Predictors of in-hospital mortality in elderly unvaccinated patients during SARS-CoV-2 Alpha variants epidemic
et al., Infection Prevention in Practice, doi:10.1016/j.infpip.2024.100341, Jan 2024
Retrospective 132 hospitalized COVID-19 patients over age 65 in Japan during the Alpha variant surge, showing higher mortality with favipiravir in unadjusted results, without statistical significance.
Potential risks of favipiravir include kidney injury1-3, liver injury2-5, cardiovascular events5,6, pulmonary toxicity6,7, and mutagenicity, carcinogenicity, teratogenicity, embryotoxicity, and the creation of dangerous variants8-14.
Standard of Care (SOC) for COVID-19 in the study country,
Japan, is very poor with very low average efficacy for approved treatments15.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
This study is excluded in the after exclusion results of meta-analysis:
unadjusted results with no group details.
|
risk of death, 168.3% higher, RR 2.68, p = 0.06, treatment 7 of 40 (17.5%), control 6 of 92 (6.5%).
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Abdulaziz et al., Clinical Features and Prognosis of Acute Kidney Injury in Hospital-Admitted Patients with COVID-19 in Egypt: A Single-Center Experience, Mansoura Medical Journal, doi:10.58775/2735-3990.1433.
2.
Ülger et al., Experimental evaluation of favipiravir (T-705)-induced liver and kidney toxicity in rats, Food and Chemical Toxicology, doi:10.1016/j.fct.2025.115472.
3.
El-Fetouh et al., Experimental Studies on Some Drugs Used in Covid-19 Treatment (Favipiravir and Dexamethasone) in Albino Rats, Journal of Advanced Veterinary Research, 13:10, www.advetresearch.com/index.php/AVR/article/view/1635.
4.
Almutairi et al., Liver Injury in Favipiravir-Treated COVID-19 Patients: Retrospective Single-Center Cohort Study, Tropical Medicine and Infectious Disease, doi:10.3390/tropicalmed8020129.
5.
Siby et al., Temporal Trends in Serious Adverse Events Associated with Oral Antivirals During the COVID-19 Pandemic: Insights from the FAERS Database (2020–2023), Open Forum Infectious Diseases, doi:10.1093/ofid/ofaf695.1825.
6.
Ozhan et al., Evaluation of the cardiopulmonary effects of repurposed COVID-19 therapeutics in healthy rats, Scientific Reports, doi:10.1038/s41598-025-31048-4.
7.
Ülger (B) et al., Evaluation of the effects of favipiravir (T-705) on the lung tissue of healty rats: An experimental study, Food and Chemical Toxicology, doi:10.1016/j.fct.2025.115235.
8.
Zhirnov et al., Favipiravir: the hidden threat of mutagenic action, Journal of microbiology, epidemiology and immunobiology, doi:10.36233/0372-9311-114.
9.
Waters et al., Human genetic risk of treatment with antiviral nucleoside analog drugs that induce lethal mutagenesis: the special case of molnupiravir, Environmental and Molecular Mutagenesis, doi:10.1002/em.22471.
10.
Hadj Hassine et al., Lethal Mutagenesis of RNA Viruses and Approved Drugs with Antiviral Mutagenic Activity, Viruses, doi:10.3390/v14040841.
11.
Shum, C., An investigational study into the drug-associated mutational signature in SARS-CoV-2 viruses, The University of Hong Kong, PhD Thesis, hub.hku.hk/handle/10722/344396.
12.
Shiraki et al., Convenient screening of the reproductive toxicity of favipiravir and antiviral drugs in Caenorhabditis elegans, Heliyon, doi:10.1016/j.heliyon.2024.e35331.
13.
Cenikli et al., Does Favipiravir interact with DNA? Design of electrochemical DNA nanobiosensor to investigate the interaction between DNA and Favipiravir used in the treatment of COVID-19, Talanta, doi:10.1016/j.talanta.2025.128084.
Saito et al., 28 Jan 2024, retrospective, Japan, peer-reviewed, 6 authors, study period February 2020 - June 2021, average treatment delay 6.9 days.
Contact: zyst_0404@yahoo.co.jp.
Predictors of in-hospital mortality in elderly unvaccinated patients during SARS-CoV-2 Alpha variants epidemic
Infection Prevention in Practice, doi:10.1016/j.infpip.2024.100341
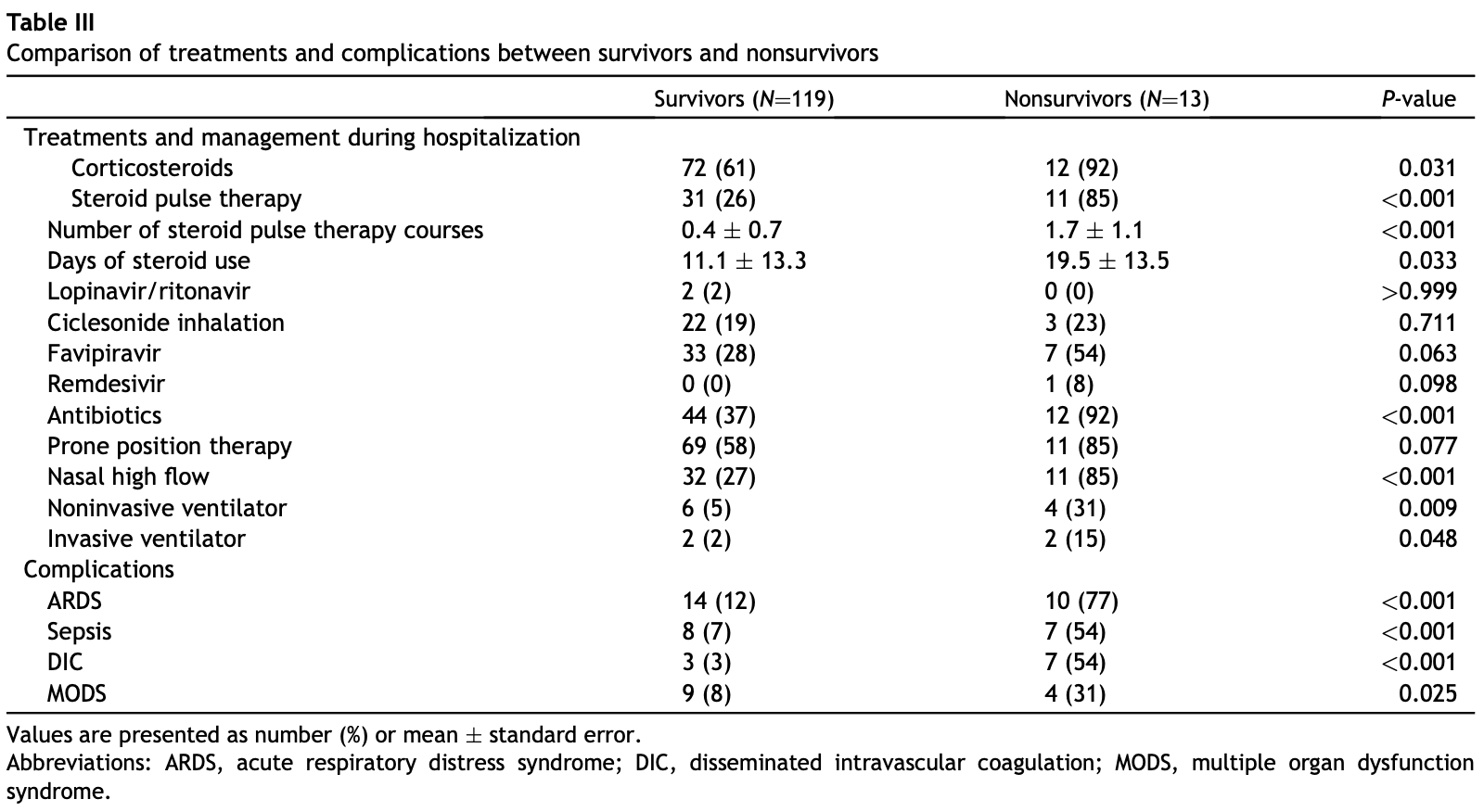
Background: COVID-19, caused by SARS-CoV-2, has caused a global pandemic. This study aimed to identify predictors of in-hospital mortality in unvaccinated elderly patients with COVID-19 by comparing various predictive factors between the survivors and nonsurvivors. Methods: We retrospectively selected 132 unvaccinated patients aged over 65 years with COVID-19 at a hospital in Kanagawa, Japan, during SARS-CoV-2 Alpha variants epidemic. We compared the clinical characteristics, laboratory and radiological findings, treatment, and complications of the survivors and non-survivors. In logistic regression analysis, variables that were significant in the univariate analysis were subjected to multivariate analysis using the variable increase method. Results: There were 119 and 13 patients in the survivor and non-survivor groups, respectively. Multivariate regression revealed increasing odds with the presence of ARDS and DIC (odd ratio (OR) ¼ 16.35, 34.36; P¼0.002, 0.001, respectively) and prolonged hospital stay (OR ¼ 1.17; P¼0.004). Conclusions: We found the complications of ARDS and DIC and hospital length of stay to be independent predictors of in-hospital mortality in elderly unvaccinated patients with COVID-19. Establishing treatments and prevention methods for ARDS and DIC could result in lower mortality rates.
Credit author statement Zenya Saito: Conceptualization, Original draft, Writing, Reviewing and Editing. Shota Uchiyama: Data collection, investigation, reviewing final manuscript. Saiko Nishioka: Data collection, investigation, reviewing final manuscript. Kentaro Tamura: Data collection, investigation, reviewing final manuscript. Nobumasa Tamura: Data collection, investigation, reviewing final manuscript. Kazuyoshi Kuwano: Validation, Methodology, Data analysis, Supervision.
Conflict of interest statement The authors declare that they have no competing interests.
References
Albitar, Ballouze, Ooi, Ghadzi, Risk factors for mortality among COVID-19 patients, Diabetes Res Clin Pract
Ards Definition, Force, Ranieri, Rubenfeld, Thompson et al., Acute respiratory distress syndrome: the Berlin Definition, JAMA
Asakura, Ogawa, COVID-19-associated coagulopathy and disseminated intravascular coagulation, Int J Hematol
Asakura, Takahashi, Uchiyama, Eguchi, Okamoto et al., Proposal for new diagnostic criteria for DIC from the Japanese Society on Thrombosis and Hemostasis, Thromb J
Beitler, Shaefi, Montesi, Devlin, Loring et al., Prone positioning reduces mortality from acute respiratory distress syndrome in the low tidal volume era: a meta-analysis, Intensive Care Med
Buising, Thursky, Black, Macgregor, Street et al., A prospective comparison of severity scores for identifying patients with severe community acquired pneumonia: reconsidering what is meant by severe pneumonia, Thorax
Chalmers, Crichton, Goeminne, Cao, Humbert et al., Management of hospitalized adults with coronavirus disease 2019 (COVID-19): a European Respiratory Society living guideline, Eur Respir J
Coppo, Bellani, Winterton, Pierro, Soria et al., Feasibility and physiological effects of prone positioning in non-intubated patients with acute respiratory failure due to COVID-19 (PRON-COVID): a prospective cohort study, Lancet Respir Med
Ding, Li, Chen, Shu, Song et al., Association of liver abnormalities with in-hospital mortality in patients with COVID-19, J Hepatol
Freund, Lemachatti, Krastinova, Van Laer, Claessens et al., Prognostic accuracy of sepsis-3 criteria for inhospital mortality among patients with suspected infection presenting to the emergency department, JAMA
Huang, Pranata, Lim, Oehadian, Alisjahbana, C-reactive protein, procalcitonin, D-dimer, and ferritin in severe coronavirus disease-2019: a meta-analysis, Ther Adv Respir Dis
Inoue, Yamamoto, Identification of an existing Japanese pancreatitis drug, nafamostat, which is expected to prevent the transmission of new coronavirus infection (COVID-19
Kasamatsu, Yamaguchi, Kawaguchi, Tanaka, Oka et al., Usefulness of a semi-quantitative procalcitonin test and the A-DROP Japanese prognostic scale for predicting mortality among adults hospitalized with community-acquired pneumonia, Respirol
Lambden, Laterre, Levy, Francois, The SOFA scoreddevelopment, utility and challenges of accurate assessment in clinical trials, Crit Care
Li, Xu, Yu, Wang, Tao et al., Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan, J Allergy Clin Immunol
Osterbur, Mann, Kuroki, Declue, Multiple organ dysfunction syndrome in humans and animals, J Vet Intern Med
Shindo, Sato, Maruyama, Ohashi, Ogawa et al., Comparison of severity scoring systems A-DROP and CURB-65 for community-acquired pneumonia, Respirol
Singer, Deutschman, Seymour, Shankar-Hari, Annane et al., The third international consensus definitions for sepsis and septic shock (Sepsis-3), JAMA
Tabata, Imai, Kawano, Ikeda, Kodama et al., Clinical characteristics of COVID-19 in 104 people with SARS-CoV-2 infection on the Diamond Princess cruise ship: a retrospective analysis, Lancet Infect Dis
Tang, Bai, Chen, Gong, Li et al., Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy, J Thromb Haemost
Thachil, Tang, Gando, Falanga, Cattaneo et al., ISTH interim guidance on recognition and management of coagulopathy in COVID-19, J Thromb Haemost
Toma, Abu-Hanna, Bosman, Discovery and inclusion of SOFA score episodes in mortality prediction, J Biomed Inform
Wang, Zhang, Yu, Tao, Xie, 15-day mortality and associated risk factors for hospitalized patients with COVID-19 in Wuhan, China: an ambispective observational cohort study, Intensive Care Med
Wang, Zhao, Zai, Li, Cross-species transmission of the newly identified coronavirus 2019-nCoV, J Med Virol
Wu, Chen, Cai, Xia, Zhou et al., Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus Disease 2019 pneumonia in Wuhan, China, JAMA Intern Med
Yang, Yu, Xu, Shu, Xia et al., Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study, Lancet Respir Med
Zhang, Cao, Tan, Dong, Wang et al., Clinical, radiological, and laboratory characteristics and risk factors for severity and mortality of 289 hospitalized COVID-19 patients, Allergy
Zhou, Yu, Du, Fan, Liu et al., Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet
DOI record:
{
"DOI": "10.1016/j.infpip.2024.100341",
"ISSN": [
"2590-0889"
],
"URL": "http://dx.doi.org/10.1016/j.infpip.2024.100341",
"alternative-id": [
"S2590088924000052"
],
"article-number": "100341",
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Predictors of in-hospital mortality in elderly unvaccinated patients during SARS-CoV-2 Alpha variants epidemic"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Infection Prevention in Practice"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.infpip.2024.100341"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2024 The Authors. Published by Elsevier Ltd on behalf of The Healthcare Infection Society."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0001-7945-0976",
"affiliation": [],
"authenticated-orcid": false,
"family": "Saito",
"given": "Zenya",
"sequence": "first"
},
{
"affiliation": [],
"family": "Uchiyama",
"given": "Shota",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nishioka",
"given": "Saiko",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tamura",
"given": "Kentaro",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tamura",
"given": "Nobumasa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kuwano",
"given": "Kazuyoshi",
"sequence": "additional"
}
],
"container-title": "Infection Prevention in Practice",
"container-title-short": "Infection Prevention in Practice",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2024,
1,
28
]
],
"date-time": "2024-01-28T13:43:51Z",
"timestamp": 1706449431000
},
"deposited": {
"date-parts": [
[
2024,
2,
16
]
],
"date-time": "2024-02-16T20:20:24Z",
"timestamp": 1708114824000
},
"indexed": {
"date-parts": [
[
2024,
2,
17
]
],
"date-time": "2024-02-17T00:15:47Z",
"timestamp": 1708128947186
},
"is-referenced-by-count": 0,
"issue": "1",
"issued": {
"date-parts": [
[
2024,
3
]
]
},
"journal-issue": {
"issue": "1",
"published-print": {
"date-parts": [
[
2024,
3
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
3,
1
]
],
"date-time": "2024-03-01T00:00:00Z",
"timestamp": 1709251200000
}
},
{
"URL": "http://creativecommons.org/licenses/by-nc-nd/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
1,
23
]
],
"date-time": "2024-01-23T00:00:00Z",
"timestamp": 1705968000000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S2590088924000052?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S2590088924000052?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "100341",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2024,
3
]
]
},
"published-print": {
"date-parts": [
[
2024,
3
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1002/jmv.25682",
"article-title": "Cross-species transmission of the newly identified coronavirus 2019-nCoV",
"author": "Ji",
"doi-asserted-by": "crossref",
"first-page": "433",
"journal-title": "J Med Virol",
"key": "10.1016/j.infpip.2024.100341_bib1",
"volume": "92",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"article-title": "Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study",
"author": "Zhou",
"doi-asserted-by": "crossref",
"first-page": "1054",
"journal-title": "Lancet",
"key": "10.1016/j.infpip.2024.100341_bib2",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1038/s41564-020-0695-z",
"article-title": "The species severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2",
"doi-asserted-by": "crossref",
"first-page": "536",
"journal-title": "Nat Microbiol",
"key": "10.1016/j.infpip.2024.100341_bib3",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1016/S1473-3099(20)30482-5",
"article-title": "Clinical characteristics of COVID-19 in 104 people with SARS-CoV-2 infection on the Diamond Princess cruise ship: a retrospective analysis",
"author": "Tabata",
"doi-asserted-by": "crossref",
"first-page": "1043",
"journal-title": "Lancet Infect Dis",
"key": "10.1016/j.infpip.2024.100341_bib4",
"volume": "20",
"year": "2020"
},
{
"key": "10.1016/j.infpip.2024.100341_bib5",
"unstructured": "The Ministry of Health, Labour and Welfare of Japan. Domestic outbreak trends of new coronavirus infections [in Japanese]. Available from: https://www.mhlw.go.jp/content/10906000/000716059.pdf."
},
{
"DOI": "10.1016/j.diabres.2020.108293",
"article-title": "Risk factors for mortality among COVID-19 patients",
"author": "Albitar",
"doi-asserted-by": "crossref",
"journal-title": "Diabetes Res Clin Pract",
"key": "10.1016/j.infpip.2024.100341_bib6",
"volume": "166",
"year": "2020"
},
{
"DOI": "10.1016/j.jhep.2020.12.012",
"article-title": "Association of liver abnormalities with in-hospital mortality in patients with COVID-19",
"author": "Ding",
"doi-asserted-by": "crossref",
"first-page": "1295",
"journal-title": "J Hepatol",
"key": "10.1016/j.infpip.2024.100341_bib7",
"volume": "74",
"year": "2021"
},
{
"DOI": "10.1177/1753466620937175",
"article-title": "C-reactive protein, procalcitonin, D-dimer, and ferritin in severe coronavirus disease-2019: a meta-analysis",
"author": "Huang",
"doi-asserted-by": "crossref",
"journal-title": "Ther Adv Respir Dis",
"key": "10.1016/j.infpip.2024.100341_bib8",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1111/all.14496",
"article-title": "Clinical, radiological, and laboratory characteristics and risk factors for severity and mortality of 289 hospitalized COVID-19 patients",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "533",
"journal-title": "Allergy",
"key": "10.1016/j.infpip.2024.100341_bib9",
"volume": "76",
"year": "2021"
},
{
"DOI": "10.1001/jamainternmed.2020.0994",
"article-title": "Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus Disease 2019 pneumonia in Wuhan, China",
"author": "Wu",
"doi-asserted-by": "crossref",
"first-page": "934",
"journal-title": "JAMA Intern Med",
"key": "10.1016/j.infpip.2024.100341_bib10",
"volume": "180",
"year": "2020"
},
{
"DOI": "10.1016/S2213-2600(20)30079-5",
"article-title": "Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study",
"author": "Yang",
"doi-asserted-by": "crossref",
"first-page": "475",
"journal-title": "Lancet Respir Med",
"key": "10.1016/j.infpip.2024.100341_bib11",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/j.jaci.2020.04.006",
"article-title": "Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "110",
"journal-title": "J Allergy Clin Immunol",
"key": "10.1016/j.infpip.2024.100341_bib12",
"volume": "146",
"year": "2020"
},
{
"DOI": "10.1007/s00134-020-06047-w",
"article-title": "15-day mortality and associated risk factors for hospitalized patients with COVID-19 in Wuhan, China: an ambispective observational cohort study",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "1472",
"journal-title": "Intensive Care Med",
"key": "10.1016/j.infpip.2024.100341_bib13",
"volume": "46",
"year": "2020"
},
{
"key": "10.1016/j.infpip.2024.100341_bib14",
"unstructured": "Japanese guidelines on Novel coronavirus (COVID-19) created on 26 February 2020. Last Updated 04 Aug 2021. Compiled by colleagues at Bukkyo University, co-ordinated by Prof. Hajime Takeuchi MD. https://evidenceaid.org/coronavirus-covid-19-evidence-collection/coronavirus-resources/japanese-guidelines-on-novel-coronavirus-covid-19/."
},
{
"DOI": "10.1111/j.1440-1843.2008.01329.x",
"article-title": "Comparison of severity scoring systems A-DROP and CURB-65 for community-acquired pneumonia",
"author": "Shindo",
"doi-asserted-by": "crossref",
"first-page": "731",
"journal-title": "Respirol",
"key": "10.1016/j.infpip.2024.100341_bib15",
"volume": "13",
"year": "2008"
},
{
"DOI": "10.1136/thx.2005.051326",
"article-title": "A prospective comparison of severity scores for identifying patients with severe community acquired pneumonia: reconsidering what is meant by severe pneumonia",
"author": "Buising",
"doi-asserted-by": "crossref",
"first-page": "419",
"journal-title": "Thorax",
"key": "10.1016/j.infpip.2024.100341_bib16",
"volume": "61",
"year": "2006"
},
{
"DOI": "10.1111/j.1440-1843.2011.02101.x",
"article-title": "Usefulness of a semi-quantitative procalcitonin test and the A-DROP Japanese prognostic scale for predicting mortality among adults hospitalized with community-acquired pneumonia",
"author": "Kasamatsu",
"doi-asserted-by": "crossref",
"first-page": "330",
"journal-title": "Respirol",
"key": "10.1016/j.infpip.2024.100341_bib17",
"volume": "17",
"year": "2012"
},
{
"article-title": "Acute respiratory distress syndrome: the Berlin Definition",
"author": "Ranieri",
"first-page": "2526",
"journal-title": "JAMA",
"key": "10.1016/j.infpip.2024.100341_bib18",
"volume": "307",
"year": "2012"
},
{
"DOI": "10.1001/jama.2016.0287",
"article-title": "The third international consensus definitions for sepsis and septic shock (Sepsis-3)",
"author": "Singer",
"doi-asserted-by": "crossref",
"first-page": "801",
"journal-title": "JAMA",
"key": "10.1016/j.infpip.2024.100341_bib19",
"volume": "315",
"year": "2016"
},
{
"DOI": "10.1016/j.jbi.2007.03.007",
"article-title": "Discovery and inclusion of SOFA score episodes in mortality prediction",
"author": "Toma",
"doi-asserted-by": "crossref",
"first-page": "649",
"journal-title": "J Biomed Inform",
"key": "10.1016/j.infpip.2024.100341_bib20",
"volume": "40",
"year": "2007"
},
{
"DOI": "10.1186/s13054-019-2663-7",
"article-title": "The SOFA score—development, utility and challenges of accurate assessment in clinical trials",
"author": "Lambden",
"doi-asserted-by": "crossref",
"first-page": "374",
"journal-title": "Crit Care",
"key": "10.1016/j.infpip.2024.100341_bib21",
"volume": "23",
"year": "2019"
},
{
"DOI": "10.1001/jama.2016.20329",
"article-title": "Prognostic accuracy of sepsis-3 criteria for in-hospital mortality among patients with suspected infection presenting to the emergency department",
"author": "Freund",
"doi-asserted-by": "crossref",
"first-page": "301",
"journal-title": "JAMA",
"key": "10.1016/j.infpip.2024.100341_bib22",
"volume": "317",
"year": "2017"
},
{
"DOI": "10.1186/s12959-016-0117-x",
"article-title": "Proposal for new diagnostic criteria for DIC from the Japanese Society on Thrombosis and Hemostasis",
"author": "Asakura",
"doi-asserted-by": "crossref",
"first-page": "42",
"journal-title": "Thromb J",
"key": "10.1016/j.infpip.2024.100341_bib23",
"volume": "14",
"year": "2016"
},
{
"DOI": "10.1111/jvim.12364",
"article-title": "Multiple organ dysfunction syndrome in humans and animals",
"author": "Osterbur",
"doi-asserted-by": "crossref",
"first-page": "1141",
"journal-title": "J Vet Intern Med",
"key": "10.1016/j.infpip.2024.100341_bib24",
"volume": "28",
"year": "2014"
},
{
"DOI": "10.1007/s00134-013-3194-3",
"article-title": "Prone positioning reduces mortality from acute respiratory distress syndrome in the low tidal volume era: a meta-analysis",
"author": "Beitler",
"doi-asserted-by": "crossref",
"first-page": "332",
"journal-title": "Intensive Care Med",
"key": "10.1016/j.infpip.2024.100341_bib25",
"volume": "40",
"year": "2014"
},
{
"DOI": "10.1016/S2213-2600(20)30268-X",
"article-title": "Feasibility and physiological effects of prone positioning in non-intubated patients with acute respiratory failure due to COVID-19 (PRON-COVID): a prospective cohort study",
"author": "Coppo",
"doi-asserted-by": "crossref",
"first-page": "765",
"journal-title": "Lancet Respir Med",
"key": "10.1016/j.infpip.2024.100341_bib26",
"volume": "8",
"year": "2020"
},
{
"article-title": "Management of hospitalized adults with coronavirus disease 2019 (COVID-19): a European Respiratory Society living guideline",
"author": "Chalmers",
"first-page": "57",
"journal-title": "Eur Respir J",
"key": "10.1016/j.infpip.2024.100341_bib27",
"year": "2021"
},
{
"DOI": "10.1007/s12185-020-03029-y",
"article-title": "COVID-19-associated coagulopathy and disseminated intravascular coagulation",
"author": "Asakura",
"doi-asserted-by": "crossref",
"first-page": "45",
"journal-title": "Int J Hematol",
"key": "10.1016/j.infpip.2024.100341_bib28",
"volume": "113",
"year": "2021"
},
{
"DOI": "10.1111/jth.14810",
"article-title": "ISTH interim guidance on recognition and management of coagulopathy in COVID-19",
"author": "Thachil",
"doi-asserted-by": "crossref",
"first-page": "1023",
"journal-title": "J Thromb Haemost",
"key": "10.1016/j.infpip.2024.100341_bib29",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.1111/jth.14817",
"article-title": "Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy",
"author": "Tang",
"doi-asserted-by": "crossref",
"first-page": "1094",
"journal-title": "J Thromb Haemost",
"key": "10.1016/j.infpip.2024.100341_bib30",
"volume": "18",
"year": "2020"
},
{
"key": "10.1016/j.infpip.2024.100341_bib31",
"unstructured": "Inoue J, Yamamoto M. Identification of an existing Japanese pancreatitis drug, nafamostat, which is expected to prevent the transmission of new coronavirus infection (COVID-19). https://www.u-tokyo.ac.jp/focus/en/articles/z0508_00083.html."
}
],
"reference-count": 31,
"references-count": 31,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S2590088924000052"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Infectious Diseases",
"Public Health, Environmental and Occupational Health"
],
"subtitle": [],
"title": "Predictors of in-hospital mortality in elderly unvaccinated patients during SARS-CoV-2 Alpha variants epidemic",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "6"
}