Vitamin D Status in Hospitalized Patients with SARS-CoV-2 Infection
et al., The Journal of Clinical Endocrinology & Metabolism, doi:10.1210/clinem/dgaa733, Oct 2020
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
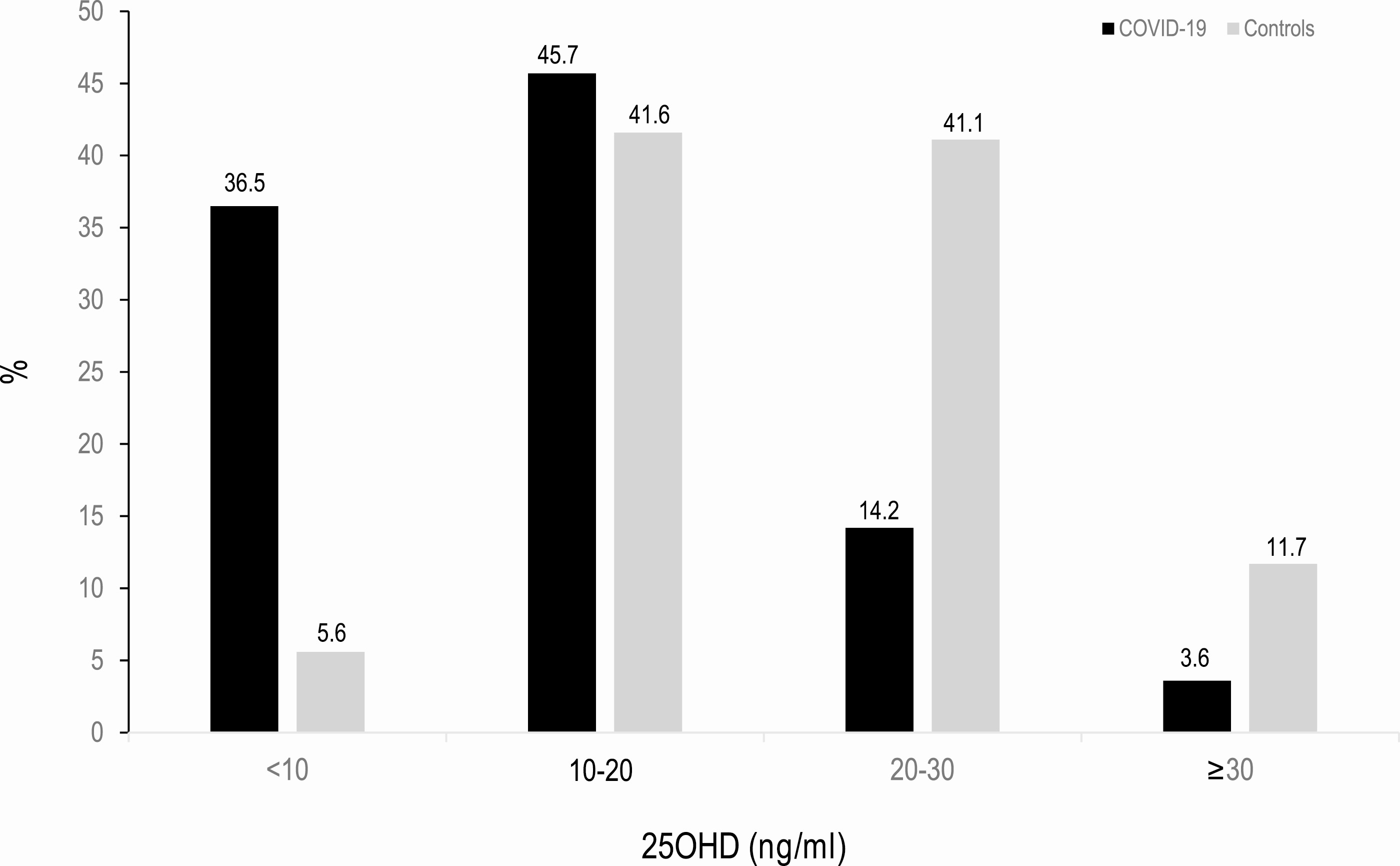
Retrospective 216 COVID-19 patients and 197 population controls, showing vitamin D deficiency in 82.2% of COVID-19 cases and 47.2% of population-based controls (P < 0.0001). Authors note: "We did not find any relationship between vitamin D concentrations or vitamin deficiency and the severity of the disease". While no association was found within hospitalized patients, there is an association with hospitalization, and hospitalization is an indication of COVID-19 severity.
19 of the COVID-19 patients were taking vitamin D supplements, showing lower ventilation and ICU admission, but no significant difference in mortality.
This is the 23rd of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
risk of combined death/ICU/ventilation, 83.0% lower, RR 0.17, p < 0.001, high D levels 35, low D levels 162, ≥20ng/mL risk of hospitalization * risk of death/ICU/ventilation | hospitalization.
|
|
risk of combined death/ICU/ventilation if hospitalized, 12.0% lower, RR 0.88, p = 0.86, high D levels 35, low D levels 162, ≥20ng/mL risk of death/ICU/ventilation | hospitalization.
|
|
risk of hospitalization, 80.6% lower, RR 0.19, p < 0.001, ≥20ng/mL.
|
|
risk of death, 3.7% higher, RR 1.04, p = 1.00, high D levels 2 of 19 (10.5%), low D levels 20 of 197 (10.2%), supplementation.
|
|
risk of mechanical ventilation, 75.9% lower, RR 0.24, p = 0.13, high D levels 1 of 19 (5.3%), low D levels 43 of 197 (21.8%), NNT 6.0, supplementation.
|
|
risk of ICU admission, 79.3% lower, RR 0.21, p = 0.05, high D levels 1 of 19 (5.3%), low D levels 50 of 197 (25.4%), NNT 5.0, supplementation.
|
|
hospitalization time, 33.3% lower, relative time 0.67, p = 0.11, high D levels 19, low D levels 197, supplementation.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Hernández et al., 27 Oct 2020, retrospective, Spain, peer-reviewed, mean age 60.9, 12 authors.
Vitamin D Status in Hospitalized Patients with SARS-CoV-2 Infection
The Journal of Clinical Endocrinology & Metabolism, doi:10.1210/clinem/dgaa733
Background: The role of vitamin D status in COVID-19 patients is a matter of debate. Objectives: To assess serum 25-hydroxyvitamin D (25OHD) levels in hospitalized patients with COVID-19 and to analyze the possible influence of vitamin D status on disease severity. Methods: Retrospective case-control study of 216 COVID-19 patients and 197 populationbased controls. Serum 25OHD levels were measured in both groups. The association of serum 25OHD levels with COVID-19 severity (admission to the intensive care unit, requirements for mechanical ventilation, or mortality) was also evaluated. Results: Of the 216 patients, 19 were on vitamin D supplements and were analyzed separately. In COVID-19 patients, mean ± standard deviation 25OHD levels were 13.8 ± 7.2 ng/mL, compared with 20.9 ± 7.4 ng/mL in controls (P < .0001). 25OHD values were lower in men than in women. Vitamin D deficiency was found in 82.2% of COVID-19 cases and 47.2% of population-based controls (P < .0001). 25OHD inversely correlates with serum ferritin (P = .013) and D-dimer levels (P = .027). Vitamin D-deficient COVID-19 patients had a greater prevalence of hypertension and cardiovascular diseases, raised
Additional Information Correspondence and Reprint Requests: José Luis Hernández, Department of Internal Medicine, Hospital Universitario Marqués de Valdecilla, University of Cantabria, Avda. Valdecilla s/n. 39008, Santander, Spain. E-mail: joseluis.hernandez@scsalud.es. Disclosure Summary: Dr. Hernández reports research grants form Amgen and fees for lectures or speaker bureau from Amgen, MSD, and Bayer, outside the submitted work. Dr. Crespo reports grants and research support from Gilead Sciences, AbbVie, MSD and Intercept Pharmaceuticals (all outside the submitted work) and speaker for Gilead Sciences and AbbVie. Drs. Martínez-Taboada, Nan, Fernández-Ayala, Hernández-Hernández, López-Hoyos, García-Unzueta, Muñoz-Cacho, Olmos, Cubillán, and Gutiérrez-Cuadra, have nothing to disclose. Data Availability: Some or all datasets generated during and/ or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
References
Alvarez-Rodriguez, Lopez-Hoyos, Garcia-Unzueta, Amado, Cacho et al., Age and low levels of circulating vitamin D are associated with impaired innate immune function, J Leukoc Biol
Ananthakrishnan, Cheng, Cai, Association between reduced plasma 25-hydroxy vitamin D and increased risk of cancer in patients with inflammatory bowel diseases, Clin Gastroenterol Hepatol
Armiñanzas, Arnaiz, Arnaiz, Ayarza, Baldeón et al., Financial Support: The Camargo Cohort Study was supported by grants from the Instituto de Salud Carlos III (PI18/00762), Ministerio de Economía y Competitividad, Spain, which included FEDER funds from the EU. Author Contributions
Baktash, Hosack, Patel, Vitamin D status and outcomes for hospitalised older patients with COVID-19
C ; González-Molero, Morcillo, Valdés, critically revised the manuscript. All authors discussed the results and con, Eur J Clin Nutr
D'avolio, Avataneo, Manca, 25-hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2, Nutrients
Dariya, Nagaraju, Understanding novel COVID-19: its impact on organ failure and risk assessment for diabetic and cancer patients, Cytokine Growth Factor Rev
Filippo, Formenti, Rovere-Querini, Hypocalcemia is highly prevalent and predicts hospitalization in patients with COVID-19, Endocrine
Gois, Ferreira, Olenski, Vitamin D and infectious diseases: simple bystander or contributing factor?, Nutrients
Grant, Lahore, Mcdonnell, Evidence that Vitamin D supplementation could reduce risk of influenza COVID-19 infections and deaths, Nutrients
Guan, Ni, Hu, China Medical Treatment Expert Group for Covid-19. Clinical characteristics of coronavirus disease 2019 in China, N Engl J Med
Haberman, Axelrad, Chen, Covid-19 in immunemediated inflammatory diseases-case series from New York, N Engl J Med
Hastie, Mackay, Ho, Vitamin D concentrations and COVID-19 infection in UK Biobank, Diabetes Metab Syndr
Hernández, Olmos, Pariente, Metabolic syndrome and bone metabolism: the Camargo Cohort study, Menopause
Hewison, An update on vitamin D and human immunity, Clin Endocrinol (Oxf)
Ilie, Stefanescu, Smith, The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality, Aging Clin Exp Res
Jeffery, Burke, Mura, 1,25-Dihydroxyvitamin D3 and IL-2 combine to inhibit T cell production of inflammatory cytokines and promote development of regulatory T cells expressing CTLA-4 and FoxP3, J Immunol
Joukar, Naghipour, Hassanipour, Association of serum levels of Vitamin D with blood pressure status in Northern Iranian population: the PERSIAN Guilan Cohort Study (PGCS)
Khafaie, Rahim, Cross-country comparison of case fatality rates of COVID-19/SARS-COV-2, Osong Public Health Res Perspect
Lips, Cashman, Lamberg-Allardt, Current vitamin D status in European and Middle East countries and strategies to prevent vitamin D deficiency: a position statement of the European Calcified Tissue Society, Eur J Endocrinol
Metlay, Waterer, Long, Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America, Am J Respir Crit Care Med
Mosekilde, Vitamin D and the elderly, Clin Endocrinol (Oxf)
Napoli, Elderkin, Kiel, Khosla, Managing fragility fractures during the COVID-19 pandemic, Nat Rev Endocrinol
Olmos, Hernández, Pariente, Martínez, González-Macías, Serum 25-Hydroxyvitamin D in obese Spanish adults: the Camargo Cohort Study, Obes Surg
Radujkovic, Hippchen, Tiwari-Heckler, Dreher, Boxberger, Vitamin D deficiency and outcome of COVID-19 patients, Nutrients
Schwalfenberg, Vitamin D and diabetes: improvement of glycemic control with vitamin D3 repletion, Can Fam Physician
Shi, Liu, Yao, Chronic vitamin D deficiency induces lung fibrosis through activation of the renin-angiotensin system, Sci Rep
Tay, Poh, Rénia, Macary, Ng, The trinity of COVID-19: immunity, inflammation and intervention, Nat Rev Immunol
Tramontana, Napoli, El-Hajj Fuleihan, Strollo, The D-side of COVID-19: musculoskeletal benefits of vitamin D and beyond, Endocrine
Van Der Wielen, Löwik, Van Den Berg, Serum vitamin D concentrations among elderly people in Europe, Lancet
Waldron, Ashby, Cornes, Vitamin D: a negative acute phase reactant, J Clin Pathol
Watkins, Lemonovich, Salata, An update on the association of vitamin D deficiency with common infectious diseases, Can J Physiol Pharmacol
Yu, Tsourdi, Clarke, Bauer, Drake, Osteoporosis management in the era of COVID-19, J Bone Miner Res
Zhang, Leung, Richers, Vitamin D inhibits monocyte/macrophage proinflammatory cytokine production by targeting MAPK phosphatase-1, J Immunol
Zhou, Yu, Du, Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet
Zhu, Rhee, Cheng, Cardiovascular complications in patients with COVID-19: consequences of viral toxicities and host immune response, Curr Cardiol Rep
DOI record:
{
"DOI": "10.1210/clinem/dgaa733",
"ISSN": [
"0021-972X",
"1945-7197"
],
"URL": "http://dx.doi.org/10.1210/clinem/dgaa733",
"abstract": "<jats:title>Abstract</jats:title>\n <jats:sec>\n <jats:title>Background</jats:title>\n <jats:p>The role of vitamin D status in COVID-19 patients is a matter of debate.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Objectives</jats:title>\n <jats:p>To assess serum 25-hydroxyvitamin D (25OHD) levels in hospitalized patients with COVID-19 and to analyze the possible influence of vitamin D status on disease severity.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Methods</jats:title>\n <jats:p>Retrospective case–control study of 216 COVID-19 patients and 197 population-based controls. Serum 25OHD levels were measured in both groups. The association of serum 25OHD levels with COVID-19 severity (admission to the intensive care unit, requirements for mechanical ventilation, or mortality) was also evaluated.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Results</jats:title>\n <jats:p>Of the 216 patients, 19 were on vitamin D supplements and were analyzed separately. In COVID-19 patients, mean ± standard deviation 25OHD levels were 13.8 ± 7.2 ng/mL, compared with 20.9 ± 7.4 ng/mL in controls (P &lt; .0001). 25OHD values were lower in men than in women. Vitamin D deficiency was found in 82.2% of COVID-19 cases and 47.2% of population-based controls (P &lt; .0001). 25OHD inversely correlates with serum ferritin (P = .013) and D-dimer levels (P = .027). Vitamin D-deficient COVID-19 patients had a greater prevalence of hypertension and cardiovascular diseases, raised serum ferritin and troponin levels, as well as a longer length of hospital stay than those with serum 25OHD levels ≥20 ng/mL. No causal relationship was found between vitamin D deficiency and COVID-19 severity as a combined endpoint or as its separate components.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Conclusions</jats:title>\n <jats:p>25OHD levels are lower in hospitalized COVID-19 patients than in population-based controls and these patients had a higher prevalence of deficiency. We did not find any relationship between vitamin D concentrations or vitamin deficiency and the severity of the disease.</jats:p>\n </jats:sec>",
"author": [
{
"ORCID": "http://orcid.org/0000-0002-6585-8847",
"affiliation": [
{
"name": "Department of Internal Medicine, Hospital Marqués de Valdecilla-IDIVAL, Santander, Spain"
},
{
"name": "University of Cantabria, Santander, Spain"
}
],
"authenticated-orcid": false,
"family": "Hernández",
"given": "José L",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Hospital Marqués de Valdecilla-IDIVAL, Santander, Spain"
},
{
"name": "University of Cantabria, Santander, Spain"
}
],
"family": "Nan",
"given": "Daniel",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Hospital Marqués de Valdecilla-IDIVAL, Santander, Spain"
}
],
"family": "Fernandez-Ayala",
"given": "Marta",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Clinical Biochemistry, Hospital Marqués de Valdecilla-IDIVAL, Santander, Spain"
}
],
"family": "García-Unzueta",
"given": "Mayte",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Intensive Care, Hospital Marqués de Valdecilla-IDIVAL, Santander, Spain"
}
],
"family": "Hernández-Hernández",
"given": "Miguel A",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Immunology, Hospital Marqués de Valdecilla-IDIVAL, Santander, Spain"
}
],
"family": "López-Hoyos",
"given": "Marcos",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Gerencia de Atención Primaria, Servicio Cántabro de Salud, Santander, Spain"
}
],
"family": "Muñoz-Cacho",
"given": "Pedro",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Hospital Marqués de Valdecilla-IDIVAL, Santander, Spain"
},
{
"name": "University of Cantabria, Santander, Spain"
}
],
"family": "Olmos",
"given": "José M",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Infectious Diseases, Hospital Marqués de Valdecilla-IDIVAL, Santander, Spain"
}
],
"family": "Gutiérrez-Cuadra",
"given": "Manuel",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Pneumology, Hospital Marqués de Valdecilla-IDIVAL, Santander, Spain"
}
],
"family": "Ruiz-Cubillán",
"given": "Juan J",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Gastroenterology, Hospital Marqués de Valdecilla-IDIVAL, Santander, Spain"
},
{
"name": "University of Cantabria, Santander, Spain"
}
],
"family": "Crespo",
"given": "Javier",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Rheumatology, Hospital Marqués de Valdecilla-IDIVAL, Santander, Spain"
},
{
"name": "University of Cantabria, Santander, Spain"
}
],
"family": "Martínez-Taboada",
"given": "Víctor M",
"sequence": "additional"
}
],
"container-title": "The Journal of Clinical Endocrinology & Metabolism",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2020,
11,
7
]
],
"date-time": "2020-11-07T10:21:28Z",
"timestamp": 1604744488000
},
"deposited": {
"date-parts": [
[
2021,
12,
21
]
],
"date-time": "2021-12-21T17:54:05Z",
"timestamp": 1640109245000
},
"funder": [
{
"DOI": "10.13039/501100004587",
"award": [
"PI18/00762"
],
"doi-asserted-by": "publisher",
"name": "Instituto de Salud Carlos III"
},
{
"DOI": "10.13039/501100003329",
"doi-asserted-by": "publisher",
"name": "Ministerio de Economía y Competitividad"
}
],
"indexed": {
"date-parts": [
[
2024,
4,
8
]
],
"date-time": "2024-04-08T12:36:12Z",
"timestamp": 1712579772204
},
"is-referenced-by-count": 182,
"issue": "3",
"issued": {
"date-parts": [
[
2020,
10,
27
]
]
},
"journal-issue": {
"issue": "3",
"published-online": {
"date-parts": [
[
2020,
10,
27
]
]
},
"published-print": {
"date-parts": [
[
2021,
3,
8
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://academic.oup.com/journals/pages/open_access/funder_policies/chorus/standard_publication_model",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2020,
10,
27
]
],
"date-time": "2020-10-27T00:00:00Z",
"timestamp": 1603756800000
}
}
],
"link": [
{
"URL": "https://academic.oup.com/jcem/article-pdf/106/3/e1343/41832650/dgaa733.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "syndication"
},
{
"URL": "https://academic.oup.com/jcem/article-pdf/106/3/e1343/41832650/dgaa733.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "80",
"original-title": [],
"page": "e1343-e1353",
"prefix": "10.1210",
"published": {
"date-parts": [
[
2020,
10,
27
]
]
},
"published-online": {
"date-parts": [
[
2020,
10,
27
]
]
},
"published-other": {
"date-parts": [
[
2021,
3,
1
]
]
},
"published-print": {
"date-parts": [
[
2021,
3,
8
]
]
},
"publisher": "The Endocrine Society",
"reference": [
{
"DOI": "10.1038/ejcn.2010.265",
"article-title": "Vitamin D deficiency in Spain: a population-based cohort study",
"author": "González-Molero",
"doi-asserted-by": "crossref",
"first-page": "321",
"issue": "3",
"journal-title": "Eur J Clin Nutr.",
"key": "2021122117335203600_CIT0001",
"volume": "65",
"year": "2011"
},
{
"DOI": "10.24171/j.phrp.2020.11.2.03",
"article-title": "Cross-country comparison of case fatality rates of COVID-19/SARS-COV-2",
"author": "Khafaie",
"doi-asserted-by": "crossref",
"first-page": "74",
"issue": "2",
"journal-title": "Osong Public Health Res Perspect.",
"key": "2021122117335203600_CIT0002",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1189/jlb.1011523",
"article-title": "Age and low levels of circulating vitamin D are associated with impaired innate immune function",
"author": "Alvarez-Rodriguez",
"doi-asserted-by": "crossref",
"first-page": "829",
"issue": "5",
"journal-title": "J Leukoc Biol.",
"key": "2021122117335203600_CIT0003",
"volume": "91",
"year": "2012"
},
{
"DOI": "10.3390/nu9070651",
"article-title": "Vitamin D and infectious diseases: simple bystander or contributing factor?",
"author": "Gois",
"doi-asserted-by": "crossref",
"first-page": "651",
"issue": "7",
"journal-title": "Nutrients",
"key": "2021122117335203600_CIT0004",
"volume": "9",
"year": "2017"
},
{
"DOI": "10.1139/cjpp-2014-0352",
"article-title": "An update on the association of vitamin D deficiency with common infectious diseases",
"author": "Watkins",
"doi-asserted-by": "crossref",
"first-page": "363",
"issue": "5",
"journal-title": "Can J Physiol Pharmacol.",
"key": "2021122117335203600_CIT0005",
"volume": "93",
"year": "2015"
},
{
"DOI": "10.1016/j.cgh.2013.10.011",
"article-title": "Association between reduced plasma 25-hydroxy vitamin D and increased risk of cancer in patients with inflammatory bowel diseases",
"author": "Ananthakrishnan",
"doi-asserted-by": "crossref",
"first-page": "821",
"issue": "5",
"journal-title": "Clin Gastroenterol Hepatol.",
"key": "2021122117335203600_CIT0006",
"volume": "12",
"year": "2014"
},
{
"article-title": "Vitamin D and diabetes: improvement of glycemic control with vitamin D3 repletion",
"author": "Schwalfenberg",
"first-page": "864",
"issue": "6",
"journal-title": "Can Fam Physician.",
"key": "2021122117335203600_CIT0007",
"volume": "54",
"year": "2008"
},
{
"DOI": "10.2147/IJGM.S244472",
"article-title": "Association of serum levels of Vitamin D with blood pressure status in Northern Iranian population: the PERSIAN Guilan Cohort Study (PGCS)",
"author": "Joukar",
"doi-asserted-by": "crossref",
"first-page": "99",
"journal-title": "Int J Gen Med.",
"key": "2021122117335203600_CIT0008",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.1111/j.1365-2265.2005.02226.x",
"article-title": "Vitamin D and the elderly",
"author": "Mosekilde",
"doi-asserted-by": "crossref",
"first-page": "265",
"issue": "3",
"journal-title": "Clin Endocrinol (Oxf).",
"key": "2021122117335203600_CIT0009",
"volume": "62",
"year": "2005"
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"article-title": "Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study",
"author": "Zhou",
"doi-asserted-by": "crossref",
"first-page": "1054",
"issue": "10229",
"journal-title": "Lancet.",
"key": "2021122117335203600_CIT0010",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1016/j.cytogfr.2020.05.001",
"article-title": "Understanding novel COVID-19: its impact on organ failure and risk assessment for diabetic and cancer patients",
"author": "Dariya",
"doi-asserted-by": "crossref",
"first-page": "43",
"journal-title": "Cytokine Growth Factor Rev.",
"key": "2021122117335203600_CIT0011",
"volume": "53",
"year": "2020"
},
{
"DOI": "10.4049/jimmunol.1102412",
"article-title": "Vitamin D inhibits monocyte/macrophage proinflammatory cytokine production by targeting MAPK phosphatase-1",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "2127",
"issue": "5",
"journal-title": "J Immunol.",
"key": "2021122117335203600_CIT0012",
"volume": "188",
"year": "2012"
},
{
"DOI": "10.1038/s41598-017-03474-6",
"article-title": "Chronic vitamin D deficiency induces lung fibrosis through activation of the renin-angiotensin system",
"author": "Shi",
"doi-asserted-by": "crossref",
"first-page": "3312",
"issue": "1",
"journal-title": "Sci Rep.",
"key": "2021122117335203600_CIT0013",
"volume": "7",
"year": "2017"
},
{
"DOI": "10.1097/gme.0b013e3181e39a15",
"article-title": "Metabolic syndrome and bone metabolism: the Camargo Cohort study",
"author": "Hernández",
"doi-asserted-by": "crossref",
"first-page": "955",
"issue": "5",
"journal-title": "Menopause.",
"key": "2021122117335203600_CIT0014",
"volume": "17",
"year": "2010"
},
{
"DOI": "10.1007/s11695-018-3430-6",
"article-title": "Serum 25-Hydroxyvitamin D in obese Spanish adults: the Camargo Cohort Study",
"author": "Olmos",
"doi-asserted-by": "crossref",
"first-page": "3862",
"issue": "12",
"journal-title": "Obes Surg.",
"key": "2021122117335203600_CIT0015",
"volume": "28",
"year": "2018"
},
{
"DOI": "10.1164/rccm.201908-1581ST",
"article-title": "Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America",
"author": "Metlay",
"doi-asserted-by": "crossref",
"first-page": "e45",
"issue": "7",
"journal-title": "Am J Respir Crit Care Med.",
"key": "2021122117335203600_CIT0016",
"volume": "200",
"year": "2019"
},
{
"author": "Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias.",
"key": "2021122117335203600_CIT0017"
},
{
"DOI": "10.1530/EJE-18-0736",
"article-title": "Current vitamin D status in European and Middle East countries and strategies to prevent vitamin D deficiency: a position statement of the European Calcified Tissue Society",
"author": "Lips",
"doi-asserted-by": "crossref",
"first-page": "P23",
"issue": "4",
"journal-title": "Eur J Endocrinol.",
"key": "2021122117335203600_CIT0018",
"volume": "180",
"year": "2019"
},
{
"DOI": "10.1111/j.1365-2265.2011.04261.x",
"article-title": "An update on vitamin D and human immunity",
"author": "Hewison",
"doi-asserted-by": "crossref",
"first-page": "315",
"issue": "3",
"journal-title": "Clin Endocrinol (Oxf).",
"key": "2021122117335203600_CIT0019",
"volume": "76",
"year": "2012"
},
{
"DOI": "10.3390/nu12040988",
"article-title": "Evidence that Vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths",
"author": "Grant",
"doi-asserted-by": "crossref",
"first-page": "988",
"issue": "4",
"journal-title": "Nutrients.",
"key": "2021122117335203600_CIT0020",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2002032",
"article-title": "Clinical characteristics of coronavirus disease 2019 in China",
"author": "Guan",
"doi-asserted-by": "crossref",
"first-page": "1708",
"issue": "18",
"journal-title": "N Engl J Med.",
"key": "2021122117335203600_CIT0021",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(95)91266-5",
"article-title": "Serum vitamin D concentrations among elderly people in Europe",
"author": "van der Wielen",
"doi-asserted-by": "crossref",
"first-page": "207",
"issue": "8969",
"journal-title": "Lancet.",
"key": "2021122117335203600_CIT0022",
"volume": "346",
"year": "1995"
},
{
"DOI": "10.1007/s40520-020-01570-8",
"article-title": "The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality",
"author": "Ilie",
"doi-asserted-by": "crossref",
"first-page": "1195",
"issue": "7",
"journal-title": "Aging Clin Exp Res.",
"key": "2021122117335203600_CIT0023",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.1007/s11886-020-01292-3",
"article-title": "Cardiovascular complications in patients with COVID-19: consequences of viral toxicities and host immune response",
"author": "Zhu",
"doi-asserted-by": "crossref",
"first-page": "32",
"issue": "5",
"journal-title": "Curr Cardiol Rep.",
"key": "2021122117335203600_CIT0024",
"volume": "22",
"year": "2020"
},
{
"DOI": "10.1038/s41577-020-0311-8",
"article-title": "The trinity of COVID-19: immunity, inflammation and intervention",
"author": "Tay",
"doi-asserted-by": "crossref",
"first-page": "363",
"issue": "6",
"journal-title": "Nat Rev Immunol.",
"key": "2021122117335203600_CIT0025",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1007/s12020-020-02407-0",
"article-title": "The D-side of COVID-19: musculoskeletal benefits of vitamin D and beyond",
"author": "Tramontana",
"doi-asserted-by": "crossref",
"first-page": "237",
"issue": "2",
"journal-title": "Endocrine.",
"key": "2021122117335203600_CIT0026",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.4049/jimmunol.0803217",
"article-title": "1,25-Dihydroxyvitamin D3 and IL-2 combine to inhibit T cell production of inflammatory cytokines and promote development of regulatory T cells expressing CTLA-4 and FoxP3",
"author": "Jeffery",
"doi-asserted-by": "crossref",
"first-page": "5458",
"issue": "9",
"journal-title": "J Immunol.",
"key": "2021122117335203600_CIT0027",
"volume": "183",
"year": "2009"
},
{
"DOI": "10.1016/j.dsx.2020.04.050",
"article-title": "Vitamin D concentrations and COVID-19 infection in UK Biobank",
"author": "Hastie",
"doi-asserted-by": "crossref",
"first-page": "561",
"issue": "4",
"journal-title": "Diabetes Metab Syndr.",
"key": "2021122117335203600_CIT0028",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.3390/nu12051359",
"article-title": "25-hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2",
"author": "D’Avolio",
"doi-asserted-by": "crossref",
"first-page": "1359",
"issue": "5",
"journal-title": "Nutrients.",
"key": "2021122117335203600_CIT0029",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1136/jclinpath-2012-201301",
"article-title": "Vitamin D: a negative acute phase reactant",
"author": "Waldron",
"doi-asserted-by": "crossref",
"first-page": "620",
"issue": "7",
"journal-title": "J Clin Pathol.",
"key": "2021122117335203600_CIT0030",
"volume": "66",
"year": "2013"
},
{
"DOI": "10.1136/postgradmedj-2020-138712",
"article-title": "Vitamin D status and outcomes for hospitalised older patients with COVID-19",
"author": "Baktash",
"doi-asserted-by": "crossref",
"journal-title": "Postgrad Med J.",
"key": "2021122117335203600_CIT0031",
"year": "2020"
},
{
"DOI": "10.3390/nu12092757",
"article-title": "Vitamin D deficiency and outcome of COVID-19 patients",
"author": "Radujkovic",
"doi-asserted-by": "crossref",
"first-page": "E2757",
"issue": "9",
"journal-title": "Nutrients.",
"key": "2021122117335203600_CIT0032",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1056/NEJMc2009567",
"article-title": "Covid-19 in immune-mediated inflammatory diseases–case series from New York.",
"author": "Haberman",
"doi-asserted-by": "crossref",
"first-page": "85",
"issue": "(1)",
"journal-title": "N Engl J Med.",
"key": "2021122117335203600_CIT0033",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.1007/s12020-020-02383-5",
"article-title": "Hypocalcemia is highly prevalent and predicts hospitalization in patients with COVID-19",
"author": "Di Filippo",
"doi-asserted-by": "crossref",
"first-page": "475",
"issue": "3",
"journal-title": "Endocrine.",
"key": "2021122117335203600_CIT0034",
"volume": "68",
"year": "2020"
},
{
"DOI": "10.1002/jbmr.4049",
"article-title": "Osteoporosis management in the era of COVID-19",
"author": "Yu",
"doi-asserted-by": "crossref",
"first-page": "1009",
"issue": "6",
"journal-title": "J Bone Miner Res.",
"key": "2021122117335203600_CIT0035",
"volume": "35",
"year": "2020"
},
{
"DOI": "10.1038/s41574-020-0379-z",
"article-title": "Managing fragility fractures during the COVID-19 pandemic",
"author": "Napoli",
"doi-asserted-by": "crossref",
"first-page": "467",
"issue": "9",
"journal-title": "Nat Rev Endocrinol.",
"key": "2021122117335203600_CIT0036",
"volume": "16",
"year": "2020"
}
],
"reference-count": 36,
"references-count": 36,
"relation": {},
"resource": {
"primary": {
"URL": "https://academic.oup.com/jcem/article/106/3/e1343/5934827"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Biochemistry (medical)",
"Clinical Biochemistry",
"Endocrinology",
"Biochemistry",
"Endocrinology, Diabetes and Metabolism"
],
"subtitle": [],
"title": "Vitamin D Status in Hospitalized Patients with SARS-CoV-2 Infection",
"type": "journal-article",
"volume": "106"
}
