Vitamin D Status and SARS-CoV-2 Infection and COVID-19 Clinical Outcomes
et al., Frontiers in Public Health, doi:10.3389/fpubh.2021.736665, Dec 2021
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Meta analysis concluding that "patients with low vitamin D levels present an increased risk of ARDS requiring admission to intensive care unit (ICU) or mortality due to SARS-CoV-2 infection and a higher susceptibility to SARS-CoV-2 infection and related hospitalization".
20 meta-analyses show significant improvements with vitamin D treatment for mortality1-14,
mechanical ventilation1,5,6,11,15-17 ,
ICU admission1,3,5,6,9,11,13,15-19 ,
hospitalization11,
severity2,4,5,10,20 , and
cases7,19,20 .
Currently there are 136 vitamin D treatment for COVID-19 studies, showing 39% lower mortality [31‑45%], 17% lower ventilation [-5‑35%], 45% lower ICU admission [28‑57%], 22% lower hospitalization [13‑30%], and 17% fewer cases [9‑25%].
1.
Shah et al., Does vitamin D supplementation reduce COVID-19 severity? - a systematic review, QJM: An International Journal of Medicine, doi:10.1093/qjmed/hcac040.
2.
Nikniaz et al., The impact of vitamin D supplementation on mortality rate and clinical outcomes of COVID-19 patients: A systematic review and meta-analysis, Pharmaceutical Sciences, doi:10.34172/PS.2021.13.
3.
Hosseini et al., Effects of Vitamin D Supplementation on COVID-19 Related Outcomes: A Systematic Review and Meta-Analysis, Nutrients, doi:10.3390/nu14102134.
4.
D’Ecclesiis et al., Vitamin D and SARS-CoV2 infection, severity and mortality: A systematic review and meta-analysis, PLOS ONE, doi:10.1371/journal.pone.0268396.
5.
Xie et al., Micronutrient perspective on COVID-19: Umbrella review and reanalysis of meta-analyses, Critical Reviews in Food Science and Nutrition, doi:10.1080/10408398.2023.2174948.
6.
Hariyanto et al., Vitamin D supplementation and Covid‐19 outcomes: A systematic review, meta‐analysis and meta‐regression, Reviews in Medical Virology, doi:10.1002/rmv.2269.
7.
Begum et al., The Role of Vitamin D in COVID-19 Survival and Prevention: A Meta-analysis, Sudan Journal of Medical Sciences, doi:10.18502/sjms.v19i1.15776.
8.
Jamilian et al., The role of vitamin D in outcomes of critical care in COVID-19 patients: Evidence from an umbrella meta-analysis of interventional and observational studies, Public Health Nutrition, doi:10.1017/S1368980024000934.
9.
Sobczak et al., Effect of Vitamin D3 Supplementation on Severe COVID-19: A Meta-Analysis of Randomized Clinical Trials, Nutrients, doi:10.3390/nu16101402.
10.
Petrelli et al., Therapeutic and prognostic role of vitamin D for COVID-19 infection: A systematic review and meta-analysis of 43 observational studies, The Journal of Steroid Biochemistry and Molecular Biology, doi:10.1016/j.jsbmb.2021.105883.
11.
Asla et al., Vitamin D on COVID-19 Patients During the Pandemic, 2022. A Systematic Review and Meta-Analysis, Current Research in Nutrition and Food Science Journal, doi:10.12944/CRNFSJ.11.1.3.
12.
Kow et al., The impact of vitamin D administration on mortality in COVID-19 patients: a systematic review and meta-analysis of randomized controlled trials, Inflammopharmacology, doi:10.1007/s10787-024-01564-2.
13.
Zhang et al., The impact of supplementing vitamin D through different methods on the prognosis of COVID-19 patients: a systematic review and meta-analysis, Frontiers in Nutrition, doi:10.3389/fnut.2024.1441847.
14.
Doustmohammadian et al., Impact of vitamin D supplementation on COVID-19 mortality: A systematic review and meta-analysis, Nutrition Clinique et Métabolisme, doi:10.1016/j.nupar.2025.12.001.
15.
Meng et al., The role of vitamin D in the prevention and treatment of SARS-CoV-2 infection: A meta-analysis of randomized controlled trials, Clinical Nutrition, doi:10.1016/j.clnu.2023.09.008.
16.
Yang et al., Therapeutic effects of vitamin D supplementation on COVID-19 aggravation: a systematic review and meta-analysis of randomized controlled trials, Frontiers in Pharmacology, doi:10.3389/fphar.2024.1367686.
17.
Szarpak et al., Vitamin D supplementation to treat SARS-CoV-2 positive patients. Evidence from meta-analysis, Cardiology Journal, doi:10.5603/CJ.a2021.0122.
18.
Tentolouris et al., The effect of vitamin D supplementation on mortality and intensive care unit admission of COVID-19 patients. A systematic review, meta-analysis and meta-regression, Diabetes/Metabolism Research and Reviews, doi:10.1002/dmrr.3517.
Chiodini et al., 22 Dec 2021, peer-reviewed, 13 authors.
Vitamin D Status and SARS-CoV-2 Infection and COVID-19 Clinical Outcomes
Frontiers in Public Health, doi:10.3389/fpubh.2021.736665
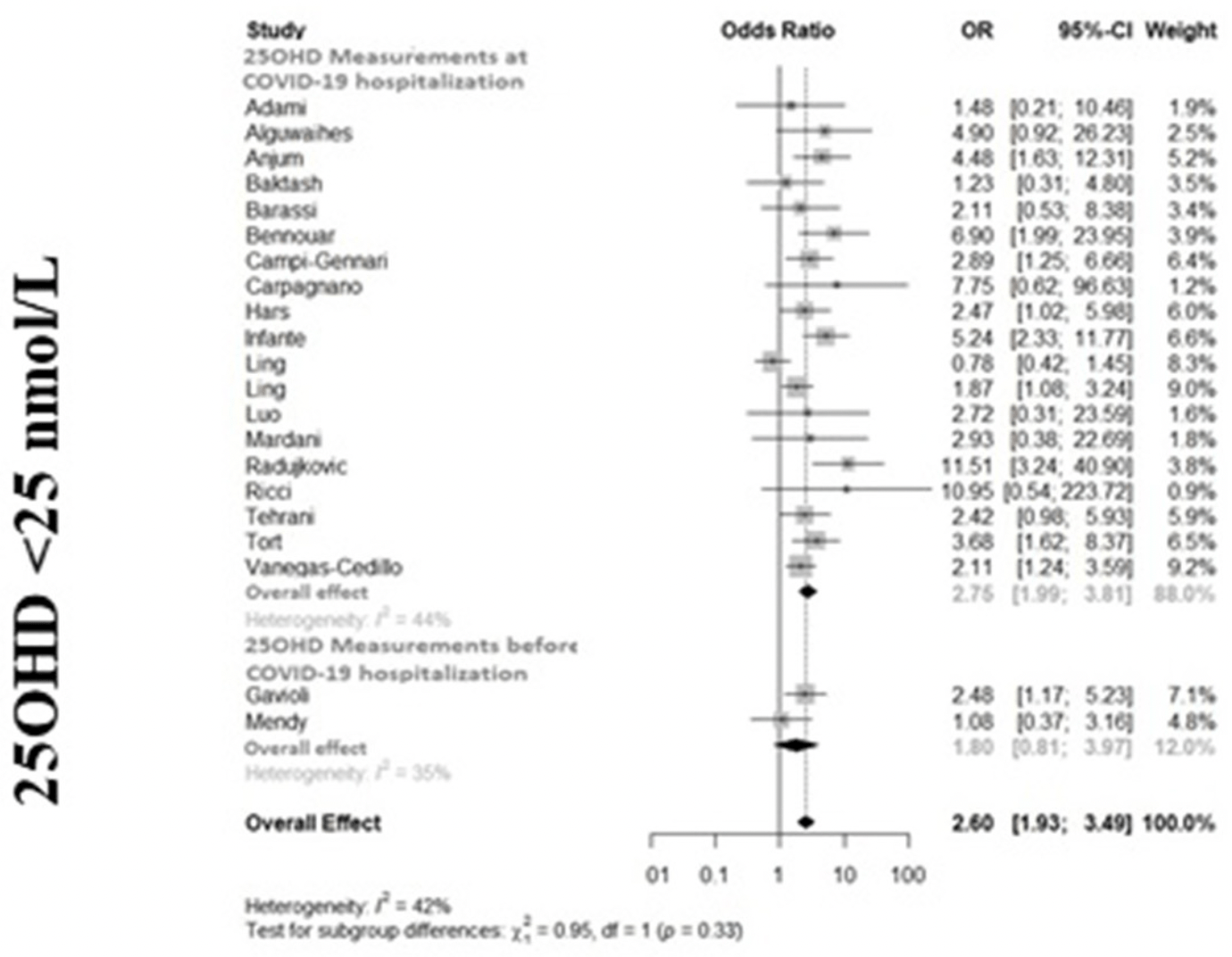
Background: Several studies suggest an association between serum 25-hydroxyvitamin D (25OHD) and the outcomes of Severe Acute Respiratory Syndrome Corona-Virus-2 (SARS-CoV-2) infection, in particular Coronavirus Disease-2019 (COVID-19) related severity and mortality. The aim of the present meta-analysis was to investigate whether vitamin D status is associated with the COVID-19 severity, defined as ARDS requiring admission to intensive care unit (ICU) or mortality (primary endpoints) and with the susceptibility to SARS-CoV-2 and COVID-19-related hospitalization (secondary endpoints). Methods: A search in PubMed, ScienceDirect, Web of Science, Google Scholar, Scopus, and preprints repositories was performed until March 31th 2021 to identify all original observational studies reporting association measures, or enough data to calculate them, between Vitamin D status (insufficiency <75, deficiency <50, or severe deficiency <25 nmol/L) and risk of SARS-CoV-2 infection, COVID-19 hospitalization, ICU admission, or death during COVID-19 hospitalization. Findings: Fifty-four studies (49 as fully-printed and 5 as pre-print publications) were included for a total of 1,403,715 individuals. The association between vitamin D status and SARS-CoV2 infection, COVID-19 related hospitalization, COVID-19 related ICU admission, and COVID-19 related mortality was reported in 17, 9, 27, and 35 studies, respectively. Severe deficiency, deficiency and insufficiency of vitamin D were all associated with ICU admission (odds ratio [OR], 95% confidence intervals [95%CIs]:
SUPPLEMENTARY MATERIAL The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh. 2021.736665/full#supplementary-material Supplementary Figure 1
Conflict of Interest: IC received speaker fees from HRA Pharma, Corcept Therapeutics, Eli-Lilly, Amgen, and UCB. DG received honoraria and/or speaker fees from Amgen, Celgene, Eli-Lilly, MSD-italia, Organon, and UCB. DM received honoraria form UCB Pharma and Savio Pharma. GA has received advisory board honoraria and consultancy fees from Theramex. CE-V has received advisory board honoraria from Kyowa Kirin, Sandoz. MR has received advisory board honoraria, consultancy fees, and/or speaker fees from Abiogen, Amgen, Abbvie, BMS, Eli-Lilly, Galapagos, Menarini, MSD, Novartis, Pfizer, Sandoz, Theramex, and UCB. LP received consultancy fees, and/or speaker fees from Merck, Sandoz, Recordati. LG received honoraria from Sandoz and Kyowa Kirin. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Abdollahi, Salehinia, Badeli, Karimi, Gandomkar et al., The biochemical parameters and Vitamin D levels in ICU patients with COVID-19: a cross-sectional study, Endocr Metab Immune Disord Drug Targets, doi:10.2174/1871530321666210316103403
Abrishami, Dalili, Torbati, Asgari, Arab-Ahmadi et al., Possible association of vitamin D status with lung involvement and outcome in patients with COVID-19: a retrospective study, Eur J Nutr, doi:10.1007/s00394-020-02411-0
Adami, Giollo, Fassio, Benini, Bertoldo et al., Vitamina D e gravità della malattia da coronavirus 19 (COVID-19), Reumatismo, doi:10.4081/reumatismo.2020.1333
Agraz-Cibrian, U-Is, 25-Dihydroxyvitamin D3 induces formation of neutrophil extracellular trap-like structures and modulates the transcription of genes whose products are neutrophil extracellular trap-associated proteins: a pilot study, Steroids, doi:10.1016/j.steroids.2018.11.001
Ahmadpoor, Rostaing, Why the immune system fails to mount an adaptive immune response to a COVID-19 infection, Transpl Int, doi:10.1111/tri.13611
Aihara, Azuma, Akaike, Ikeda, Yamashita et al., Disruption of nuclear vitamin D receptor gene causes enhanced thrombogenicity in mice, J Biol Chem, doi:10.1074/jbc.M404865200
Alguwaihes, Sabico, Hasanato, Sofani, Megdad et al., Severe vitamin D deficiency is not related to SARS CoV 2 infection but may increase mortality risk in hospitalized adults: a retrospective casecontrol study in an Arab Gulf country, Aging Clin Exp Res, doi:10.1007/s40520-021-01831-0
Alipio, Vitamin D supplementation could possibly improve clinical outcomes of patients infected with coronavirus-2019 (COVID-2019), SSRN Electron J, doi:10.2139/ssrn.3571484
Ames, Grant, Willett, Does the high prevalence of vitamin D deficiency in African Americans contribute to health disparities?, Nutrients, doi:10.3390/nu13020499
Amrein, Scherkl, Hoffmann, Neuwersch-Sommeregger, Köstenberger et al., Vitamin D deficiency 2.0: an update on the current status worldwide, Eur J Clin Nutr, doi:10.1038/s41430-020-0558-y
Angelidi, Belanger, Lorinsky, Karamanis, Chamorro-Pareja et al., Vitamin D status is associated with in-hospital mortality and mechanical ventilation: a cohort of COVID-19 hospitalized patients, Mayo Clin Proc, doi:10.1016/j.mayocp.2021.01.001
Anjum, Suleman, Afridi, Yasmeen, Shah et al., None, Pakistan Journal of Medical and Health Sciences
Annweiler, Corvaisier, Gautier, Dubée, Legrand et al., Vitamin D supplementation associated to better survival in hospitalized frail elderly COVID-19 patients: the GERIA-COVID quasi-experimental study, Nutrients, doi:10.3390/nu12113377
Arvinte, Singh, Marik, Serum levels of vitamin C and Vitamin D in a cohort of critically ill COVID-19 patients of a North American Community hospital intensive care unit in may 2020: a pilot study, Med Drug Discov, doi:10.1016/j.medidd.2020.100064
Baktash, Hosack, Shah, Kandiah, Van Den Abbeele, Vitamin D status and outcomes for hospitalised older patients with COVID-19, Postgrad Med J, doi:10.1136/postgradmedj-2020-138712
Barassi, Pezzilli, Mondoni, Rinaldo, Davì et al., Vitamin D in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) patients with non-invasive ventilation support, Panminerva Med, doi:10.23736/S0031-0808.21.04277-4
Basaran, Adas, Gokden, Turgut, Yildirmak et al., The relationship between vitamin D and the severity of COVID-19, Bratisl Med J, doi:10.4149/BLL_2021_034
Bennouar, Cherif, Kessirac, Bennouar, Abdia, Vitamin D deficiency and low serum calcium as predictors of poor prognosis in patients with severe COVID-19, J Am Coll Nutr, doi:10.1080/07315724.2020.1856013
Borsche, Glauner, Mendel, COVID-19 mortality risk correlates inversely with Vitamin D3 status, and a mortality rate close to zero could theoretically be achieved at 50 ng/mL 25(OH)D3: Results of a systematic review and meta-analysis, Nutrients, doi:10.3390/nu13103596
Bouillon, Marcocci, Carmeliet, White, Hughes et al., Skeletal and extraskeletal actions of Vitamin D: current evidence and outstanding questions, Endocr Rev, doi:10.1210/er.2018-00126
Brandão, Chiamolera, Biscolla, Lima, Junior et al., No association between vitamin D status and COVID-19 infection in São Paulo, Brazil, Arch Endocrinol Metab, doi:10.20945/2359-3997000000343
Campi, Gennari, Merlotti, Mingiano, Frosali et al., Vitamin D and COVID-19 severity and related mortality: a prospective study in Italy, BMC Infect Dis, doi:10.1186/s12879-021-06281-7
Carpagnano, Lecce, Quaranta, Zito, Buonamico et al., Vitamin D deficiency as a predictor of poor prognosis in patients with acute respiratory failure due to COVID-19, J Endocrinol Invest, doi:10.1007/s40618-020-01370-x
Castillo, Costa, Barrios, Díaz, Miranda et al., Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: a pilot randomized clinical study, J Steroid Biochem Mol Biol, doi:10.1016/j.jsbmb.2020.105751
Cereda, Bogliolo, Klersy, Lobascio, Masi et al., Vitamin D 25OH deficiency in COVID-19 patients admitted to a tertiary referral hospital, Clin Nutr, doi:10.1016/j.clnu.2020.10.055
Chang, Ding, Freund, Johnson, Schwarz et al., Prior diagnoses and medications as risk factors for COVID-19 in a Los Angeles Health System, medRxiv, doi:10.1101/2020.07.03.20145581
Charoenngam, Shirvani, Holick, Vitamin D and its potential benefit for the COVID-19 pandemic, Endocr Pract, doi:10.1016/j.eprac.2021.03.006
Charoenngam, Shirvani, Reddy, Vodopivec, Apovian et al., Association of Vitamin D status with hospital morbidity and mortality in adult hospitalized patients with COVID-19, Endocr Pract, doi:10.1016/j.eprac.2021.02.013
Cianferotti, Bertoldo, Bischoff-Ferrari, Bruyere, Cooper et al., Vitamin D supplementation in the prevention and management of major chronic diseases not related to mineral homeostasis in adults: research for evidence and a scientific statement from the European society for clinical and economic aspects of osteoporosis, Endocrine, doi:10.1007/s12020-017-1290-9
Cortegiani, Catalisano, Ippolito, Giarratano, Absalom et al., Retracted papers on SARS-CoV-2 and COVID-19, Br J Anaesth, doi:10.1016/j.bja.2021.01.008
Cuñat, Ojeda, Calvo, Vitamin D deficiency in critically ill patients diagnosed with COVID−19. Are we doing enough? A retrospective analysis of 226 patients, Research Square, doi:10.21203/rs.3.rs-30390/v1
D'avolio, Avataneo, Manca, Cusato, Nicolò et al., 25-hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2, Nutrients, doi:10.3390/nu12051359
Dancer, Parekh, Lax, Souza, Zheng et al., Vitamin D deficiency contributes directly to the acute respiratory distress syndrome (ARDS), Thorax, doi:10.1136/thoraxjnl-2014-206680
Darling, Ahmadi, Ward, Harvey, Alves et al., Vitamin D status, body mass index, ethnicity and COVID-19: Initial analysis of the first-reported UK Biobank COVID-19 positive cases (n 580) compared with negative controls, medRxiv, doi:10.1101/2020.04.29.20084277
Demir, Demir, Aygun, Vitamin D deficiency is associated with COVID-19 positivity and the severity of the disease, J Med Virol, doi:10.1002/jmv.26832
Dersimonian, Laird, Meta-analysis in clinical trials, Control Clin Trials, doi:10.1016/0197-2456(86)90046-2
Egger, Smith, Schneider, Minder, Bias in metaanalysis detected by a simple, graphical test, BMJ, doi:10.1136/bmj.315.7109.629
Faniyi, Lugg, Faustini, Webster, Duffy et al., Vitamin D status and seroconversion for COVID-19 in UK healthcare workers who isolated for COVID-19 like symptoms during the 2020 pandemic, Eur Respir J, doi:10.1101/2020.10.05.20206706
Faul, Kerley, Love, 'neill, Cody et al., Vitamin d deficiency and ards after sars-cov-2 infection, Ir Med J
Ferrari, Locatelli, No significant association between vitamin D and COVID-19. a retrospective study from a northern Italian hospital, Int J Vitam Nutr Res, doi:10.1024/0300-9831/a000687
Gaudio, Murabito, Agodi, Montineri, Castellino et al., Vitamin D levels are reduced at the time of hospital admission in sicilian SARS-CoV-2-positive patients, Int J Environ Res Public Health, doi:10.3390/ijerph18073491
Gavioli, Miyashita, Hassaneen, Siau, An evaluation of serum 25-Hydroxy vitamin D levels in patients with COVID-19 in New York City, J Am Coll Nutr, doi:10.1080/07315724.2020.1869626
Ghelani, Alesi, Mousa, Vitamin D COVID-19: an overview of recent evidence, Int J Mol Sci, doi:10.3390/ijms221910559
Godlee, Editor's Choice COVID-19: transparency and communication are key, BMJ, doi:10.1136/bmj.m4764
Griffin, Hewison, Hopkin, Kenny, Quinton et al., Vitamin D and COVID-19: evidence and recommendations for supplementation, R Soc Open Sci, doi:10.1098/rsos.201912
Hansdottir, Monick, Hinde, Lovan, Look et al., Respiratory epithelial cells convert inactive vitamin d to its active form: potential effects on host defense, J Immunol, doi:10.4049/jimmunol.181.10.7090
Hars, Mendes, Serratrice, Herrmann, Gold et al., Sex-specific association between vitamin D deficiency and COVID-19 mortality in older patients, Osteoporos Int, doi:10.1007/s00198-020-05677-6
Hastie, Mackay, Ho, Celis-Morales, Katikireddi et al., Vitamin D concentrations and COVID-19 infection in UK Biobank, Diabetes Metab Syndr Clin Res Rev, doi:10.1016/j.dsx.2020.04.050
Hastie, Pell, Sattar, Vitamin D and COVID-19 infection and mortality in UK Biobank, Eur J Nutr, doi:10.1007/s00394-020-02372-4
Hernández, Nan, Fernandez-Ayala, García-Unzueta, Hernández-Hernández et al., Vitamin d status in hospitalized patients with Sars-Cov-2 infection, J Clin Endocrinol Metab, doi:10.1210/clinem/dgaa733
Higgins, Thompson, Quantifying heterogeneity in a meta-analysis, Stat Med, doi:10.1002/sim.1186
Holick, Binkley, Bischoff-Ferrari, Gordon, Hanley et al., Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline, J Clin Endocrinol Metab, doi:10.1210/jc.2011-0385
Hosack, Baktash, Mandal, Missouris, Prognostic implications of vitamin D in patients with COVID-19, Eur J Nutr, doi:10.1007/s00394-020-02429-4
Hu, Guo, Zhou, Shi, Characteristics of SARS-CoV-2 and COVID-19, Nat Rev Microbiol, doi:10.1038/s41579-020-00459-7
Huang, Soleimani, Herasevich, Pinevich, Pennington et al., Clinical characteristics, treatment, and outcomes of critically ill patients with COVID-19: a scoping review, Mayo Clin Proc, doi:10.1016/j.mayocp.2020.10.022
Im, Je, Baek, Chung, Yoon Kwon et al., Nutritional status of patients with COVID-19, Int J Infect Dis, doi:10.1016/j.ijid.2020.08.018
Infante, Buoso, Pieri, Lupisella, Nuccetelli et al., Low Vitamin D status at admission as a risk factor for poor survival in hospitalized patients with COVID-19: an Italian retrospective study, J Am Coll Nutr, doi:10.1080/07315724.2021.1877580
Jain, Chaurasia, Sengar, Singh, Mahor et al., Analysis of vitamin D level among asymptomatic and critically ill COVID -19 patients and its correlation with inflammatory markers, Sci Rep, doi:10.1038/s41598-020-77093-z
Jayawardena, Jeyakumar, Francis, Misra, Impact of the vitamin D deficiency on COVID-19 infection and mortality in Asian countries, Diabetes Metab Syndr, doi:10.1016/j.dsx.2021.03.006
Jeng, Yamshchikov, Judd, Blumberg, Martin et al., Alterations in vitamin D status and antimicrobial peptide levels in patients in the intensive care unit with sepsis, J Transl Med, doi:10.1186/1479-5876-7-28
Jevalikar, Mithal, Singh, Sharma, Farooqui et al., Lack of association of baseline 25-hydroxyvitamin D levels with disease severity and mortality in Indian patients hospitalized for COVID-19, Sci Rep, doi:10.1038/s41598-021-85809-y
Jolliffe, Camargo, Jr, Sluyter, Aglipay et al., Vitamin D supplementation to prevent acute respiratory infections: a systematic review and meta-analysis of aggregate data from randomised controlled trials, Lancet Diabetes Endocrinol
Karahan, Katkat, Impact of serum 25(OH) Vitamin D level on mortality in patients with COVID-19 in Turkey, J Nutr Heal Aging, doi:10.1007/s12603-020-1479-0
Karonova, Andreeva, Vashukova, serum 25(OH)D level in patients with COVID-19, J Infektologii, doi:10.22625/2072-6732-2020-12-3-21-27
Katz, Yue, Xue, Increased risk for COVID-19 in patients with vitamin D deficiency, Nutrition, doi:10.1016/j.nut.2020.111106
Kaufman, Niles, Kroll, Bi, Holick, SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels, PLoS One, doi:10.1371/journal.pone.0239252
Kazemi, Mohammadi, Aghababaee, Golzarand, Clark et al., Association of Vitamin D status with SARS-CoV-2 infection or COVID-19 severity: a systematic review and meta-analysis, Adv Nutr, doi:10.1093/advances/nmab012
Laird, Rhodes, Kenny, Vitamin D and inflammation: potential implications for severity of COVID-19, Ir Med J
Lau, Majumder, Torabi, Saeg, Hoffman et al., Vitamin D insufficiency is prevalent in severe COVID-19, medRxiv, doi:10.1101/2020.04.24.20075838
Li, Cao, Yang, Zhang, Xu et al., Metabolic healthy obesity, Vitamin D status, and risk of COVID-19, Aging Dis, doi:10.14336/AD.2020.1108
Ling, Broad, Murphy, Pappachan, Pardesi-Newton et al., High-dose cholecalciferol booster therapy is associated with a reduced risk of mortality in patients with COVID-19: a cross-sectional multi-centre observational study, Nutrients, doi:10.3390/nu12123799
Liu, Sun, Wang, Zhang, Zhao et al., Low vitamin D status is associated with coronavirus disease 2019 outcomes: a systematic review and meta-analysis, Int J Infect Dis, doi:10.1016/j.ijid.2020.12.077
Lohia, Nguyen, Patel, Kapur, Exploring the link between vitamin D and clinical outcomes in COVID-19, Am J Physiol Endocrinol Metab, doi:10.1152/ajpendo.00517.2020
Long, Liu, Deng, Wu, Deng et al., Antibody responses to SARS-CoV-2 in patients with COVID-19, Nat Med, doi:10.1038/s41591-020-0897-1
Louw, Werbeck, Louw, Kotze, Cooper et al., Blood vitamin concentrations during the acute-phase response, Crit Care Med, doi:10.1097/00003246-199207000-00007
Luo, Liao, Shen, Li, Cheng, Vitamin D deficiency is inversely associated with COVID-19 incidence and disease severity in Chinese People, J Nutr, doi:10.1093/jn/nxaa332
Macaya, Espejo, Valls, Fernández-Ortiz, Del Castillo et al., Interaction between age and vitamin d deficiency in severe COVID-19 infection, Nutr Hosp, doi:10.20960/nh.03193
Maghbooli, Sahraian, Ebrahimi, Pazoki, Kafan et al., Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection, PLoS One, doi:10.1371/journal.pone.0239799
Manios, Moschonis, Lambrinou, Tsoutsoulopoulou, Binou et al., A systematic review of vitamin D status in southern European countries, Eur J Nutr, doi:10.1007/s00394-017-1564-2
Mardani, Alamdary, Nasab, Gholami, Ahmadi et al., Association of vitamin D with the modulation of the disease severity in COVID-19, Virus Res, doi:10.1016/j.virusres.2020.198148
Martineau, Jolliffe, Hooper, Greenberg, Aloia et al., Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data, BMJ, doi:10.1136/bmj.i6583
Mazziotti, Lavezzi, Brunetti, Mirani, Favacchio et al., Humanitas COVID19 task force. Vitamin D deficiency, secondary hyperparathyroidism and respiratory insufficiency in hospitalized patients with COVID-19, J Endocrinol Invest, doi:10.1007/s40618-021-01535-2
Mccullough, Lehrer, Amend, Daily oral dosing of vitamin D3 using 5000 TO 50,000 international units a day in long-term hospitalized patients: insights from a seven year experience, Steroid Biochem Mol Biol, doi:10.1016/j.jsbmb.2018.12.010
Meltzer, Best, Zhang, Vokes, Arora et al., Association of Vitamin D status and other clinical characteristics with COVID-19 test results, JAMA Netw Open, doi:10.1001/jamanetworkopen.2020.19722
Mendy, Apewokin, Wells, Morrow, Factors associated with hospitalization and disease severity in a racially and ethnically diverse population of COVID-19 Patients, medRxiv, doi:10.1101/2020.06.25.20137323
Merzon, Tworowski, Gorohovski, Vinker, Cohen et al., Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study, FEBS J, doi:10.1111/febs.15495
Mok, Ng, Ahidjo, Lee, Loe et al., Calcitriol, the active form of vitamin D, is a promising candidate for COVID-19 prophylaxis, bioRxiv, doi:10.1101/2020.06.21.162396
Munshi, Hussein, Toraih, Elshazli, Jardak et al., Vitamin D insufficiency as a potential culprit in critical COVID-19 patients, J Med Virol, doi:10.1002/jmv.26360
Murai, Fernandes, Sales, Pinto, Goessler et al., Effect of a single high dose of Vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: a randomized clinical trial, JAMA, doi:10.1001/jama.2020.26848
Nidadavolu, Walston, Underlying vulnerabilities to the cytokine storm and adverse COVID-19 outcomes in the aging immune system, J Gerontol A Biol Sci Med Sci, doi:10.1093/gerona/glaa209
Nogues, Ovejero, Pineda-Moncusí, Bouillon, Arenas et al., Calcifediol treatment and COVID-19-related outcomes, J Clin Endocrinol Metab, doi:10.1210/clinem/dgab405
Ohsawa, Koyama, Yamamoto, Hirosawa, Kamei et al., 1alpha,25-dihydroxyvitamin D(3) its potent synthetic analogs downregulate tissue factor upregulate thrombomodulin expression in monocytic cells, Circulation, doi:10.1161/01.CIR.102.23.2867
Orchard, Baldry, Nasim-Mohi, Monck, Saeed et al., Vitamin-D levels and intensive care unit outcomes of a cohort of critically ill COVID-19 patients, Clin Chem Lab Med, doi:10.1515/cclm-2020-1567
Page, Mckenzie, Bossuyt, Boutron, Hoffmann et al., The PRISMA 2020 statement: an updated guideline for reporting systematic reviews, BMJ, doi:10.1016/j.ijsu.2021.105906
Pal, Banerjee, Bhadada, Shetty, Singh et al., Vitamin D supplementation and clinical outcomes in COVID-19: a systematic review and meta-analysis, J Endocrinol Invest, doi:10.1007/s40618-021-01614-4
Panagiotou, Tee, Ihsan Y Athar, Marchitelli, Kelly, Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalized with COVID-19 are associated with greater disease severity, Clin Endocrinol, doi:10.1111/cen.14276
Pereira, Damascena, Azevedo, De Almeida Oliveira, Da et al., Vitamin D deficiency aggravates COVID-19: systematic review and meta-analysis, Crit Rev Food Sci Nutr, doi:10.1080/10408398.2020.1841090
Pinzon, Pradana, Vitamin D deficiency among patients with COVID-19: case series and recent literature review, Trop Med Health, doi:10.1186/s41182-020-00277-w
Pizzini, Aichner, Sahanic, Böhm, Egger et al., Impact of vitamin d deficiency on COVID-19-a prospective analysis from the COVID registry, Nutrients, doi:10.3390/nu12092775
Quesada-Gomez, Entrenas-Castillo, Bouillon, Vitamin D receptor stimulation to reduce acute respiratory distress syndrome (ARDS) in patients with coronavirus SARS-CoV-2 infections, J Steroid Biochem Mol Biol, doi:10.1016/j.jsbmb.2020.105719
Quraishi, Bittner, Blum, Hutter, Camargo, Association between preoperative 25-hydroxyvitamin D level and hospital-acquired infections following Roux-en-Y gastric bypass surgery, JAMA Surg, doi:10.1001/jamasurg.2013.3176
Quraishi, Bittner, Christopher, Camargo, Vitamin D status and community-acquired pneumonia: results from the third National Health and Nutrition Examination Survey, PLoS One, doi:10.1371/journal.pone.0081120
Radujkovic, Hippchen, Tiwari-Heckler, Dreher, Boxberger, Vitamin D deficiency and outcome of COVID-19 patients, Nutrients, doi:10.3390/nu12092757
Raharusuna, Priambada, Budiarti, Patterns of mortality and vitamin D : an indonesian study, medRxiv, doi:10.2139/ssrn.3585561
Raisi-Estabragh, Mccracken, Bethell, Cooper, Cooper et al., Greater risk of severe COVID-19 in Black, Asian and Minority Ethnic populations is not explained by cardiometabolic, socioeconomic or behavioural factors, or by 25(OH)-vitamin D status: study of 1326 cases from the UK Biobank, J Public Heal, doi:10.1093/pubmed/fdaa095
Reid, Knox, Talwar, Reilly, Blackwell et al., Acute changes in the systemic inflammatory response is associated with transient decreases in circulating 25-hydroxyvitamin D concentrations following elective knee arthoplasty, Ann Clin Biochem, doi:10.1016/S1744-1161(10)70509-3
Ricci, Pagliuca, 'ascanio, Innammorato, Vitis et al., Circulating Vitamin D levels status and clinical prognostic indices in COVID-19 patients, Respir Res, doi:10.1186/s12931-021-01666-3
Schultze, Aschenbrenner, COVID-19 and the human innate immune system, Cell, doi:10.1016/j.cell.2021.02.029
Smet, Smet, Herroelen, Gryspeerdt, Martens, Vitamin D deficiency as risk factor for severe COVID-19: a convergence of two pandemics, Am J Clin Pathol, doi:10.1101/2020.05.01.20079376
Szeto, Zucker, Lasota, Rubin, Walker et al., Vitamin D status and COVID-19 clinical outcomes in hospitalized patients, Endocr Res, doi:10.1080/07435800.2020.1867162
Tehrani, Khabiri, Moradi, Mosavat, Khabiri, Evaluation of vitamin D levels in COVID-19 patients referred to Labafinejad hospital in Tehran and its relationship with disease severity and mortality, Clin Nutr ESPEN, doi:10.1016/j.clnesp.2021.01.014
Tort, Mercado, Cuazitl, Puente Nieto, Pérez, La deficiencia de vitamina D es un factor de riesgo de mortalidad en pacientes con COVID-19, Rev Sanid Milit, doi:10.35366/93773
Vanegas-Cedillo, Bello-Chavolla, Ramírez-Pedraza, Encinas, Carrión et al., Serum Vitamin 1 D levels are associated with increased COVID-19 2 severity and mortality independent of visceral adiposity, medRxiv
Vasheghani, Jannati, Baghaei, Rezaei, Marjani, The association of 25 (OH) Vitamin D levels and severity and outcome of COVID-19: a crosssectional study, Sci Rep, doi:10.21203/rs.3.rs-141034/v1
Vassiliou, Jahaj, Pratikaki M Orfanos, Dimopoulou, Kotanidou, Low 25-Hydroxyvitamin D levels on admission to the intensive care unit may predispose COVID-19 pneumonia patients to a higher 28-day mortality risk: a pilot study on a Greek ICU cohort, Nutrients, doi:10.3390/nu12123773
Walk, Vitamin D -contrary to vitamin K -does not associate with clinical outcome in hospitalized COVID-19 patients, medRxiv, doi:10.1101/2020.11.07.20227512
Wells, Shea, Connell, Peterson, Welch et al., The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses
Xu, Yang, Chen, Luo, Zhang et al., Vitamin D alleviates lipopolysaccharide-induced acute lung injury via regulation of the renin-angiotensin system, Mol Med Rep, doi:10.3892/mmr.2017.7546
Yazdanpanah, Hamblin, Rezaei, The immune system and COVID-19: friend or foe?, Life Sci, doi:10.1016/j.lfs.2020.117900
Ye, Tang, Liao, Shaw, Deng et al., Does serum Vitamin D level affect COVID-19 infection and its severity?-A case-control study, J Am Coll Nutr, doi:10.1080/07315724.2020.1826005
Zhou, Zhang, Qu, Coronavirus disease 2019. (COVID-19): a clinical update, Front Med, doi:10.1007/s11684-020-0767-8
DOI record:
{
"DOI": "10.3389/fpubh.2021.736665",
"ISSN": [
"2296-2565"
],
"URL": "http://dx.doi.org/10.3389/fpubh.2021.736665",
"abstract": "<jats:p><jats:bold>Background:</jats:bold> Several studies suggest an association between serum 25-hydroxyvitamin D (25OHD) and the outcomes of Severe Acute Respiratory Syndrome Corona-Virus-2 (SARS-CoV-2) infection, in particular Coronavirus Disease-2019 (COVID-19) related severity and mortality. The aim of the present meta-analysis was to investigate whether vitamin D status is associated with the COVID-19 severity, defined as ARDS requiring admission to intensive care unit (ICU) or mortality (primary endpoints) and with the susceptibility to SARS-CoV-2 and COVID-19-related hospitalization (secondary endpoints).</jats:p><jats:p><jats:bold>Methods:</jats:bold> A search in PubMed, ScienceDirect, Web of Science, Google Scholar, Scopus, and preprints repositories was performed until March 31th 2021 to identify all original observational studies reporting association measures, or enough data to calculate them, between Vitamin D status (insufficiency &lt;75, deficiency &lt;50, or severe deficiency &lt;25 nmol/L) and risk of SARS-CoV-2 infection, COVID-19 hospitalization, ICU admission, or death during COVID-19 hospitalization.</jats:p><jats:p><jats:bold>Findings:</jats:bold> Fifty-four studies (49 as fully-printed and 5 as pre-print publications) were included for a total of 1,403,715 individuals. The association between vitamin D status and SARS-CoV2 infection, COVID-19 related hospitalization, COVID-19 related ICU admission, and COVID-19 related mortality was reported in 17, 9, 27, and 35 studies, respectively. Severe deficiency, deficiency and insufficiency of vitamin D were all associated with ICU admission (odds ratio [OR], 95% confidence intervals [95%CIs]: 2.63, 1.45–4.77; 2.16, 1.43–3.26; 2.83, 1.74–4.61, respectively), mortality (OR, 95%CIs: 2.60, 1.93–3.49; 1.84, 1.26–2.69; 4.15, 1.76–9.77, respectively), SARS-CoV-2 infection (OR, 95%CIs: 1.68, 1.32–2.13; 1.83, 1.43–2.33; 1.49, 1.16–1.91, respectively) and COVID-19 hospitalization (OR, 95%CIs 2.51, 1.63–3.85; 2.38, 1.56–3.63; 1.82, 1.43–2.33). Considering specific subgroups (i.e., Caucasian patients, high quality studies, and studies reporting adjusted association estimates) the results of primary endpoints did not change.</jats:p><jats:p><jats:bold>Interpretations:</jats:bold> Patients with low vitamin D levels present an increased risk of ARDS requiring admission to intensive care unit (ICU) or mortality due to SARS-CoV-2 infection and a higher susceptibility to SARS-CoV-2 infection and related hospitalization.</jats:p>",
"alternative-id": [
"10.3389/fpubh.2021.736665"
],
"author": [
{
"affiliation": [],
"family": "Chiodini",
"given": "Iacopo",
"sequence": "first"
},
{
"affiliation": [],
"family": "Gatti",
"given": "Davide",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Soranna",
"given": "Davide",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Merlotti",
"given": "Daniela",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mingiano",
"given": "Christian",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fassio",
"given": "Angelo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Adami",
"given": "Giovanni",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Falchetti",
"given": "Alberto",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Eller-Vainicher",
"given": "Cristina",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rossini",
"given": "Maurizio",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Persani",
"given": "Luca",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zambon",
"given": "Antonella",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gennari",
"given": "Luigi",
"sequence": "additional"
}
],
"container-title": [
"Frontiers in Public Health"
],
"content-domain": {
"crossmark-restriction": true,
"domain": [
"frontiersin.org"
]
},
"created": {
"date-parts": [
[
2021,
12,
22
]
],
"date-time": "2021-12-22T06:14:35Z",
"timestamp": 1640153675000
},
"deposited": {
"date-parts": [
[
2021,
12,
22
]
],
"date-time": "2021-12-22T06:14:42Z",
"timestamp": 1640153682000
},
"funder": [
{
"DOI": "10.13039/501100003196",
"doi-asserted-by": "publisher",
"name": "Ministero della Salute"
}
],
"indexed": {
"date-parts": [
[
2021,
12,
22
]
],
"date-time": "2021-12-22T06:59:28Z",
"timestamp": 1640156368719
},
"is-referenced-by-count": 0,
"issn-type": [
{
"type": "electronic",
"value": "2296-2565"
}
],
"issued": {
"date-parts": [
[
2021,
12,
22
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
12,
22
]
],
"date-time": "2021-12-22T00:00:00Z",
"timestamp": 1640131200000
}
}
],
"link": [
{
"URL": "https://www.frontiersin.org/articles/10.3389/fpubh.2021.736665/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1965",
"original-title": [],
"prefix": "10.3389",
"published": {
"date-parts": [
[
2021,
12,
22
]
]
},
"published-online": {
"date-parts": [
[
2021,
12,
22
]
]
},
"publisher": "Frontiers Media SA",
"reference": [
{
"DOI": "10.1007/s11684-020-0767-8",
"article-title": "Coronavirus disease 2019. (COVID-19): a clinical update.",
"author": "Min Zhou",
"doi-asserted-by": "publisher",
"first-page": "126",
"journal-title": "Front Med.",
"key": "B1",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1038/s41579-020-00459-7",
"article-title": "Characteristics of SARS-CoV-2 and COVID-19",
"author": "Hu",
"doi-asserted-by": "publisher",
"first-page": "141",
"journal-title": "Nat Rev Microbiol.",
"key": "B2",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.1016/j.mayocp.2020.10.022",
"article-title": "Clinical characteristics, treatment, and outcomes of critically ill patients with COVID-19: a scoping review",
"author": "Huang",
"doi-asserted-by": "publisher",
"first-page": "183",
"journal-title": "Mayo Clin Proc.",
"key": "B3",
"volume": "96",
"year": "2021"
},
{
"DOI": "10.1007/s00394-017-1564-2",
"article-title": "A systematic review of vitamin D status in southern European countries",
"author": "Manios",
"doi-asserted-by": "publisher",
"first-page": "2001",
"journal-title": "Eur J Nutr.",
"key": "B4",
"volume": "57",
"year": "2018"
},
{
"article-title": "Vitamin D and inflammation: potential implications for severity of COVID-19",
"author": "Laird",
"first-page": "81",
"journal-title": "Ir Med J",
"key": "B5",
"volume": "113",
"year": "2020"
},
{
"DOI": "10.3390/nu13020499",
"article-title": "Does the high prevalence of vitamin D deficiency in African Americans contribute to health disparities?",
"author": "Ames",
"doi-asserted-by": "publisher",
"first-page": "499",
"journal-title": "Nutrients.",
"key": "B6",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1136/bmj.i6583",
"article-title": "Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data",
"author": "Martineau",
"doi-asserted-by": "publisher",
"first-page": "i6583",
"journal-title": "BMJ.",
"key": "B7",
"volume": "356",
"year": "2017"
},
{
"DOI": "10.1007/s12020-017-1290-9",
"article-title": "Vitamin D supplementation in the prevention and management of major chronic diseases not related to mineral homeostasis in adults: research for evidence and a scientific statement from the European society for clinical and economic aspects of osteoporosis",
"author": "Cianferotti",
"doi-asserted-by": "publisher",
"first-page": "245",
"journal-title": "Endocrine.",
"key": "B8",
"volume": "56",
"year": "2017"
},
{
"key": "B9",
"unstructured": ""
},
{
"DOI": "10.1016/S2213-8587(21)00051-6",
"article-title": "Vitamin D supplementation to prevent acute respiratory infections: a systematic review and meta-analysis of aggregate data from randomised controlled trials",
"author": "Jolliffe",
"doi-asserted-by": "crossref",
"first-page": "276",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "B10",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1210/er.2018-00126",
"article-title": "Skeletal and extraskeletal actions of Vitamin D: current evidence and outstanding questions",
"author": "Bouillon",
"doi-asserted-by": "publisher",
"first-page": "1109",
"journal-title": "Endocr Rev.",
"key": "B11",
"volume": "40",
"year": "2019"
},
{
"DOI": "10.1016/j.jsbmb.2020.105719",
"article-title": "Vitamin D receptor stimulation to reduce acute respiratory distress syndrome (ARDS) in patients with coronavirus SARS-CoV-2 infections",
"author": "Quesada-Gomez",
"doi-asserted-by": "publisher",
"first-page": "105719",
"journal-title": "J Steroid Biochem Mol Biol",
"key": "B12",
"volume": "202",
"year": "2020"
},
{
"DOI": "10.1101/2020.06.21.162396",
"article-title": "Calcitriol, the active form of vitamin D, is a promising candidate for COVID-19 prophylaxis",
"author": "Mok",
"doi-asserted-by": "publisher",
"journal-title": "bioRxiv.",
"key": "B13",
"year": "2021"
},
{
"DOI": "10.3390/nu12113377",
"article-title": "Vitamin D supplementation associated to better survival in hospitalized frail elderly COVID-19 patients: the GERIA-COVID quasi-experimental study",
"author": "Annweiler",
"doi-asserted-by": "publisher",
"first-page": "3377",
"journal-title": "Nutrients.",
"key": "B14",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1016/j.jsbmb.2020.105751",
"article-title": "Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: a pilot randomized clinical study",
"author": "Entrenas Castillo",
"doi-asserted-by": "publisher",
"first-page": "105751",
"journal-title": "J Steroid Biochem Mol Biol.",
"key": "B15",
"volume": "203",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.26848",
"article-title": "Effect of a single high dose of Vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: a randomized clinical trial",
"author": "Murai",
"doi-asserted-by": "publisher",
"first-page": "1053",
"journal-title": "JAMA.",
"key": "B16",
"volume": "325",
"year": "2021"
},
{
"DOI": "10.1080/10408398.2020.1841090",
"article-title": "Vitamin D deficiency aggravates COVID-19: systematic review and meta-analysis",
"author": "Pereira",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Crit Rev Food Sci Nutr.",
"key": "B17",
"volume": "4",
"year": "2020"
},
{
"DOI": "10.1002/jmv.26360",
"article-title": "Vitamin D insufficiency as a potential culprit in critical COVID-19 patients",
"author": "Munshi",
"doi-asserted-by": "publisher",
"first-page": "733",
"journal-title": "J Med Virol",
"key": "B18",
"volume": "93",
"year": "2020"
},
{
"DOI": "10.1093/advances/nmab012",
"article-title": "Association of Vitamin D status with SARS-CoV-2 infection or COVID-19 severity: a systematic review and meta-analysis",
"author": "Kazemi",
"doi-asserted-by": "publisher",
"first-page": "1636",
"journal-title": "Adv Nutr.",
"key": "B19",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1136/bmj.m4764",
"article-title": "Editor's Choice COVID-19: transparency and communication are key",
"author": "Godlee",
"doi-asserted-by": "publisher",
"first-page": "m4764",
"journal-title": "BMJ.",
"key": "B20",
"volume": "371",
"year": "2020"
},
{
"DOI": "10.1016/S1744-1161(10)70509-3",
"article-title": "Acute changes in the systemic inflammatory response is associated with transient decreases in circulating 25-hydroxyvitamin D concentrations following elective knee arthoplasty",
"author": "Reid",
"doi-asserted-by": "publisher",
"first-page": "95",
"journal-title": "Ann Clin Biochem.",
"key": "B21",
"volume": "47",
"year": "2010"
},
{
"DOI": "10.1097/00003246-199207000-00007",
"article-title": "Blood vitamin concentrations during the acute-phase response",
"author": "Louw",
"doi-asserted-by": "publisher",
"first-page": "934",
"journal-title": "Crit Care Med.",
"key": "B22",
"volume": "20",
"year": "1992"
},
{
"DOI": "10.1016/j.ijsu.2021.105906",
"article-title": "The PRISMA 2020 statement: an updated guideline for reporting systematic reviews",
"author": "Page",
"doi-asserted-by": "publisher",
"first-page": "105906",
"journal-title": "BMJ.",
"key": "B23",
"volume": "88",
"year": "2021"
},
{
"DOI": "10.1210/jc.2011-0385",
"article-title": "Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline",
"author": "Holick",
"doi-asserted-by": "publisher",
"first-page": "1911",
"journal-title": "J Clin Endocrinol Metab.",
"key": "B24",
"volume": "96",
"year": "2011"
},
{
"DOI": "10.1038/s41430-020-0558-y",
"article-title": "Vitamin D deficiency 2.0: an update on the current status worldwide.",
"author": "Amrein",
"doi-asserted-by": "publisher",
"first-page": "1498",
"journal-title": "Eur J Clin Nutr.",
"key": "B25",
"volume": "74",
"year": "2020"
},
{
"key": "B26",
"unstructured": "The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses\n WellsG\n SheaB\n O'ConnellD\n PetersonJ\n WelchV\n LososM\n 2009"
},
{
"DOI": "10.1016/0197-2456(86)90046-2",
"article-title": "Meta-analysis in clinical trials",
"author": "DerSimonian",
"doi-asserted-by": "publisher",
"first-page": "177",
"journal-title": "Control Clin Trials.",
"key": "B27",
"volume": "7",
"year": "1986"
},
{
"DOI": "10.1002/sim.1186",
"article-title": "Quantifying heterogeneity in a meta-analysis",
"author": "Higgins",
"doi-asserted-by": "publisher",
"first-page": "1539",
"journal-title": "Stat Med.",
"key": "B28",
"volume": "21",
"year": "2002"
},
{
"DOI": "10.1136/bmj.315.7109.629",
"article-title": "Bias in meta-analysis detected by a simple, graphical test",
"author": "Egger",
"doi-asserted-by": "publisher",
"first-page": "629",
"journal-title": "BMJ.",
"key": "B29",
"volume": "315",
"year": "1997"
},
{
"DOI": "10.2139/ssrn.3571484",
"article-title": "Vitamin D supplementation could possibly improve clinical outcomes of patients infected with coronavirus-2019 (COVID-2019)",
"author": "Alipio",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "SSRN Electron J.",
"key": "B30",
"volume": "2019",
"year": "2020"
},
{
"DOI": "10.2139/ssrn.3585561",
"article-title": "Patterns of mortality and vitamin D : an indonesian study",
"author": "Raharusuna",
"doi-asserted-by": "publisher",
"journal-title": "medRxiv",
"key": "B31",
"year": "2020"
},
{
"DOI": "10.1016/j.bja.2021.01.008",
"article-title": "Retracted papers on SARS-CoV-2 and COVID-19",
"author": "Cortegiani",
"doi-asserted-by": "publisher",
"first-page": "e155",
"journal-title": "Br J Anaesth.",
"key": "B32",
"volume": "126",
"year": "2021"
},
{
"DOI": "10.1016/j.medidd.2020.100064",
"article-title": "Serum levels of vitamin C and Vitamin D in a cohort of critically ill COVID- 19 patients of a North American Community hospital intensive care unit in may 2020: a pilot study",
"author": "Arvinte",
"doi-asserted-by": "publisher",
"first-page": "100064",
"journal-title": "Med Drug Discov.",
"key": "B33",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.21203/rs.3.rs-30390/v1",
"article-title": "Vitamin D deficiency in critically ill patients diagnosed with COVID−19. Are we doing enough? A retrospective analysis of 226 patients",
"author": "Cuñat",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Research Square.",
"key": "B34",
"year": "2020"
},
{
"DOI": "10.3390/nu12051359",
"article-title": "25-hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2",
"author": "D'Avolio",
"doi-asserted-by": "publisher",
"first-page": "1359",
"journal-title": "Nutrients",
"key": "B35",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1186/s41182-020-00277-w",
"article-title": "Vitamin D deficiency among patients with COVID-19: case series and recent literature review",
"author": "Pinzon",
"doi-asserted-by": "publisher",
"first-page": "102",
"journal-title": "Trop Med Health.",
"key": "B36",
"volume": "48",
"year": "2020"
},
{
"DOI": "10.3390/nu12092775",
"article-title": "Impact of vitamin d deficiency on COVID-19—a prospective analysis from the COVID registry",
"author": "Pizzini",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Nutrients.",
"key": "B37",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.3390/ijerph18073491",
"article-title": "Vitamin D levels are reduced at the time of hospital admission in sicilian SARS-CoV-2-positive patients",
"author": "Gaudio",
"doi-asserted-by": "publisher",
"first-page": "3491",
"journal-title": "Int J Environ Res Public Health",
"key": "B38",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0239252",
"article-title": "SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels",
"author": "Kaufman",
"doi-asserted-by": "publisher",
"first-page": "e0239252",
"journal-title": "PLoS One.",
"key": "B39",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1007/s40618-021-01535-2",
"article-title": "Humanitas COVID19 task force. Vitamin D deficiency, secondary hyperparathyroidism and respiratory insufficiency in hospitalized patients with COVID-19",
"author": "Mazziotti",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "J Endocrinol Invest.",
"key": "B40",
"volume": "5",
"year": "2021"
},
{
"DOI": "10.1016/j.dsx.2020.04.050",
"article-title": "Vitamin D concentrations and COVID-19 infection in UK Biobank",
"author": "Hastie",
"doi-asserted-by": "publisher",
"first-page": "561",
"journal-title": "Diabetes Metab Syndr Clin Res Rev.",
"key": "B41",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1007/s00394-020-02372-4",
"article-title": "Vitamin D and COVID-19 infection and mortality in UK Biobank",
"author": "Hastie",
"doi-asserted-by": "publisher",
"first-page": "545",
"journal-title": "Eur J Nutr.",
"key": "B42",
"volume": "60",
"year": "2020"
},
{
"DOI": "10.1101/2020.04.29.20084277",
"article-title": "Vitamin D status, body mass index, ethnicity and COVID-19: Initial analysis of the first-reported UK Biobank COVID-19 positive cases (n 580) compared with negative controls (n 723)",
"author": "Darling",
"doi-asserted-by": "publisher",
"journal-title": "medRxiv.",
"key": "B43",
"year": "2020"
},
{
"DOI": "10.1093/pubmed/fdaa095",
"article-title": "Greater risk of severe COVID-19 in Black, Asian and Minority Ethnic populations is not explained by cardiometabolic, socioeconomic or behavioural factors, or by 25(OH)-vitamin D status: study of 1326 cases from the UK Biobank",
"author": "Raisi-Estabragh",
"doi-asserted-by": "publisher",
"first-page": "451",
"journal-title": "J Public Heal",
"key": "B44",
"volume": "42",
"year": "2020"
},
{
"DOI": "10.14336/AD.2020.1108",
"article-title": "Metabolic healthy obesity, Vitamin D status, and risk of COVID-19",
"author": "Li",
"doi-asserted-by": "publisher",
"first-page": "61",
"journal-title": "Aging Dis.",
"key": "B45",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.2174/1871530321666210316103403",
"article-title": "The biochemical parameters and Vitamin D levels in ICU patients with COVID-19: a cross-sectional study",
"author": "Abdollahi",
"doi-asserted-by": "publisher",
"journal-title": "Endocr Metab Immune Disord Drug Targets.",
"key": "B46",
"year": "2021"
},
{
"DOI": "10.1007/s40520-021-01831-0",
"article-title": "Severe vitamin D deficiency is not related to SARS CoV 2 infection but may increase mortality risk in hospitalized adults: a retrospective case–control study in an Arab Gulf country",
"author": "Alguwaihes",
"doi-asserted-by": "publisher",
"first-page": "1415",
"journal-title": "Aging Clin Exp Res.",
"key": "B47",
"volume": "33",
"year": "2021"
},
{
"DOI": "10.20945/2359-3997000000343",
"article-title": "No association between vitamin D status and COVID-19 infection in São Paulo, Brazil",
"author": "Brandão",
"doi-asserted-by": "publisher",
"first-page": "381",
"journal-title": "Arch Endocrinol Metab.",
"key": "B48",
"volume": "65",
"year": "2021"
},
{
"DOI": "10.1186/s12879-021-06281-7",
"article-title": "Vitamin D and COVID-19 severity and related mortality: a prospective study in Italy",
"author": "Campi",
"doi-asserted-by": "publisher",
"first-page": "566",
"journal-title": "BMC Infect Dis",
"key": "B49",
"volume": "21",
"year": ""
},
{
"DOI": "10.1101/2020.07.03.20145581",
"article-title": "UCLA Health Data Mart Working Group, Daniel H Geschwind MJB, Pasaniuc B. Prior diagnoses and medications as risk factors for COVID-19 in a Los Angeles Health System 2020",
"author": "Chang",
"doi-asserted-by": "publisher",
"first-page": "2020",
"journal-title": "medRxiv",
"key": "B50",
"volume": "4",
"year": "2020"
},
{
"DOI": "10.1002/jmv.26832",
"article-title": "Vitamin D deficiency is associated with COVID-19 positivity and the severity of the disease",
"author": "Demir",
"doi-asserted-by": "publisher",
"first-page": "2992",
"journal-title": "J Med Virol.",
"key": "B51",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1101/2020.05.01.20079376",
"article-title": "Vitamin D deficiency as risk factor for severe COVID-19: a convergence of two pandemics",
"author": "De Smet",
"doi-asserted-by": "publisher",
"journal-title": "Am J Clin Pathol.",
"key": "B52",
"year": "2020"
},
{
"DOI": "10.1101/2020.10.05.20206706",
"article-title": "Vitamin D status and seroconversion for COVID-19 in UK healthcare workers who isolated for COVID-19 like symptoms during the 2020 pandemic",
"author": "Faniyi",
"doi-asserted-by": "publisher",
"first-page": "2004234",
"journal-title": "Eur Respir J",
"key": "B53",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1024/0300-9831/a000687",
"article-title": "No significant association between vitamin D and COVID-19. a retrospective study from a northern Italian hospital",
"author": "Ferrari",
"doi-asserted-by": "publisher",
"first-page": "200",
"journal-title": "Int J Vitam Nutr Res",
"key": "B54",
"volume": "91",
"year": "2020"
},
{
"DOI": "10.1210/clinem/dgaa733",
"article-title": "Vitamin d status in hospitalized patients with Sars-Cov-2 infection",
"author": "Hernández",
"doi-asserted-by": "publisher",
"first-page": "e1343",
"journal-title": "J Clin Endocrinol Metab.",
"key": "B55",
"volume": "106",
"year": "2020"
},
{
"DOI": "10.1016/j.nut.2020.111106",
"article-title": "Increased risk for COVID-19 in patients with vitamin D deficiency",
"author": "Katz",
"doi-asserted-by": "publisher",
"first-page": "111106",
"journal-title": "Nutrition.",
"key": "B56",
"volume": "84",
"year": "2020"
},
{
"DOI": "10.1016/j.ijid.2020.08.018",
"article-title": "Nutritional status of patients with COVID-19",
"author": "Im",
"doi-asserted-by": "publisher",
"first-page": "390",
"journal-title": "Int J Infect Dis",
"key": "B57",
"volume": "100",
"year": "2020"
},
{
"DOI": "10.1016/j.virusres.2020.198148",
"article-title": "Association of vitamin D with the modulation of the disease severity in COVID-19",
"author": "Mardani",
"doi-asserted-by": "publisher",
"first-page": "198148",
"journal-title": "Virus Res.",
"key": "B58",
"volume": "289",
"year": "2020"
},
{
"DOI": "10.1001/jamanetworkopen.2020.19722",
"article-title": "Association of Vitamin D status and other clinical characteristics with COVID-19 test results",
"author": "Meltzer",
"doi-asserted-by": "publisher",
"first-page": "e2019722",
"journal-title": "JAMA Netw Open.",
"key": "B59",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1111/febs.15495",
"article-title": "Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study",
"author": "Merzon",
"doi-asserted-by": "publisher",
"first-page": "3693",
"journal-title": "FEBS J.",
"key": "B60",
"volume": "287",
"year": "2020"
},
{
"DOI": "10.1080/07315724.2020.1826005",
"article-title": "Does serum Vitamin D level affect COVID-19 infection and its severity?-A case-control study.",
"author": "Ye",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "J Am Coll Nutr.",
"key": "B61",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.4149/BLL_2021_034",
"article-title": "The relationship between vitamin D and the severity of COVID-19",
"author": "Basaran",
"doi-asserted-by": "publisher",
"first-page": "200",
"journal-title": "Bratisl Med J.",
"key": "B62",
"volume": "122",
"year": "2021"
},
{
"DOI": "10.1080/07315724.2020.1869626",
"article-title": "An evaluation of serum 25-Hydroxy vitamin D levels in patients with COVID-19 in New York City",
"author": "Gavioli",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "J Am Coll Nutr.",
"key": "B63",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.20960/nh.03193",
"article-title": "Interaction between age and vitamin d deficiency in severe COVID-19 infection",
"author": "Macaya",
"doi-asserted-by": "publisher",
"first-page": "1039",
"journal-title": "Nutr Hosp.",
"key": "B64",
"volume": "37",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0239799",
"article-title": "Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection",
"author": "Maghbooli",
"doi-asserted-by": "publisher",
"first-page": "e0239799",
"journal-title": "PLoS One.",
"key": "B65",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1101/2020.06.25.20137323",
"article-title": "Factors associated with hospitalization and disease severity in a racially and ethnically diverse population of COVID-19 Patients",
"author": "Mendy",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "medRxiv.",
"key": "B66",
"year": "2020"
},
{
"DOI": "10.3390/nu12092757",
"article-title": "Vitamin D deficiency and outcome of COVID-19 patients",
"author": "Radujkovic",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Nutrients.",
"key": "B67",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.4081/reumatismo.2020.1333",
"article-title": "Vitamina D e gravità della malattia da coronavirus 19 (COVID-19)",
"author": "Adami",
"doi-asserted-by": "publisher",
"first-page": "189",
"journal-title": "Reumatismo.",
"key": "B68",
"volume": "72",
"year": "2021"
},
{
"DOI": "10.1016/j.mayocp.2021.01.001",
"article-title": "Vitamin D status is associated with in-hospital mortality and mechanical ventilation: a cohort of COVID-19 hospitalized patients",
"author": "Angelidi",
"doi-asserted-by": "publisher",
"first-page": "875",
"journal-title": "Mayo Clin Proc.",
"key": "B69",
"volume": "96",
"year": "2021"
},
{
"DOI": "10.1136/postgradmedj-2020-138712",
"article-title": "Vitamin D status and outcomes for hospitalised older patients with COVID-19",
"author": "Baktash",
"doi-asserted-by": "publisher",
"first-page": "442",
"journal-title": "Postgrad Med J.",
"key": "B70",
"volume": "97",
"year": "2020"
},
{
"DOI": "10.23736/S0031-0808.21.04277-4",
"article-title": "Vitamin D in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) patients with non-invasive ventilation support",
"author": "Barassi",
"doi-asserted-by": "publisher",
"journal-title": "Panminerva Med",
"key": "B71",
"year": "2021"
},
{
"DOI": "10.1007/s40618-020-01370-x",
"article-title": "Vitamin D deficiency as a predictor of poor prognosis in patients with acute respiratory failure due to COVID-19",
"author": "Carpagnano",
"doi-asserted-by": "publisher",
"first-page": "765",
"journal-title": "J Endocrinol Invest.",
"key": "B72",
"volume": "44",
"year": "2021"
},
{
"DOI": "10.1016/j.clnu.2020.10.055",
"article-title": "NUTRI-COVID19 IRCCS San Matteo Pavia Collaborative Group. Vitamin D 25OH deficiency in COVID-19 patients admitted to a tertiary referral hospital",
"author": "Cereda",
"doi-asserted-by": "publisher",
"first-page": "2469",
"journal-title": "Clin Nutr.",
"key": "B73",
"volume": "40",
"year": "2021"
},
{
"DOI": "10.1016/j.eprac.2021.02.013",
"article-title": "Association of Vitamin D status with hospital morbidity and mortality in adult hospitalized patients with COVID-19",
"author": "Charoenngam",
"doi-asserted-by": "publisher",
"first-page": "271",
"journal-title": "Endocr Pract",
"key": "B74",
"volume": "27",
"year": "2021"
},
{
"article-title": "Vitamin d deficiency and ards after sars-cov-2 infection",
"author": "Faul",
"first-page": "4",
"journal-title": "Ir Med J.",
"key": "B75",
"volume": "113",
"year": "2020"
},
{
"DOI": "10.1038/s41598-020-77093-z",
"article-title": "Analysis of vitamin D level among asymptomatic and critically ill COVID - 19 patients and its correlation with inflammatory markers",
"author": "Jain",
"doi-asserted-by": "publisher",
"journal-title": "Sci Rep",
"key": "B76",
"year": "2020"
},
{
"DOI": "10.1038/s41598-021-85809-y",
"article-title": "Lack of association of baseline 25-hydroxyvitamin D levels with disease severity and mortality in Indian patients hospitalized for COVID-19",
"author": "Jevalikar",
"doi-asserted-by": "publisher",
"first-page": "6258",
"journal-title": "Sci Rep.",
"key": "B77",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.22625/2072-6732-2020-12-3-21-27",
"article-title": "serum 25(OH)D level in patients with COVID-19",
"author": "Karonova",
"doi-asserted-by": "publisher",
"first-page": "21",
"journal-title": "J Infektologii.",
"key": "B78",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1101/2020.04.24.20075838",
"article-title": "Vitamin D insufficiency is prevalent in severe COVID-19",
"author": "Lau",
"doi-asserted-by": "publisher",
"journal-title": "medRxiv.",
"key": "B79",
"year": "2020"
},
{
"DOI": "10.1152/ajpendo.00517.2020",
"article-title": "Exploring the link between vitamin D and clinical outcomes in COVID-19",
"author": "Lohia",
"doi-asserted-by": "publisher",
"first-page": "E520",
"journal-title": "Am J Physiol Endocrinol Metab.",
"key": "B80",
"volume": "320",
"year": "2021"
},
{
"DOI": "10.1515/cclm-2020-1567",
"article-title": "Vitamin-D levels and intensive care unit outcomes of a cohort of critically ill COVID-19 patients",
"author": "Orchard",
"doi-asserted-by": "publisher",
"first-page": "1155",
"journal-title": "Clin Chem Lab Med.",
"key": "B81",
"volume": "59",
"year": "2021"
},
{
"DOI": "10.1111/cen.14276",
"article-title": "Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalized with COVID-19 are associated with greater disease severity",
"author": "Panagiotou",
"doi-asserted-by": "publisher",
"first-page": "508",
"journal-title": "Clin Endocrinol.",
"key": "B82",
"volume": "93",
"year": "2020"
},
{
"DOI": "10.1080/07435800.2020.1867162",
"article-title": "Vitamin D status and COVID-19 clinical outcomes in hospitalized patients",
"author": "Szeto",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Endocr Res.",
"key": "B83",
"volume": "30",
"year": "2020"
},
{
"article-title": "Serum Vitamin 1 D levels are associated with increased COVID-19 2 severity and mortality independent of visceral adiposity",
"author": "Vanegas-Cedillo",
"journal-title": "medRxiv",
"key": "B84",
"year": "2021"
},
{
"DOI": "10.21203/rs.3.rs-141034/v1",
"article-title": "The association of 25 (OH) Vitamin D levels and severity and outcome of COVID-19: a cross-sectional study",
"author": "Vasheghani",
"doi-asserted-by": "publisher",
"first-page": "17594",
"journal-title": "Sci Rep.",
"key": "B85",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1101/2020.11.07.20227512",
"article-title": "Vitamin D – contrary to vitamin K – does not associate with clinical outcome in hospitalized COVID-19 patients",
"author": "Walk",
"doi-asserted-by": "publisher",
"journal-title": "medRxiv",
"key": "B86",
"year": "2020"
},
{
"DOI": "10.1007/s00394-020-02411-0",
"article-title": "Possible association of vitamin D status with lung involvement and outcome in patients with COVID-19: a retrospective study",
"author": "Abrishami",
"doi-asserted-by": "publisher",
"first-page": "2249",
"journal-title": "Eur J Nutr.",
"key": "B87",
"volume": "60",
"year": "2020"
},
{
"author": "Anjum",
"first-page": "1184",
"journal-title": "Pakistan Journal of Medical and Health Sciences",
"key": "B88",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1080/07315724.2020.1856013",
"article-title": "Vitamin D deficiency and low serum calcium as predictors of poor prognosis in patients with severe COVID-19",
"author": "Bennouar",
"doi-asserted-by": "publisher",
"first-page": "104",
"journal-title": "J Am Coll Nutr.",
"key": "B89",
"volume": "40",
"year": "2021"
},
{
"DOI": "10.1007/s00198-020-05677-6",
"article-title": "Sex-specific association between vitamin D deficiency and COVID-19 mortality in older patients",
"author": "Hars",
"doi-asserted-by": "publisher",
"first-page": "2495",
"journal-title": "Osteoporos Int.",
"key": "B90",
"volume": "31",
"year": "2020"
},
{
"DOI": "10.1080/07315724.2021.1877580",
"article-title": "Low Vitamin D status at admission as a risk factor for poor survival in hospitalized patients with COVID-19: an Italian retrospective study",
"author": "Infante",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "J Am Coll Nutr.",
"key": "B91",
"year": "2021"
},
{
"DOI": "10.1007/s12603-020-1479-0",
"article-title": "Impact of serum 25(OH) Vitamin D level on mortality in patients with COVID-19 in Turkey",
"author": "Karahan",
"doi-asserted-by": "publisher",
"first-page": "189",
"journal-title": "J Nutr Heal Aging.",
"key": "B92",
"volume": "25",
"year": "2021"
},
{
"DOI": "10.3390/nu12123799",
"article-title": "High-dose cholecalciferol booster therapy is associated with a reduced risk of mortality in patients with COVID-19: a cross-sectional multi-centre observational study",
"author": "Ling",
"doi-asserted-by": "publisher",
"first-page": "3799",
"journal-title": "Nutrients.",
"key": "B93",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1093/jn/nxaa332",
"article-title": "Vitamin D deficiency is inversely associated with COVID-19 incidence and disease severity in Chinese People",
"author": "Luo",
"doi-asserted-by": "publisher",
"first-page": "98",
"journal-title": "J Nutr.",
"key": "B94",
"volume": "151",
"year": "2021"
},
{
"DOI": "10.1186/s12931-021-01666-3",
"article-title": "Circulating Vitamin D levels status and clinical prognostic indices in COVID-19 patients",
"author": "Ricci",
"doi-asserted-by": "publisher",
"first-page": "76",
"journal-title": "Respir Res.",
"key": "B95",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1016/j.clnesp.2021.01.014",
"article-title": "Evaluation of vitamin D levels in COVID-19 patients referred to Labafinejad hospital in Tehran and its relationship with disease severity and mortality",
"author": "Tehrani",
"doi-asserted-by": "publisher",
"first-page": "313",
"journal-title": "Clin Nutr ESPEN.",
"key": "B96",
"volume": "42",
"year": "2021"
},
{
"DOI": "10.35366/93773",
"article-title": "La deficiencia de vitamina D es un factor de riesgo de mortalidad en pacientes con COVID-19",
"author": "Tort",
"doi-asserted-by": "publisher",
"first-page": "106",
"journal-title": "Rev Sanid Milit.",
"key": "B97",
"volume": "74",
"year": "2020"
},
{
"DOI": "10.3390/nu12123773",
"article-title": "Low 25-Hydroxyvitamin D levels on admission to the intensive care unit may predispose COVID-19 pneumonia patients to a higher 28-day mortality risk: a pilot study on a Greek ICU cohort",
"author": "Vassiliou",
"doi-asserted-by": "publisher",
"first-page": "3773",
"journal-title": "Nutrients.",
"key": "B98",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1016/j.cell.2021.02.029",
"article-title": "COVID-19 and the human innate immune system",
"author": "Schultze",
"doi-asserted-by": "publisher",
"first-page": "1671",
"journal-title": "Cell",
"key": "B99",
"volume": "84",
"year": "2021"
},
{
"DOI": "10.1093/gerona/glaa209",
"article-title": "Underlying vulnerabilities to the cytokine storm and adverse COVID-19 outcomes in the aging immune system",
"author": "Nidadavolu",
"doi-asserted-by": "publisher",
"first-page": "e13",
"journal-title": "J Gerontol A Biol Sci Med Sci",
"key": "B100",
"volume": "76",
"year": "2021"
},
{
"DOI": "10.1016/j.lfs.2020.117900",
"article-title": "The immune system and COVID-19: friend or foe?",
"author": "Yazdanpanah",
"doi-asserted-by": "publisher",
"first-page": "117900",
"journal-title": "Life Sci.",
"key": "B101",
"volume": "256",
"year": "2020"
},
{
"DOI": "10.1016/j.eprac.2021.03.006",
"article-title": "Vitamin D and its potential benefit for the COVID-19 pandemic",
"author": "Charoenngam",
"doi-asserted-by": "publisher",
"first-page": "484",
"journal-title": "Endocr Pract.",
"key": "B102",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1111/tri.13611",
"article-title": "Why the immune system fails to mount an adaptive immune response to a COVID-19 infection",
"author": "Ahmadpoor",
"doi-asserted-by": "publisher",
"first-page": "824",
"journal-title": "Transpl Int",
"key": "B103",
"volume": "33",
"year": "2020"
},
{
"DOI": "10.3390/ijms221910559",
"article-title": "Vitamin D COVID-19: an overview of recent evidence",
"author": "Ghelani",
"doi-asserted-by": "publisher",
"first-page": "10559",
"journal-title": "Int J Mol Sci.",
"key": "B104",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1016/j.dsx.2021.03.006",
"article-title": "Impact of the vitamin D deficiency on COVID-19 infection and mortality in Asian countries",
"author": "Jayawardena",
"doi-asserted-by": "publisher",
"first-page": "757",
"journal-title": "Diabetes Metab Syndr.",
"key": "B105",
"volume": "15",
"year": "2021"
},
{
"DOI": "10.1016/j.steroids.2018.11.001",
"article-title": "U-IS. 25-Dihydroxyvitamin D3 induces formation of neutrophil extracellular trap-like structures and modulates the transcription of genes whose products are neutrophil extracellular trap-associated proteins: a pilot study.",
"author": "Agraz-Cibrian",
"doi-asserted-by": "publisher",
"first-page": "14",
"journal-title": "Steroids",
"key": "B106",
"volume": "141",
"year": "2019"
},
{
"DOI": "10.4049/jimmunol.181.10.7090",
"article-title": "Respiratory epithelial cells convert inactive vitamin d to its active form: potential effects on host defense",
"author": "Hansdottir",
"doi-asserted-by": "publisher",
"first-page": "7090",
"journal-title": "J Immunol.",
"key": "B107",
"volume": "81",
"year": "2008"
},
{
"DOI": "10.1136/thoraxjnl-2014-206680",
"article-title": "Vitamin D deficiency contributes directly to the acute respiratory distress syndrome (ARDS)",
"author": "Dancer",
"doi-asserted-by": "publisher",
"first-page": "617",
"journal-title": "Thorax.",
"key": "B108",
"volume": "70",
"year": "2015"
},
{
"DOI": "10.3892/mmr.2017.7546",
"article-title": "Vitamin D alleviates lipopolysaccharide-induced acute lung injury via regulation of the renin-angiotensin system",
"author": "Xu",
"doi-asserted-by": "publisher",
"first-page": "7432",
"journal-title": "Mol Med Rep.",
"key": "B109",
"volume": "16",
"year": "2017"
},
{
"DOI": "10.1161/01.CIR.102.23.2867",
"article-title": "1alpha,25-dihydroxyvitamin D(3) its potent synthetic analogs downregulate tissue factor upregulate thrombomodulin expression in monocytic cells",
"author": "Ohsawa",
"doi-asserted-by": "publisher",
"first-page": "2867",
"journal-title": "Circulation",
"key": "B110",
"volume": "102",
"year": "2000"
},
{
"DOI": "10.1074/jbc.M404865200",
"article-title": "Disruption of nuclear vitamin D receptor gene causes enhanced thrombogenicity in mice",
"author": "Aihara",
"doi-asserted-by": "publisher",
"first-page": "35798",
"journal-title": "J Biol Chem.",
"key": "B111",
"volume": "279",
"year": "2004"
},
{
"DOI": "10.1186/1479-5876-7-28",
"article-title": "Alterations in vitamin D status and antimicrobial peptide levels in patients in the intensive care unit with sepsis",
"author": "Jeng",
"doi-asserted-by": "publisher",
"first-page": "28",
"journal-title": "J Transl Med.",
"key": "B112",
"volume": "7",
"year": "2009"
},
{
"DOI": "10.1007/s00394-020-02429-4",
"article-title": "Prognostic implications of vitamin D in patients with COVID-19",
"author": "Hosack",
"doi-asserted-by": "publisher",
"first-page": "549",
"journal-title": "Eur J Nutr",
"key": "B113",
"volume": "60",
"year": "2020"
},
{
"DOI": "10.3390/nu13103596",
"article-title": "COVID-19 mortality risk correlates inversely with Vitamin D3 status, and a mortality rate close to zero could theoretically be achieved at 50 ng/mL 25(OH)D3: Results of a systematic review and meta-analysis",
"author": "Borsche",
"doi-asserted-by": "publisher",
"first-page": "3596",
"journal-title": "Nutrients.",
"key": "B114",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0081120",
"article-title": "Vitamin D status and community-acquired pneumonia: results from the third National Health and Nutrition Examination Survey",
"author": "Quraishi",
"doi-asserted-by": "publisher",
"first-page": "e81120",
"journal-title": "PLoS One",
"key": "B115",
"volume": "8",
"year": "2013"
},
{
"DOI": "10.1001/jamasurg.2013.3176",
"article-title": "Association between preoperative 25-hydroxyvitamin D level and hospital-acquired infections following Roux-en-Y gastric bypass surgery",
"author": "Quraishi",
"doi-asserted-by": "publisher",
"first-page": "112",
"journal-title": "JAMA Surg.",
"key": "B116",
"volume": "149",
"year": "2014"
},
{
"DOI": "10.1016/j.ijid.2020.12.077",
"article-title": "Low vitamin D status is associated with coronavirus disease 2019 outcomes: a systematic review and meta-analysis",
"author": "Liu",
"doi-asserted-by": "publisher",
"first-page": "58",
"journal-title": "Int J Infect Dis.",
"key": "B117",
"volume": "104",
"year": "2021"
},
{
"DOI": "10.1210/clinem/dgab405",
"article-title": "Calcifediol treatment and COVID-19-related outcomes",
"author": "Nogues",
"doi-asserted-by": "publisher",
"first-page": "e4017",
"journal-title": "J Clin Endocrinol Metab.",
"key": "B118",
"volume": "106",
"year": "2021"
},
{
"DOI": "10.1007/s40618-021-01614-4",
"article-title": "Vitamin D supplementation and clinical outcomes in COVID-19: a systematic review and meta-analysis",
"author": "Pal",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "J Endocrinol Invest.",
"key": "B119",
"volume": "24",
"year": "2021"
},
{
"DOI": "10.1098/rsos.201912",
"article-title": "Vitamin D and COVID-19: evidence and recommendations for supplementation",
"author": "Griffin",
"doi-asserted-by": "publisher",
"first-page": "201912",
"journal-title": "R Soc Open Sci.",
"key": "B120",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1038/s41591-020-0897-1",
"article-title": "Antibody responses to SARS-CoV-2 in patients with COVID-19",
"author": "Long",
"doi-asserted-by": "publisher",
"first-page": "845",
"journal-title": "Nat Med.",
"key": "B121",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1016/j.jsbmb.2018.12.010",
"article-title": "Daily oral dosing of vitamin D3 using 5000 TO 50,000 international units a day in long-term hospitalized patients: insights from a seven year experience",
"author": "McCullough",
"doi-asserted-by": "publisher",
"first-page": "228",
"journal-title": "Steroid Biochem Mol Biol.",
"key": "B122",
"volume": "189",
"year": "2019"
}
],
"reference-count": 122,
"references-count": 122,
"relation": {},
"score": 1,
"short-container-title": [
"Front. Public Health"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Public Health, Environmental and Occupational Health"
],
"subtitle": [],
"title": [
"Vitamin D Status and SARS-CoV-2 Infection and COVID-19 Clinical Outcomes"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.3389/crossmark-policy",
"volume": "9"
}
