The Role of Vitamin D in COVID-19 Survival and Prevention: A Meta-analysis
et al., Sudan Journal of Medical Sciences, doi:10.18502/sjms.v19i1.15776, Mar 2024
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Meta analysis of 16 studies including over 5.9 million patients showing significantly lower mortality and cases with vitamin D treatment.
20 meta-analyses show significant improvements with vitamin D treatment for mortality1-14,
mechanical ventilation1,5,6,11,15-17 ,
ICU admission1,3,5,6,9,11,13,15-19 ,
hospitalization11,
severity2,4,5,10,20 , and
cases7,19,20 .
Currently there are 136 vitamin D treatment for COVID-19 studies, showing 39% lower mortality [31‑45%], 17% lower ventilation [-5‑35%], 45% lower ICU admission [28‑57%], 22% lower hospitalization [13‑30%], and 17% fewer cases [9‑25%].
|
risk of death, 56.7% lower, OR 0.43, p < 0.001, inverted to make OR<1 favor treatment, RR approximated with OR.
|
|
risk of case, 47.9% lower, OR 0.52, p = 0.046, inverted to make OR<1 favor treatment, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Shah et al., Does vitamin D supplementation reduce COVID-19 severity? - a systematic review, QJM: An International Journal of Medicine, doi:10.1093/qjmed/hcac040.
2.
Nikniaz et al., The impact of vitamin D supplementation on mortality rate and clinical outcomes of COVID-19 patients: A systematic review and meta-analysis, Pharmaceutical Sciences, doi:10.34172/PS.2021.13.
3.
Hosseini et al., Effects of Vitamin D Supplementation on COVID-19 Related Outcomes: A Systematic Review and Meta-Analysis, Nutrients, doi:10.3390/nu14102134.
4.
D’Ecclesiis et al., Vitamin D and SARS-CoV2 infection, severity and mortality: A systematic review and meta-analysis, PLOS ONE, doi:10.1371/journal.pone.0268396.
5.
Xie et al., Micronutrient perspective on COVID-19: Umbrella review and reanalysis of meta-analyses, Critical Reviews in Food Science and Nutrition, doi:10.1080/10408398.2023.2174948.
6.
Hariyanto et al., Vitamin D supplementation and Covid‐19 outcomes: A systematic review, meta‐analysis and meta‐regression, Reviews in Medical Virology, doi:10.1002/rmv.2269.
7.
Begum et al., The Role of Vitamin D in COVID-19 Survival and Prevention: A Meta-analysis, Sudan Journal of Medical Sciences, doi:10.18502/sjms.v19i1.15776.
8.
Jamilian et al., The role of vitamin D in outcomes of critical care in COVID-19 patients: Evidence from an umbrella meta-analysis of interventional and observational studies, Public Health Nutrition, doi:10.1017/S1368980024000934.
9.
Sobczak et al., Effect of Vitamin D3 Supplementation on Severe COVID-19: A Meta-Analysis of Randomized Clinical Trials, Nutrients, doi:10.3390/nu16101402.
10.
Petrelli et al., Therapeutic and prognostic role of vitamin D for COVID-19 infection: A systematic review and meta-analysis of 43 observational studies, The Journal of Steroid Biochemistry and Molecular Biology, doi:10.1016/j.jsbmb.2021.105883.
11.
Asla et al., Vitamin D on COVID-19 Patients During the Pandemic, 2022. A Systematic Review and Meta-Analysis, Current Research in Nutrition and Food Science Journal, doi:10.12944/CRNFSJ.11.1.3.
12.
Kow et al., The impact of vitamin D administration on mortality in COVID-19 patients: a systematic review and meta-analysis of randomized controlled trials, Inflammopharmacology, doi:10.1007/s10787-024-01564-2.
13.
Zhang et al., The impact of supplementing vitamin D through different methods on the prognosis of COVID-19 patients: a systematic review and meta-analysis, Frontiers in Nutrition, doi:10.3389/fnut.2024.1441847.
14.
Doustmohammadian et al., Impact of vitamin D supplementation on COVID-19 mortality: A systematic review and meta-analysis, Nutrition Clinique et Métabolisme, doi:10.1016/j.nupar.2025.12.001.
15.
Meng et al., The role of vitamin D in the prevention and treatment of SARS-CoV-2 infection: A meta-analysis of randomized controlled trials, Clinical Nutrition, doi:10.1016/j.clnu.2023.09.008.
16.
Yang et al., Therapeutic effects of vitamin D supplementation on COVID-19 aggravation: a systematic review and meta-analysis of randomized controlled trials, Frontiers in Pharmacology, doi:10.3389/fphar.2024.1367686.
17.
Szarpak et al., Vitamin D supplementation to treat SARS-CoV-2 positive patients. Evidence from meta-analysis, Cardiology Journal, doi:10.5603/CJ.a2021.0122.
18.
Tentolouris et al., The effect of vitamin D supplementation on mortality and intensive care unit admission of COVID-19 patients. A systematic review, meta-analysis and meta-regression, Diabetes/Metabolism Research and Reviews, doi:10.1002/dmrr.3517.
Begum et al., 29 Mar 2024, peer-reviewed, 2 authors.
The Role of Vitamin D in COVID-19 Survival and Prevention: A Meta-analysis
doi:10.18502/sjms.v19i1.15776
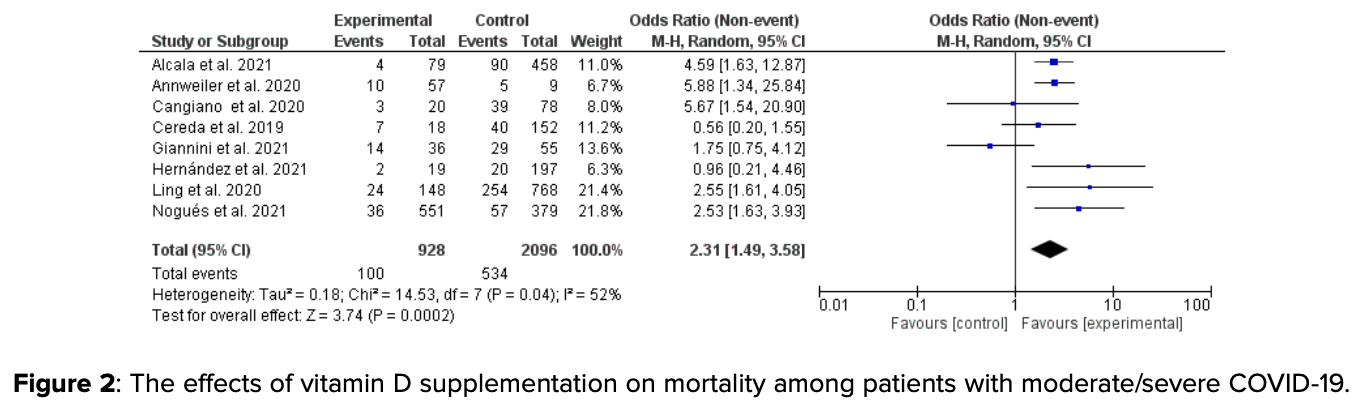
Background: COVID-19 is still ongoing with frequently discovered new strains, although vaccines are highly effective for prevention. Literature on vitamin D supplementation in COVID-19 prevention and its effect on survival is scarce. This meta-analysis assessed the role of vitamin D supplementation in COVID-19 prevention and survival. Methods: Four databases (Web of Science, SCOPUS, PubMed, MEDLINE, and the first 100 articles of Google Scholar) were searched for articles published up to September 2023. The keywords used were COVID-19, mortality, vitamin D supplementation, calcitriol, cholecalciferol, Calcifediol, survival, death, and prevention. Six hundred and seven studies were retrieved, and four hundred and three remained after duplication removal; of them eighty-three full texts were screened, and of them, only sixteen (prospective, randomized controlled trials, and retrospective studies) were included in the final meta-analysis. Results: Sixteen observational studies including 5905,109 patients and 186,500 events were included. Vitamin D supplementation reduced mortality among patients with odd ratio, 2.31, 95% CI,; in addition, supplementation was effective in COVID-19 prevention, odd ratio, 1.92, 95% CI, 1.01-3.64. Conclusion: Vitamin D supplementation prevented COVID-19 and increased survival among patients admitted with moderate/severe COVID-19.
Ethical Considerations The authors did not include any manuscript published by them.
Competing Interests None
References
Alcala-Diaz, Limia-Perez, Gomez-Huelgas, Martin-Escalante, Cortes-Rodriguez et al., Calcifediol treatment and hospital mortality due to COVID-19: A cohort study, Nutrients, doi:10.3390/nu13061760
Alcalá-Santiago, Rodríguez-Barranco, Rava, Jiménez-Sousa, Gil et al., Vitamin D deficiency and COVID-19: A biological database study on pathways and gene-disease associations, International Journal of Molecular Sciences, doi:10.3390/ijms232214256
Annweiler, Beaudenon, Gautier, Gonsard, Boucher et al., Highdose versus standard-dose vitamin D supplementation in older adults with COVID-19 (COVIT-TRIAL): A multicenter, open-label, randomized controlled superiority trial, PLoS Medicine, doi:10.1371/journal.pmed.1003999
Annweiler, Corvaisier, Gautier, Dubée, Legrand et al., Vitamin D supplementation associated to better survival in hospitalized frail elderly COVID-19 patients: The GERIA-COVID quasi-experimental study, Nutrients, doi:10.3390/nu12113377
Annweiler, Hanotte, Grandin De L'eprevier, Sabatier, Lafaie et al., Vitamin D and survival in COVID-19 patients: A quasi-experimental study, The Journal of Steroid Biochemistry and Molecular Biology, doi:10.1016/j.jsbmb.2020.105771
Bassatne, Basbous, Chakhtoura, El Zein, Rahme et al., The link between COVID-19 and VItamin D (VIVID): A systematic review and meta-analysis, Metabolism: Clinical and Experimental, doi:10.1016/j.metabol.2021.154753
Bilezikian, Bikle, Hewison, Lazaretti-Castro, Formenti et al., Mechanisms in endocrinology: Vitamin D and COVID-19, European Journal of Endocrinology, doi:10.1530/EJE-20-0665
Brunvoll, Nygaard, Ellingjord-Dale, Holland, Istre et al., Prevention of covid-19 and other acute respiratory infections with cod liver oil supplementation, a low dose vitamin D supplement: Sudan Journal of Medical Sciences Begum, Mirghani Quadruple blinded, randomised placebo controlled trial, BMJ (Clinical Research Ed, doi:10.1136/bmj-2022-071245
Butler-Laporte, Nakanishi, Mooser, Morrison, Abdullah et al., Vitamin D and COVID-19 susceptibility and severity in the COVID-19 Host Genetics Initiative: A Mendelian randomization study, PLoS Medicine, doi:10.1371/journal.pmed.1003605
Cangiano, Fatti, Danesi, Gazzano, Croci et al., Mortality in an Italian nursing home during COVID-19 pandemic: Correlation with gender, age, ADL, vitamin D supplementation, and limitations of the diagnostic tests, Aging, doi:10.18632/aging.202307
Cannata-Andía, Díaz-Sottolano, Fernández, Palomo-Antequera, Herrero-Puente et al., COVID-VIT-D trial collaborators. A single-oral bolus of 100,000 IU of cholecalciferol at hospital admission did not improve outcomes in the COVID-19 disease: The COVID-VIT-D-a randomised multicentre international clinical trial, BMC Medicine, doi:10.1186/s12916-022-02290-8
Castillo, Entrenas Costa, Vaquero Barrios, Alcalá Díaz, López Miranda et al., Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19, The Journal of Steroid Biochemistry and Molecular Biology, doi:10.1016/j.jsbmb.2020.105751
Cereda, Bogliolo, Lobascio, Barichella, Zecchinelli et al., Vitamin D supplementation and outcomes in coronavirus disease 2019 (COVID-19) patients from the outbreak area of Lombardy, Italy. Nutrition, doi:10.1016/j.nut.2020.111055
Chang, Wang, Zhou, Long, STAT3 roles in viral infection: Antiviral or proviral?, Future Virology, doi:10.2217/fvl-2018-0033
Chen, Haupert, Zimmermann, Shi, Fritsche et al., Global prevalence of post-coronavirus disease 2019 (COVID-19) condition or long COVID: A meta-analysis and systematic review, The Journal of Infectious Diseases, doi:10.1093/infdis/jiac136
D'avolio, Avataneo, Manca, Cusato, De Nicolò et al., 25-Hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2, Nutrients, doi:10.3390/nu12051359
Dirks, Ackermans, Lips, De Jongh, Vervloet et al., The when, what & how of measuring vitamin D metabolism in clinical medicine, Nutrients, doi:10.3390/nu10040482
Feentved Ødum, Kongsbak-Wismann, Vitamin D and SARS-CoV-2, Basic & Clinical Pharmacology & Toxicology, doi:10.1111/bcpt.13872
Fernandes, Murai, Reis, Sales, Santos et al., Effect of a single high dose of vitamin D3 on cytokines, chemokines, and growth factor in patients with moderate to severe COVID-19, The American Journal of Clinical Nutrition, doi:10.1093/ajcn/nqab426
Gharibi, Babaloo, Hosseini, Abdollahpour-Alitappeh, Hashemi et al., Targeting STAT3 in cancer and autoimmune diseases, European Journal of Pharmacology, doi:10.1016/j.ejphar.2020.173107
Giannini, Passeri, Tripepi, Sella, Fusaro et al., Effectiveness of in-hospital cholecalciferol use on clinical outcomes in comorbid COVID-19 patients: A hypothesis-generating study, Nutrients, doi:10.3390/nu13010219
Griffin, Hewison, Hopkin, Kenny, Quinton et al., Perspective: Vitamin D supplementation prevents rickets and acute respiratory infections when given as daily maintenance but not as intermittent bolus: Implications for COVID-19, Clinical Medicine, doi:10.7861/clinmed.2021-0035
Hartling, Milne, Hamm, Vandermeer, Ansari et al., Testing the Newcastle Ottawa Scale showed low reliability between individual reviewers, Journal of Clinical Epidemiology, doi:10.1016/j.jclinepi.2013.03.003
Hastie, Pell, Sattar, Vitamin D and COVID-19 infection and mortality in UK Biobank, European Journal of Nutrition, doi:10.1007/s00394-020-02372-4
Hernández, Nan, Fernandez-Ayala, García-Unzueta, Hernández-Hernández et al., Vitamin D status in hospitalized patients with SARS-CoV-2 infection, The Journal of Clinical Endocrinology and Metabolism, doi:10.1210/clinem/dgaa733
Hosseini, El Abd, Ducharme, Effects of vitamin D supplementation on COVID-19 related outcomes: A systematic review and meta-analysis, Nutrients, doi:10.3390/nu14102134
Hu, Kung, Cave, Banh, Effects of vitamin D serum level on morbidity and mortality in patients with COVID-19: A systematic review and meta-analysis, Journal of Pharmacy & Pharmaceutical Sciences, doi:10.18433/jpps32590
Igelström, Campbell, Craig, Katikireddi, Cochrane's risk of bias tool for non-randomized studies (ROBINS-I) is frequently misapplied: A methodological systematic review, Journal of Clinical Epidemiology, doi:10.1016/j.jclinepi.2021.08.022
Jolliffe, Camargo, Jr, Sluyter, Aglipay et al., Vitamin D supplementation to prevent acute respiratory infections: systematic review and meta-analysis of aggregate data from randomised controlled trials, medRxiv, doi:10.1101/2020.07.14.20152728
Jolliffe, Holt, Greenig, Talaei, Perdek et al., Effect of a test-and-treat approach to vitamin D supplementation on risk of all cause acute respiratory tract infection and covid-19: Phase 3 randomised controlled trial (CORONAVIT), BMJ (Clinical Research Ed, doi:10.1136/bmj-2022-071230
Karonova, Chernikova, Golovatyuk, Bykova, Grant et al., Vitamin D intake may reduce SARS-CoV-2 infection morbidity in health care workers, Nutrients, doi:10.3390/nu14030505
Kouhpayeh, Shariati, Boshtam, Rahimmanesh, Mirian et al., The molecular basis of COVID-19 pathogenesis, conventional and nanomedicine therapy, International Journal of Molecular Sciences, doi:10.3390/ijms22115438
Ling, Broad, Murphy, Pappachan, Pardesi-Newton et al., High-dose cholecalciferol booster therapy is associated with a reduced risk of mortality in patients with COVID-19: A cross-sectional multicentre observational study, Nutrients, doi:10.3390/nu12123799
Ma, Zhou, Heianza, Qi, Habitual use of vitamin D supplements and risk of coronavirus disease 2019 (COVID-19) infection: A prospective study in UK Biobank, The American Journal of Clinical Nutrition, doi:10.1093/ajcn/nqaa381
Marino, Misra, Extraskeletal effects of vitamin D, Nutrients, doi:10.3390/nu11071460
Martineau, Jolliffe, Hooper, Greenberg, Aloia et al., Vitamin D supplementation to prevent acute respiratory tract infections: Systematic review and meta-analysis of individual participant data, BMJ (Clinical Research Ed, doi:10.1136/bmj.i6583
Meltzer, Best, Zhang, Vokes, Arora et al., Association of vitamin D status and other clinical characteristics with COVID-19 test results, JAMA Network Open, doi:10.1001/jamanetworkopen.2020.19722
Murai, Fernandes, Sales, Pinto, Goessler et al., Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: A randomized clinical trial, Journal of the American Medical Association, doi:10.1001/jama.2020.26848
Nguyen, Raju, Da Graca, Wang, Mohamed et al., 25-hydroxyvitamin D is a predictor of COVID-19 severity of hospitalized patients, PLoS One, doi:10.1371/journal.pone.0268038
Nikniaz, Akbarzadeh, Hosseinifard, Hosseini, The impact of vitamin D supplementation on mortality rate and clinical outcomes of COVID-19 patients: A systematic review and meta-analysis, MedRxiv, doi:10.1101/2021.01.04.21249219
Nogues, Ovejero, Pineda-Moncusí, Bouillon, Arenas et al., Calcifediol treatment and COVID-19-related outcomes, The Journal of Clinical Endocrinology and Metabolism, doi:10.1210/clinem/dgab405
Oristrell, Oliva, Subirana, Casado, Domínguez et al., Association of calcitriol supplementation with reduced COVID-19 mortality in patients with chronic kidney disease: A populationbased study, Biomedicines, doi:10.3390/biomedicines9050509
Pal, Banerjee, Bhadada, Shetty, Singh et al., Vitamin D supplementation and clinical outcomes in COVID-19: A systematic review and meta-analysis, Journal of Endocrinological Investigation, doi:10.1007/s40618-021-01614-4
Quesada-Gomez, Entrenas-Castillo, Bouillon, Vitamin D receptor stimulation to reduce acute respiratory distress syndrome (ARDS) in patients with coronavirus SARS-CoV-2 infections: Revised Ms SBMB 2020_166, The Journal of Steroid Biochemistry and Molecular Biology, doi:10.1016/j.jsbmb.2020.105719
Rawat, Roy, Maitra, Shankar, Khanna et al., Vitamin D supplementation and COVID-19 treatment: A systematic review and meta-analysis, Diabetes & Metabolic Syndrome, doi:10.1016/j.dsx.2021.102189
Shah, Saxena, Mavalankar, Vitamin D supplementation, COVID-19 and disease severity: A meta-analysis, QJM, doi:10.1093/qjmed/hcab009
Silva, Lazaretti-Castro, Vitamin D metabolism and extraskeletal outcomes: An update, Archives of Endocrinology and Metabolism, doi:10.20945/2359-3997000000565
Tomaszewska, Rustecka, Lipińska-Opałka, Piprek, Kloc et al., The role of vitamin D in COVID-19 and the impact of pandemic restrictions on vitamin D blood content, Frontiers in Pharmacology, doi:10.3389/fphar.2022.836738
Villasis-Keever, López-Alarcón, Miranda-Novales, Zurita-Cruz, Barrada-Vázquez et al., Efficacy and safety of vitamin D supplementation to prevent COVID-19 in frontline healthcare workers. A randomized clinical trial, Archives of Medical Research, doi:10.1016/j.arcmed.2022.04.003
Wang, Paulson, Pease, Watson, Comfort et al., Estimating excess mortality due to the COVID-19 pandemic: A systematic analysis of COVID-19related mortality, 2020-21, Lancet, doi:10.1016/S0140-6736(21)02796-3
