Metabolic Healthy Obesity, Vitamin D Status, and Risk of COVID-19
et al., Aging and Disease, doi:10.14336/AD.2020.1108, Jan 2021
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
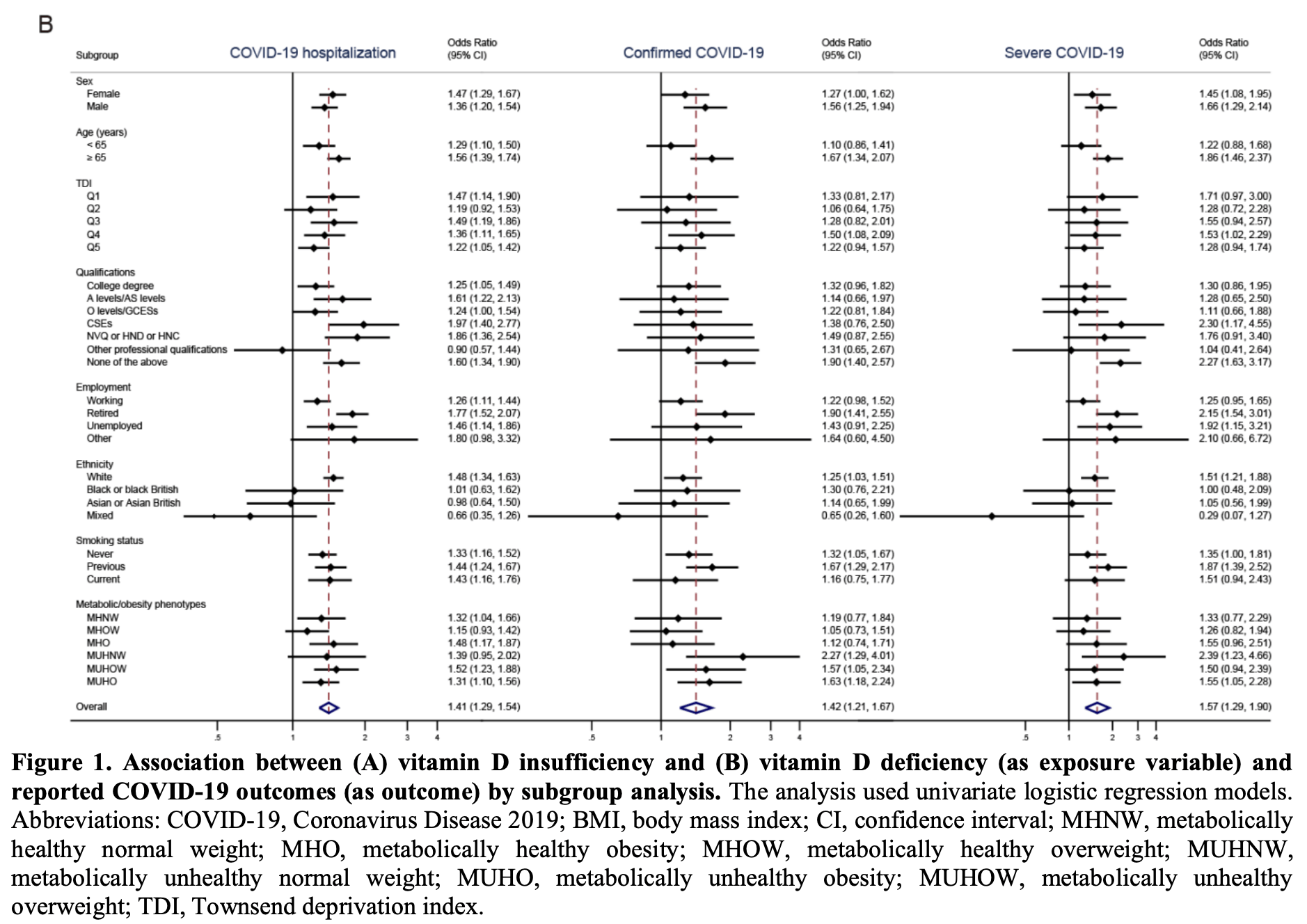
UK Biobank retrospective 353,299 patients showing that vitamin D insufficiency and deficiency are associated with increased COVID-19 risk. This study also analyzes metabolic/obesity phenotypes and the combination with vitamin D status.
Note that the outcome definitions are unusual - COVID-19 hospitalization includes patients that tested negative, and severe COVID-19 was defined as hospitalized patients that tested positive.
This is the 39th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
Standard of Care (SOC) for COVID-19 in the study country,
the United Kingdom, is very poor with very low average efficacy for approved treatments1.
The United Kingdom focused on expensive high-profit treatments, approving only one low-cost early treatment, which required a prescription and had limited adoption. The high-cost prescription treatment strategy reduces the probability of early treatment due to access and cost barriers, and eliminates complementary and synergistic benefits seen with many low-cost treatments.
|
risk of hospitalization, 36.2% lower, RR 0.64, p < 0.001, NNT 932, inverted to make RR<1 favor high D levels, odds ratio converted to relative risk, >25nmol/L.
|
|
risk of case, 29.5% lower, RR 0.71, p < 0.001, NNT 823, inverted to make RR<1 favor high D levels, odds ratio converted to relative risk, >25nmol/L.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Li et al., 11 Jan 2021, retrospective, population-based cohort, United Kingdom, peer-reviewed, 6 authors.
Metabolic Healthy Obesity, Vitamin D Status, and Risk of COVID-19
Aging and disease, doi:10.14336/ad.2020.1108
Aging and obesity-related conditions seem to worsen the effect of Coronavirus Disease 2019 (COVID-19). This study assessed the possible roles of metabolic/obesity phenotypes and vitamin D status in increasing the greater severity of COVID-19. We studied 353,299 UK Biobank participants from England with a mean age of 67.7 years. Metabolic/obesity phenotypes were defined as a combination of metabolic components (hypertension, high cholesterol, and diabetes) and obesity. Multivariate logistic regression analysis was performed to test whether the addition of metabolic disorders and vitamin D insufficiency increased obesity associations with COVID-19 hospitalization, confirmed COVID-19, and severe COVID-19. Metabolically unhealthy obesity (MUHO) represented 12.3% of the total analytic samples, and 21.5%, 18.5%, and 19.8% of the included subpopulations with COVID-19 hospitalization, confirmed COVID-19, and severe COVID-19, respectively. Vitamin D insufficiency phenotypes represented 53.5% of the total analytic samples, and 59.5%, 61.7%, and 61.5% of the included subpopulations with COVID-19 hospitalization, confirmed COVID-19, and severe COVID-19, respectively. In multivariate logistic regression, MUHO and vitamin D insufficiency and their combination were significantly associated with COVID-19 illness severity (odds ratio [OR] for COVID-19 hospitalization = 2.33, 95% confidence interval [CI], 2.02-2.70; OR for confirmed COVID-19 = 2.06, 95% CI, 1.58-2.70; OR for severe COVID-19 = 2.06, 95% CI, 1.47-2.87). Elderly men were prone to have a higher risk of COVID-19 than women. Our findings showed that MUHO and vitamin D insufficiency are associated with a significantly increased risk of COVID-19 severity, especially for adults 65 years and older. Susceptible individuals should be aware of their conditions and avoid contact with new coronavirus.
Conflicts of interest The authors declare that they have no competing interests.
Supplementary Materials The Supplemenantry data can be found online at: www.aginganddisease.org/EN/10.14336/AD.2020.1108.
References
Alghamdi, Hussain, Almalki, Alghamdi, Alghamdi et al., The pattern of Middle East respiratory syndrome coronavirus in Saudi Arabia: a descriptive epidemiological analysis of data from the Saudi Ministry of Health, Int J Gen Med
Apicella, Campopiano, Mantuano, Mazoni, Coppelli et al., COVID-19 in people with diabetes: understanding the reasons for worse outcomes, Lancet Diabetes Endocrinol
Bornstein, Dalan, Hopkins, Mingrone, Boehm, Endocrine and metabolic link to coronavirus infection, Nat Rev Endocrinol
Bornstein, Rubino, Khunti, Mingrone, Hopkins et al., Practical recommendations for the management of diabetes in patients with COVID-19, Lancet Diabetes Endocrinol
Bourgonje, Abdulle, Timens, Hillebrands, Navis et al., Angiotensinconverting enzyme 2 (ACE2), SARS-CoV-2 and the pathophysiology of coronavirus disease 2019 (COVID-19), J Pathol
Cai, Sex difference and smoking predisposition in patients with COVID-19, Lancet Respir Med
Catapano, Graham, Backer, Wiklund, Chapman et al., 2016 ESC/EAS Guidelines for the Management of Dyslipidaemias, Eur Heart J
Channappanavar, Fett, Mack, Eyck, Meyerholz et al., Sex-Based Differences in Susceptibility to Severe Acute Respiratory Syndrome Coronavirus Infection, J Immunol
Docherty, Harrison, Green, Hardwick, Pius et al., Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study, BMJ
Eckel, Li, Kuxhaus, Stefan, Hu et al., Transition from metabolic healthy to unhealthy phenotypes and association with cardiovascular disease risk across BMI categories in 90 257 women (the Nurses' Health Study): 30 year followup from a prospective cohort study, Lancet Diabetes Endocrinol
Galbadage, Peterson, Awada, Buck, Ramirez et al., Systematic Review and Meta-Analysis of Sex-Specific COVID-19 Clinical Outcomes, Front Med
Gilbert, Arum, Smith, Vitamin D deficiency and chronic lung disease, Can Respir J
Guan, Liang, Zhao, Liang, Chen et al., Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis, Eur Respir J
Hastie, Mackay, Ho, Celis-Morales, Katikireddi et al., Vitamin D concentrations and COVID-19 infection in UK Biobank, Diabetes Metab Syndr
Hauser, Counotte, Margossian, Konstantinoudis, Low et al., Estimation of SARS-CoV-2 mortality during the early stages of an epidemic: A modeling study in Hubei, China, and six regions in Europe, PLoS Med
Jeong, Yoon, Lee, Diabetes and COVID-19: Global and regional perspectives, Diabetes Res Clin Pract
Jin, Bai, He, Wu, Liu et al., Gender Differences in Patients With COVID-19: Focus on Severity and Mortality, Front Public Health
Karlberg, Chong, Lai, Do men have a higher case fatality rate of severe acute respiratory syndrome than women do?, Am J Epidemiol
Liu, Chen, Liu, Nie, Lu, Comorbid Chronic Diseases are Strongly Correlated with Disease Severity among COVID-19 Patients: A Systematic Review and Meta-Analysis, Aging Dis
Liu, Dong, Yin, Yao, Shen et al., Meta-analysis of vitamin D and lung function in patients with asthma, Respir Res
Martineau, Jolliffe, Hooper, Greenberg, Aloia et al., Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data, BMJ
Mitchell, Vitamin-D and COVID-19: do deficient risk a poorer outcome?, Lancet Diabetes Endocrinol
Ng, Fleming, Robinson, Thomson, Graetz et al., Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study, Lancet
Ollier, Sprosen, Peakman, UK Biobank: from concept to reality, Pharmacogenomics
Petersen, Bressem, Albrecht, Thiess, Vahldiek et al., The role of visceral adiposity in the severity of COVID-19: Highlights a unicenter cross-sectional pilot study in Germany, Metabolism
Remuzzi, Remuzzi, COVID-19 and Italy: what next?, Lancet
Sharma, Volgman, Michos, Sex Differences in Mortality From COVID-19 Pandemic: Are Men Vulnerable and Women Protected?, JACC Case Rep
Stefan, Birkenfeld, Schulze, Ludwig, Obesity and impaired metabolic health in patients with COVID-19, Nat Rev Endocrinol
Stefan, Causes, consequences, and treatment of metabolically unhealthy fat distribution, Lancet Diabetes Endocrinol
Stefan, Haring, Schulze, Metabolically healthy obesity: the low-hanging fruit in obesity treatment?, Lancet Diabetes Endocrinol
Vignera, Cannarella, Condorelli, Torre, Aversa et al., Sex-Specific SARS-CoV-2 Mortality: Among Hormone-Modulated ACE2 Expression, Risk of Venous Thromboembolism and Hypovitaminosis D, Int J Mol Sci
Williamson, Walker, Bhaskaran, Bacon, Bates et al., Factors associated with COVID-19-related death using OpenSAFELY, Nature
Wimalawansa, Associations of vitamin D with insulin resistance, obesity, type 2 diabetes, and metabolic syndrome, J Steroid Biochem Mol Biol
Zheng, Peng, Xu, Zhao, Liu et al., Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis, J Infect
Zhu, Hasegawa, Ma, Fujiogi, Camargo et al., Association of asthma and its genetic predisposition with the risk of severe COVID-19, J Allergy Clin Immunol
DOI record:
{
"DOI": "10.14336/ad.2020.1108",
"ISSN": [
"2152-5250"
],
"URL": "http://dx.doi.org/10.14336/AD.2020.1108",
"author": [
{
"affiliation": [],
"family": "Li",
"given": "Shu",
"sequence": "first"
},
{
"affiliation": [],
"family": "Cao",
"given": "Zhi",
"sequence": "first"
},
{
"affiliation": [],
"family": "Yang",
"given": "Hongxi",
"sequence": "first"
},
{
"affiliation": [],
"family": "Zhang",
"given": "Yuan",
"sequence": "first"
},
{
"affiliation": [],
"family": "Xu",
"given": "Fusheng",
"sequence": "first"
},
{
"affiliation": [],
"family": "Wang",
"given": "Yaogang",
"sequence": "first"
}
],
"container-title": "Aging and disease",
"container-title-short": "Aging and disease",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
1,
13
]
],
"date-time": "2021-01-13T02:25:40Z",
"timestamp": 1610504740000
},
"deposited": {
"date-parts": [
[
2021,
7,
29
]
],
"date-time": "2021-07-29T02:12:35Z",
"timestamp": 1627524755000
},
"indexed": {
"date-parts": [
[
2024,
3,
30
]
],
"date-time": "2024-03-30T16:30:26Z",
"timestamp": 1711816226199
},
"is-referenced-by-count": 20,
"issue": "1",
"issued": {
"date-parts": [
[
2021
]
]
},
"journal-issue": {
"issue": "1",
"published-print": {
"date-parts": [
[
2021
]
]
}
},
"language": "en",
"link": [
{
"URL": "http://www.aginganddisease.org/fileup/2152-5250/PDF/ad-0-0-0-2011130737-1.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "5462",
"original-title": [],
"page": "61",
"prefix": "10.14336",
"published": {
"date-parts": [
[
2021
]
]
},
"published-print": {
"date-parts": [
[
2021
]
]
},
"publisher": "Aging and Disease",
"reference": [
{
"DOI": "10.1371/journal.pmed.1003189",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-1",
"unstructured": "Hauser A, Counotte MJ, Margossian CC, Konstantinoudis G, Low N, Althaus CL, et al. (2020). Estimation of SARS-CoV-2 mortality during the early stages of an epidemic: A modeling study in Hubei, China, and six regions in Europe. PLoS Med, 17:e1003189."
},
{
"DOI": "10.1038/s41586-020-2521-4",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-2",
"unstructured": "Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, et al. (2020). Factors associated with COVID-19-related death using OpenSAFELY. Nature, 584:430-436."
},
{
"DOI": "10.14336/AD.2020.0502",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-3",
"unstructured": "Liu H, Chen S, Liu M, Nie H, Lu H (2020). Comorbid Chronic Diseases are Strongly Correlated with Disease Severity among COVID-19 Patients: A Systematic Review and Meta-Analysis. Aging Dis, 11:668-678."
},
{
"DOI": "10.1038/s41574-020-0364-6",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-4",
"unstructured": "Stefan N, Birkenfeld AL, Schulze MB, Ludwig DS (2020). Obesity and impaired metabolic health in patients with COVID-19. Nat Rev Endocrinol, 16:341-342."
},
{
"DOI": "10.1016/S2213-8587(20)30152-2",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-5",
"unstructured": "Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL, et al. (2020). Practical recommendations for the management of diabetes in patients with COVID-19. Lancet Diabetes Endocrinol, 8:546-550."
},
{
"DOI": "10.1016/S0140-6736(20)30627-9",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-6",
"unstructured": "Remuzzi A, Remuzzi G (2020). COVID-19 and Italy: what next? Lancet, 395:1225-1228."
},
{
"DOI": "10.1016/S2213-8587(20)30183-2",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-7",
"unstructured": "Mitchell F (2020). Vitamin-D and COVID-19: do deficient risk a poorer outcome? Lancet Diabetes Endocrinol, 8:570."
},
{
"DOI": "10.1155/2009/829130",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-8",
"unstructured": "Gilbert CR, Arum SM, Smith CM (2009). Vitamin D deficiency and chronic lung disease. Can Respir J, 16:75-80."
},
{
"DOI": "10.1186/s12931-019-1072-4",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-9",
"unstructured": "Liu J, Dong YQ, Yin J, Yao J, Shen J, Sheng GJ, et al. (2019). Meta-analysis of vitamin D and lung function in patients with asthma. Respir Res, 20:161."
},
{
"DOI": "10.1183/13993003.01227-2020",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-10",
"unstructured": "Guan WJ, Liang WH, Zhao Y, Liang HR, Chen ZS, Li YM, et al. (2020). Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J, 55."
},
{
"DOI": "10.1016/j.diabres.2020.108303",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-11",
"unstructured": "Jeong IK, Yoon KH, Lee MK (2020). Diabetes and COVID-19: Global and regional perspectives. Diabetes Res Clin Pract, 166:108303."
},
{
"DOI": "10.2217/14622416.6.6.639",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-12",
"unstructured": "Ollier W, Sprosen T, Peakman T (2005). UK Biobank: from concept to reality. Pharmacogenomics, 6:639-646."
},
{
"DOI": "10.1016/S2213-8587(18)30137-2",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-13",
"unstructured": "Eckel N, Li Y, Kuxhaus O, Stefan N, Hu FB, Schulze MB (2018). Transition from metabolic healthy to unhealthy phenotypes and association with cardiovascular disease risk across BMI categories in 90 257 women (the Nurses' Health Study): 30 year follow-up from a prospective cohort study. Lancet Diabetes Endocrinol, 6:714-724."
},
{
"DOI": "10.1016/j.jaci.2020.06.001",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-14",
"unstructured": "Zhu Z, Hasegawa K, Ma B, Fujiogi M, Camargo CAJr, Liang L (2020). Association of asthma and its genetic predisposition with the risk of severe COVID-19. J Allergy Clin Immunol, 146:327-329 e324."
},
{
"DOI": "10.1016/S2213-8587(17)30292-9",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-15",
"unstructured": "Stefan N, Haring HU, Schulze MB (2018). Metabolically healthy obesity: the low-hanging fruit in obesity treatment? Lancet Diabetes Endocrinol, 6:249-258."
},
{
"DOI": "10.1016/S2213-8587(20)30110-8",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-16",
"unstructured": "Stefan N (2020). Causes, consequences, and treatment of metabolically unhealthy fat distribution. Lancet Diabetes Endocrinol, 8:616-627."
},
{
"DOI": "10.1093/eurheartj/ehw272",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-17",
"unstructured": "Catapano AL, Graham I, De Backer G, Wiklund O, Chapman MJ, Drexel H, et al. (2016). 2016 ESC/EAS Guidelines for the Management of Dyslipidaemias. Eur Heart J, 37:2999-3058."
},
{
"DOI": "10.1038/s41574-020-0353-9",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-18",
"unstructured": "Bornstein SR, Dalan R, Hopkins D, Mingrone G, Boehm BO (2020). Endocrine and metabolic link to coronavirus infection. Nat Rev Endocrinol, 16:297-298."
},
{
"DOI": "10.1016/j.metabol.2020.154317",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-19",
"unstructured": "Petersen A, Bressem K, Albrecht J, Thiess HM, Vahldiek J, Hamm B, et al. (2020). The role of visceral adiposity in the severity of COVID-19: Highlights from a unicenter cross-sectional pilot study in Germany. Metabolism, 110:154317."
},
{
"DOI": "10.1016/S2213-8587(20)30238-2",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-20",
"unstructured": "Apicella M, Campopiano MC, Mantuano M, Mazoni L, Coppelli A, Del Prato S (2020). COVID-19 in people with diabetes: understanding the reasons for worse outcomes. Lancet Diabetes Endocrinol, 8:782-792."
},
{
"DOI": "10.2337/dbi19-0023",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-21",
"unstructured": "Mauvais-Jarvis F (2020). Aging, Male Sex, Obesity, and Metabolic Inflammation Create the Perfect Storm for COVID-19. Diabetes, 69:1857-1863."
},
{
"key": "key-10.14336/AD.2020.1108-22",
"unstructured": "Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. (2014). Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet, 384:766-781."
},
{
"DOI": "10.1136/bmj.i6583",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-23",
"unstructured": "Martineau AR, Jolliffe DA, Hooper RL, Greenberg L, Aloia JF, Bergman P, et al. (2017). Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. BMJ, 356:i6583."
},
{
"DOI": "10.1016/j.dsx.2020.04.050",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-24",
"unstructured": "Hastie CE, Mackay DF, Ho F, Celis-Morales CA, Katikireddi SV, Niedzwiedz CL, et al. (2020). Vitamin D concentrations and COVID-19 infection in UK Biobank. Diabetes Metab Syndr, 14:561-565."
},
{
"DOI": "10.1016/j.jsbmb.2016.09.017",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-25",
"unstructured": "Wimalawansa SJ (2018). Associations of vitamin D with insulin resistance, obesity, type 2 diabetes, and metabolic syndrome. J Steroid Biochem Mol Biol, 175:177-189."
},
{
"DOI": "10.1016/j.jinf.2020.04.021",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-26",
"unstructured": "Zheng Z, Peng F, Xu B, Zhao J, Liu H, Peng J, et al. (2020). Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis. J Infect, 81:e16-e25."
},
{
"DOI": "10.3389/fpubh.2020.00152",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-27",
"unstructured": "Jin JM, Bai P, He W, Wu F, Liu XF, Han DM, et al. (2020). Gender Differences in Patients With COVID-19: Focus on Severity and Mortality. Front Public Health, 8:152."
},
{
"DOI": "10.3389/fmed.2020.00348",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-28",
"unstructured": "Galbadage T, Peterson BM, Awada J, Buck AS, Ramirez DA, Wilson J, et al. (2020). Systematic Review and Meta-Analysis of Sex-Specific COVID-19 Clinical Outcomes. Front Med (Lausanne), 7:348."
},
{
"DOI": "10.1136/bmj.m1985",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-29",
"unstructured": "Docherty AB, Harrison EM, Green CA, Hardwick HE, Pius R, Norman L, et al. (2020). Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ, 369:m1985."
},
{
"DOI": "10.4049/jimmunol.1601896",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-30",
"unstructured": "Channappanavar R, Fett C, Mack M, Ten Eyck PP, Meyerholz DK, Perlman S (2017). Sex-Based Differences in Susceptibility to Severe Acute Respiratory Syndrome Coronavirus Infection. J Immunol, 198:4046-4053."
},
{
"DOI": "10.1093/aje/kwh056",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-31",
"unstructured": "Karlberg J, Chong DS, Lai WY (2004). Do men have a higher case fatality rate of severe acute respiratory syndrome than women do? Am J Epidemiol, 159:229-231."
},
{
"DOI": "10.2147/IJGM.S67061",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-32",
"unstructured": "Alghamdi IG, HussainII, Almalki SS, Alghamdi MS, Alghamdi MM, El-Sheemy MA (2014). The pattern of Middle East respiratory syndrome coronavirus in Saudi Arabia: a descriptive epidemiological analysis of data from the Saudi Ministry of Health. Int J Gen Med, 7:417-423."
},
{
"DOI": "10.3390/ijms21082948",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-33",
"unstructured": "La Vignera S, Cannarella R, Condorelli RA, Torre F, Aversa A, Calogero AE (2020). Sex-Specific SARS-CoV-2 Mortality: Among Hormone-Modulated ACE2 Expression, Risk of Venous Thromboembolism and Hypovitaminosis D. Int J Mol Sci, 21."
},
{
"DOI": "10.1002/path.5471",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-34",
"unstructured": "Bourgonje AR, Abdulle AE, Timens W, Hillebrands JL, Navis GJ, Gordijn SJ, et al. (2020). Angiotensin-converting enzyme 2 (ACE2), SARS-CoV-2 and the pathophysiology of coronavirus disease 2019 (COVID-19). J Pathol, 251:228-248."
},
{
"DOI": "10.1016/S2213-2600(20)30117-X",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-35",
"unstructured": "Cai H (2020). Sex difference and smoking predisposition in patients with COVID-19. Lancet Respir Med, 8:e20."
},
{
"DOI": "10.1016/j.jaccas.2020.04.027",
"doi-asserted-by": "crossref",
"key": "key-10.14336/AD.2020.1108-36",
"unstructured": "Sharma G, Volgman AS, Michos ED (2020). Sex Differences in Mortality From COVID-19 Pandemic: Are Men Vulnerable and Women Protected? JACC Case Rep, 2:1407-1410."
}
],
"reference-count": 36,
"references-count": 36,
"relation": {},
"resource": {
"primary": {
"URL": "http://www.aginganddisease.org/EN/10.14336/AD.2020.1108"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Cell Biology",
"Neurology (clinical)",
"Geriatrics and Gerontology",
"Pathology and Forensic Medicine"
],
"subtitle": [],
"title": "Metabolic Healthy Obesity, Vitamin D Status, and Risk of COVID-19",
"type": "journal-article",
"volume": "12"
}
