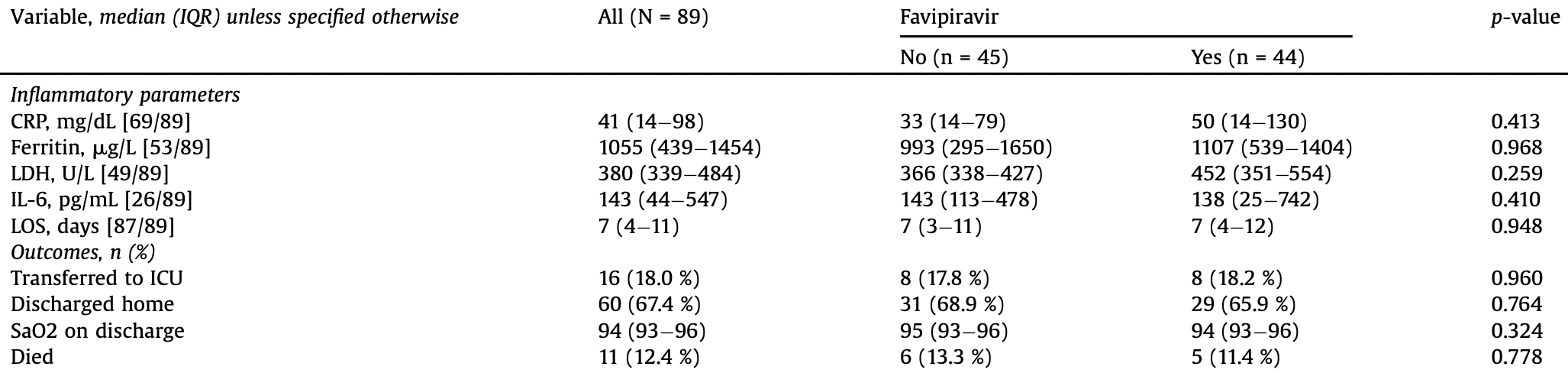
To evaluate the therapeutic effectiveness of favipiravir combined with inhaled interferon beta-1b in adult patients hospitalized with moderate to severe COVID-19 pneumonia. Methods: A randomized, open-label controlled trial of oral favipiravir in adults hospitalized with moderate to severe COVID-19 pneumonia from June 22nd 2020 to August 13th 2020 was conducted. Patients were randomly assigned to receive either a combination of favipiravir with interferon beta-1b by inhalation aerosol or hydroxychloroquine (HCQ). The outcome endpoints included improvement in inflammatory markers, lower length of hospital stay (LOS), discharges and lower overall 14-day mortality. Results: A total of 89 patients underwent randomization with 49% (n = 44) assigned to favipiravir and 51% (n = 45) assigned HCQ. The overall mean age was 55 AE 14 years and 58% (n = 52) were males. There were no significant differences in the inflammatory biomarkers at hospital discharge between the two groups; C-reactive protein (p = 0.413), ferritin (p = 0.968), lactate dehydrogenase (p = 0.259) and interleukin 6 (p = 0.410). There were also no significant differences between the two groups with regards to the overall LOS (7 vs 7 days; p = 0.948), transfers to the ICU (18.2% vs 17.8%; p = 0.960), discharges (65.9% vs 68.9%; p = 0.764) and overall mortality (11.4% vs 13.3%; p = 0.778). Conclusions: No differences in clinical outcomes were found between favipiravir plus inhaled interferon beta-1b and hydroxychloroquine in adults hospitalized with moderate to severe COVID-19 pneumonia.
Conflicts of interest The authors have no conflicts of interest to declare.
References
Agrawal, Raju, Udwadia, Favipiravir: a new and emerging antiviral option in COVID-19, Med J Armed Forces India
Cai, Yang, Liu, Chen, Shu et al., Experimental Treatment with Favipiravir for COVID-19: an Open-Label Control Study
Doi, Ikeda, Hayase, Moriya, Morimura et al., Study Group. Nafamostat mesylate treatment in combination with favipiravir for patients critically ill with Covid-19: a case series, Crit Care
Dong, Hu, Gao, Discovering drugs to treat coronavirus disease 2019 (COVID-19), Drug Discov Ther
Fang, Wang, Advanced researches on the inhibition of influenza virus by Favipiravir and Baloxavir, Biosafety Health
Faryal, Badria, Ibrahim, Ahmed, Salah, Epidemiology of COVID-19 infection in Oman: analysis of the first 1304 cases, Oman Med J
Freedman, Selchen, Arnold, Prat, Banwell et al., Treatment optimization in MS: Canadian MS Working Group updated recommendations, Can J Neurol Sci
Fu, Liu, Xia, Li, Song et al., A clinical pilot study on the safety and efficacy of aerosol inhalation treatment of IFN-k plus TFF2 in patients with moderate COVID-19, E Clin Med
Furuta, Gowen, Takahashi, Shiraki, Smee et al., Favipiravir (T-705), a novel viral RNA polymerase inhibitor, Antiviral Res
Geleris, Sun, Platt, Zucker, Baldwin et al., Observational study on hydroxychloroquine in hospitalized patients with COVID-19, N Engl J Med, doi:10.1056/NEJMoa2012410
Gonçalves, Bertrand, Ke, Commets, De Lamballerie et al., Timing of Antiviral Treatment Initiation is Critical to Reduce SARS-CoV-2 Viral, CPT Pharmacometrics Syst Pharmacol
Hung, Lung, Tso, Liu, Chung et al., Triple combination of interferon beta-1b, lopinavir-ritonavir, and ribavirin in the treatment of patients admitted to hospital with COVID-19: an open-label, randomised, phase 2 trial, Lancet
Hurwitz, Jeffery, Arnason, Bigley, Coyle et al., Tolerability and safety profile of 12-to 28-week treatment with interferon beta-1b 250 and 500 microg QOD in patients with relapsing-remitting multiple sclerosis: a multicenter, randomized, double-blind, parallel-group pilot study, Clin Ther
Kaptein, Jacobs, Langendries, Seldeslachts, Horst et al., Favipiravir at high doses has potent antiviral activity in SARS-CoV-2-infected hamsters, whereas hydroxychloroquine lacks activity, Proct Natl Acad Sci
Khamis, Al Naabi, Lawati, None, International Journal of Infectious Diseases
Khamis, Al Naabi, Lawati, None, International Journal of Infectious Diseases
Kumari, Rawat, Saha, Pipeline Pharmacological Therapies in Clinical Trial for COVID-19 Pandemic: a Recent Update, Curr Pharmacol Rep
Lampl, Nagl, Arnason, Comi, Connor et al., Efficacy and safety of interferon beta-1b sc in older RRMS patients-a posthoc analysis of the BEYOND study, J Neurol
Lee, Hsueh, Emerging threats from zoonotic coronaviruses-from SARS and MERS to 2019-nCoV, J Microbiol Immunol Infect
Lokugamage, Hage, De Vries, Valero-Jimenez, Schindewolf et al., Type I interferon susceptibility distinguishes SARS-CoV-2 from SARS-CoV, J Virol, doi:10.1128/JVI.01410-20
Lu, Drug treatment options for the 2019-new coronavirus (2019-nCoV), Biosci Trends
Madelain, Nguyen, Olivo, De Lamballerie, Guedj et al., Ebola Virus Infection: Review of the Pharmacokinetic and Pharmacodynamic Properties of Drugs Considered for Testing in Human Efficacy Trials, Clin Pharmacokinet
Madelain, Oestereich, Graw, Nguyen, De Lamballerie et al., Ebola virus dynamics in mice treated with favipiravir, Antiviral Res
Malvy, Taburet, De Lamballerie, Mentre, Extramiana, The safety profile of favipiravir should not be the first argument to suspend its evaluation in viral hemorrhagic fevers, PLoS Negl Trop Dis
Mdvi, Phase 3 efficacy and safety study of favipiravir for treatment of uncomplicated influenza in adults
Mentré, Taburet, Guedj, Anglaret, Keita et al., Dose regimen of favipiravir for Ebola virus disease, Lancet Infect Dis
Moriguchi, Sato, Treatment of SARS with human interferons, Lancet, doi:10.1016/S0140-6736(03)14484-4
Nguyen, Guedj, Anglaret, Laouenan, Madelain et al., Favipiravir pharmacokinetics in Ebola-Infected patients of the JIKI trial reveals concentrations lower than targeted, PLoS Negl Trop Dis
Oestereich, Lüdtke, Wurr, Rieger, Muñoz-Fontela et al., Successful treatment of advanced Ebola virus infection with T-705 (favipiravir) in a small animal model, Antiviral Res
Pilkington, Pepperrell, Hill, A review of the safety of favipiravir -a potential treatment in the COVID-19 pandemic?, J Virus Erad
Sallard, Lescure, Yazdanpanah, Mentre, Peiffer-Smadja, Type 1 interferons as a potential treatment against COVID-19, Antiviral Res
Shalhoub, Interferon beta-1b for COVID-19, Lancet
Shiraki, Daikoku, Favipiravir, an anti-influenza drug against life-threatening RNA virus infections, Pharmacol Ther
Sissoko, Laouenan, Folkesson, Lebing, Beavogui et al., Experimental Treatment with Favipiravir for Ebola Virus Disease (the JIKI Trial): A Historically Controlled, Single-Arm Proof-of-Concept Trial in Guinea, PLoS Med
Smith, Dodds, Bentley, Yeo, Rayner, Dosing will be a key success factor in repurposing antivirals for COVID-19, Br J Clin Pharmacol, doi:10.1111/bcp.14314
Tang, Cao, Han, Wang, Chen et al., Hydroxychloroquine in patients mainly with mild to moderate COVID-19: an open-label, randomised, controlled trial, BMJ, doi:10.1136/bmj.m1849
DOI record:
{
"DOI": "10.1016/j.ijid.2020.11.008",
"ISSN": [
"1201-9712"
],
"URL": "http://dx.doi.org/10.1016/j.ijid.2020.11.008",
"alternative-id": [
"S1201971220323195"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Randomized controlled open label trial on the use of favipiravir combined with inhaled interferon beta-1b in hospitalized patients with moderate to severe COVID-19 pneumonia"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "International Journal of Infectious Diseases"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.ijid.2020.11.008"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2020 The Authors. Published by Elsevier Ltd on behalf of International Society for Infectious Diseases."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-5107-921X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Khamis",
"given": "Faryal",
"sequence": "first"
},
{
"affiliation": [],
"family": "Al Naabi",
"given": "Hanan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Al Lawati",
"given": "Adil",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ambusaidi",
"given": "Zaiyana",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Al Sharji",
"given": "Mariam",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Al Barwani",
"given": "Umkulthum",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pandak",
"given": "Nenad",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Al Balushi",
"given": "Zakariya",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Al Bahrani",
"given": "Maher",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Al Salmi",
"given": "Issa",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3626-4230",
"affiliation": [],
"authenticated-orcid": false,
"family": "Al-Zakwani",
"given": "Ibrahim",
"sequence": "additional"
}
],
"container-title": [
"International Journal of Infectious Diseases"
],
"content-domain": {
"crossmark-restriction": true,
"domain": [
"ijidonline.com",
"clinicalkey.jp",
"clinicalkey.com",
"clinicalkey.es",
"clinicalkey.fr",
"clinicalkey.com.au",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2020,
11,
9
]
],
"date-time": "2020-11-09T18:08:21Z",
"timestamp": 1604945301000
},
"deposited": {
"date-parts": [
[
2021,
4,
21
]
],
"date-time": "2021-04-21T21:32:08Z",
"timestamp": 1619040728000
},
"indexed": {
"date-parts": [
[
2022,
1,
10
]
],
"date-time": "2022-01-10T12:28:10Z",
"timestamp": 1641817690526
},
"is-referenced-by-count": 29,
"issn-type": [
{
"type": "print",
"value": "1201-9712"
}
],
"issued": {
"date-parts": [
[
2021,
1
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
1,
1
]
],
"date-time": "2021-01-01T00:00:00Z",
"timestamp": 1609459200000
}
},
{
"URL": "http://creativecommons.org/licenses/by-nc-nd/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2020,
11,
4
]
],
"date-time": "2020-11-04T00:00:00Z",
"timestamp": 1604448000000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S1201971220323195?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S1201971220323195?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "538-543",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2021,
1
]
]
},
"published-print": {
"date-parts": [
[
2021,
1
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1016/j.mjafi.2020.08.004",
"article-title": "Favipiravir: a new and emerging antiviral option in COVID-19",
"author": "Agrawal",
"doi-asserted-by": "crossref",
"journal-title": "Med J Armed Forces India",
"key": "10.1016/j.ijid.2020.11.008_bib0005",
"year": "2020"
},
{
"article-title": "Experimental Treatment with Favipiravir for COVID-19: an Open-Label Control Study [published online ahead of print, 2020 Mar 18]",
"author": "Cai",
"journal-title": "Engineering (Beijing)",
"key": "10.1016/j.ijid.2020.11.008_bib0010",
"year": "2020"
},
{
"DOI": "10.1186/s13054-020-03078-z",
"article-title": "COVID-UTH Study Group. Nafamostat mesylate treatment in combination with favipiravir for patients critically ill with Covid-19: a case series",
"author": "Doi",
"doi-asserted-by": "crossref",
"first-page": "392",
"issue": "1",
"journal-title": "Crit Care",
"key": "10.1016/j.ijid.2020.11.008_bib0015",
"volume": "24",
"year": "2020"
},
{
"DOI": "10.5582/ddt.2020.01012",
"article-title": "Discovering drugs to treat coronavirus disease 2019 (COVID-19)",
"author": "Dong",
"doi-asserted-by": "crossref",
"first-page": "58",
"issue": "1",
"journal-title": "Drug Discov Ther",
"key": "10.1016/j.ijid.2020.11.008_bib0020",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1016/j.bsheal.2020.04.004",
"article-title": "Advanced researches on the inhibition of influenza virus by Favipiravir and Baloxavir",
"author": "Fang",
"doi-asserted-by": "crossref",
"first-page": "64",
"issue": "2",
"journal-title": "Biosafety Health",
"key": "10.1016/j.ijid.2020.11.008_bib0025",
"volume": "2",
"year": "2020"
},
{
"DOI": "10.1017/S0317167100014244",
"article-title": "Treatment optimization in MS: Canadian MS Working Group updated recommendations",
"author": "Freedman",
"doi-asserted-by": "crossref",
"first-page": "307",
"issue": "3",
"journal-title": "Can J Neurol Sci",
"key": "10.1016/j.ijid.2020.11.008_bib0030",
"volume": "40",
"year": "2013"
},
{
"article-title": "A clinical pilot study on the safety and efficacy of aerosol inhalation treatment of IFN-κ plus TFF2 in patients with moderate COVID-19",
"author": "Fu",
"journal-title": "E Clin Med",
"key": "10.1016/j.ijid.2020.11.008_bib0035",
"volume": "25",
"year": "2020"
},
{
"DOI": "10.1016/j.antiviral.2013.09.015",
"article-title": "Favipiravir (T-705), a novel viral RNA polymerase inhibitor",
"author": "Furuta",
"doi-asserted-by": "crossref",
"first-page": "446",
"issue": "2",
"journal-title": "Antiviral Res",
"key": "10.1016/j.ijid.2020.11.008_bib0040",
"volume": "100",
"year": "2013"
},
{
"DOI": "10.1056/NEJMoa2012410",
"article-title": "Observational study on hydroxychloroquine in hospitalized patients with COVID-19",
"author": "Geleris",
"doi-asserted-by": "crossref",
"first-page": "2411",
"journal-title": "N Engl J Med",
"key": "10.1016/j.ijid.2020.11.008_bib0045",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1002/psp4.12543",
"article-title": "Timing of Antiviral Treatment Initiation is Critical to Reduce SARS-CoV-2 Viral",
"author": "Gonçalves",
"doi-asserted-by": "crossref",
"first-page": "509",
"issue": "9",
"journal-title": "CPT Pharmacometrics Syst Pharmacol",
"key": "10.1016/j.ijid.2020.11.008_bib0050",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)31042-4",
"article-title": "Triple combination of interferon beta-1b, lopinavir-ritonavir, and ribavirin in the treatment of patients admitted to hospital with COVID-19: an open-label, randomised, phase 2 trial",
"author": "Hung",
"doi-asserted-by": "crossref",
"first-page": "1695",
"issue": "10238",
"journal-title": "Lancet",
"key": "10.1016/j.ijid.2020.11.008_bib0055",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1016/j.clinthera.2008.06.013",
"article-title": "Tolerability and safety profile of 12- to 28-week treatment with interferon beta-1b 250 and 500 microg QOD in patients with relapsing-remitting multiple sclerosis: a multicenter, randomized, double-blind, parallel-group pilot study",
"author": "Hurwitz",
"doi-asserted-by": "crossref",
"first-page": "1102",
"issue": "6",
"journal-title": "Clin Ther",
"key": "10.1016/j.ijid.2020.11.008_bib0060",
"volume": "30",
"year": "2008"
},
{
"DOI": "10.1073/pnas.2014441117",
"article-title": "Favipiravir at high doses has potent antiviral activity in SARS-CoV-2-infected hamsters, whereas hydroxychloroquine lacks activity",
"author": "Kaptein",
"doi-asserted-by": "crossref",
"first-page": "26955",
"issue": "43",
"journal-title": "Proct Natl Acad Sci USA",
"key": "10.1016/j.ijid.2020.11.008_bib0065",
"volume": "117",
"year": "2020"
},
{
"DOI": "10.5001/omj.2020.60",
"article-title": "Epidemiology of COVID-19 infection in Oman: analysis of the first 1304 cases",
"author": "Khamis",
"doi-asserted-by": "crossref",
"first-page": "141",
"issue": "3",
"journal-title": "Oman Med J",
"key": "10.1016/j.ijid.2020.11.008_bib0070",
"volume": "35",
"year": "2020"
},
{
"article-title": "Pipeline Pharmacological Therapies in Clinical Trial for COVID-19 Pandemic: a Recent Update",
"author": "Kumari",
"first-page": "1",
"journal-title": "Curr Pharmacol Rep",
"key": "10.1016/j.ijid.2020.11.008_bib0075",
"year": "2020"
},
{
"DOI": "10.1007/s00415-013-6888-0",
"article-title": "Efficacy and safety of interferon beta-1b sc in older RRMS patients--a posthoc analysis of the BEYOND study",
"author": "Lampl",
"doi-asserted-by": "crossref",
"first-page": "1838",
"issue": "7",
"journal-title": "J Neurol",
"key": "10.1016/j.ijid.2020.11.008_bib0080",
"volume": "260",
"year": "2013"
},
{
"DOI": "10.1016/j.jmii.2020.02.001",
"article-title": "Emerging threats from zoonotic coronaviruses-from SARS and MERS to 2019-nCoV",
"author": "Lee",
"doi-asserted-by": "crossref",
"first-page": "365",
"issue": "3",
"journal-title": "J Microbiol Immunol Infect",
"key": "10.1016/j.ijid.2020.11.008_bib0085",
"volume": "53",
"year": "2020"
},
{
"DOI": "10.1128/JVI.01410-20",
"article-title": "Type I interferon susceptibility distinguishes SARS-CoV-2 from SARS-CoV",
"author": "Lokugamage",
"doi-asserted-by": "crossref",
"journal-title": "J Virol",
"key": "10.1016/j.ijid.2020.11.008_bib0090",
"year": "2020"
},
{
"DOI": "10.5582/bst.2020.01020",
"article-title": "Drug treatment options for the 2019-new coronavirus (2019-nCoV)",
"author": "Lu",
"doi-asserted-by": "crossref",
"first-page": "69",
"issue": "1",
"journal-title": "Biosci Trends",
"key": "10.1016/j.ijid.2020.11.008_bib0095",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1007/s40262-015-0364-1",
"article-title": "Ebola Virus Infection: Review of the Pharmacokinetic and Pharmacodynamic Properties of Drugs Considered for Testing in Human Efficacy Trials",
"author": "Madelain",
"doi-asserted-by": "crossref",
"first-page": "907",
"issue": "8",
"journal-title": "Clin Pharmacokinet",
"key": "10.1016/j.ijid.2020.11.008_bib0100",
"volume": "55",
"year": "2016"
},
{
"DOI": "10.1016/j.antiviral.2015.08.015",
"article-title": "Ebola virus dynamics in mice treated with favipiravir",
"author": "Madelain",
"doi-asserted-by": "crossref",
"first-page": "70",
"journal-title": "Antiviral Res",
"key": "10.1016/j.ijid.2020.11.008_bib0105",
"volume": "123",
"year": "2015"
},
{
"DOI": "10.1371/journal.pntd.0008259",
"article-title": "The safety profile of favipiravir should not be the first argument to suspend its evaluation in viral hemorrhagic fevers",
"author": "Malvy",
"doi-asserted-by": "crossref",
"issue": "6",
"journal-title": "PLoS Negl Trop Dis",
"key": "10.1016/j.ijid.2020.11.008_bib0110",
"volume": "14",
"year": "2020"
},
{
"author": "MDVI, LLC",
"key": "10.1016/j.ijid.2020.11.008_bib0115",
"series-title": "Phase 3 efficacy and safety study of favipiravir for treatment of uncomplicated influenza in adults",
"year": "2020"
},
{
"DOI": "10.1016/S1473-3099(14)71047-3",
"article-title": "Dose regimen of favipiravir for Ebola virus disease",
"author": "Mentré",
"doi-asserted-by": "crossref",
"first-page": "150",
"issue": "2",
"journal-title": "Lancet Infect Dis",
"key": "10.1016/j.ijid.2020.11.008_bib0120",
"volume": "15",
"year": "2015"
},
{
"author": "Ministry of Health Oman",
"key": "10.1016/j.ijid.2020.11.008_bib0125",
"series-title": "Number of registered corona virus (COVID-19): Cases in Oman-update",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(03)14484-4",
"article-title": "Treatment of SARS with human interferons",
"author": "Moriguchi",
"doi-asserted-by": "crossref",
"first-page": "1159",
"issue": "9390",
"journal-title": "Lancet",
"key": "10.1016/j.ijid.2020.11.008_bib0130",
"volume": "362",
"year": "2003"
},
{
"DOI": "10.1371/journal.pntd.0005389",
"article-title": "Favipiravir pharmacokinetics in Ebola-Infected patients of the JIKI trial reveals concentrations lower than targeted",
"author": "Nguyen",
"doi-asserted-by": "crossref",
"issue": "2",
"journal-title": "PLoS Negl Trop Dis",
"key": "10.1016/j.ijid.2020.11.008_bib0135",
"volume": "11",
"year": "2017"
},
{
"DOI": "10.1016/j.antiviral.2014.02.014",
"article-title": "Successful treatment of advanced Ebola virus infection with T-705 (favipiravir) in a small animal model",
"author": "Oestereich",
"doi-asserted-by": "crossref",
"first-page": "17",
"journal-title": "Antiviral Res",
"key": "10.1016/j.ijid.2020.11.008_bib0140",
"volume": "105",
"year": "2014"
},
{
"DOI": "10.1016/S2055-6640(20)30016-9",
"article-title": "A review of the safety of favipiravir - a potential treatment in the COVID-19 pandemic?",
"author": "Pilkington",
"doi-asserted-by": "crossref",
"first-page": "45",
"issue": "2",
"journal-title": "J Virus Erad",
"key": "10.1016/j.ijid.2020.11.008_bib0145",
"volume": "6",
"year": "2020"
},
{
"DOI": "10.1016/j.antiviral.2020.104791",
"article-title": "Type 1 interferons as a potential treatment against COVID-19",
"author": "Sallard",
"doi-asserted-by": "crossref",
"journal-title": "Antiviral Res",
"key": "10.1016/j.ijid.2020.11.008_bib0150",
"volume": "178",
"year": "2020"
},
{
"author": "Saudi Ministry of Health",
"key": "10.1016/j.ijid.2020.11.008_bib0155",
"series-title": "Coronavirus Diseases 19 (COVID-19) Protocol for Patients Suspected Confirmed with COVID-9. Supportive care and antiviral treatment of suspected or confirmed COVID-19 infection",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)31101-6",
"article-title": "Interferon beta-1b for COVID-19",
"author": "Shalhoub",
"doi-asserted-by": "crossref",
"first-page": "1670",
"issue": "10238",
"journal-title": "Lancet",
"key": "10.1016/j.ijid.2020.11.008_bib0160",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1016/j.pharmthera.2020.107512",
"article-title": "Favipiravir, an anti-influenza drug against life-threatening RNA virus infections",
"author": "Shiraki",
"doi-asserted-by": "crossref",
"journal-title": "Pharmacol Ther",
"key": "10.1016/j.ijid.2020.11.008_bib0165",
"volume": "209",
"year": "2020"
},
{
"DOI": "10.1371/journal.pmed.1001967",
"article-title": "Experimental Treatment with Favipiravir for Ebola Virus Disease (the JIKI Trial): A Historically Controlled, Single-Arm Proof-of-Concept Trial in Guinea",
"author": "Sissoko",
"doi-asserted-by": "crossref",
"first-page": "e1001967",
"issue": "3",
"journal-title": "PLoS Med",
"key": "10.1016/j.ijid.2020.11.008_bib0170",
"volume": "13",
"year": "2016"
},
{
"DOI": "10.1111/bcp.14314",
"article-title": "Dosing will be a key success factor in repurposing antivirals for COVID‐19",
"author": "Smith",
"doi-asserted-by": "crossref",
"journal-title": "Br J Clin Pharmacol",
"key": "10.1016/j.ijid.2020.11.008_bib0175",
"year": "2020"
},
{
"article-title": "Hydroxychloroquine in patients mainly with mild to moderate COVID-19: an open-label, randomised, controlled trial",
"author": "Tang",
"journal-title": "BMJ",
"key": "10.1016/j.ijid.2020.11.008_bib0180",
"volume": "369",
"year": "2020"
},
{
"author": "United Arab Emirates Ministry of Health and Prevention",
"key": "10.1016/j.ijid.2020.11.008_bib0185",
"series-title": "National Guidelines for Clinical Management and Treatment of COVID-19",
"year": "2020"
},
{
"author": "World Health Organization",
"key": "10.1016/j.ijid.2020.11.008_bib0190",
"series-title": "WHO declares COVID-19 as a global pandemic",
"year": "2020"
}
],
"reference-count": 38,
"references-count": 38,
"relation": {},
"score": 1,
"short-container-title": [
"International Journal of Infectious Diseases"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Infectious Diseases",
"Microbiology (medical)",
"General Medicine"
],
"subtitle": [],
"title": [
"Randomized controlled open label trial on the use of favipiravir combined with inhaled interferon beta-1b in hospitalized patients with moderate to severe COVID-19 pneumonia"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "102"
}
khamis