Antiviral Used among Non-Severe COVID-19 Cases in Relation to Time till Viral Clearance: A Retrospective Cohort Study
et al., Antibiotics, doi:10.3390/antibiotics11040498, Apr 2022
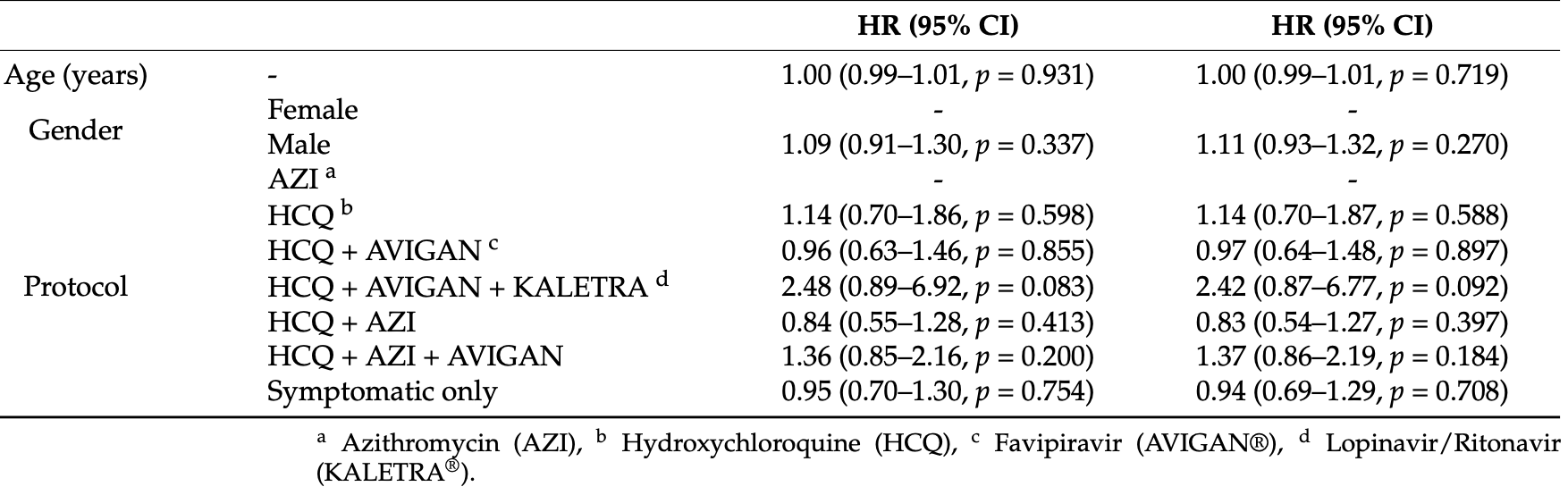
Retrospective hospitalized patients in the United Arab Emirates, showing no significant difference in viral clearance with different combinations of HCQ, AZ, favipiravir, and lopinavir/ritonavir.
Potential risks of favipiravir include kidney injury1-3, liver injury2-5, cardiovascular events5,6, pulmonary toxicity6,7, and mutagenicity, carcinogenicity, teratogenicity, embryotoxicity, and the creation of dangerous variants8-14.
Study covers HCQ and favipiravir.
|
viral clearance time, 3.1% higher, HR 1.03, p = 0.09, treatment 59, control 1,446, inverted to make HR<1 favor treatment, HCQ + favipiravir, Cox proportional hazards.
|
|
viral clearance time, 58.7% lower, HR 0.41, p = 0.09, treatment 4, control 1,446, inverted to make HR<1 favor treatment, HCQ + favipiravir + lopinavir/ritonavir, Cox proportional hazards.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Abdulaziz et al., Clinical Features and Prognosis of Acute Kidney Injury in Hospital-Admitted Patients with COVID-19 in Egypt: A Single-Center Experience, Mansoura Medical Journal, doi:10.58775/2735-3990.1433.
2.
Ülger et al., Experimental evaluation of favipiravir (T-705)-induced liver and kidney toxicity in rats, Food and Chemical Toxicology, doi:10.1016/j.fct.2025.115472.
3.
El-Fetouh et al., Experimental Studies on Some Drugs Used in Covid-19 Treatment (Favipiravir and Dexamethasone) in Albino Rats, Journal of Advanced Veterinary Research, 13:10, www.advetresearch.com/index.php/AVR/article/view/1635.
4.
Almutairi et al., Liver Injury in Favipiravir-Treated COVID-19 Patients: Retrospective Single-Center Cohort Study, Tropical Medicine and Infectious Disease, doi:10.3390/tropicalmed8020129.
5.
Siby et al., Temporal Trends in Serious Adverse Events Associated with Oral Antivirals During the COVID-19 Pandemic: Insights from the FAERS Database (2020–2023), Open Forum Infectious Diseases, doi:10.1093/ofid/ofaf695.1825.
6.
Ozhan et al., Evaluation of the cardiopulmonary effects of repurposed COVID-19 therapeutics in healthy rats, Scientific Reports, doi:10.1038/s41598-025-31048-4.
7.
Ülger (B) et al., Evaluation of the effects of favipiravir (T-705) on the lung tissue of healty rats: An experimental study, Food and Chemical Toxicology, doi:10.1016/j.fct.2025.115235.
8.
Zhirnov et al., Favipiravir: the hidden threat of mutagenic action, Journal of microbiology, epidemiology and immunobiology, doi:10.36233/0372-9311-114.
9.
Waters et al., Human genetic risk of treatment with antiviral nucleoside analog drugs that induce lethal mutagenesis: the special case of molnupiravir, Environmental and Molecular Mutagenesis, doi:10.1002/em.22471.
10.
Hadj Hassine et al., Lethal Mutagenesis of RNA Viruses and Approved Drugs with Antiviral Mutagenic Activity, Viruses, doi:10.3390/v14040841.
11.
Shum, C., An investigational study into the drug-associated mutational signature in SARS-CoV-2 viruses, The University of Hong Kong, PhD Thesis, hub.hku.hk/handle/10722/344396.
12.
Shiraki et al., Convenient screening of the reproductive toxicity of favipiravir and antiviral drugs in Caenorhabditis elegans, Heliyon, doi:10.1016/j.heliyon.2024.e35331.
Hafez et al., 8 Apr 2022, retrospective, United Arab Emirates, peer-reviewed, 6 authors, this trial uses multiple treatments in the treatment arm (combined with HCQ) - results of individual treatments may vary.
Antiviral Used among Non-Severe COVID-19 Cases in Relation to Time till Viral Clearance: A Retrospective Cohort Study
Antibiotics, doi:10.3390/antibiotics11040498
1) Background: The WHO identified COVID-19 as a fast-growing epidemic worldwide. A few antivirals have shown promising effectiveness in treating COVID-19. This study aimed to assess the correlation between antiviral drugs and the time until viral clearance of SARS-CoV-2. (2) Methods: This was a retrospective cohort study that included 1731 non-severe COVID-19 patients treated in NMC Royal Hospital, UAE. (3) Results: A total of 1446 patients received symptomatic treatment only (mean age of 35.6 ± 9.0 years). The analyzed antiviral treatment protocols were azithromycin, hydroxychloroquine, lopinavir/ritonavir, and favipiravir. The produced Kaplan-Meier plots showed no significant differences in the time until viral clearance among the compared protocols, which showed overlapping confidence intervals, which were determined by performing the log-rank and adjusted pairwise log-rank tests (p = 0.2, log-rank = 9.3). The age and gender of patients did not significantly affect the rate of viral clearance regardless of the antiviral therapy administered, even when compared to patients who received symptomatic treatment only, with the exception of hydroxychloroquine (HCQ), azithromycin, and favipiravir, which increased the odds of a faster rate of viral clearance by 46% after adjustments. (4) Conclusions: No significant differences were observed regarding the time until viral clearance among non-severe COVID-19 patients following the prescription of different antiviral drugs.
References
Alhumaid, Al Mutair, Al Alawi, Alhmeed, Zaidi et al., Efficacy and Safety of Lopinavir/Ritonavir for Treatment of COVID-19: A Systematic Review and Meta-Analysis, Trop. Med. Infect. Dis, doi:10.3390/tropicalmed5040180
Badu, Oyebola, Zahouli, Fagbamigbe, De Souza et al., SARS-CoV-2 Viral Shedding and Transmission Dynamics: Implications of WHO COVID-19 Discharge Guidelines, Front. Med, doi:10.3389/fmed.2021.648660
Cai, Yang, Liu, Chen, Shu et al., Experimental Treatment with Favipiravir for COVID-19: An Open-Label Control Study, Eng. Beijing China, doi:10.1016/j.eng.2020.03.007
Canini, Perelson, Viral Kinetic Modeling: State of the Art, J. Pharmacokinet. Pharmacodyn, doi:10.1007/s10928-014-9363-3
Cao, Wang, Wen, Liu, Wang et al., A Trial of Lopinavir-Ritonavir in Adults Hospitalized with Severe COVID-19, N. Engl. J. Med, doi:10.1056/NEJMoa2001282
Chan, Yao, Yeung, Deng, Bao et al., Treatment with Lopinavir/Ritonavir or Interferon-B1b Improves Outcome of MERS-CoV Infection in a Nonhuman Primate Model of Common Marmoset, J. Infect. Dis, doi:10.1093/infdis/jiv392
Chen, Hu, Zhang, Jiang, Han et al., Efficacy of Hydroxychloroquine in Patients with COVID-19: Results of a Randomized Clinical Trial, MedRxiv, doi:10.1101/2020.03.22.20040758
Chen, Zhang, Huang, Yin, Cheng et al., Favipiravir versus Arbidol for COVID-19: A Randomized Clinical Trial, MedRxiv, doi:10.1101/2020.03.17.20037432
Chu, Cheng, Hung, Wong, Chan et al., Role of Lopinavir/Ritonavir in the Treatment of SARS: Initial Virological and Clinical Findings, Thorax, doi:10.1136/thorax.2003.012658
Corman, Albarrak, Omrani, Albarrak, Farah et al., Viral Shedding and Antibody Response in 37 Patients with Middle East Respiratory Syndrome Coronavirus Infection, Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am, doi:10.1093/cid/civ951
De Wilde, Jochmans, Posthuma, Zevenhoven-Dobbe, Van Nieuwkoop et al., Screening of an FDA-Approved Compound Library Identifies Four Small-Molecule Inhibitors of Middle East Respiratory Syndrome Coronavirus Replication in Cell Culture, Antimicrob. Agents Chemother, doi:10.1128/AAC.03011-14
Devaux, Rolain, Colson, Raoult, New Insights on the Antiviral Effects of Chloroquine against Coronavirus: What to Expect for COVID-19?, Int. J. Antimicrob. Agents, doi:10.1016/j.ijantimicag.2020.105938
Ding, Li, Hong, Yu, Ye et al., Viral Kinetics and Factors Associated with Rapid Viral Clearance during Lopinavir/Ritonavir-Based Combination Therapy in Non-Severe COVID-19 Patients, Eur. Rev. Med. Pharmacol. Sci, doi:10.26355/eurrev_202005_21373
Echeverría-Esnal, Martin-Ontiyuelo, Navarrete-Rouco, De-Antonio Cuscó, Ferrández et al., Azithromycin in the Treatment of COVID-19: A Review, Expert Rev. Anti Infect. Ther, doi:10.1080/14787210.2020.1813024
Furtado, Berwanger, Fonseca, Corrêa, Ferraz et al., Azithromycin in Addition to Standard of Care versus Standard of Care Alone in the Treatment of Patients Admitted to the Hospital with Severe COVID-19 in Brazil (COALITION II): A Randomised Clinical Trial, Lancet, doi:10.1016/S0140-6736(20)31862-6
Gagliardini, Cozzi-Lepri, Mariano, Taglietti, Vergori et al., No Efficacy of the Combination of Lopinavir/Ritonavir Plus Hydroxychloroquine Versus Standard of Care in Patients Hospitalized With COVID-19: A Non-Randomized Comparison, Front. Pharmacol, doi:10.3389/fphar.2021.621676
Gastine, Pang, Boshier, Carter, Lonsdale et al., Systematic Review and Patient-Level Meta-Analysis of SARS-CoV-2 Viral Dynamics to Model Response to Antiviral Therapies, Clin. Pharmacol. Ther, doi:10.1002/cpt.2223
Gautret, Lagier, Parola, Hoang, Meddeb et al., Clinical and Microbiological Effect of a Combination of Hydroxychloroquine and Azithromycin in 80 COVID-19 Patients with at Least a Six-Day Follow up: A Pilot Observational Study, Travel Med. Infect. Dis, doi:10.1016/j.tmaid.2020.101663
Gbinigie, Frie, Should Azithromycin Be Used to Treat COVID-19? A Rapid Review, BJGP Open, doi:10.3399/bjgpopen20X101094
Guner, Hasanoglu, Kayaaslan, Aypak, Akinci et al., Comparing ICU Admission Rates of Mild/Moderate COVID-19 Patients Treated with Hydroxychloroquine, Favipiravir, and Hydroxychloroquine plus Favipiravir, J. Infect. Public Health, doi:10.1016/j.jiph.2020.12.017
Jacobs, Persistent SARS-2 Infections Contribute to Long COVID-19, Med. Hypotheses, doi:10.1016/j.mehy.2021.110538
Kim, Iwanami, Oda, Fujita, Kuba et al., Incomplete Antiviral Treatment May Induce Longer Durations of Viral Shedding during SARS-CoV-2 Infection, Life Sci. Alliance, doi:10.26508/lsa.202101049
Kim, Ko, Kim, Kim, Kim et al., Viral Load Kinetics of SARS-CoV-2 Infection in First Two Patients in Korea, J. Korean Med. Sci, doi:10.3346/jkms.2020.35.e86
Klein, Sex Influences Immune Responses to Viruses, and Efficacy of Prophylaxis and Treatments for Viral Diseases, BioEssays News Rev. Mol. Cell. Dev. Biol, doi:10.1002/bies.201200099
Kocayi Git, Özmen, Süner, Tomak, Demir et al., Observational Study of the Effects of Favipiravir vs Lopinavir/Ritonavir on Clinical Outcomes in Critically Ill Patients with COVID-19, J. Clin. Pharm. Ther, doi:10.1111/jcpt.13305
Li, Xie, Lin, Cai, Wen et al., Efficacy and Safety of Lopinavir/Ritonavir or Arbidol in Adult Patients with Mild/Moderate COVID-19: An Exploratory Randomized Controlled Trial, Med, doi:10.1016/j.medj.2020.04.001
Lu, Drug Treatment Options for the 2019-New Coronavirus (2019-NCoV), Biosci. Trends, doi:10.5582/bst.2020.01020
Million, Lagier, Gautret, Colson, Fournier et al., Early Treatment of COVID-19 Patients with Hydroxychloroquine and Azithromycin: A Retrospective Analysis of 1061 Cases in Marseille, France, Travel Med. Infect. Dis, doi:10.1016/j.tmaid.2020.101738
Pontali, Volpi, Antonucci, Castellaneta, Buzzi et al., Safety and Efficacy of Early High-Dose IV Anakinra in Severe COVID-19 Lung Disease, J. Allergy Clin. Immunol, doi:10.1016/j.jaci.2020.05.002
Rosenberg, Dufort, Udo, Wilberschied, Kumar et al., Association of Treatment with Hydroxychloroquine or Azithromycin with In-Hospital Mortality in Patients with COVID-19 in New York State, JAMA, doi:10.1001/jama.2020.8630
Salciccia, Eisenberg, Maggi, Lai, Mastroianni et al., Modeling the Contribution of Male Testosterone Levels to the Duration of Positive COVID Testing among Hospitalized Male COVID-19 Patients, Diagnostics, doi:10.3390/diagnostics11040581
Schrezenmeier, Dörner, Mechanisms of Action of Hydroxychloroquine and Chloroquine: Implications for Rheumatology, Nat. Rev. Rheumatol, doi:10.1038/s41584-020-0372-x
Sheahan, Sims, Leist, Schäfer, Won et al., Comparative Therapeutic Efficacy of Remdesivir and Combination Lopinavir, Ritonavir, and Interferon Beta against MERS-CoV, Nat. Commun, doi:10.1038/s41467-019-13940-6
Smith, Dodds, Bentley, Yeo, Rayner, Dosing Will Be a Key Success Factor in Repurposing Antivirals for COVID-19, Br. J. Clin. Pharmacol, doi:10.1111/bcp.14314
Totura, Bavari, Broad-Spectrum Coronavirus Antiviral Drug Discovery, Expert Opin. Drug Discov
Yan, Liu, Zhu, Huang, Dan et al., Factors Associated with Prolonged Viral Shedding and Impact of Lopinavir/Ritonavir Treatment in Hospitalised Non-Critically Ill Patients with SARS-CoV-2 Infection, Eur. Respir. J, doi:10.1183/13993003.00799-2020
Yao, Ye, Zhang, Cui, Huang et al., Vitro Antiviral Activity and Projection of Optimized Dosing Design of Hydroxychloroquine for the Treatment of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am, doi:10.1093/cid/ciaa237
Zhao, Zhang, Zhu, Chen, Chen et al., Favipiravir in the Treatment of Patients with SARS-CoV-2 RNA Recurrent Positive after Discharge: A Multicenter, Open-Label, Randomized Trial, Int. Immunopharmacol, doi:10.1016/j.intimp.2021.107702
Zhou, Ding, Bao, Xue, Han et al., Clinical Features in Coronavirus Disease 2019 (COVID-19) Patients with Early Clearance and Prolonged Shedding of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) RNA, Ann. Transl. Med, doi:10.21037/atm-21-445
Zhou, Yu, Du, Fan, Liu et al., Clinical Course and Risk Factors for Mortality of Adult Inpatients with COVID-19 in Wuhan, China: A Retrospective Cohort Study, Lancet
Zhu, Lu, Xu, Chen, Yang et al., Arbidol Monotherapy Is Superior to Lopinavir/Ritonavir in Treating COVID-19, J. Infect, doi:10.1016/j.jinf.2020.03.060
DOI record:
{
"DOI": "10.3390/antibiotics11040498",
"ISSN": [
"2079-6382"
],
"URL": "http://dx.doi.org/10.3390/antibiotics11040498",
"abstract": "<jats:p>(1) Background: The WHO identified COVID-19 as a fast-growing epidemic worldwide. A few antivirals have shown promising effectiveness in treating COVID-19. This study aimed to assess the correlation between antiviral drugs and the time until viral clearance of SARS-CoV-2. (2) Methods: This was a retrospective cohort study that included 1731 non-severe COVID-19 patients treated in NMC Royal Hospital, UAE. (3) Results: A total of 1446 patients received symptomatic treatment only (mean age of 35.6 ± 9.0 years). The analyzed antiviral treatment protocols were azithromycin, hydroxychloroquine, lopinavir/ritonavir, and favipiravir. The produced Kaplan–Meier plots showed no significant differences in the time until viral clearance among the compared protocols, which showed overlapping confidence intervals, which were determined by performing the log-rank and adjusted pairwise log-rank tests (p = 0.2, log-rank = 9.3). The age and gender of patients did not significantly affect the rate of viral clearance regardless of the antiviral therapy administered, even when compared to patients who received symptomatic treatment only, with the exception of hydroxychloroquine (HCQ), azithromycin, and favipiravir, which increased the odds of a faster rate of viral clearance by 46% after adjustments. (4) Conclusions: No significant differences were observed regarding the time until viral clearance among non-severe COVID-19 patients following the prescription of different antiviral drugs.</jats:p>",
"alternative-id": [
"antibiotics11040498"
],
"author": [
{
"affiliation": [],
"family": "Hafez",
"given": "Wael",
"sequence": "first"
},
{
"affiliation": [],
"family": "Saleh",
"given": "Husam",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4220-3266",
"affiliation": [],
"authenticated-orcid": false,
"family": "Al Baha",
"given": "Ziad",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tariq",
"given": "Mishal",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hamdan",
"given": "Samah",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ahmed",
"given": "Shougyat",
"sequence": "additional"
}
],
"container-title": [
"Antibiotics"
],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
4,
8
]
],
"date-time": "2022-04-08T16:11:14Z",
"timestamp": 1649434274000
},
"deposited": {
"date-parts": [
[
2022,
4,
8
]
],
"date-time": "2022-04-08T16:20:55Z",
"timestamp": 1649434855000
},
"indexed": {
"date-parts": [
[
2022,
4,
8
]
],
"date-time": "2022-04-08T16:42:00Z",
"timestamp": 1649436120529
},
"is-referenced-by-count": 0,
"issn-type": [
{
"type": "electronic",
"value": "2079-6382"
}
],
"issue": "4",
"issued": {
"date-parts": [
[
2022,
4,
8
]
]
},
"journal-issue": {
"issue": "4",
"published-online": {
"date-parts": [
[
2022,
4
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
4,
8
]
],
"date-time": "2022-04-08T00:00:00Z",
"timestamp": 1649376000000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2079-6382/11/4/498/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "498",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2022,
4,
8
]
]
},
"published-online": {
"date-parts": [
[
2022,
4,
8
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.5582/bst.2020.01020",
"doi-asserted-by": "publisher",
"key": "ref1"
},
{
"DOI": "10.1128/AAC.03011-14",
"doi-asserted-by": "publisher",
"key": "ref2"
},
{
"DOI": "10.1093/infdis/jiv392",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.1136/thorax.2003.012658",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.1038/s41467-019-13940-6",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.1016/j.eng.2020.03.007",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.1016/j.jinf.2020.03.060",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.1093/cid/ciaa237",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"DOI": "10.1016/j.ijantimicag.2020.105938",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"DOI": "10.1038/s41584-020-0372-x",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.1080/14787210.2020.1813024",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.1016/S0140-6736(20)31862-6",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.1016/j.medj.2020.04.001",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"DOI": "10.3390/tropicalmed5040180",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.1080/17460441.2019.1581171",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.1093/cid/civ951",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.1016/j.mehy.2021.110538",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.26355/eurrev_202005_21373",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.1007/s10928-014-9363-3",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.3346/jkms.2020.35.e86",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"DOI": "10.1002/cpt.2223",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"DOI": "10.1056/NEJMoa2001282",
"doi-asserted-by": "publisher",
"key": "ref23"
},
{
"DOI": "10.1101/2020.03.17.20037432",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.1111/jcpt.13305",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"DOI": "10.1016/j.intimp.2021.107702",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.1016/j.jiph.2020.12.017",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.1016/j.jaci.2020.05.002",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.3389/fphar.2021.621676",
"doi-asserted-by": "publisher",
"key": "ref29"
},
{
"DOI": "10.1101/2020.03.22.20040758",
"doi-asserted-by": "publisher",
"key": "ref30"
},
{
"DOI": "10.1016/j.tmaid.2020.101663",
"doi-asserted-by": "publisher",
"key": "ref31"
},
{
"DOI": "10.1016/j.tmaid.2020.101738",
"doi-asserted-by": "publisher",
"key": "ref32"
},
{
"DOI": "10.1001/jama.2020.8630",
"doi-asserted-by": "publisher",
"key": "ref33"
},
{
"DOI": "10.3399/bjgpopen20X101094",
"doi-asserted-by": "publisher",
"key": "ref34"
},
{
"DOI": "10.1002/bies.201200099",
"doi-asserted-by": "publisher",
"key": "ref35"
},
{
"DOI": "10.3390/diagnostics11040581",
"doi-asserted-by": "publisher",
"key": "ref36"
},
{
"DOI": "10.21037/atm-21-445",
"doi-asserted-by": "publisher",
"key": "ref37"
},
{
"DOI": "10.1111/bcp.14314",
"doi-asserted-by": "publisher",
"key": "ref38"
},
{
"DOI": "10.1183/13993003.00799-2020",
"doi-asserted-by": "publisher",
"key": "ref39"
},
{
"DOI": "10.3389/fmed.2021.648660",
"doi-asserted-by": "publisher",
"key": "ref40"
},
{
"DOI": "10.26508/lsa.202101049",
"doi-asserted-by": "publisher",
"key": "ref41"
},
{
"key": "ref42"
},
{
"key": "ref43",
"unstructured": "Clinical Managment of COVID-19—Intterim Guidance\nhttps://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwiD8On8jID3AhVDXRoKHcrIBOgQFnoECAsQAQ&url=https%3A%2F%2Fapps.who.int%2Firis%2Fbitstream%2Fhandle%2F10665%2F332196%2FWHO-2019-nCoV-clinical-2020.5-eng.pdf&usg=AOvVaw3KMolfl2CddTXJJH9o7N4J"
}
],
"reference-count": 43,
"references-count": 43,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2079-6382/11/4/498"
}
},
"score": 1,
"short-container-title": [
"Antibiotics"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Pharmacology (medical)",
"Infectious Diseases",
"Microbiology (medical)",
"General Pharmacology, Toxicology and Pharmaceutics",
"Biochemistry",
"Microbiology"
],
"subtitle": [],
"title": [
"Antiviral Used among Non-Severe COVID-19 Cases in Relation to Time till Viral Clearance: A Retrospective Cohort Study"
],
"type": "journal-article",
"volume": "11"
}
hafez