Effect of a Single High Dose of Vitamin D3 on Hospital Length of Stay in Patients With Moderate to Severe COVID-19: A Randomized Clinical Trial
et al., JAMA, doi:10.1001/jama.2020.26848, NCT04449718, Nov 2020 (preprint)
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Very late stage (mean 10 days from symptom onset, 90% on oxygen at baseline) vitamin D supplementation RCT not showing significant differences.
Ethnicity was poorly matched between arms, and diabetes was 41% in the treatment arm vs. 29% in the control arm. Baseline ventilation was 15% in the treatment arm vs. 12% control. Calcifediol or calcitriol, which avoids several days delay in conversion, may be more successful, especially with this very late stage usage. Treatment was dissolved in 10mL of peanut oil.
Cholecalciferol was used in this study.
Meta-analysis shows that late stage treatment with calcitriol / calcifediol (or
paricalcitol, alfacalcidol, etc.) is more effective than cholecalciferol: 66% [47‑78%] lower risk vs. 45% [34‑54%] lower risk.
Cholecalciferol requires two hydroxylation steps to become activated - first
in the liver to calcifediol, then in the kidney to calcitriol. Calcitriol,
paricalcitol, and alfacalcidol are active vitamin D analogs that do not
require conversion. This allows them to have more rapid onset of action
compared to cholecalciferol. The time delay for cholecalciferol to increase
serum calcifediol levels can be 2-3 days, and the delay for converting
calcifediol to active calcitriol can be up to 7 days.
Bolus treatment is less effective.
Pharmacokinetics and the potential side effects of high bolus doses suggest
that ongoing treatment spread over time is more appropriate.
Research has confirmed that lower dose regular treatment with vitamin D is more
effective than intermittent high-dose bolus treatment for various conditions,
including rickets and acute respiratory infections1,2. The biological mechanisms supporting these
findings involve the induction of enzymes such as 24-hydroxylase and
fibroblast growth factor 23 (FGF23) by high-dose bolus treatments. These
enzymes play roles in inactivating vitamin D, which can paradoxically reduce
levels of activated vitamin D and suppress its activation for extended periods
post-dosage. Evidence indicates that 24-hydroxylase activity may remain
elevated for several weeks following a bolus dose, leading to reduced levels
of the activated form of vitamin D. Additionally, FGF23 levels can increase
for at least three months after a large bolus dose, which also contributes to
the suppression of vitamin D activation1.
This is the 3rd of 40 COVID-19 RCTs for vitamin D, which collectively show efficacy with p=0.0000001.
This is the 12th of 135 COVID-19 controlled studies for vitamin D, which collectively show efficacy with p<0.0000000001.
This study is excluded in the after exclusion results of meta-analysis:
very late stage, >50% on oxygen/ventilation at baseline; very late stage study using cholecalciferol instead of calcifediol or calcitriol.
|
risk of death, 48.7% higher, RR 1.49, p = 0.43, treatment 9 of 119 (7.6%), control 6 of 118 (5.1%).
|
|
risk of mechanical ventilation, 47.5% lower, RR 0.52, p = 0.09, treatment 9 of 119 (7.6%), control 17 of 118 (14.4%), NNT 15.
|
|
risk of ICU admission, 24.6% lower, RR 0.75, p = 0.30, treatment 19 of 119 (16.0%), control 25 of 118 (21.2%), NNT 19.
|
|
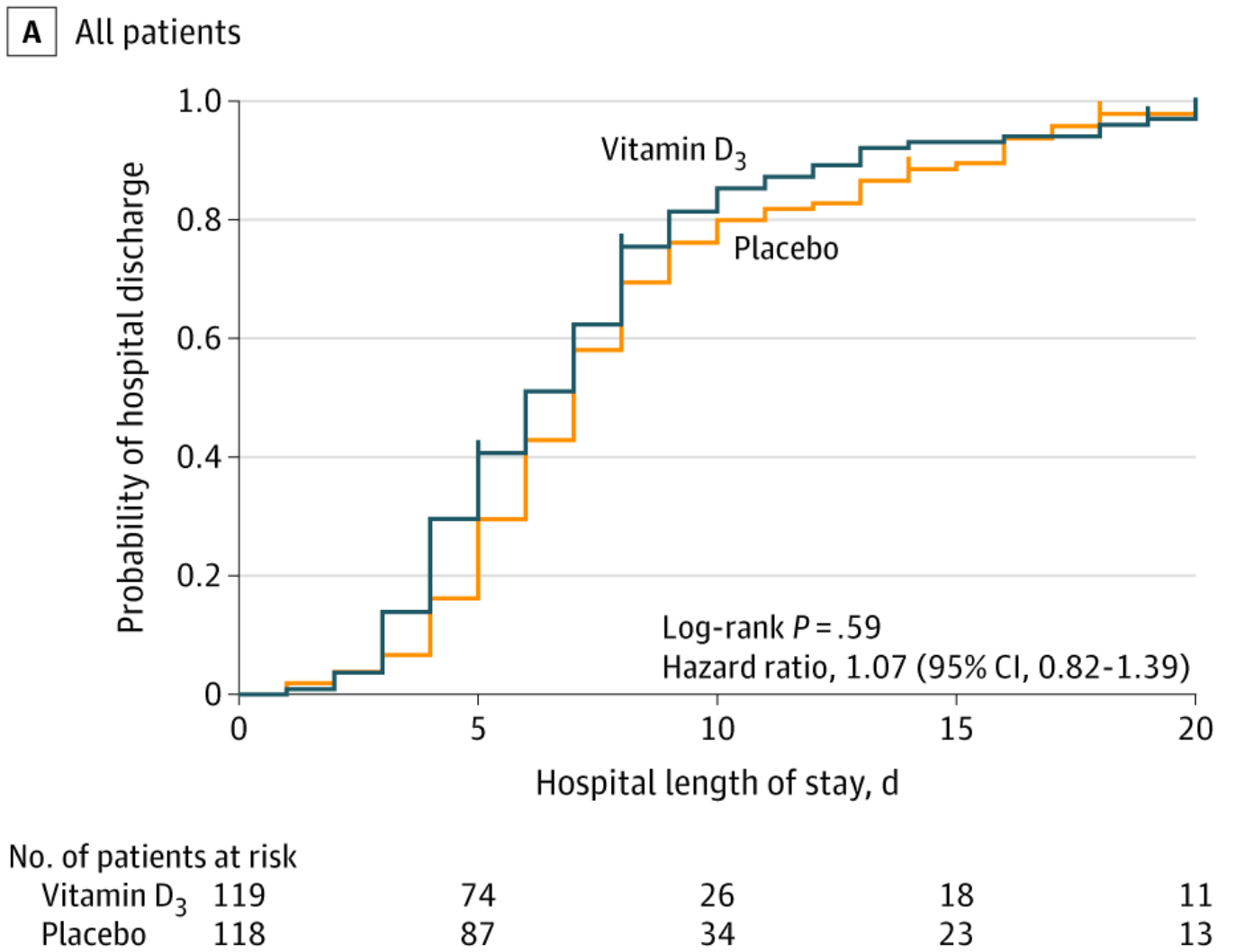
risk of no hospital discharge, 6.5% lower, HR 0.93, p = 0.63, treatment 119, control 118, inverted to make HR<1 favor treatment.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Murai et al., 17 Nov 2020, Double Blind Randomized Controlled Trial, Brazil, peer-reviewed, 17 authors, study period 2 June, 2020 - 27 August, 2020, average treatment delay 10.2 days, dosage 200,000IU single dose, trial NCT04449718 (history).
Effect of a Single High Dose of Vitamin D3 on Hospital Length of Stay in Patients With Moderate to Severe COVID-19
JAMA, doi:10.1001/jama.2020.26848
IMPORTANCE The efficacy of vitamin D 3 supplementation in coronavirus disease 2019 (COVID-19) remains unclear. OBJECTIVE To investigate the effect of a single high dose of vitamin D 3 on hospital length of stay in patients with COVID-19.
DESIGN, SETTING, AND PARTICIPANTS This was a multicenter, double-blind, randomized, placebo-controlled trial conducted in 2 sites in Sao Paulo, Brazil. The study included 240 hospitalized patients with COVID-19 who were moderately to severely ill at the time of enrollment from June 2, 2020, to August 27, 2020. The final follow-up was on October 7, 2020. INTERVENTIONS Patients were randomly assigned to receive a single oral dose of 200 000 IU of vitamin D 3 (n = 120) or placebo (n = 120).
MAIN OUTCOMES AND MEASURES The primary outcome was length of stay, defined as the time from the date of randomization to hospital discharge. Prespecified secondary outcomes included mortality during hospitalization; the number of patients admitted to the intensive care unit; the number of patients who required mechanical ventilation and the duration of mechanical ventilation; and serum levels of 25-hydroxyvitamin D, total calcium, creatinine, and C-reactive protein.
RESULTS Of 240 randomized patients, 237 were included in the primary analysis (mean [SD] age, 56.2 [14.4] years; 104 [43.9%] women; mean [SD] baseline 25-hydroxyvitamin D level, 20.9 [9.2] ng/mL). Median (interquartile range) length of stay was not significantly different between the vitamin D 3 (7.0 [4.0-10.0] days) and placebo groups (7.0 [5.0-13.0] days) (log-rank P = .59; unadjusted hazard ratio for hospital discharge, 1.07 [95% CI, 0.82-1.39]; P = .62). The difference between the vitamin D 3 group and the placebo group was not significant for in-hospital mortality (7.6% vs 5.1%; difference, 2.5% [95% CI, -4.1% to 9.2%]; P = .43), admission to the intensive care unit (16.0% vs 21.2%; difference, -5.2% [95% CI, -15.1% to 4.7%]; P = .30), or need for mechanical ventilation (7.6% vs 14.4%; difference, -6.8% [95% CI, -15.1% to 1.2%]; P = .09). Mean serum levels of 25-hydroxyvitamin D significantly increased after a single dose of vitamin D 3 vs placebo (44.4 ng/mL vs 19.8 ng/mL; difference, 24.1 ng/mL [95% CI, 19.5-28.7]; P < .001). There were no adverse events, but an episode of vomiting was associated with the intervention. CONCLUSIONS AND RELEVANCE Among hospitalized patients with COVID-19, a single high dose of vitamin D 3 , compared with placebo, did not significantly reduce hospital length of stay. The findings do not support the use of a high dose of vitamin D 3 for treatment of moderate to severe COVID-19.
Author Contributions: Dr Pereira had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Drs Murai
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. Data Sharing Statement: See Supplement 3.
Additional Contributions: The authors are thankful to Monica Pinheiro, MD, MSc, and Roberta Costa, MSc (Ibirapuera field hospital), for assistance with the study; Cleuber Esteves Chaves, BSc (pharmacy unit of the clinical hospital), for the vitamin D 3 and placebo solution preparation; Rogério Ruscitto do Prado, PhD (Albert Einstein Hospital), for conducting statistical analyses; Cibele Russo, PhD (University of Sao Paulo), for statistical review; Mayara Diniz Santos, MS (School of Medicine of University of Sao Paulo), for technical support; all of the staff members from both centers; and all of the patients who participated in this study. None of these individuals received compensation for their participation.
References
Aglipay, Birken, Parkin, Effect of high-dose vs standard-dose wintertime vitamin D supplementation on viral upper respiratory tract infections in young healthy children, JAMA, doi:10.1001/jama.2017.8708?utm_campaign=articlePDF%26utm_medium=articlePDFlink%26utm_source=articlePDF%26utm_content=jama.2020.26848
Aibana, Huang, Aboud, Vitamin D status and risk of incident tuberculosis disease: a nested case-control study, systematic review, and individual-participant data meta-analysis, PLoS Med, doi:10.1371/journal.pmed.1002907
Autier, Boniol, Pizot, Mullie, Vitamin D status and ill health: a systematic review, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(13)70165-7
Bacchetti, Current sample size conventions: flaws, harms, and alternatives, BMC Med, doi:10.1186/1741-7015-8-17
Bacchetti, Mcculloch, Segal, Franco, Freitas et al., Vitamin D supplementation and disease activity in patients with immune-mediated rheumatic diseases: a systematic review and meta-analysis, Biometrics, doi:10.1097/MD.0000000000007024
Bilezikian, Bikle, Hewison, Mechanisms in endocrinology: vitamin D and COVID-19, Eur J Endocrinol, doi:10.1530/EJE-20-0665
Campbell, Spector, Etten, Mathieu, Autophagy induction by vitamin D inhibits both Mycobacterium tuberculosis and human immunodeficiency virus type 1, J Steroid Biochem Mol Biol, doi:10.1016/j.jsbmb.2005.06.002
Cannell, Vieth, Umhau, Epidemic influenza and vitamin D, Epidemiol Infect, doi:10.1017/S0950268806007175
Carpagnano, Lecce, Quaranta, Vitamin D supplementation associated to better survival in hospitalized frail elderly COVID-19 patients: the GERIA-COVID quasi-experimental study, J Endocrinol Invest. Published online, doi:10.3390/nu12113377
Hernández, Nan, Fernandez-Ayala, Vitamin D status in hospitalized patients with SARS-CoV-2 infection, J Clin Endocrinol Metab, doi:10.1210/clinem/dgaa733
Ilie, Stefanescu, Smith, The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality, Aging Clin Exp Res, doi:10.1007/s40520-020-01570-8
Kaufman, Niles, Kroll, Bi, Holick, SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels, PLoS One, doi:10.1371/journal.pone.0239252
Kearns, Alvarez, Tangpricha, Large, single-dose, oral vitamin D supplementation in adult populations: a systematic review, Endocr Pract, doi:10.4158/EP13265.RA
Laplana, Royo, Fibla, Vitamin D receptor polymorphisms and risk of enveloped virus infection: a meta-analysis, Gene, doi:10.1016/j.gene.2018.08.017
Liu, Stenger, Li, Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response, Science, doi:10.1126/science.1123933
Martineau, Forouhi, Vitamin D for COVID-19: a case to answer?, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30268-0
Martineau, Jolliffe, Hooper, Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data, BMJ, doi:10.1136/bmj.i6583
Meltzer, Best, Zhang, Vokes, Arora et al., Association of vitamin D status and other clinical characteristics with COVID-19 test results, JAMA Netw Open, doi:10.1001/jamanetworkopen.2020.19722?utm_campaign=articlePDF%26utm_medium=articlePDFlink%26utm_source=articlePDF%26utm_content=jama.2020.26848
Mitchell, Vitamin-D and COVID-19: do deficient risk a poorer outcome?, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30183-2
Sabetta, Depetrillo, Cipriani, Smardin, Burns et al., Serum 25-hydroxyvitamin d and the incidence of acute viral respiratory tract infections in healthy adults, PLoS One, doi:10.1371/journal.pone.0011088
DOI record:
{
"DOI": "10.1001/jama.2020.26848",
"ISSN": [
"0098-7484"
],
"URL": "http://dx.doi.org/10.1001/jama.2020.26848",
"author": [
{
"affiliation": [
{
"name": "Rheumatology Division, Hospital das Clinicas HCFMUSP, Faculdade de Medicina da Universidade de Sao Paulo, Sao Paulo, Brazil"
}
],
"family": "Murai",
"given": "Igor H.",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Rheumatology Division, Hospital das Clinicas HCFMUSP, Faculdade de Medicina da Universidade de Sao Paulo, Sao Paulo, Brazil"
}
],
"family": "Fernandes",
"given": "Alan L.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Rheumatology Division, Hospital das Clinicas HCFMUSP, Faculdade de Medicina da Universidade de Sao Paulo, Sao Paulo, Brazil"
}
],
"family": "Sales",
"given": "Lucas P.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Applied Physiology & Nutrition Research Group, Faculdade de Medicina da Universidade de Sao Paulo, Sao Paulo, Brazil"
}
],
"family": "Pinto",
"given": "Ana J.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Applied Physiology & Nutrition Research Group, Faculdade de Medicina da Universidade de Sao Paulo, Sao Paulo, Brazil"
}
],
"family": "Goessler",
"given": "Karla F.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Rheumatology Division, Hospital das Clinicas HCFMUSP, Faculdade de Medicina da Universidade de Sao Paulo, Sao Paulo, Brazil"
}
],
"family": "Duran",
"given": "Camila S. C.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Rheumatology Division, Hospital das Clinicas HCFMUSP, Faculdade de Medicina da Universidade de Sao Paulo, Sao Paulo, Brazil"
}
],
"family": "Silva",
"given": "Carla B. R.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Rheumatology Division, Hospital das Clinicas HCFMUSP, Faculdade de Medicina da Universidade de Sao Paulo, Sao Paulo, Brazil"
}
],
"family": "Franco",
"given": "André S.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Rheumatology Division, Hospital das Clinicas HCFMUSP, Faculdade de Medicina da Universidade de Sao Paulo, Sao Paulo, Brazil"
}
],
"family": "Macedo",
"given": "Marina B.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Rheumatology Division, Hospital das Clinicas HCFMUSP, Faculdade de Medicina da Universidade de Sao Paulo, Sao Paulo, Brazil"
}
],
"family": "Dalmolin",
"given": "Henrique H. H.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Rheumatology Division, Hospital das Clinicas HCFMUSP, Faculdade de Medicina da Universidade de Sao Paulo, Sao Paulo, Brazil"
}
],
"family": "Baggio",
"given": "Janaina",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Rheumatology Division, Hospital das Clinicas HCFMUSP, Faculdade de Medicina da Universidade de Sao Paulo, Sao Paulo, Brazil"
}
],
"family": "Balbi",
"given": "Guilherme G. M.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Rheumatology Division, Hospital das Clinicas HCFMUSP, Faculdade de Medicina da Universidade de Sao Paulo, Sao Paulo, Brazil"
}
],
"family": "Reis",
"given": "Bruna Z.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Clinical Pathology Division, Hospital das Clinicas HCFMUSP, Faculdade de Medicina da Universidade de Sao Paulo, Sao Paulo, Brazil"
}
],
"family": "Antonangelo",
"given": "Leila",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Rheumatology Division, Hospital das Clinicas HCFMUSP, Faculdade de Medicina da Universidade de Sao Paulo, Sao Paulo, Brazil"
}
],
"family": "Caparbo",
"given": "Valeria F.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Applied Physiology & Nutrition Research Group, Faculdade de Medicina da Universidade de Sao Paulo, Sao Paulo, Brazil"
},
{
"name": "Food Research Center, Universidade de Sao Paulo, Sao Paulo, Brazil"
}
],
"family": "Gualano",
"given": "Bruno",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Rheumatology Division, Hospital das Clinicas HCFMUSP, Faculdade de Medicina da Universidade de Sao Paulo, Sao Paulo, Brazil"
}
],
"family": "Pereira",
"given": "Rosa M. R.",
"sequence": "additional"
}
],
"container-title": "JAMA",
"container-title-short": "JAMA",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
2,
20
]
],
"date-time": "2021-02-20T15:58:59Z",
"timestamp": 1613836739000
},
"deposited": {
"date-parts": [
[
2021,
3,
16
]
],
"date-time": "2021-03-16T17:59:00Z",
"timestamp": 1615917540000
},
"indexed": {
"date-parts": [
[
2024,
4,
2
]
],
"date-time": "2024-04-02T15:01:53Z",
"timestamp": 1712070113879
},
"is-referenced-by-count": 354,
"issue": "11",
"issued": {
"date-parts": [
[
2021,
3,
16
]
]
},
"journal-issue": {
"issue": "11",
"published-print": {
"date-parts": [
[
2021,
3,
16
]
]
}
},
"language": "en",
"link": [
{
"URL": "https://jamanetwork.com/journals/jama/articlepdf/2776738/jama_murai_2021_oi_200145_1615225415.22388.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "10",
"original-title": [],
"page": "1053",
"prefix": "10.1001",
"published": {
"date-parts": [
[
2021,
3,
16
]
]
},
"published-print": {
"date-parts": [
[
2021,
3,
16
]
]
},
"publisher": "American Medical Association (AMA)",
"reference": [
{
"DOI": "10.1126/science.1123933",
"article-title": "Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response.",
"author": "Liu",
"doi-asserted-by": "publisher",
"first-page": "1770",
"issue": "5768",
"journal-title": "Science",
"key": "joi200145r1",
"volume": "311",
"year": "2006"
},
{
"DOI": "10.1001/jama.2017.8708",
"article-title": "Effect of high-dose vs standard-dose wintertime vitamin D supplementation on viral upper respiratory tract infections in young healthy children.",
"author": "Aglipay",
"doi-asserted-by": "publisher",
"first-page": "245",
"issue": "3",
"journal-title": "JAMA",
"key": "joi200145r2",
"volume": "318",
"year": "2017"
},
{
"DOI": "10.4161/auto.21154",
"article-title": "Autophagy induction by vitamin D inhibits both Mycobacterium tuberculosis and human immunodeficiency virus type 1.",
"author": "Campbell",
"doi-asserted-by": "publisher",
"first-page": "1523",
"issue": "10",
"journal-title": "Autophagy",
"key": "joi200145r3",
"volume": "8",
"year": "2012"
},
{
"DOI": "10.1016/j.jsbmb.2005.06.002",
"article-title": "Immunoregulation by 1,25-dihydroxyvitamin D3: basic concepts.",
"author": "van Etten",
"doi-asserted-by": "publisher",
"first-page": "93",
"issue": "1-2",
"journal-title": "J Steroid Biochem Mol Biol",
"key": "joi200145r4",
"volume": "97",
"year": "2005"
},
{
"DOI": "10.1016/j.gene.2018.08.017",
"article-title": "Vitamin D receptor polymorphisms and risk of enveloped virus infection: a meta-analysis.",
"author": "Laplana",
"doi-asserted-by": "publisher",
"first-page": "384",
"journal-title": "Gene",
"key": "joi200145r5",
"volume": "678",
"year": "2018"
},
{
"DOI": "10.1530/EJE-20-0665",
"article-title": "Mechanisms in endocrinology: vitamin D and COVID-19.",
"author": "Bilezikian",
"doi-asserted-by": "publisher",
"first-page": "R133",
"issue": "5",
"journal-title": "Eur J Endocrinol",
"key": "joi200145r6",
"volume": "183",
"year": "2020"
},
{
"DOI": "10.1016/S2213-8587(13)70165-7",
"article-title": "Vitamin D status and ill health: a systematic review.",
"author": "Autier",
"doi-asserted-by": "publisher",
"first-page": "76",
"issue": "1",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "joi200145r7",
"volume": "2",
"year": "2014"
},
{
"DOI": "10.1371/journal.pmed.1002907",
"article-title": "Vitamin D status and risk of incident tuberculosis disease: a nested case-control study, systematic review, and individual-participant data meta-analysis.",
"author": "Aibana",
"doi-asserted-by": "crossref",
"issue": "9",
"journal-title": "PLoS Med",
"key": "joi200145r8",
"volume": "16",
"year": "2019"
},
{
"DOI": "10.1136/bmj.i6583",
"article-title": "Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data.",
"author": "Martineau",
"doi-asserted-by": "publisher",
"first-page": "i6583",
"journal-title": "BMJ",
"key": "joi200145r9",
"volume": "356",
"year": "2017"
},
{
"DOI": "10.1371/journal.pone.0011088",
"article-title": "Serum 25-hydroxyvitamin d and the incidence of acute viral respiratory tract infections in healthy adults.",
"author": "Sabetta",
"doi-asserted-by": "crossref",
"issue": "6",
"journal-title": "PLoS One",
"key": "joi200145r10",
"volume": "5",
"year": "2010"
},
{
"DOI": "10.1016/S2213-8587(20)30183-2",
"article-title": "Vitamin-D and COVID-19: do deficient risk a poorer outcome?",
"author": "Mitchell",
"doi-asserted-by": "publisher",
"first-page": "570",
"issue": "7",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "joi200145r11",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/S2213-8587(20)30268-0",
"article-title": "Vitamin D for COVID-19: a case to answer?",
"author": "Martineau",
"doi-asserted-by": "publisher",
"first-page": "735",
"issue": "9",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "joi200145r12",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1001/jamanetworkopen.2020.19722",
"article-title": "Association of vitamin D status and other clinical characteristics with COVID-19 test results.",
"author": "Meltzer",
"doi-asserted-by": "crossref",
"issue": "9",
"journal-title": "JAMA Netw Open",
"key": "joi200145r13",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0239252",
"article-title": "SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels.",
"author": "Kaufman",
"doi-asserted-by": "crossref",
"issue": "9",
"journal-title": "PLoS One",
"key": "joi200145r14",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1007/s40520-020-01570-8",
"article-title": "The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality.",
"author": "Ilie",
"doi-asserted-by": "publisher",
"first-page": "1195",
"issue": "7",
"journal-title": "Aging Clin Exp Res",
"key": "joi200145r15",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.4158/EP13265.RA",
"article-title": "Large, single-dose, oral vitamin D supplementation in adult populations: a systematic review.",
"author": "Kearns",
"doi-asserted-by": "publisher",
"first-page": "341",
"issue": "4",
"journal-title": "Endocr Pract",
"key": "joi200145r16",
"volume": "20",
"year": "2014"
},
{
"DOI": "10.1186/1741-7015-8-17",
"article-title": "Current sample size conventions: flaws, harms, and alternatives.",
"author": "Bacchetti",
"doi-asserted-by": "publisher",
"first-page": "17",
"journal-title": "BMC Med",
"key": "joi200145r17",
"volume": "8",
"year": "2010"
},
{
"DOI": "10.1111/j.1541-0420.2008.01004_1.x",
"article-title": "Simple, defensible sample sizes based on cost efficiency.",
"author": "Bacchetti",
"doi-asserted-by": "publisher",
"first-page": "577",
"issue": "2",
"journal-title": "Biometrics",
"key": "joi200145r18",
"volume": "64",
"year": "2008"
},
{
"DOI": "10.1097/MD.0000000000007024",
"article-title": "Vitamin D supplementation and disease activity in patients with immune-mediated rheumatic diseases: a systematic review and meta-analysis.",
"author": "Franco",
"doi-asserted-by": "crossref",
"issue": "23",
"journal-title": "Medicine (Baltimore)",
"key": "joi200145r19",
"volume": "96",
"year": "2017"
},
{
"DOI": "10.1017/S0950268806007175",
"article-title": "Epidemic influenza and vitamin D.",
"author": "Cannell",
"doi-asserted-by": "publisher",
"first-page": "1129",
"issue": "6",
"journal-title": "Epidemiol Infect",
"key": "joi200145r20",
"volume": "134",
"year": "2006"
},
{
"article-title": "Vitamin D deficiency as a predictor of poor prognosis in patients with acute respiratory failure due to COVID-19.",
"author": "Carpagnano",
"journal-title": "J Endocrinol Invest",
"key": "joi200145r21",
"year": "2020"
},
{
"DOI": "10.3390/nu12113377",
"article-title": "Vitamin D supplementation associated to better survival in hospitalized frail elderly COVID-19 patients: the GERIA-COVID quasi-experimental study.",
"author": "Annweiler",
"doi-asserted-by": "crossref",
"issue": "11",
"journal-title": "Nutrients",
"key": "joi200145r22",
"volume": "12",
"year": "2020"
},
{
"article-title": "Vitamin D status in hospitalized patients with SARS-CoV-2 infection.",
"author": "Hernández",
"journal-title": "J Clin Endocrinol Metab",
"key": "joi200145r23",
"year": "2020"
}
],
"reference-count": 23,
"references-count": 23,
"relation": {},
"resource": {
"primary": {
"URL": "https://jamanetwork.com/journals/jama/fullarticle/2776738"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [
"A Randomized Clinical Trial"
],
"title": "Effect of a Single High Dose of Vitamin D<sub>3</sub> on Hospital Length of Stay in Patients With Moderate to Severe COVID-19",
"type": "journal-article",
"volume": "325"
}
