Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers
et al., Nature, doi:10.1038/s41598-020-77093-z, Nov 2020
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Prospective study of 91 asymptomatic and 63 ICU patients showing significantly higher vitamin D deficiency in the ICU patients (97% vs. 33%).
This is the 28th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
risk of death, 85.2% lower, RR 0.15, p = 0.001, high D levels 2 of 64 (3.1%), low D levels 19 of 90 (21.1%), NNT 5.6, >20ng/mL.
|
|
risk of ICU admission, 95.4% lower, RR 0.05, p < 0.001, high D levels 2 of 64 (3.1%), low D levels 61 of 90 (67.8%), NNT 1.5, >20ng/mL.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Jain et al., 19 Nov 2020, prospective, India, peer-reviewed, 6 authors.
Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers
Scientific Reports, doi:10.1038/s41598-020-77093-z
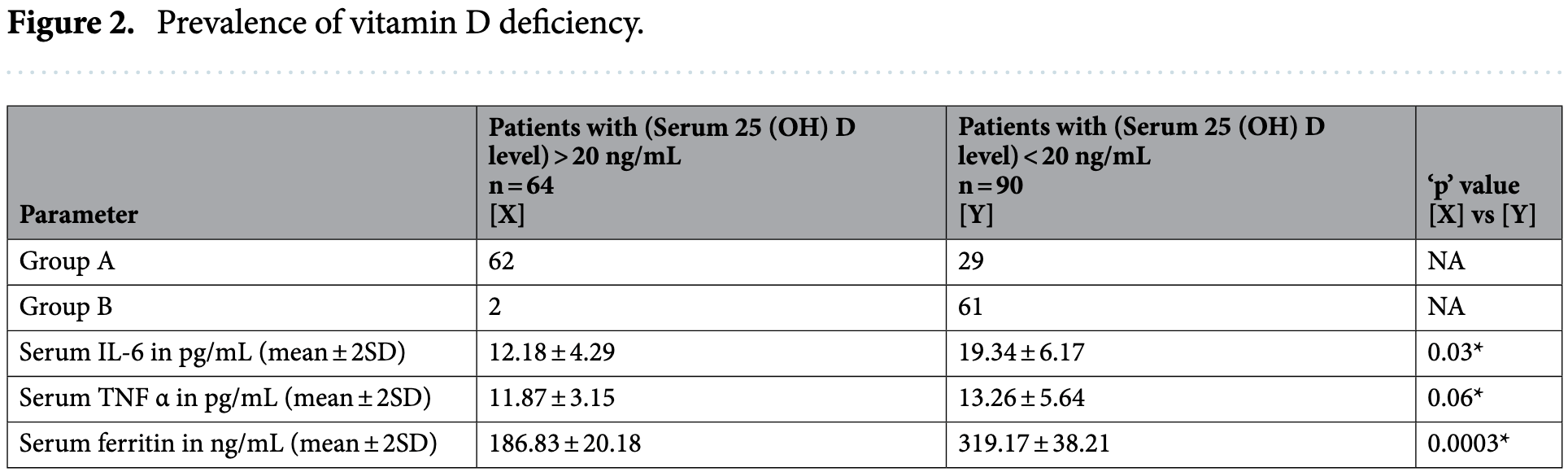
COVID-19 is characterized by marked variability in clinical severity. Vitamin D had recently been reviewed as one of the factors that may affect the severity in COVID-19. The objective of current study is to analyze the vitamin D level in COVID-19 patients and its impact on the disease severity. After approval from Ethics Committee, M.L.B Medical College the current study was undertaken as continuous prospective observational study of 6 weeks. Participants were COVID-19 patients of age group 30-60 years admitted during the study period of 6 weeks. Study included either asymptomatic COVID-19 patients (Group A) or severely ill patients requiring ICU admission (Group B). Serum concentration of 25 (OH)D, were measured along with serum IL-6; TNFα and serum ferritin. Standard statistical analysis was performed to analyze the differences. Current Study enrolled 154 patients, 91 in Group A and 63 patients in Group B. The mean level of vitamin D (in ng/mL) was 27.89 ± 6.21 in Group A and 14.35 ± 5.79 in Group B, the difference was highly significant. The prevalence of vitamin D deficiency was 32.96% and 96.82% respectively in Group A and Group B. Out of total 154 patients, 90 patients were found to be deficient in vitamin D (Group A: 29; Group B: 61). Serum level of inflammatory markers was found to be higher in vitamin D deficient COVID-19 patients viz. IL-6 level (in pg/mL) 19.34 ± 6.17 vs 12.18 ± 4.29; Serum ferritin 319.17 ± 38.21 ng/mL vs 186.83 ± 20.18 ng/ mL; TNFα level (in pg/mL) 13.26 ± 5.64 vs 11.87 ± 3.15. The fatality rate was high in vitamin D deficient (21% vs 3.1%). Vitamin D level is markedly low in severe COVID-19 patients. Inflammatory response is high in vitamin D deficient COVID-19 patients. This all translates into increased mortality in vitamin D deficient COVID-19 patients. As per the flexible approach in the current COVID-19 pandemic authors recommend mass administration of vitamin D supplements to population at risk for COVID-19. In December 2019, several cases of pneumonia with unknown etiology reported in Wuhan, Hubei Province, China 1,2 . The disease spread quickly to other provinces of China and overseas. On 7 January 2020, a novel coronavirus was identified in the throat swab sample of one such patient and later declared to be the etiologic virus and was subsequently named as 2019nCoV by World Health Organization (WHO) 3 . On worsening of the situation WHO declared the outbreak as the public health emergency of international concern (PHEIC). In February 2020, WHO provided a nomenclature to the epidemic disease caused by SARS-CoV-2 as coronavirus disease 2019 (COVID-19) 4 . As on 12th August 2020 there are more than 20 million cases worldwide 5 , so for now it's almost impossible to contain the disease spread and focus is diverting towards better treatment and prevention of factors that enhance the severity of COVID-19. COVID-19 is characterized by its high infectivity and marked variability in clinical severity, of which..
Author contributions
Competing interests The authors declare no competing interests.
References
Aparna, Muthathal, Nongkynrih, Gupta, Vitamin D deficiency in India, J. Family Med. Prim. Care, doi:10.4103/jfmpc.jfmpc_78_18
Argyropoulos, Association of initial viral load in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) patients with outcome and symptoms, Am. J. Pathol, doi:10.1016/j.ajpath.2020.07.001
Baeke, Takiishi, Korf, Vitamin D: modulator of the immune system, Curr. Opin. Pharmacol
Biesalski, Vitamin D deficiency and co-morbidities in COVID-19 patients: a fatal relationship?, Nfs J, doi:10.1016/j.nfs.2020.06.001
Bikle, Vitamin D metabolism, mechanism of action, and clinical applications, Chem. Biol, doi:10.1016/j.chembiol.2013.12.016
Cardoso, Pereira, Native vitamin D in pre-dialysis chronic kidney disease, Nefrologia, doi:10.1016/j.nefro.2018.07.004
Cascella, Evaluation and Treatment Coronavirus (COVID-19)
Chen, Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study, Lancet, doi:10.1016/S0140-6736(20)30211-7
Ciceri, Microvascular COVID-19 lung vessels obstructive thromboinflammatory syndrome (MicroCLOTS): an atypical acute respiratory distress syndrome working hypothesis, Crit. Care Resusc
Gombart, Pierre, Maggini, A review of micronutrients and the immune system-working in harmony to reduce the risk of infection, Nutrients, doi:10.3390/nu12010236
Hill, Mantzoros, Sowers, Commentary: COVID-19 in patients with diabetes, Metabolism, doi:10.1016/j.metabol.2020.154217
Holick, Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline [published correction appears in, J Clin Endocrinol Metab
Huang, Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet, doi:10.1016/S0140-6736(20)30183-5
Hughes, Norton, Vitamin D and respiratory health, Clin. Exp. Immunol, doi:10.1111/j.1365-2249.2009.04001.x
Hunter, Jones, IL-6 as a keystone cytokine in health and disease, Nat. Immunol
Jones, Jenkins, Recent insights into targeting the IL-6 cytokine family in inflammatory diseases and cancer, Nat. Rev. Immunol, doi:10.1038/s41577-018-0066-7
Kamboj, Dwivedi, Toteja, Prevalence of hypovitaminosis D in India & way forward, Indian J. Med. Res, doi:10.4103/ijmr.IJMR_1807_18
Laird, Rhodes, Kenny, Vitamin D and inflammation: potential implications for severity of covid-19, Ir. Med. J
Latz, Blood type and outcomes in patients with COVID-19, Ann. Hematol, doi:10.1007/s00277-020-04169-1
Magro, SARS-CoV-2 and COVID-19: is interleukin-6 (IL-6) the "culprit lesion" of ARDS onset? What is there besides Tocilizumab?, Cytokine X, doi:10.1016/j.cytox.2020.100029
Martineau, Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data, BMJ
Nile, COVID-19: pathogenesis, cytokine storm and therapeutic potential of interferons, Cytokine Growth Factor Rev, doi:10.1016/j.cytogfr.2020.05.002
Prietl, Treiber, Piber, Amrein, Vitamin D and immune function, Nutrients
Thacher, Clarke, Vitamin D insufficiency, Mayo Clin. Proc, doi:10.4065/mcp.2010.0567
Wacker, Holick, Vitamin D: effects on skeletal and extraskeletal health and the need for supplementation, Nutrients, doi:10.3390/nu5010111
Wu, Mcgoogan, Characteristics of and important lessons from the coronavirus disease, doi:10.1001/jama.2020.2648
Xu, Vitamin D alleviates lipopolysaccharide-induced acute lung injury via regulation of the renin-angiotensin system, Mol. Med. Rep, doi:10.3892/mmr.2017.7546
DOI record:
{
"DOI": "10.1038/s41598-020-77093-z",
"ISSN": [
"2045-2322"
],
"URL": "http://dx.doi.org/10.1038/s41598-020-77093-z",
"abstract": "<jats:title>Abstract</jats:title><jats:p>COVID-19 is characterized by marked variability in clinical severity. Vitamin D had recently been reviewed as one of the factors that may affect the severity in COVID-19. The objective of current study is to analyze the vitamin D level in COVID-19 patients and its impact on the disease severity. After approval from Ethics Committee, M.L.B Medical College the current study was undertaken as continuous prospective observational study of 6 weeks. Participants were COVID-19 patients of age group 30–60 years admitted during the study period of 6 weeks. Study included either asymptomatic COVID-19 patients (Group A) or severely ill patients requiring ICU admission (Group B). Serum concentration of 25 (OH)D, were measured along with serum IL-6; TNFα and serum ferritin. Standard statistical analysis was performed to analyze the differences. Current Study enrolled 154 patients, 91 in Group A and 63 patients in Group B. The mean level of vitamin D (in ng/mL) was 27.89 ± 6.21 in Group A and 14.35 ± 5.79 in Group B, the difference was highly significant. The prevalence of vitamin D deficiency was 32.96% and 96.82% respectively in Group A and Group B. Out of total 154 patients, 90 patients were found to be deficient in vitamin D (Group A: 29; Group B: 61). Serum level of inflammatory markers was found to be higher in vitamin D deficient COVID-19 patients viz. IL-6 level (in pg/mL) 19.34 ± 6.17 vs 12.18 ± 4.29; Serum ferritin 319.17 ± 38.21 ng/mL vs 186.83 ± 20.18 ng/mL; TNFα level (in pg/mL) 13.26 ± 5.64 vs 11.87 ± 3.15. The fatality rate was high in vitamin D deficient (21% vs 3.1%). Vitamin D level is markedly low in severe COVID-19 patients. Inflammatory response is high in vitamin D deficient COVID-19 patients. This all translates into increased mortality in vitamin D deficient COVID-19 patients. As per the flexible approach in the current COVID-19 pandemic authors recommend mass administration of vitamin D supplements to population at risk for COVID-19.</jats:p>",
"alternative-id": [
"77093"
],
"article-number": "20191",
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "21 August 2020"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "23 October 2020"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "19 November 2020"
},
{
"group": {
"label": "Competing interests",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1,
"value": "The authors declare no competing interests."
}
],
"author": [
{
"affiliation": [],
"family": "Jain",
"given": "Anshul",
"sequence": "first"
},
{
"affiliation": [],
"family": "Chaurasia",
"given": "Rachna",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sengar",
"given": "Narendra Singh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Singh",
"given": "Mayank",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mahor",
"given": "Sachin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Narain",
"given": "Sumit",
"sequence": "additional"
}
],
"container-title": "Scientific Reports",
"container-title-short": "Sci Rep",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2020,
11,
19
]
],
"date-time": "2020-11-19T11:03:51Z",
"timestamp": 1605783831000
},
"deposited": {
"date-parts": [
[
2022,
12,
6
]
],
"date-time": "2022-12-06T23:25:14Z",
"timestamp": 1670369114000
},
"indexed": {
"date-parts": [
[
2024,
4,
8
]
],
"date-time": "2024-04-08T09:09:23Z",
"timestamp": 1712567363358
},
"is-referenced-by-count": 193,
"issue": "1",
"issued": {
"date-parts": [
[
2020,
11,
19
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2020,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2020,
11,
19
]
],
"date-time": "2020-11-19T00:00:00Z",
"timestamp": 1605744000000
}
},
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2020,
11,
19
]
],
"date-time": "2020-11-19T00:00:00Z",
"timestamp": 1605744000000
}
}
],
"link": [
{
"URL": "https://www.nature.com/articles/s41598-020-77093-z.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.nature.com/articles/s41598-020-77093-z",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.nature.com/articles/s41598-020-77093-z.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1038",
"published": {
"date-parts": [
[
2020,
11,
19
]
]
},
"published-online": {
"date-parts": [
[
2020,
11,
19
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"author": "C Huang",
"doi-asserted-by": "publisher",
"first-page": "497",
"journal-title": "Lancet",
"key": "77093_CR1",
"unstructured": "Huang, C. et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395, 497–506. https://doi.org/10.1016/S0140-6736(20)30183-5 (2020).",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30211-7",
"author": "N Chen",
"doi-asserted-by": "publisher",
"first-page": "507",
"issue": "10223",
"journal-title": "Lancet",
"key": "77093_CR2",
"unstructured": "Chen, N. et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 395(10223), 507–513. https://doi.org/10.1016/S0140-6736(20)30211-7 (2020).",
"volume": "395",
"year": "2020"
},
{
"key": "77093_CR3",
"unstructured": "WHO Clinical management of severe acute respiratory infection when Novel coronavirus (nCoV) infection is suspected: interim guidance. (2020). https://www.who.int/internal-publications-detail/clinical-management-of-severe-acute-respiratory-infection-when-novel-coronavirus-(ncov)-infection-is-suspected."
},
{
"key": "77093_CR4",
"unstructured": "Notice of the National Health Commission of the People’s Republic of China on revising the English name of novel coronavirus pneumonia (2020) https://www.nhc.gov.cn/yzygj/s7653p/202002/33393aa53d984ccdb1053a52b6bef810.shtml. Accessed 29 Feb 2020 (in Chinese)."
},
{
"key": "77093_CR5",
"unstructured": "WHO Coronavirus Disease (COVID-19) Dashboard Data last updated: 2020/8/12, 3:41pm CEST. https://covid19.who.int/WHO-COVID-19-global-data.csv. Accessed 13 Aug 2020."
},
{
"DOI": "10.1001/jama.2020.2648",
"author": "Z Wu",
"doi-asserted-by": "publisher",
"journal-title": "JAMA",
"key": "77093_CR6",
"unstructured": "Wu, Z. & McGoogan, J. M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA https://doi.org/10.1001/jama.2020.2648 (2020).",
"year": "2020"
},
{
"DOI": "10.1016/j.metabol.2020.154217",
"author": "MA Hill",
"doi-asserted-by": "publisher",
"first-page": "154217",
"journal-title": "Metabolism.",
"key": "77093_CR7",
"unstructured": "Hill, M. A., Mantzoros, C. & Sowers, J. R. Commentary: COVID-19 in patients with diabetes. Metabolism. 107, 154217. https://doi.org/10.1016/j.metabol.2020.154217 (2020).",
"volume": "107",
"year": "2020"
},
{
"key": "77093_CR8",
"unstructured": "Ross, A. C., Taylor, C. L., Yaktine, A. L. et al. (eds) Dietary Reference Intakes for Calcium and Vitamin D. Institute of Medicine (US) Committee to Review Dietary Reference Intakes for Vitamin D and Calcium (National Academies Press, Washington, DC, 2011).",
"volume-title": "Dietary Reference Intakes for Calcium and Vitamin D. Institute of Medicine (US) Committee to Review Dietary Reference Intakes for Vitamin D and Calcium",
"year": "2011"
},
{
"DOI": "10.3390/nu5010111",
"author": "M Wacker",
"doi-asserted-by": "publisher",
"first-page": "111",
"issue": "1",
"journal-title": "Nutrients.",
"key": "77093_CR9",
"unstructured": "Wacker, M. & Holick, M. F. Vitamin D: effects on skeletal and extraskeletal health and the need for supplementation. Nutrients. 5(1), 111–148. https://doi.org/10.3390/nu5010111 (2013).",
"volume": "5",
"year": "2013"
},
{
"DOI": "10.1210/jc.2011-0385",
"author": "MF Holick",
"doi-asserted-by": "publisher",
"first-page": "1911",
"issue": "7",
"journal-title": "J. Clin. Endocrinol. Metab.",
"key": "77093_CR10",
"unstructured": "Holick, M. F. et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline [published correction appears in [J Clin Endocrinol Metab 2011;96(12):3908]. J. Clin. Endocrinol. Metab. 96(7), 1911–1930. https://doi.org/10.1210/jc.2011-0385 (2011).",
"volume": "96",
"year": "2011"
},
{
"DOI": "10.1016/j.nefro.2018.07.004",
"author": "MP Cardoso",
"doi-asserted-by": "publisher",
"first-page": "18",
"issue": "1",
"journal-title": "Nefrologia.",
"key": "77093_CR11",
"unstructured": "Cardoso, M. P. & Pereira, L. A. L. Native vitamin D in pre-dialysis chronic kidney disease. Nefrologia. 39(1), 18–28. https://doi.org/10.1016/j.nefro.2018.07.004 (2019).",
"volume": "39",
"year": "2019"
},
{
"DOI": "10.1016/j.chembiol.2013.12.016",
"author": "DD Bikle",
"doi-asserted-by": "publisher",
"first-page": "319",
"issue": "3",
"journal-title": "Chem. Biol.",
"key": "77093_CR12",
"unstructured": "Bikle, D. D. Vitamin D metabolism, mechanism of action, and clinical applications. Chem. Biol. 21(3), 319–329. https://doi.org/10.1016/j.chembiol.2013.12.016 (2014).",
"volume": "21",
"year": "2014"
},
{
"DOI": "10.1111/j.1365-2249.2009.04001.x",
"author": "DA Hughes",
"doi-asserted-by": "publisher",
"first-page": "20",
"issue": "1",
"journal-title": "Clin. Exp. Immunol.",
"key": "77093_CR13",
"unstructured": "Hughes, D. A. & Norton, R. Vitamin D and respiratory health. Clin. Exp. Immunol. 158(1), 20–25. https://doi.org/10.1111/j.1365-2249.2009.04001.x (2009).",
"volume": "158",
"year": "2009"
},
{
"DOI": "10.4103/jfmpc.jfmpc_78_18",
"author": "P Aparna",
"doi-asserted-by": "publisher",
"first-page": "324",
"issue": "2",
"journal-title": "J. Family Med. Prim. Care.",
"key": "77093_CR14",
"unstructured": "Aparna, P., Muthathal, S., Nongkynrih, B. & Gupta, S. K. Vitamin D deficiency in India. J. Family Med. Prim. Care. 7(2), 324–330. https://doi.org/10.4103/jfmpc.jfmpc_78_18 (2018).",
"volume": "7",
"year": "2018"
},
{
"DOI": "10.4065/mcp.2010.0567",
"author": "TD Thacher",
"doi-asserted-by": "publisher",
"first-page": "50",
"issue": "1",
"journal-title": "Mayo Clin. Proc.",
"key": "77093_CR15",
"unstructured": "Thacher, T. D. & Clarke, B. L. Vitamin D insufficiency. Mayo Clin. Proc. 86(1), 50–60. https://doi.org/10.4065/mcp.2010.0567 (2011).",
"volume": "86",
"year": "2011"
},
{
"DOI": "10.1016/j.ajpath.2020.07.001",
"author": "KV Argyropoulos",
"doi-asserted-by": "publisher",
"journal-title": "Am. J. Pathol.",
"key": "77093_CR16",
"unstructured": "Argyropoulos, K. V. et al. Association of initial viral load in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) patients with outcome and symptoms. Am. J. Pathol. https://doi.org/10.1016/j.ajpath.2020.07.001 (2020).",
"year": "2020"
},
{
"DOI": "10.1007/s00277-020-04169-1",
"author": "CA Latz",
"doi-asserted-by": "publisher",
"first-page": "2113",
"issue": "9",
"journal-title": "Ann. Hematol.",
"key": "77093_CR17",
"unstructured": "Latz, C. A. et al. Blood type and outcomes in patients with COVID-19. Ann. Hematol. 99(9), 2113–2118. https://doi.org/10.1007/s00277-020-04169-1 (2020).",
"volume": "99",
"year": "2020"
},
{
"author": "M Cascella",
"key": "77093_CR18",
"unstructured": "Cascella, M. et al. Features, Evaluation and Treatment Coronavirus (COVID-19) (StatPearls Publishing, Treasure Island, 2020).",
"volume-title": "Features, Evaluation and Treatment Coronavirus (COVID-19)",
"year": "2020"
},
{
"DOI": "10.1016/j.cytogfr.2020.05.002",
"author": "SH Nile",
"doi-asserted-by": "publisher",
"first-page": "66",
"journal-title": "Cytokine Growth Factor Rev.",
"key": "77093_CR19",
"unstructured": "Nile, S. H. et al. COVID-19: pathogenesis, cytokine storm and therapeutic potential of interferons. Cytokine Growth Factor Rev. 53, 66–70. https://doi.org/10.1016/j.cytogfr.2020.05.002 (2020).",
"volume": "53",
"year": "2020"
},
{
"author": "F Ciceri",
"first-page": "95",
"issue": "2",
"journal-title": "Crit. Care Resusc.",
"key": "77093_CR20",
"unstructured": "Ciceri, F. et al. Microvascular COVID-19 lung vessels obstructive thromboinflammatory syndrome (MicroCLOTS): an atypical acute respiratory distress syndrome working hypothesis. Crit. Care Resusc. 22(2), 95–97 (2020).",
"volume": "22",
"year": "2020"
},
{
"DOI": "10.1016/j.cytox.2020.100029",
"author": "G Magro",
"doi-asserted-by": "publisher",
"first-page": "100029",
"issue": "2",
"journal-title": "Cytokine X.",
"key": "77093_CR21",
"unstructured": "Magro, G. SARS-CoV-2 and COVID-19: is interleukin-6 (IL-6) the “culprit lesion” of ARDS onset? What is there besides Tocilizumab?. Cytokine X. 2(2), 100029. https://doi.org/10.1016/j.cytox.2020.100029 (2020).",
"volume": "2",
"year": "2020"
},
{
"DOI": "10.1038/s41577-018-0066-7",
"author": "SA Jones",
"doi-asserted-by": "publisher",
"first-page": "773",
"issue": "12",
"journal-title": "Nat. Rev. Immunol.",
"key": "77093_CR22",
"unstructured": "Jones, S. A. & Jenkins, B. J. Recent insights into targeting the IL-6 cytokine family in inflammatory diseases and cancer. Nat. Rev. Immunol. 18(12), 773–789. https://doi.org/10.1038/s41577-018-0066-7 (2018).",
"volume": "18",
"year": "2018"
},
{
"DOI": "10.1038/ni.3153",
"author": "CA Hunter",
"doi-asserted-by": "publisher",
"first-page": "448",
"journal-title": "Nat. Immunol.",
"key": "77093_CR23",
"unstructured": "Hunter, C. A. & Jones, S. A. IL-6 as a keystone cytokine in health and disease. Nat. Immunol. 16, 448–457 (2015).",
"volume": "16",
"year": "2015"
},
{
"DOI": "10.3390/nu5072502",
"author": "B Prietl",
"doi-asserted-by": "publisher",
"first-page": "2502",
"journal-title": "Nutrients.",
"key": "77093_CR24",
"unstructured": "Prietl, B., Treiber, G., Piber, T. R. & Amrein, K. Vitamin D and immune function. Nutrients. 5, 2502–2521 (2013).",
"volume": "5",
"year": "2013"
},
{
"DOI": "10.1136/bmj.i6583",
"author": "AR Martineau",
"doi-asserted-by": "publisher",
"first-page": "6583",
"journal-title": "BMJ",
"key": "77093_CR25",
"unstructured": "Martineau, A. R. Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. BMJ 356, 6583–6594 (2017).",
"volume": "356",
"year": "2017"
},
{
"DOI": "10.3390/nu12010236",
"author": "AF Gombart",
"doi-asserted-by": "publisher",
"first-page": "236",
"issue": "1",
"journal-title": "Nutrients.",
"key": "77093_CR26",
"unstructured": "Gombart, A. F., Pierre, A. & Maggini, S. A review of micronutrients and the immune system-working in harmony to reduce the risk of infection. Nutrients. 12(1), 236. https://doi.org/10.3390/nu12010236 (2020).",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1016/j.coph.2010.04.001",
"author": "F Baeke",
"doi-asserted-by": "publisher",
"first-page": "482",
"journal-title": "Curr. Opin. Pharmacol.",
"key": "77093_CR27",
"unstructured": "Baeke, F., Takiishi, T. & Korf, H. Vitamin D: modulator of the immune system. Curr. Opin. Pharmacol. 10, 482–496 (2010).",
"volume": "10",
"year": "2010"
},
{
"DOI": "10.4103/ijmr.IJMR_1807_18",
"author": "P Kamboj",
"doi-asserted-by": "publisher",
"first-page": "548",
"issue": "5",
"journal-title": "Indian J. Med. Res.",
"key": "77093_CR28",
"unstructured": "Kamboj, P., Dwivedi, S. & Toteja, G. S. Prevalence of hypovitaminosis D in India & way forward. Indian J. Med. Res. 148(5), 548–556. https://doi.org/10.4103/ijmr.IJMR_1807_18 (2018).",
"volume": "148",
"year": "2018"
},
{
"DOI": "10.3892/mmr.2017.7546",
"author": "J Xu",
"doi-asserted-by": "publisher",
"first-page": "7432",
"issue": "5",
"journal-title": "Mol. Med. Rep.",
"key": "77093_CR29",
"unstructured": "Xu, J. et al. Vitamin D alleviates lipopolysaccharide-induced acute lung injury via regulation of the renin-angiotensin system. Mol. Med. Rep. 16(5), 7432–7438. https://doi.org/10.3892/mmr.2017.7546 (2017).",
"volume": "16",
"year": "2017"
},
{
"DOI": "10.1016/j.nfs.2020.06.001",
"author": "HK Biesalski",
"doi-asserted-by": "publisher",
"first-page": "10",
"journal-title": "Nfs J.",
"key": "77093_CR30",
"unstructured": "Biesalski, H. K. Vitamin D deficiency and co-morbidities in COVID-19 patients: a fatal relationship?. Nfs J. 20, 10–21. https://doi.org/10.1016/j.nfs.2020.06.001 (2020).",
"volume": "20",
"year": "2020"
},
{
"author": "E Laird",
"first-page": "81",
"issue": "5",
"journal-title": "Ir. Med. J.",
"key": "77093_CR31",
"unstructured": "Laird, E., Rhodes, J. & Kenny, R. A. Vitamin D and inflammation: potential implications for severity of covid-19. Ir. Med. J. 113(5), 81 (2020).",
"volume": "113",
"year": "2020"
}
],
"reference-count": 31,
"references-count": 31,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.nature.com/articles/s41598-020-77093-z"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Multidisciplinary"
],
"subtitle": [],
"title": "Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "10"
}
