Vitamin D status and outcomes for hospitalised older patients with COVID-19
et al., Postgraduate Medical Journal, doi:10.1136/postgradmedj-2020-138712, Aug 2020
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Prospective study of 105 hospitalized patients, showing lower vitamin D levels in the COVID-19 positive group (27.0 nmol/L vs 52.0 nmol/L, p=0.0008), and non-statistically significant higher mortality with vitamin D deficiency.
This is the 12th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
Standard of Care (SOC) for COVID-19 in the study country,
the United Kingdom, is very poor with very low average efficacy for approved treatments1.
The United Kingdom focused on expensive high-profit treatments, approving only one low-cost early treatment, which required a prescription and had limited adoption. The high-cost prescription treatment strategy reduces the probability of early treatment due to access and cost barriers, and eliminates complementary and synergistic benefits seen with many low-cost treatments.
|
risk of death, 28.6% lower, RR 0.71, p = 0.50, high D levels 4 of 31 (12.9%), low D levels 6 of 39 (15.4%), adjusted per study, inverted to make RR<1 favor high D levels, >30nmol/L.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Baktash et al., 27 Aug 2020, prospective, United Kingdom, peer-reviewed, 8 authors.
Vitamin D status and outcomes for hospitalised older patients with COVID-19
Postgraduate Medical Journal, doi:10.1136/postgradmedj-2020-138712
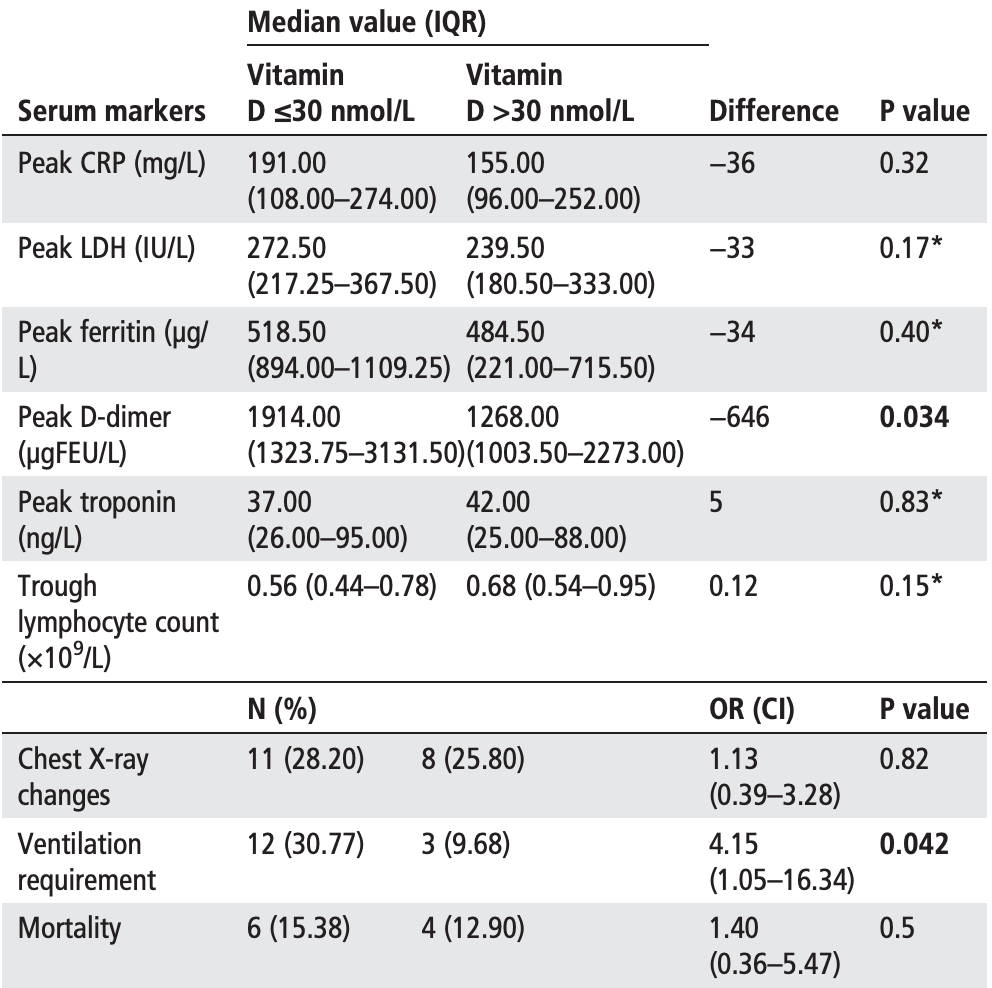
Purpose Older adults are more likely to be vitamin D deficient. The aim of the study was to determine whether these patients have worse outcomes with COVID-19. Methods We conducted a prospective cohort study between 1 March and 30 April 2020 to assess the importance of vitamin D deficiency in older patients with COVID-19. The cohort consisted of patients aged ≥65 years presenting with symptoms consistent with COVID-19 (n=105). All patients were tested for serum 25hydroxyvitamin D (25(OH)D) levels during acute illness. Diagnosis of COVID-19 was confirmed via viral reverse transcriptase PCR swab or supporting radiological evidence. COVID-19-positive arm (n=70) was sub-divided into vitamin D-deficient (≤30 nmol/L) (n=39) and -replete groups (n=35). Subgroups were assessed for disease severity using biochemical, radiological and clinical markers. Primary outcome was in-hospital mortality. Secondary outcomes were laboratory features of cytokine storm, thoracic imaging changes and requirement of non-invasive ventilation (NIV). Results COVID-19-positive arm demonstrated lower median serum 25(OH)D level of 27 nmol/L (IQR=20-47 nmol/L) compared with COVID-19-negative arm, with median level of 52 nmol/L (IQR=31.5-71.5 nmol/L) (p value=0.0008). Among patients with vitamin D deficiency, there was higher peak D-dimer level (1914.00 μgFEU/L vs 1268.00 μgFEU/L) (p=0.034) and higher incidence of NIV support and high dependency unit admission (30.77% vs 9.68%) (p=0.042). No increased mortality was observed between groups. Conclusion Older adults with vitamin D deficiency and COVID-19 may demonstrate worse morbidity outcomes. Vitamin D status may be a useful prognosticator.
Contributors All authors contributed to the manuscript. All were involved in the design of the study. VB, PK and NP collected the data. VB and TH were responsible for the statistical analysis. VB, TH, AKJM, KVDA, SS and CGM wrote the manuscript and all authors were involved in the final approval of the manuscript. Competing interests All authors understand the policy of declaration of interests. CGM is a former member of the Fellowship of Postgraduate Medicine (FPM) council and is currently an FPM Fellow. VB, TH, NP, SS, PK, KVDA, AKJM all declare that they have no competing interests. Patient consent for publication Not required. Ethics approval As an audit using clinically collected, non-identifiable data, this work does not fall under the remit of National Health Service Research Ethics Committees. This statement is also present in the 'Methods and material' section of our manuscript. Provenance and peer review Not commissioned; externally peer reviewed.
Main messages • Older patients with COVID-19 infection and vitamin D deficiency (≤30 nmol/L) have higher peak D-dimer level and higher incidence of NIV support and HDU admission. • Vitamin D deficiency may be associated with worse outcomes from COVID-19, and vitamin D status may be a useful prognosticator.
What is already known on the subject • There appears to be an association between increased COVID-19 incidence and mortality and countries with an increased prevalence of vitamin D deficiency. • Vitamin D plays an..
References
Alipio, Vitamin D Supplementation Could Possibly Improve Clinical Outcomes of Patients Infected with Coronavirus, SSRN Journal, doi:10.2139/ssrn.3571484
Almerighi, Sinistro, Cavazza, 1Alpha,25-dihydroxyvitamin D3 inhibits CD40L-induced pro-inflammatory and immunomodulatory activity in human monocytes, Cytokine, doi:10.1016/j.cyto.2008.12.009
Barrat, Cua, Boonstra, In vitro generation of interleukin 10-producing regulatory CD4(+) T cells is induced by immunosuppressive drugs and inhibited by T helper type 1 (Th1)-and Th2-inducing cytokines, J Exp Med, doi:10.1084/jem.20011629
Boonstra, Barrat, Crain, 1alpha,25-Dihydroxyvitamin d3 has a direct effect on naive CD4(+) T cells to enhance the development of Th2 cells, J Immunol, doi:10.4049/jimmunol.167.9.4974
Cantorna, Mechanisms underlying the effect of vitamin D on the immune system, Proc Nutr Soc, doi:10.1017/S0029665110001722
Charlson, Pompei, Ales, A new method of classifying prognostic comorbidity in longitudinal studies: development and validation, J Chronic Dis, doi:10.1016/0021-9681(87)90171-8
D'avolio, Avataneo, Manca, 25-hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2, Nutrients, doi:10.3390/nu12051359
Dancer, Parekh, Lax, Vitamin D deficiency contributes directly to the acute respiratory distress syndrome (ARDS), Thorax, doi:10.1136/thoraxjnl-2014-206680
Daniel, Sartory, Zahn, Immune modulatory treatment of trinitrobenzene sulfonic acid colitis with calcitriol is associated with a change of a T helper (Th) 1/Th17 to a Th2 and regulatory T cell profile, J Pharmacol Exp Ther, doi:10.1124/jpet.107.127209
Francis, Aspray, Bowring, National osteoporosis society practical clinical guideline on vitamin D and bone health, Maturitas, doi:10.1016/j.maturitas.2014.11.018
Gibson, Davis, Zhu, Dietary vitamin D and its metabolites non-genomically stabilize the endothelium, PLoS One, doi:10.1371/journal.pone.0140370
Giustina, Adler, Binkley, Controversies in vitamin D: summary statement from an international conference, J Clin Endocrinol Metab, doi:10.1210/jc.2018-01414
Gorman, Kuritzky, Judge, Topically applied 1,25-dihydroxyvitamin D3 enhances the suppressive activity of CD4+CD25+ cells in the draining lymph nodes, J Immunol, doi:10.4049/jimmunol.179.9.6273
Hastie, Mackay, Ho, Vitamin D concentrations and COVID-19 infection in UK Biobank, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.04.050
Ilie, Stefanescu, Smith, The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality, Aging Clin Exp Res, doi:10.1007/s40520-020-01570-8
Jose, Manuel, COVID-19 cytokine storm: the interplay between inflammation and coagulation, The Lancet Respiratory Medicine, doi:10.1016/S2213-2600(20)30216-2
Kuka, Imai, Penninger, Angiotensin-converting enzyme 2 in lung diseases, Curr Opin Pharmacol, doi:10.1016/j.coph.2006.03.001
Levi, Thachil, Iba, Levy, Coagulation abnormalities and thrombosis in patients with COVID-19, Lancet Haematol, doi:10.1016/S2352-3026(20)30145-9
Lippi, Plebani, Laboratory abnormalities in patients with COVID-2019 infection, Clin Chem Lab Med, doi:10.1515/cclm-2020-0198
Martineau, Jolliffe, Hooper, Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individuals participant data, BMJ, doi:10.1136/bmj.i6583
Mattner, Smiroldo, Galbiati, Inhibition of Th1 development and treatment of chronic-relapsing experimental allergic encephalomyelitis by a non-hypercalcemic analogue of 1,25-dihydroxyvitamin D(3), Eur J Immunol, doi:10.1002/1521-4141(200002)30:2%3C498::AID-IMMU498%3E3.0.CO;2-Q
Panarese, Shahini, COVID-19, and vitamin D, Aliment Pharm Ther, doi:10.1111/apt.15752
Penna, Roncari, Amuchastegui, Expression of the inhibitory receptor ILT3 on dendritic cells is dispensable for induction of CD4+Foxp3+ regulatory T cells by 1,25-dihydroxyvitamin D3, Blood, doi:10.1182/blood-2005-05-2044
Rockwood, Song, Macknight, Global clinical measure of fitness and frailty in elderly people, CMAJ, doi:10.1503/cmaj.050051
Shi, Han, Jiang, Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study, Lancet Infect Dis, doi:10.1016/S1473-3099(20)30086-4
Shorr, Thomas, Alkins, D-dimer correlates with proinflammatory cytokine levels and outcomes in critically ill patients, Chest, doi:10.1378/chest.121.4.1262
Tang, Zhou, Luger, Calcitriol suppresses antiretinal autoimmunity through inhibitory effects on the Th17 effector response, J Immunol, doi:10.4049/jimmunol.0801543
Wong, Lam, Fong, Frequency and distribution of chest radiographic findings in COVID-19 positive patients, Radiology, doi:10.1148/radiol.2020201160
DOI record:
{
"DOI": "10.1136/postgradmedj-2020-138712",
"ISSN": [
"1469-0756",
"0032-5473"
],
"URL": "http://dx.doi.org/10.1136/postgradmedj-2020-138712",
"abstract": "<jats:title>ABSTRACT</jats:title>\n <jats:sec>\n <jats:title>Purpose</jats:title>\n <jats:p>Older adults are more likely to be vitamin D deficient. The aim of the study was to determine whether these patients have worse outcomes with COVID-19.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Methods</jats:title>\n <jats:p>We conducted a prospective cohort study between 1 March and 30 April 2020 to assess the importance of vitamin D deficiency in older patients with COVID-19. The cohort consisted of patients aged ≥65 years presenting with symptoms consistent with COVID-19 (n=105). All patients were tested for serum 25-hydroxyvitamin D (25(OH)D) levels during acute illness. Diagnosis of COVID-19 was confirmed via viral reverse transcriptase PCR swab or supporting radiological evidence. COVID-19-positive arm (n=70) was sub-divided into vitamin D-deficient (≤30 nmol/L) (n=39) and -replete groups (n=35). Subgroups were assessed for disease severity using biochemical, radiological and clinical markers. Primary outcome was in-hospital mortality. Secondary outcomes were laboratory features of cytokine storm, thoracic imaging changes and requirement of non-invasive ventilation (NIV).</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Results</jats:title>\n <jats:p>COVID-19-positive arm demonstrated lower median serum 25(OH)D level of 27 nmol/L (IQR=20–47 nmol/L) compared with COVID-19-negative arm, with median level of 52 nmol/L (IQR=31.5–71.5 nmol/L) (p value=0.0008). Among patients with vitamin D deficiency, there was higher peak D-dimer level (1914.00 μgFEU/L vs 1268.00 μgFEU/L) (p=0.034) and higher incidence of NIV support and high dependency unit admission (30.77% vs 9.68%) (p=0.042). No increased mortality was observed between groups.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Conclusion</jats:title>\n <jats:p>Older adults with vitamin D deficiency and COVID-19 may demonstrate worse morbidity outcomes. Vitamin D status may be a useful prognosticator.</jats:p>\n </jats:sec>",
"author": [
{
"affiliation": [
{
"name": "Department of Medicine, Frimley Health NHS Foundation Trust, Wexham Park Hospital , Slough, UK"
}
],
"family": "Baktash",
"given": "Vadir",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Department of Medicine, Frimley Health NHS Foundation Trust, Wexham Park Hospital , Slough, UK"
}
],
"family": "Hosack",
"given": "Tom",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine, Frimley Health NHS Foundation Trust, Wexham Park Hospital , Slough, UK"
}
],
"family": "Zahari",
"given": "Nishil",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine, Frimley Health NHS Foundation Trust, Wexham Park Hospital , Slough, UK"
}
],
"family": "Shah",
"given": "Shital",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine, Frimley Health NHS Foundation Trust, Wexham Park Hospital , Slough, UK"
}
],
"family": "Kandiah",
"given": "Pirabakaran",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine, Frimley Health NHS Foundation Trust, Wexham Park Hospital , Slough, UK"
}
],
"family": "Van den Abbeele",
"given": "Koenraad",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0986-5927",
"affiliation": [
{
"name": "Department of Medicine, Frimley Health NHS Foundation Trust, Wexham Park Hospital , Slough, UK"
}
],
"authenticated-orcid": false,
"family": "Mandal",
"given": "Amit K J",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine, Frimley Health NHS Foundation Trust, Wexham Park Hospital , Slough, UK"
},
{
"name": "Department of Cardiology, University of Cyprus Medical School , Nicosia, Cyprus"
}
],
"family": "Missouris",
"given": "Constantinos G",
"sequence": "additional"
}
],
"container-title": "Postgraduate Medical Journal",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"bmj.com"
]
},
"created": {
"date-parts": [
[
2021,
1,
9
]
],
"date-time": "2021-01-09T06:37:25Z",
"timestamp": 1610174245000
},
"deposited": {
"date-parts": [
[
2023,
5,
22
]
],
"date-time": "2023-05-22T22:03:44Z",
"timestamp": 1684793024000
},
"indexed": {
"date-parts": [
[
2024,
3,
26
]
],
"date-time": "2024-03-26T23:18:26Z",
"timestamp": 1711495106206
},
"is-referenced-by-count": 152,
"issue": "1149",
"issued": {
"date-parts": [
[
2020,
8,
27
]
]
},
"journal-issue": {
"issue": "1149",
"published-online": {
"date-parts": [
[
2020,
8,
27
]
]
},
"published-print": {
"date-parts": [
[
2021,
7,
1
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 864,
"start": {
"date-parts": [
[
2023,
1,
8
]
],
"date-time": "2023-01-08T00:00:00Z",
"timestamp": 1673136000000
}
},
{
"URL": "https://bmj.com/coronavirus/usage",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2020,
8,
27
]
],
"date-time": "2020-08-27T00:00:00Z",
"timestamp": 1598486400000
}
}
],
"link": [
{
"URL": "https://academic.oup.com/pmj/article-pdf/97/1149/442/50416964/postgradmedj-97-442.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "syndication"
},
{
"URL": "https://academic.oup.com/pmj/article-pdf/97/1149/442/50416964/postgradmedj-97-442.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "286",
"original-title": [],
"page": "442-447",
"prefix": "10.1093",
"published": {
"date-parts": [
[
2020,
8,
27
]
]
},
"published-online": {
"date-parts": [
[
2020,
8,
27
]
]
},
"published-other": {
"date-parts": [
[
2021,
7
]
]
},
"published-print": {
"date-parts": [
[
2021,
7,
1
]
]
},
"publisher": "Oxford University Press (OUP)",
"reference": [
{
"DOI": "10.1111/apt.15752",
"article-title": "COVID-19, and vitamin D",
"author": "Panarese",
"doi-asserted-by": "crossref",
"first-page": "993",
"journal-title": "Aliment Pharm Ther",
"key": "2023052222031285500_R1",
"volume": "51",
"year": "2020"
},
{
"DOI": "10.2139/ssrn.3571484",
"article-title": "Vitamin D Supplementation Could Possibly Improve Clinical Outcomes of Patients Infected with Coronavirus-2019 (COVID-2019).",
"author": "Alipio",
"doi-asserted-by": "crossref",
"key": "2023052222031285500_R2",
"volume-title": "SSRN Journal"
},
{
"DOI": "10.1017/S0029665110001722",
"article-title": "Mechanisms underlying the effect of vitamin D on the immune system",
"author": "Cantorna",
"doi-asserted-by": "crossref",
"first-page": "286",
"journal-title": "Proc Nutr Soc",
"key": "2023052222031285500_R3",
"volume": "69",
"year": "2010"
},
{
"author": "GOV.UK",
"key": "2023052222031285500_R4",
"volume-title": "SACN vitamin D and health report",
"year": "2016"
},
{
"author": "British Nutrition Foundation",
"key": "2023052222031285500_R5",
"volume-title": "BNF busts the myths on nutrition and COVID-19",
"year": "2020"
},
{
"author": "GOV.UK",
"key": "2023052222031285500_R6",
"volume-title": "COVID-19: investigation and initial clinical management of possible cases",
"year": "2020"
},
{
"DOI": "10.1210/jc.2018-01414",
"article-title": "Controversies in vitamin D: summary statement from an international conference",
"author": "Giustina",
"doi-asserted-by": "crossref",
"first-page": "234",
"journal-title": "J Clin Endocrinol Metab",
"key": "2023052222031285500_R7",
"volume": "104",
"year": "2019"
},
{
"DOI": "10.1503/cmaj.050051",
"article-title": "Global clinical measure of fitness and frailty in elderly people",
"author": "Rockwood",
"doi-asserted-by": "crossref",
"first-page": "489",
"journal-title": "CMAJ",
"key": "2023052222031285500_R8",
"volume": "173",
"year": "2005"
},
{
"DOI": "10.1016/0021-9681(87)90171-8",
"article-title": "A new method of classifying prognostic comorbidity in longitudinal studies: development and validation",
"author": "Charlson",
"doi-asserted-by": "crossref",
"first-page": "373",
"journal-title": "J Chronic Dis",
"key": "2023052222031285500_R9",
"volume": "40",
"year": "1987"
},
{
"DOI": "10.1515/cclm-2020-0198",
"article-title": "Laboratory abnormalities in patients with COVID-2019 infection",
"author": "Lippi",
"doi-asserted-by": "crossref",
"first-page": "1131",
"journal-title": "Clin Chem Lab Med",
"key": "2023052222031285500_R10",
"volume": "58",
"year": "2020"
},
{
"DOI": "10.1148/radiol.2020201160",
"article-title": "Frequency and distribution of chest radiographic findings in COVID-19 positive patients",
"author": "Wong",
"doi-asserted-by": "crossref",
"first-page": "E72",
"journal-title": "Radiology",
"key": "2023052222031285500_R11",
"volume": "296",
"year": "2020"
},
{
"DOI": "10.1016/S1473-3099(20)30086-4",
"article-title": "Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study",
"author": "Shi",
"doi-asserted-by": "crossref",
"first-page": "425",
"journal-title": "Lancet Infect Dis",
"key": "2023052222031285500_R12",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.3390/nu12051359",
"article-title": "25-hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2",
"author": "D’Avolio",
"doi-asserted-by": "crossref",
"first-page": "1359",
"journal-title": "Nutrients",
"key": "2023052222031285500_R13",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1007/s40520-020-01570-8",
"article-title": "The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality",
"author": "Ilie",
"doi-asserted-by": "crossref",
"first-page": "1195",
"journal-title": "Aging Clin Exp Res",
"key": "2023052222031285500_R14",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.1016/j.dsx.2020.04.050",
"article-title": "Vitamin D concentrations and COVID-19 infection in UK Biobank",
"author": "Hastie",
"doi-asserted-by": "crossref",
"first-page": "561",
"journal-title": "Diabetes Metab Syndr",
"key": "2023052222031285500_R15",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1016/j.cyto.2008.12.009",
"article-title": "1Alpha,25-dihydroxyvitamin D3 inhibits CD40L-induced pro-inflammatory and immunomodulatory activity in human monocytes",
"author": "Almerighi",
"doi-asserted-by": "crossref",
"first-page": "190",
"journal-title": "Cytokine",
"key": "2023052222031285500_R16",
"volume": "45",
"year": "2009"
},
{
"DOI": "10.1002/1521-4141(200002)30:2<498::AID-IMMU498>3.0.CO;2-Q",
"article-title": "Inhibition of Th1 development and treatment of chronic-relapsing experimental allergic encephalomyelitis by a non-hypercalcemic analogue of 1,25-dihydroxyvitamin D(3)",
"author": "Mattner",
"doi-asserted-by": "crossref",
"first-page": "498",
"journal-title": "Eur J Immunol",
"key": "2023052222031285500_R17",
"volume": "30",
"year": "2000"
},
{
"article-title": "Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individuals participant data",
"author": "Martineau",
"first-page": "i6583",
"key": "2023052222031285500_R18",
"volume-title": "BMJ",
"year": "2017"
},
{
"DOI": "10.1016/S2352-3026(20)30145-9",
"article-title": "Coagulation abnormalities and thrombosis in patients with COVID-19.",
"author": "Levi",
"doi-asserted-by": "crossref",
"first-page": "e438",
"issue": "6",
"journal-title": "Lancet Haematol",
"key": "2023052222031285500_R19",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1016/S2213-2600(20)30216-2",
"article-title": "COVID-19 cytokine storm: the interplay between inflammation and coagulation.",
"author": "Jose",
"doi-asserted-by": "crossref",
"first-page": "e46",
"issue": "6",
"journal-title": "The Lancet Respiratory Medicine",
"key": "2023052222031285500_R20",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1378/chest.121.4.1262",
"article-title": "D-dimer correlates with proinflammatory cytokine levels and outcomes in critically ill patients",
"author": "Shorr",
"doi-asserted-by": "crossref",
"first-page": "1262",
"journal-title": "Chest",
"key": "2023052222031285500_R21",
"volume": "121",
"year": "2002"
},
{
"DOI": "10.4049/jimmunol.167.9.4974",
"article-title": "1alpha,25-Dihydroxyvitamin d3 has a direct effect on naive CD4(+) T cells to enhance the development of Th2 cells",
"author": "Boonstra",
"doi-asserted-by": "crossref",
"first-page": "4974",
"journal-title": "J Immunol",
"key": "2023052222031285500_R22",
"volume": "167",
"year": "2001"
},
{
"DOI": "10.4049/jimmunol.0801543",
"article-title": "Calcitriol suppresses antiretinal autoimmunity through inhibitory effects on the Th17 effector response",
"author": "Tang",
"doi-asserted-by": "crossref",
"first-page": "4624",
"journal-title": "J Immunol",
"key": "2023052222031285500_R23",
"volume": "182",
"year": "2009"
},
{
"DOI": "10.1124/jpet.107.127209",
"article-title": "Immune modulatory treatment of trinitrobenzene sulfonic acid colitis with calcitriol is associated with a change of a T helper (Th) 1/Th17 to a Th2 and regulatory T cell profile",
"author": "Daniel",
"doi-asserted-by": "crossref",
"first-page": "23",
"journal-title": "J Pharmacol Exp Ther",
"key": "2023052222031285500_R24",
"volume": "324",
"year": "2008"
},
{
"DOI": "10.1084/jem.20011629",
"article-title": "In vitro generation of interleukin 10-producing regulatory CD4(+) T cells is induced by immunosuppressive drugs and inhibited by T helper type 1 (Th1)- and Th2-inducing cytokines",
"author": "Barrat",
"doi-asserted-by": "crossref",
"first-page": "603",
"journal-title": "J Exp Med",
"key": "2023052222031285500_R25",
"volume": "195",
"year": "2002"
},
{
"DOI": "10.4049/jimmunol.179.9.6273",
"article-title": "Topically applied 1,25-dihydroxyvitamin D3 enhances the suppressive activity of CD4+CD25+ cells in the draining lymph nodes",
"author": "Gorman",
"doi-asserted-by": "crossref",
"first-page": "6273",
"journal-title": "J Immunol",
"key": "2023052222031285500_R26",
"volume": "179",
"year": "2007"
},
{
"DOI": "10.1182/blood-2005-05-2044",
"article-title": "Expression of the inhibitory receptor ILT3 on dendritic cells is dispensable for induction of CD4+Foxp3+ regulatory T cells by 1,25-dihydroxyvitamin D3",
"author": "Penna",
"doi-asserted-by": "crossref",
"first-page": "3490",
"journal-title": "Blood",
"key": "2023052222031285500_R27",
"volume": "106",
"year": "2005"
},
{
"DOI": "10.1136/thoraxjnl-2014-206680",
"article-title": "Vitamin D deficiency contributes directly to the acute respiratory distress syndrome (ARDS)",
"author": "Dancer",
"doi-asserted-by": "crossref",
"first-page": "617",
"journal-title": "Thorax",
"key": "2023052222031285500_R28",
"volume": "70",
"year": "2015"
},
{
"DOI": "10.1371/journal.pone.0140370",
"article-title": "Dietary vitamin D and its metabolites non-genomically stabilize the endothelium",
"author": "Gibson",
"doi-asserted-by": "crossref",
"first-page": "e0140370",
"journal-title": "PLoS One",
"key": "2023052222031285500_R29",
"volume": "10",
"year": "2015"
},
{
"DOI": "10.1016/j.coph.2006.03.001",
"article-title": "Angiotensin-converting enzyme 2 in lung diseases",
"author": "Kuka",
"doi-asserted-by": "crossref",
"first-page": "271",
"journal-title": "Curr Opin Pharmacol",
"key": "2023052222031285500_R30",
"volume": "6",
"year": "2006"
},
{
"article-title": "COVID-19 rapid guideline: critical care in adults [NG159]",
"author": "National Institute for Health and Care Excellence (NICE)",
"key": "2023052222031285500_R31",
"year": "2020"
},
{
"DOI": "10.1016/j.maturitas.2014.11.018",
"article-title": "National osteoporosis society practical clinical guideline on vitamin D and bone health",
"author": "Francis",
"doi-asserted-by": "crossref",
"first-page": "119",
"journal-title": "Maturitas",
"key": "2023052222031285500_R32",
"volume": "80",
"year": "2015"
}
],
"reference-count": 32,
"references-count": 32,
"relation": {},
"resource": {
"primary": {
"URL": "https://academic.oup.com/pmj/article/97/1149/442/6969666"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Vitamin D status and outcomes for hospitalised older patients with COVID-19",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1136/crossmarkpolicy",
"volume": "97"
}
