Exploring the link between vitamin D and clinical outcomes in COVID-19
et al., American Journal of Physiology-Endocrinology and Metabolism, doi:10.1152/ajpendo.00517.2020, Mar 2021
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 270 patients with vitamin D levels measured in the last year, showing no significant difference in outcomes based on vitamin D levels or vitamin D supplementation.
This is the 52nd of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
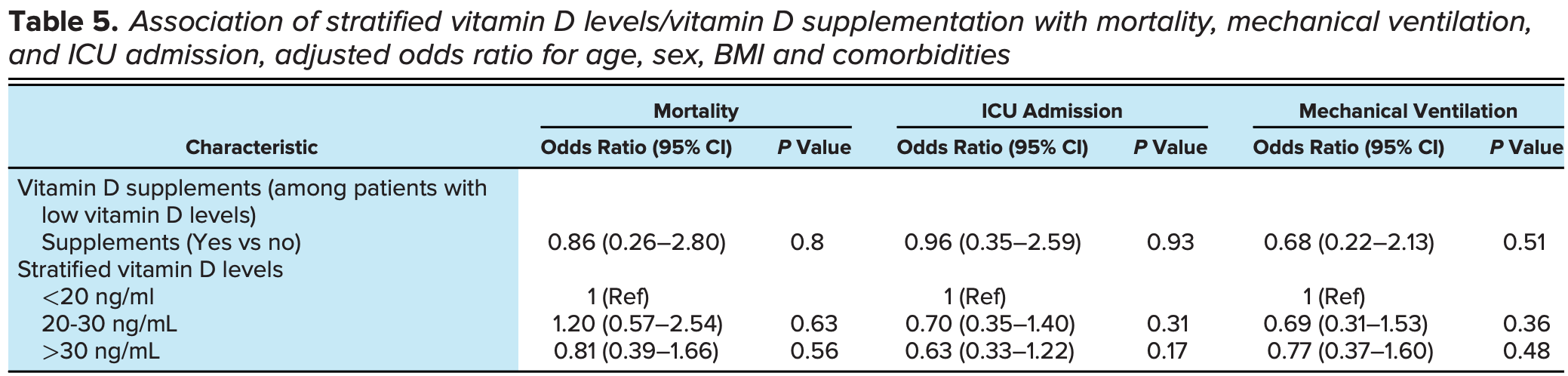
risk of death, 14.7% lower, RR 0.85, p = 0.56, high D levels 88, low D levels 95, odds ratio converted to relative risk, control prevalence approximated with overall prevalence, >30 ng/mL vs. <20 ng/mL, >30 ng/mL group size approximated.
|
|
risk of mechanical ventilation, 18.9% lower, RR 0.81, p = 0.48, high D levels 88, low D levels 95, odds ratio converted to relative risk, control prevalence approximated with overall prevalence, >30 ng/mL vs. <20 ng/mL, >30 ng/mL group size approximated.
|
|
risk of ICU admission, 28.5% lower, RR 0.72, p = 0.17, high D levels 88, low D levels 95, odds ratio converted to relative risk, control prevalence approximated with overall prevalence, >30 ng/mL vs. <20 ng/mL, >30 ng/mL group size approximated.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Lohia et al., 4 Mar 2021, retrospective, USA, peer-reviewed, 4 authors.
Exploring the link between vitamin D and clinical outcomes in COVID-19
American Journal of Physiology-Endocrinology and Metabolism, doi:10.1152/ajpendo.00517.2020
The immunomodulating role of vitamin D might play a role in COVID-19 disease. We studied the association between vitamin D and clinical outcomes in COVID-19 patients. This is a retrospective cohort study on COVID-19 patients with documented vitamin D levels within the last year. Vitamin D levels were grouped as ! 20 ng/mL or < 20 ng/mL. Main outcomes were mortality, need for mechanical ventilation, new DVT or pulmonary embolism, and ICU admission. A total of 270 patients (mean ± SD) age, 63.81 (14.69) years); 117 (43.3%) males; 216 (80%) Blacks; 139 (51.5%) in 65 and older age group were included. Vitamin D levels were less than 20 ng/mL in 95 (35.2%) patients. During admission, 72 patients (26.7%) died, 59 (21.9%) needed mechanical ventilation, and 87 (32.2%) required ICU. Vitamin D levels showed no significant association with mortality (OR = 0.69; 95% CI, 0.39-1.24; P = 0.21), need for mechanical ventilation (OR = 1.23; 95% CI, 0.68-2.24; P = 0.49), new DVT or PE(OR= 0.92; 95% CI, 0.16-5.11; P = 1.00) or ICU admission (OR = 1.38; 95% CI, 0.81-2.34; P = 0.23). We did not find any significant association of vitamin D levels with mortality, the need for mechanical ventilation, ICU admission and the development of thromboembolism in COVID-19 patients. NEW & NOTEWORTHY Low vitamin D has been associated with increased frequency and severity of respiratory tract infections in the past. Current literature linking clinical outcomes in COVID-19 with low vitamin D is debatable. This study evaluated the role of vitamin D in severe disease outcomes among COVID-19 patients and found no association of vitamin D levels with mortality, the need for mechanical ventilation, ICU admission, and thromboembolism in COVID-19.
AUTHOR CONTRIBUTIONS P.L., P.N., and N.P. conceived and designed research; P.L. and S.K. analyzed data; P.L. and S.K. interpreted results of experiments; P.L., P.N., N.P., and S.K. prepared figures; P.L., P.N., and S.K. drafted manuscript; P.L., P.N., N.P., and S.K. edited and revised manuscript; P.L., P.N., N.P., and S.K. approved final version of manuscript.
References
Adams, Ren, Liu, Chun, Lagishetty et al., Vitamin D-directed rheostatic regulation of monocyte antibacterial responses, J Immunol, doi:10.4049/jimmunol.0803736
Anderson, Geleris, Anderson, Zucker, Nobel et al., Body mass index and risk for intubation or death in SARS-CoV-2 infection: a retrospective cohort study, Ann Intern Med, doi:10.7326/M20-3214
Blondon, Rodabough, Budrys, Johnson, Berger et al., The effect of calcium plus vitamin D supplementation on the risk of venous thromboembolism: from the Women's Health Initiative Randomized Controlled Trial, Thromb Haemost, doi:10.1160/TH14-05-0478
Braun, Chang, Mahadevappa, Gibbons, Liu et al., Association of low serum 25-hydroxyvitamin D levels and mortality in the critically ill, Crit Care Med, doi:10.1097/CCM.0b013e318206ccdf
Brodin, Lerstad, Grimnes, Braekkan, Vik et al., Serum levels of vitamin D are not associated with future risk of venous thromboembolism: the Tromsø study, Thromb Haemost, doi:10.1160/TH12-10-0728
Brøndum-Jacobsen, Benn, Tybjaerg-Hansen, Nordestgaard, 25-Hydroxyvitamin D concentrations and risk of venous thromboembolism in the general population with 18,791 participants, J Thromb Haemost, doi:10.1111/jth.12118
Cannell, Vieth, Umhau, Holick, Grant et al., Epidemic influenza and vitamin D, Epidemiol Infect, doi:10.1017/S0950268806007175
Cantorna, Snyder, Lin, Yang, Vitamin D and 1,25(OH)2D regulation of T cells, Nutrients, doi:10.3390/nu7043011
Carpagnano, Lecce, Quaranta, Zito, Buonamico et al., Vitamin D deficiency as a predictor of poor prognosis in patients with acute respiratory failure due to COVID-19, J Endocrinol Invest, doi:10.1007/s40618-020-01370-x
Charan, Goyal, Saxena, Yadav, Vitamin D for prevention of respiratory tract infections: a systematic review and meta-analysis, J Pharmacol Pharmacother, doi:10.4103/0976-500X.103685
Charoenngam, Holick, Immunologic effects of vitamin D on human health and disease, Nutrients, doi:10.3390/nu12072097
D'avolio, Avataneo, Manca, Cusato, Nicol O et al., 25-Hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2, Nutrients, doi:10.3390/nu12051359
Dancer, Parekh, Lax, Souza, Zheng et al., Vitamin D deficiency contributes directly to the acute respiratory distress syndrome (ARDS), Thorax, doi:10.1136/thoraxjnl-2014-206680
De Haan, Groeneveld, De Geus, Egal, Struijs, Vitamin D deficiency as a risk factor for infection, sepsis and mortality in the critically ill: systematic review and meta-analysis, Crit Care, doi:10.1186/s13054-014-0660-4
Forrest, Stuhldreher, Prevalence and correlates of vitamin D deficiency in US adults, Nutr Res, doi:10.1016/j.nutres.2010.12.001
Ginde, Mansbach, Camargo, Association between serum 25-hydroxyvitamin D level and upper respiratory tract infection in the Third National Health and Nutrition Examination Survey, Arch Intern Med, doi:10.1001/archinternmed.2008.560
Grasselli, Zangrillo, Zanella, Antonelli, Cabrini et al., Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy, JAMA, doi:10.1001/jama.2020.5394
Greiller, Martineau, Modulation of the immune response to respiratory viruses by vitamin D, Nutrients, doi:10.3390/nu7064240
Hansdottir, Monick, Hinde, Lovan, Look et al., Respiratory epithelial cells convert inactive vitamin D to its active form: potential effects on host defense, J Immunol, doi:10.4049/jimmunol.181.10.7090
Hastie, Mackay, Ho, Celis-Morales, Katikireddi et al., Vitamin D concentrations and COVID-19 infection in UK Biobank, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.04.050
Hooper, Nápoles, Erez-Stable, COVID-19 and racial/ethnic disparities, JAMA, doi:10.1001/jama.2020.8598
Hwang, Hu, Hu, Zhu, Liu et al., Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirusinfected pneumonia in Wuhan, China, JAMA, doi:10.1001/jama.2020.1585
Ilie, Stefanescu, Smith, The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality, Aging Clin Exp Res, doi:10.1007/s40520-020-01570-8
Janssens, Bouillon, Claes, Carremans, Lehouck et al., Vitamin D deficiency is highly prevalent in COPD and correlates with variants in the vitamin D-binding gene, Thorax, doi:10.1136/thx.2009.120659
Jeffery, Burke, Mura, Zheng, Qureshi et al., 1,25-Dihydroxyvitamin D3 and IL-2 combine to inhibit T cell production of inflammatory cytokines and promote development of regulatory T cells expressing CTLA-4 and FoxP3, J Immunol, doi:10.4049/jimmunol.0803217
Jolliffe, Griffiths, Martineau, Vitamin D in the prevention of acute respiratory infection: systematic review of clinical studies, J Steroid Biochem Mol Biol, doi:10.1016/j.jsbmb.2012.11.017
Khunti, Singh, Pareek, Hanif, Is ethnicity linked to incidence or outcomes of covid-19?, BMJ, doi:10.1136/bmj.m1548
Klok, Kruip, Van Der Meer, Arbous, Gommers et al., Incidence of thrombotic complications in critically ill ICU patients with COVID-19, Thromb Res, doi:10.1016/j.thromres.2020.04.013
Kohlmeier, Avoidance of vitamin D deficiency to slow the COVID-19 pandemic, BMJ Nutr Prev Health, doi:10.1136/bmjnph-2020-000096
Laird, Rhodes, Kenny, Vitamin D and inflammation: potential implications for severity of Covid-19, Ir Med J
Lee, Eisman, Center, Vitamin D deficiency in critically ill patients, N Engl J Med, doi:10.1056/NEJMc0809996
Lei, Zhang, Cheng, Lee, Mechanisms of action of vitamin D as supplemental therapy for pneumocystis pneumonia, Antimicrob Agents Chemother, doi:10.1128/AAC.01226-17
Lemire, Adams, Kermani-Arab, Bakke, Sakai et al., 1,25-Dihydroxyvitamin D3 suppresses human T helper/inducer lymphocyte activity in vitro, J Immunol
Leow, Simpson, Cursons, Karalus, Hancox, Vitamin D, innate immunity and outcomes in community acquired pneumonia, Respirology, doi:10.1111/j.1440-1843.2011.01924.x
Liu, Stenger, Li, Wenzel, Tan et al., Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response, Science, doi:10.1126/science.1123933
Lucidarme, Messai, Mazzoni, Arcade, Cheyron, Incidence and risk factors of vitamin D deficiency in critically ill patients: results from a prospective observational study, Intensive Care Med, doi:10.1007/s00134-010-1875-8
Martineau, Jolliffe, Hooper, Greenberg, Aloia et al., Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data, BMJ, doi:10.1136/bmj.i6583
Mckinney, Bailey, Garrett, Peiris, Manning et al., Relationship between vitamin D status and ICU outcomes in veterans, J Am Med Dir Assoc, doi:10.1016/j.jamda.2010.04.004
Mehta, Mcauley, Brown, Sanchez, Tattersall et al., and HLH Across Speciality Collaboration UK. COVID-19: consider cytokine storm syndromes and immunosuppression, Lancet, doi:10.1016/S0140-6736(20)30628-0
Meltzer, Best, Zhang, Vokes, Arora et al., Association of vitamin D status and other clinical characteristics with COVID-19 test results, JAMA Netw Open, doi:10.1001/jamanetworkopen.2020.19722
Moore, June, Cytokine release syndrome in severe COVID-19, Science, doi:10.1126/science.abb8925
Munshi, Hussein, Toraih, Elshazli, Jardak et al., Vitamin D insufficiency as a potential culprit in critical COVID-19 patients, J Med Virol, doi:10.1002/jmv.26360
Olliver, Spelmink, Hiew, Meyer-Hoffert, Henriques-Normark et al., Immunomodulatory effects of vitamin D on innate and adaptive immune responses to Streptococcus pneumoniae, J Infect Dis, doi:10.1093/infdis/jit355
Parekh, Thickett, Turner, Vitamin D deficiency and acute lung injury, Inflamm Allergy Drug Targets, doi:10.2174/18715281113129990049
Pearce, Cheetham, Diagnosis and management of vitamin D deficiency, BMJ, doi:10.1136/bmj.b5664
Remmelts, Van De Garde, Meijvis, Peelen, Damoiseaux et al., Addition of vitamin D status to prognostic scores improves the prediction of outcome in community-acquired pneumonia, Clin Infect Dis, doi:10.1093/cid/cis751
Schwalfenberg, A review of the critical role of vitamin D in the functioning of the immune system and the clinical implications of vitamin D deficiency, Mol Nutr Food Res, doi:10.1002/mnfr.201000174
Scragg, Stewart, Waayer, Lawes, Toop et al., Effect of monthly high-dose vitamin D supplementation on cardiovascular disease in the vitamin D assessment study: a randomized clinical trial, JAMA Cardiol, doi:10.1001/jamacardio.2017.0175
Shi, Liu, Yao, Xing, Zhao et al., Chronic vitamin D deficiency induces lung fibrosis through activation of the renin-angiotensin system, Sci Rep, doi:10.1038/s41598-017-03474-6
Stokes, Zambrano, Anderson, Marder, Raz et al., Coronavirus Disease 2019 Case Surveillance: United States, MMWR Morb Mortal Wkly Rep, doi:10.15585/mmwr.mm6924e2
Tartof, Qian, Hong, Wei, Nadjafi et al., Obesity and mortality among patients diagnosed with COVID-19: results from an integrated health care organization, Ann Intern Med, doi:10.7326/M20-3742
Urashima, Segawa, Okazaki, Kurihara, Wada et al., Randomized trial of vitamin D supplementation to prevent seasonal influenza A in schoolchildren, Am J Clin Nutr, doi:10.3945/ajcn.2009.29094
Venkatram, Chilimuri, Adrish, Salako, Patel et al., Vitamin D deficiency is associated with mortality in the medical intensive care unit, Crit Care, doi:10.1186/cc10585
Vu Cković, Van Rein, Cannegieter, Rosendaal, Lijfering, Vitamin supplementation on the risk of venous thrombosis: results from the MEGA case-control study, Am J Clin Nutr, doi:10.3945/ajcn.114.095398
Wei, Christakos, Mechanisms underlying the regulation of innate and adaptive immunity by vitamin D, Nutrients, doi:10.3390/nu7105392
Wu, He, Low vitamin D levels are associated with the development of deep venous thromboembolic events in patients with ischemic stroke, Clin Appl Thromb Hemost, doi:10.1177/1076029618786574
Xu, Yang, Chen, Luo, Zhang et al., Vitamin D alleviates lipopolysaccharide-induced acute lung injury via regulation of the renin-angiotensin system, Mol Med Rep, doi:10.3892/mmr.2017.7546
Yang, Zheng, Gou, Pu, Chen et al., 2: a systematic review and meta-analysis
Zdrenghea, Makrinioti, Bagacean, Bush, Johnston et al., Vitamin D modulation of innate immune responses to respiratory viral infections, Rev Med Virol, doi:10.1002/rmv.1909
Zhang, Leung, Richers, Liu, Remigio et al., Vitamin D inhibits monocyte/macrophage proinflammatory cytokine production by targeting MAPK phosphatase-1, J Immunol, doi:10.4049/jimmunol.1102412
Zhang, Wan, Sun, Kan, Wang, Association between vitamin D deficiency and mortality in critically ill adult patients: a meta-analysis of cohort studies, Crit Care, doi:10.1186/s13054-014-0684-9
Zhang, Wu, Li, Zhao, Gq, Cytokine release syndrome in severe COVID-19: interleukin-6 receptor antagonist tocilizumab may be the key to reduce mortality, Int J Antimicrob Agents, doi:10.1016/j.ijantimicag.2020.105954
Zhou, Du, Huang, Wang, Shi et al., Preventive effects of vitamin D on seasonal influenza A in infants: a multicenter, randomized, open, controlled clinical trial, Pediatr Infect Dis J, doi:10.1097/INF.0000000000001890
DOI record:
{
"DOI": "10.1152/ajpendo.00517.2020",
"ISSN": [
"0193-1849",
"1522-1555"
],
"URL": "http://dx.doi.org/10.1152/ajpendo.00517.2020",
"abstract": "<jats:p>Low vitamin D has been associated with increased frequency and severity of respiratory tract infections in the past. Current literature linking clinical outcomes in COVID-19 with low vitamin D is debatable. This study evaluated the role of vitamin D in severe disease outcomes among COVID-19 patients and found no association of vitamin D levels with mortality, the need for mechanical ventilation, ICU admission, and thromboembolism in COVID-19.</jats:p>",
"alternative-id": [
"10.1152/ajpendo.00517.2020"
],
"assertion": [
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Received",
"name": "received",
"order": 0,
"value": "2020-10-21"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "2021-01-03"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Published",
"name": "published",
"order": 3,
"value": "2021-03-04"
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-4148-9597",
"affiliation": [
{
"name": "Department of Internal Medicine, Wayne State University, Detroit, Michigan"
}
],
"authenticated-orcid": false,
"family": "Lohia",
"given": "Prateek",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Wayne State University, Detroit, Michigan"
}
],
"family": "Nguyen",
"given": "Paul",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Wayne State University, Detroit, Michigan"
}
],
"family": "Patel",
"given": "Neel",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Wayne State University, Detroit, Michigan"
}
],
"family": "Kapur",
"given": "Shweta",
"sequence": "additional"
}
],
"container-title": "American Journal of Physiology-Endocrinology and Metabolism",
"container-title-short": "American Journal of Physiology-Endocrinology and Metabolism",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"journals.physiology.org"
]
},
"created": {
"date-parts": [
[
2021,
1,
6
]
],
"date-time": "2021-01-06T16:56:09Z",
"timestamp": 1609952169000
},
"deposited": {
"date-parts": [
[
2023,
10,
17
]
],
"date-time": "2023-10-17T02:22:26Z",
"timestamp": 1697509346000
},
"indexed": {
"date-parts": [
[
2024,
2,
10
]
],
"date-time": "2024-02-10T13:43:48Z",
"timestamp": 1707572628339
},
"is-referenced-by-count": 20,
"issue": "3",
"issued": {
"date-parts": [
[
2021,
3,
1
]
]
},
"journal-issue": {
"issue": "3",
"published-print": {
"date-parts": [
[
2021,
3,
1
]
]
}
},
"language": "en",
"link": [
{
"URL": "https://journals.physiology.org/doi/pdf/10.1152/ajpendo.00517.2020",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "24",
"original-title": [],
"page": "E520-E526",
"prefix": "10.1152",
"published": {
"date-parts": [
[
2021,
3,
1
]
]
},
"published-print": {
"date-parts": [
[
2021,
3,
1
]
]
},
"publisher": "American Physiological Society",
"reference": [
{
"DOI": "10.1001/jama.2020.1585",
"doi-asserted-by": "publisher",
"key": "B1"
},
{
"DOI": "10.1016/j.ijid.2020.03.017",
"doi-asserted-by": "publisher",
"key": "B2"
},
{
"DOI": "10.3390/nu7064240",
"doi-asserted-by": "publisher",
"key": "B3"
},
{
"DOI": "10.4049/jimmunol.181.10.7090",
"doi-asserted-by": "publisher",
"key": "B4"
},
{
"DOI": "10.1126/science.1123933",
"doi-asserted-by": "publisher",
"key": "B5"
},
{
"DOI": "10.1093/infdis/jit355",
"doi-asserted-by": "publisher",
"key": "B6"
},
{
"DOI": "10.1017/S0950268806007175",
"doi-asserted-by": "publisher",
"key": "B7"
},
{
"DOI": "10.1001/archinternmed.2008.560",
"doi-asserted-by": "publisher",
"key": "B8"
},
{
"DOI": "10.1136/thx.2009.120659",
"doi-asserted-by": "publisher",
"key": "B9"
},
{
"DOI": "10.1016/j.jsbmb.2012.11.017",
"doi-asserted-by": "publisher",
"key": "B10"
},
{
"DOI": "10.4103/0976-500X.103685",
"doi-asserted-by": "publisher",
"key": "B11"
},
{
"DOI": "10.1136/bmj.i6583",
"doi-asserted-by": "publisher",
"key": "B12"
},
{
"DOI": "10.3945/ajcn.2009.29094",
"doi-asserted-by": "publisher",
"key": "B13"
},
{
"DOI": "10.1097/INF.0000000000001890",
"doi-asserted-by": "publisher",
"key": "B14"
},
{
"DOI": "10.1002/mnfr.201000174",
"doi-asserted-by": "publisher",
"key": "B15"
},
{
"DOI": "10.1002/rmv.1909",
"doi-asserted-by": "publisher",
"key": "B16"
},
{
"DOI": "10.4049/jimmunol.0803736",
"doi-asserted-by": "publisher",
"key": "B17"
},
{
"DOI": "10.3390/nu7043011",
"doi-asserted-by": "publisher",
"key": "B18"
},
{
"DOI": "10.4049/jimmunol.134.5.3032",
"author": "Lemire JM",
"doi-asserted-by": "crossref",
"first-page": "3032",
"journal-title": "J Immunol",
"key": "B19",
"volume": "134",
"year": "1985"
},
{
"DOI": "10.4049/jimmunol.1102412",
"doi-asserted-by": "publisher",
"key": "B20"
},
{
"DOI": "10.4049/jimmunol.0803217",
"doi-asserted-by": "publisher",
"key": "B21"
},
{
"DOI": "10.3390/nu7105392",
"doi-asserted-by": "publisher",
"key": "B22"
},
{
"DOI": "10.1126/science.abb8925",
"doi-asserted-by": "publisher",
"key": "B23"
},
{
"DOI": "10.1016/j.ijantimicag.2020.105954",
"doi-asserted-by": "publisher",
"key": "B24"
},
{
"DOI": "10.1128/AAC.01226-17",
"doi-asserted-by": "publisher",
"key": "B25"
},
{
"DOI": "10.1038/s41598-017-03474-6",
"doi-asserted-by": "publisher",
"key": "B26"
},
{
"DOI": "10.3892/mmr.2017.7546",
"doi-asserted-by": "publisher",
"key": "B27"
},
{
"DOI": "10.1016/S0140-6736(20)30628-0",
"doi-asserted-by": "publisher",
"key": "B28"
},
{
"DOI": "10.1136/thoraxjnl-2014-206680",
"doi-asserted-by": "publisher",
"key": "B29"
},
{
"DOI": "10.1016/j.nutres.2010.12.001",
"doi-asserted-by": "publisher",
"key": "B30"
},
{
"DOI": "10.1016/j.thromres.2020.04.013",
"doi-asserted-by": "publisher",
"key": "B31"
},
{
"DOI": "10.1177/1076029618786574",
"doi-asserted-by": "publisher",
"key": "B32"
},
{
"DOI": "10.1111/jth.12118",
"doi-asserted-by": "publisher",
"key": "B33"
},
{
"DOI": "10.1160/TH12-10-0728",
"doi-asserted-by": "publisher",
"key": "B34"
},
{
"DOI": "10.1136/bmj.b5664",
"doi-asserted-by": "publisher",
"key": "B35"
},
{
"DOI": "10.7326/M20-3214",
"doi-asserted-by": "publisher",
"key": "B36"
},
{
"DOI": "10.1001/jama.2020.5394",
"doi-asserted-by": "publisher",
"key": "B37"
},
{
"DOI": "10.7326/M20-3742",
"doi-asserted-by": "publisher",
"key": "B38"
},
{
"author": "Laird E",
"first-page": "81",
"journal-title": "Ir Med J",
"key": "B39",
"volume": "113",
"year": "2020"
},
{
"DOI": "10.1007/s40520-020-01570-8",
"doi-asserted-by": "publisher",
"key": "B40"
},
{
"DOI": "10.3390/nu12051359",
"doi-asserted-by": "publisher",
"key": "B41"
},
{
"DOI": "10.1016/j.dsx.2020.04.050",
"doi-asserted-by": "publisher",
"key": "B42"
},
{
"DOI": "10.1001/jamanetworkopen.2020.19722",
"doi-asserted-by": "publisher",
"key": "B43"
},
{
"DOI": "10.1136/bmj.m1548",
"doi-asserted-by": "publisher",
"key": "B44"
},
{
"DOI": "10.15585/mmwr.mm6924e2",
"doi-asserted-by": "publisher",
"key": "B45"
},
{
"DOI": "10.1001/jama.2020.8598",
"doi-asserted-by": "publisher",
"key": "B46"
},
{
"DOI": "10.1136/bmjnph-2020-000096",
"doi-asserted-by": "publisher",
"key": "B47"
},
{
"DOI": "10.1097/CCM.0b013e318206ccdf",
"doi-asserted-by": "publisher",
"key": "B48"
},
{
"DOI": "10.1186/s13054-014-0660-4",
"doi-asserted-by": "publisher",
"key": "B49"
},
{
"DOI": "10.1056/NEJMc0809996",
"doi-asserted-by": "publisher",
"key": "B50"
},
{
"DOI": "10.1007/s00134-010-1875-8",
"doi-asserted-by": "publisher",
"key": "B51"
},
{
"DOI": "10.1016/j.jamda.2010.04.004",
"doi-asserted-by": "publisher",
"key": "B52"
},
{
"DOI": "10.1186/cc10585",
"doi-asserted-by": "publisher",
"key": "B53"
},
{
"DOI": "10.1186/s13054-014-0684-9",
"doi-asserted-by": "publisher",
"key": "B54"
},
{
"DOI": "10.1111/j.1440-1843.2011.01924.x",
"doi-asserted-by": "publisher",
"key": "B55"
},
{
"DOI": "10.1093/cid/cis751",
"doi-asserted-by": "publisher",
"key": "B56"
},
{
"DOI": "10.2174/18715281113129990049",
"doi-asserted-by": "publisher",
"key": "B57"
},
{
"DOI": "10.1002/jmv.26360",
"doi-asserted-by": "publisher",
"key": "B58"
},
{
"DOI": "10.1007/s40618-020-01370-x",
"doi-asserted-by": "publisher",
"key": "B59"
},
{
"DOI": "10.1160/TH14-05-0478",
"doi-asserted-by": "publisher",
"key": "B60"
},
{
"DOI": "10.1001/jamacardio.2017.0175",
"doi-asserted-by": "publisher",
"key": "B61"
},
{
"DOI": "10.3945/ajcn.114.095398",
"doi-asserted-by": "publisher",
"key": "B62"
},
{
"DOI": "10.3390/nu12072097",
"doi-asserted-by": "publisher",
"key": "B63"
}
],
"reference-count": 63,
"references-count": 63,
"relation": {},
"resource": {
"primary": {
"URL": "https://journals.physiology.org/doi/10.1152/ajpendo.00517.2020"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Physiology (medical)",
"Physiology",
"Endocrinology, Diabetes and Metabolism"
],
"subtitle": [],
"title": "Exploring the link between vitamin D and clinical outcomes in COVID-19",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1152/aps-crossmark-policy",
"volume": "320"
}
