The effect of vitamin D supplementation on mortality and intensive care unit admission of COVID-19 patients. A systematic review, meta-analysis and meta-regression
et al., Diabetes/Metabolism Research and Reviews, doi:10.1002/dmrr.3517, Jan 2022
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Systematic review and meta analysis of 10 vitamin D studies showing lower mortality, and ICU admission with treatment, statistically significant only for ICU admission.
20 meta-analyses show significant improvements with vitamin D treatment for mortality1-14,
mechanical ventilation1,5,6,11,15-17 ,
ICU admission1,3,5,6,9,11,13,15-19 ,
hospitalization11,
severity2,4,5,10,20 , and
cases7,19,20 .
Currently there are 136 vitamin D treatment for COVID-19 studies, showing 39% lower mortality [31‑45%], 17% lower ventilation [-5‑35%], 45% lower ICU admission [28‑57%], 22% lower hospitalization [13‑30%], and 17% fewer cases [9‑25%].
|
risk of death, 40.3% lower, OR 0.60, p = 0.11, RR approximated with OR.
|
|
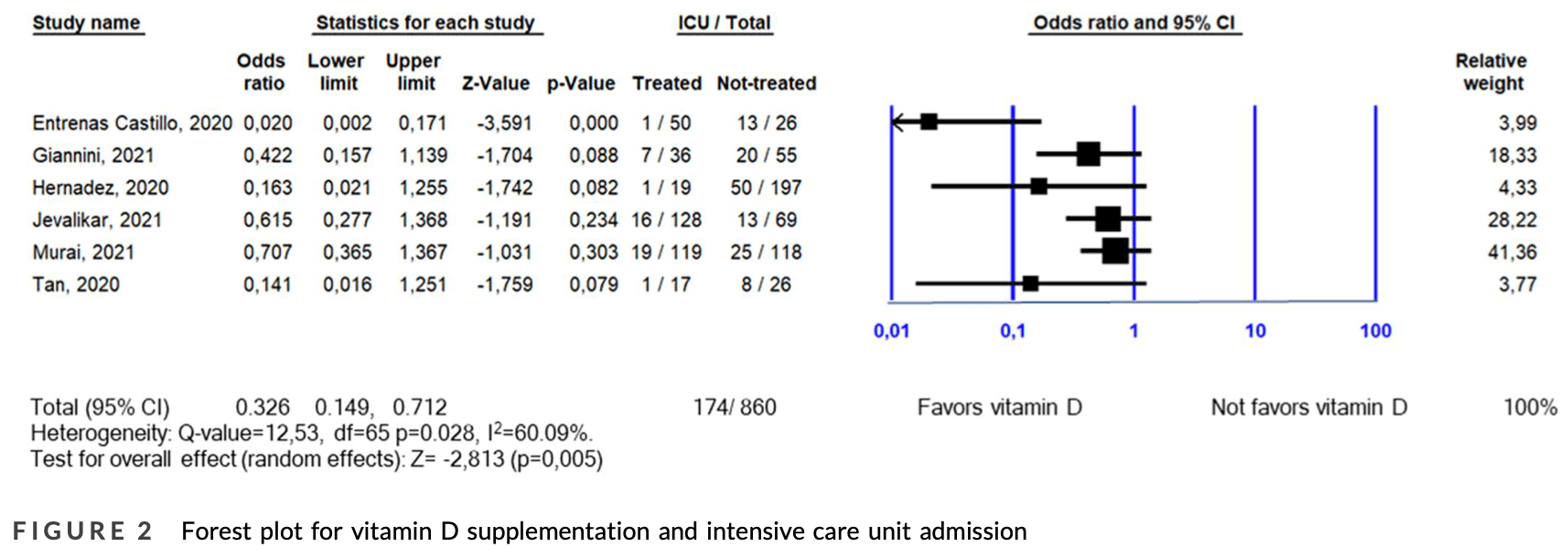
risk of ICU admission, 67.4% lower, OR 0.33, p = 0.005, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Shah et al., Does vitamin D supplementation reduce COVID-19 severity? - a systematic review, QJM: An International Journal of Medicine, doi:10.1093/qjmed/hcac040.
2.
Nikniaz et al., The impact of vitamin D supplementation on mortality rate and clinical outcomes of COVID-19 patients: A systematic review and meta-analysis, Pharmaceutical Sciences, doi:10.34172/PS.2021.13.
3.
Hosseini et al., Effects of Vitamin D Supplementation on COVID-19 Related Outcomes: A Systematic Review and Meta-Analysis, Nutrients, doi:10.3390/nu14102134.
4.
D’Ecclesiis et al., Vitamin D and SARS-CoV2 infection, severity and mortality: A systematic review and meta-analysis, PLOS ONE, doi:10.1371/journal.pone.0268396.
5.
Xie et al., Micronutrient perspective on COVID-19: Umbrella review and reanalysis of meta-analyses, Critical Reviews in Food Science and Nutrition, doi:10.1080/10408398.2023.2174948.
6.
Hariyanto et al., Vitamin D supplementation and Covid‐19 outcomes: A systematic review, meta‐analysis and meta‐regression, Reviews in Medical Virology, doi:10.1002/rmv.2269.
7.
Begum et al., The Role of Vitamin D in COVID-19 Survival and Prevention: A Meta-analysis, Sudan Journal of Medical Sciences, doi:10.18502/sjms.v19i1.15776.
8.
Jamilian et al., The role of vitamin D in outcomes of critical care in COVID-19 patients: Evidence from an umbrella meta-analysis of interventional and observational studies, Public Health Nutrition, doi:10.1017/S1368980024000934.
9.
Sobczak et al., Effect of Vitamin D3 Supplementation on Severe COVID-19: A Meta-Analysis of Randomized Clinical Trials, Nutrients, doi:10.3390/nu16101402.
10.
Petrelli et al., Therapeutic and prognostic role of vitamin D for COVID-19 infection: A systematic review and meta-analysis of 43 observational studies, The Journal of Steroid Biochemistry and Molecular Biology, doi:10.1016/j.jsbmb.2021.105883.
11.
Asla et al., Vitamin D on COVID-19 Patients During the Pandemic, 2022. A Systematic Review and Meta-Analysis, Current Research in Nutrition and Food Science Journal, doi:10.12944/CRNFSJ.11.1.3.
12.
Kow et al., The impact of vitamin D administration on mortality in COVID-19 patients: a systematic review and meta-analysis of randomized controlled trials, Inflammopharmacology, doi:10.1007/s10787-024-01564-2.
13.
Zhang et al., The impact of supplementing vitamin D through different methods on the prognosis of COVID-19 patients: a systematic review and meta-analysis, Frontiers in Nutrition, doi:10.3389/fnut.2024.1441847.
14.
Doustmohammadian et al., Impact of vitamin D supplementation on COVID-19 mortality: A systematic review and meta-analysis, Nutrition Clinique et Métabolisme, doi:10.1016/j.nupar.2025.12.001.
15.
Meng et al., The role of vitamin D in the prevention and treatment of SARS-CoV-2 infection: A meta-analysis of randomized controlled trials, Clinical Nutrition, doi:10.1016/j.clnu.2023.09.008.
16.
Yang et al., Therapeutic effects of vitamin D supplementation on COVID-19 aggravation: a systematic review and meta-analysis of randomized controlled trials, Frontiers in Pharmacology, doi:10.3389/fphar.2024.1367686.
17.
Szarpak et al., Vitamin D supplementation to treat SARS-CoV-2 positive patients. Evidence from meta-analysis, Cardiology Journal, doi:10.5603/CJ.a2021.0122.
18.
Tentolouris et al., The effect of vitamin D supplementation on mortality and intensive care unit admission of COVID-19 patients. A systematic review, meta-analysis and meta-regression, Diabetes/Metabolism Research and Reviews, doi:10.1002/dmrr.3517.
Tentolouris et al., 15 Jan 2022, peer-reviewed, 5 authors.
Contact: ntentol@med.uoa.gr.
The effect of vitamin D supplementation on mortality and intensive care unit admission of COVID‐19 patients. A systematic review, meta‐analysis and meta‐regression
Diabetes/Metabolism Research and Reviews, doi:10.1002/dmrr.3517
Aims: The aim of this systematic review and meta-analysis was to investigate the effect of vitamin D supplementation on mortality and admission to intensive care unit (ICU) of COVID-19 patients.
Methods : A systematic search of PubMed, Google Scholar, Embase, Web of Science and medRxiv with terms relative to vitamin D supplementation and COVID-19 was conducted on 26 March 2021. Comprehensive Meta-Analysis software was used for the quantitative assessment of data and random-effects model was applied. To investigate the association between the dose of vitamin D and the outcomes of interest, meta-regression analysis was performed. Results: Two thousand and seventy-eight patients from nine studies with data on mortality were included (583 received vitamin D supplementation, while 1495 did not). Sixty-one (10.46%) individuals in the treated group died, compared to 386 (25.81%) in the non-treated group (odds ratio [OR]: 0.597; 95% CI: 0.318-1.121; p = 0.109). Eight hundred and sixty patients from six studies with data on ICU admission were included (369 received vitamin D supplementation, while 491 did not). Forty-five (12.19%) individuals in the treated group were admitted to ICU, compared to 129 (26.27%) in the non-treated group (OR: 0.326; 95% CI: 0.149-0.712; p = 0.005). No significant linear relationship between vitamin D dose and log OR of mortality or log OR of ICU admission was observed. Conclusion: This meta-analysis indicates a beneficial role of vitamin D supplementation on ICU admission, but not on mortality, of COVID-19 patients. Further research is urgently needed to understand the benefit of vitamin D in COVID-19.
CONFLICT OF INTEREST The authors declare they have no conflict of interest.
ETHICS STATEMENT This study did not involve human participants or animal research. This work was based on already produced and published data.
AUTHOR CONTRIBUTIONS Georgia Samakidou and Ioanna Eleftheriadou determined the search strategy, screened the selected studies and extracted the data. Nikolaos Tentolouris and Anastasios Tentolouris performed the statistical analysis. All authors participated in the writing and revision of this paper. All authors have read and approved this final manuscript.
SUPPORTING INFORMATION Additional supporting information may be found in the online version of the article at the publisher's website.
How to cite this article:
References
Akbar, Wibowo, Pranata, Setiabudiawan, Low serum 25-hydroxyvitamin D (vitamin D) level is associated with susceptibility to COVID-19, severity, and mortality: a systematic review and metaanalysis, Front Nutr
Angelidi, Belanger, Lorinsky, Vitamin D status is associated with in-hospital mortality and mechanical ventilation: a cohort of COVID-19 hospitalized patients, Mayo Clin Proc
Annweiler, Corvaisier, Gautier, Vitamin D supplementation associated to better survival in hospitalized frail elderly 10 of 11 -TENTOLOURIS ET AL
Arnold, COVID-19 -does this disease kill due to imbalance of the renin angiotensin system (RAS) caused by genetic and gender differences in the response to viral ACE 2 attack?, Heart Lung Circ
Bassatne, Basbous, Chakhtoura, Zein, Rahme et al., The link between COVID-19 and VItamin D (VIVID): a systematic review and meta-analysis, Metabolism
Bilezikian, Bikle, Hewison, Mechanisms IN endocrinology: vitamin D and COVID-19, Eur J Endocrinol
Boucher, Vitamin D status as a predictor of Covid-19 risk in Black, Asian and other ethnic minority groups in the UK, Diabetes Metab Res Rev
Bringhurst, Demay, Kronenberg, Mineral Metabolism, Williams Textbook of Endocrinology
Cangiano, Fatti, Danesi, Mortality in an Italian nursing home during COVID-19 pandemic: correlation with gender, age, ADL, vitamin D supplementation, and limitations of the diagnostic tests, Aging
Castillo, Costa, Barrios, Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: a pilot randomized clinical study, J Steroid Biochem Mol Biol
Cereda, Bogliolo, Lobascio, Vitamin D supplementation and outcomes in coronavirus disease 2019 (COVID-19) patients from the outbreak area of Lombardy, Italy, Nutr
Charoenngam, Shirvani, Holick, Vitamin D and its potential benefit for the COVID-19 pandemic, Endocr Pract
Charoenngam, Shirvani, Reddy, Vodopivec, Apovian et al., Association of vitamin D status with hospital morbidity and mortality in adult hospitalized COVID-19 patients, Endocr Pract
Dong, Du, Gardner, An interactive web-based dashboard to track COVID-19 in real time, Lancet Infect Dis
Gao, -D, Ding, Dong, Risk factors for severe and critically ill COVID-19 patients: a review, Allergy
Giannini, Passeri, Tripepi, Effectiveness of in-hospital cholecalciferol use on clinical outcomes in comorbid COVID-19 patients: a hypothesis-generating study, Nutrients
Griffin, Hewison, Hopkin, Perspective: vitamin D supplementation prevents rickets and acute respiratory infections when given as daily maintenance but not as intermittent bolus: implications for COVID-19, Clin Med
Griffin, Hewison, Hopkin, Vitamin D and COVID-19: evidence and recommendations for supplementation, R Soc Open Sci
Hastie, Mackay, Ho, Vitamin D concentrations and COVID-19 infection in UK Biobank, Diabetes Metab Syndr
Hastie, Pell, Sattar, Vitamin D and COVID-19 infection and mortality in UK Biobank, Eur J Nutr
Hernández, Nan, Fernandez-Ayala, Vitamin D status in hospitalized patients with SARS-CoV-2 infection, J Clin Endocrinol Metab
Higgins, Thomas, Chandler, Cochrane Handbook for Systematic Reviews of Interventions Version
Holick, The vitamin D deficiency pandemic: approaches for diagnosis, treatment and prevention, Rev Endocr Metab Disord
Hu, Guo, Zhou, Shi, Characteristics of SARS-CoV-2 and COVID-19, Nat Rev Microbiol
Jevalikar, Mithal, Singh, Lack of association of baseline 25-hydroxyvitamin D levels with disease severity and mortality in Indian patients hospitalized for COVID-19, Sci Rep
Kaufman, Niles, Kroll, Bi, Holick, SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels, PLoS One
Kazemi, Mohammadi, Aghababaee, Golzarand, Clark et al., Association of vitamin D status with SARS-CoV-2 infection or COVID-19 severity: a systematic review and metaanalysis, Adv Nutr
Liberati, Altman, Tetzlaff, The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration, Br Med J
Ling, Broad, Murphy, High-dose cholecalciferol booster therapy is associated with a reduced risk of mortality in patients with COVID-19: a cross-sectional multi-centre observational study, Nutrients
Liu, Sun, Wang, Zhang, Zhao et al., Low vitamin D status is associated with coronavirus disease 2019 outcomes: a systematic review and meta-analysis, Int J Infect Dis
Maghbooli, Sahraian, Ebrahimi, Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection, PLoS One
Mcguinness, Higgins, Risk-of-bias visualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments, Res Synthesis Methods
Meltzer, Best, Zhang, Vokes, Arora et al., Association of vitamin D status and other clinical characteristics with COVID-19 test results, JAMA Netw Open
Murai, Fernandes, Sales, Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: a randomized clinical trial, JAMA
Nikniaz, Akbarzadeh, Hosseinifard, Hosseini, The impact of vitamin D supplementation on mortality rate and clinical outcomes of COVID-19 patients: a systematic review and metaanalysis, medRxiv
Pal, Banerjee, Bhadada, Shetty, Singh et al., Vitamin D supplementation and clinical outcomes in COVID-19: a systematic review and meta-analysis, J Endocrinol Invest
Panagiotou, Tee, Ihsan, Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalized with COVID-19 are associated with greater disease severity, Clin Endocrinol
Petrelli, Luciani, Perego, Dognini, Colombelli et al., Therapeutic and prognostic role of vitamin D for COVID-19 infection: a systematic review and meta-analysis of 43 observational studies, J Steroid Biochem Mol Biol
Pizzini, Aichner, Sahanic, Impact of vitamin D deficiency on COVID-19 -A prospective analysis from the CovILD registry, Nutrients
Rawat, Roy, Maitra, Shankar, Khanna et al., Vitamin D supplementation and COVID-19 treatment: a systematic review and meta-analysis, Diabetes Metab Syndr
Rhodes, Subramanian, Laird, Griffin, Kenny, Perspective: vitamin D deficiency and COVID-19 severity -plausibly linked by latitude, ethnicity, impacts on cytokines, ACE2 and thrombosis, J Intern Med
Shah, Saxena, Mavalankar, Vitamin D supplementation, COVID-19 and disease severity: a meta-analysis, Q J Med
Sterne, Hernán, Reeves, ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions, Br Med J
Sterne, Savović, Page, RoB 2: a revised tool for assessing risk of bias in randomised trials, Br Med J
Szeto, Zucker, Lasota, Vitamin D status and COVID-19 clinical outcomes in hospitalized patients, Endocr Res
Tan, Ho, Kalimuddin, Cohort study to evaluate the effect of vitamin D, magnesium, and vitamin B(12) in combination on progression to severe outcomes in older patients with coronavirus (COVID-19), Nutrition
Vassiliou, Jahaj, Pratikaki, Orfanos, Dimopoulou et al., Low 25-hydroxyvitamin D levels on admission to the intensive care unit may predispose COVID-19 pneumonia patients to a higher 28-day mortality risk: a pilot study on a Greek ICU cohort, Nutrients
DOI record:
{
"DOI": "10.1002/dmrr.3517",
"ISSN": [
"1520-7552",
"1520-7560"
],
"URL": "http://dx.doi.org/10.1002/dmrr.3517",
"alternative-id": [
"10.1002/dmrr.3517"
],
"assertion": [
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Received",
"name": "received",
"order": 0,
"value": "2021-06-28"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Accepted",
"name": "accepted",
"order": 1,
"value": "2021-11-26"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Published",
"name": "published",
"order": 2,
"value": "2022-01-15"
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-0615-2534",
"affiliation": [
{
"name": "First Department of Propaedeutic Internal Medicine Diabetes Centre Medical School National and Kapodistrian University of Athens Laiko General Hospital Athens Greece"
}
],
"authenticated-orcid": false,
"family": "Tentolouris",
"given": "Nikolaos",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0001-5567-8044",
"affiliation": [
{
"name": "First Department of Propaedeutic Internal Medicine Diabetes Centre Medical School National and Kapodistrian University of Athens Laiko General Hospital Athens Greece"
}
],
"authenticated-orcid": false,
"family": "Samakidou",
"given": "Georgia",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "First Department of Propaedeutic Internal Medicine Diabetes Centre Medical School National and Kapodistrian University of Athens Laiko General Hospital Athens Greece"
}
],
"family": "Eleftheriadou",
"given": "Ioanna",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "First Department of Propaedeutic Internal Medicine Diabetes Centre Medical School National and Kapodistrian University of Athens Laiko General Hospital Athens Greece"
}
],
"family": "Tentolouris",
"given": "Anastasios",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Tameside and Glossop Integrated Care NHS Foundation Trust Ashton‐under‐Lyne UK"
}
],
"family": "Jude",
"given": "Edward B.",
"sequence": "additional"
}
],
"container-title": "Diabetes/Metabolism Research and Reviews",
"container-title-short": "Diabetes Metabolism Res",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"onlinelibrary.wiley.com"
]
},
"created": {
"date-parts": [
[
2021,
12,
29
]
],
"date-time": "2021-12-29T18:34:07Z",
"timestamp": 1640802847000
},
"deposited": {
"date-parts": [
[
2022,
7,
20
]
],
"date-time": "2022-07-20T12:49:41Z",
"timestamp": 1658321381000
},
"indexed": {
"date-parts": [
[
2022,
10,
26
]
],
"date-time": "2022-10-26T09:48:33Z",
"timestamp": 1666777713800
},
"is-referenced-by-count": 8,
"issue": "4",
"issued": {
"date-parts": [
[
2022,
1,
15
]
]
},
"journal-issue": {
"issue": "4",
"published-print": {
"date-parts": [
[
2022,
5
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://onlinelibrary.wiley.com/termsAndConditions#vor",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
1,
15
]
],
"date-time": "2022-01-15T00:00:00Z",
"timestamp": 1642204800000
}
},
{
"URL": "http://doi.wiley.com/10.1002/tdm_license_1.1",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
1,
15
]
],
"date-time": "2022-01-15T00:00:00Z",
"timestamp": 1642204800000
}
}
],
"link": [
{
"URL": "https://onlinelibrary.wiley.com/doi/pdf/10.1002/dmrr.3517",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://onlinelibrary.wiley.com/doi/full-xml/10.1002/dmrr.3517",
"content-type": "application/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://onlinelibrary.wiley.com/doi/pdf/10.1002/dmrr.3517",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "311",
"original-title": [],
"prefix": "10.1002",
"published": {
"date-parts": [
[
2022,
1,
15
]
]
},
"published-online": {
"date-parts": [
[
2022,
1,
15
]
]
},
"published-print": {
"date-parts": [
[
2022,
5
]
]
},
"publisher": "Wiley",
"reference": [
{
"DOI": "10.1038/s41579-020-00459-7",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_2_1"
},
{
"DOI": "10.1016/S1473-3099(20)30120-1",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_3_1"
},
{
"DOI": "10.1111/all.14657",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_4_1"
},
{
"DOI": "10.1016/j.eprac.2021.03.006",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_5_1"
},
{
"DOI": "10.1007/s11154-017-9424-1",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_6_1"
},
{
"DOI": "10.1002/dmrr.3375",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_7_1"
},
{
"DOI": "10.1016/j.dsx.2020.04.050",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_8_1"
},
{
"DOI": "10.1371/journal.pone.0239252",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_9_1"
},
{
"DOI": "10.1371/journal.pone.0239799",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_10_1"
},
{
"DOI": "10.1001/jamanetworkopen.2020.19722",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_11_1"
},
{
"DOI": "10.1111/cen.14276",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_12_1"
},
{
"DOI": "10.3390/nu12092775",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_13_1"
},
{
"article-title": "Vitamin D status and COVID‐19 clinical outcomes in hospitalized patients",
"author": "Szeto B",
"first-page": "1",
"journal-title": "Endocr Res",
"key": "e_1_2_11_14_1",
"year": "2020"
},
{
"DOI": "10.3390/nu12123773",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_15_1"
},
{
"DOI": "10.1016/j.mayocp.2021.01.001",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_16_1"
},
{
"DOI": "10.1016/j.eprac.2021.02.013",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_17_1"
},
{
"DOI": "10.1007/s00394-020-02372-4",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_18_1"
},
{
"DOI": "10.1016/j.jsbmb.2021.105883",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_19_1"
},
{
"DOI": "10.1016/j.ijid.2020.12.077",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_20_1"
},
{
"DOI": "10.1093/advances/nmab012",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_21_1"
},
{
"DOI": "10.1016/j.metabol.2021.154753",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_22_1"
},
{
"DOI": "10.3389/fnut.2021.660420",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_23_1"
},
{
"DOI": "10.1136/bmj.b2700",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_24_1"
},
{
"DOI": "10.1001/jama.2020.26848",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_25_1"
},
{
"DOI": "10.1016/j.jsbmb.2020.105751",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_26_1"
},
{
"DOI": "10.3390/nu12113377",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_27_1"
},
{
"DOI": "10.1016/j.nut.2020.111055",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_28_1"
},
{
"DOI": "10.1210/clinem/dgaa733",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_29_1"
},
{
"DOI": "10.1038/s41598-021-85809-y",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_30_1"
},
{
"DOI": "10.3390/nu12123799",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_31_1"
},
{
"DOI": "10.18632/aging.202307",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_32_1"
},
{
"article-title": "Cohort study to evaluate the effect of vitamin D, magnesium, and vitamin B(12) in combination on progression to severe outcomes in older patients with coronavirus (COVID‐19)",
"author": "Tan CW",
"first-page": "79",
"journal-title": "Nutrition",
"key": "e_1_2_11_33_1",
"year": "2020"
},
{
"DOI": "10.3390/nu13010219",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_34_1"
},
{
"DOI": "10.1136/bmj.l4898",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_35_1"
},
{
"article-title": "Risk‐of‐bias visualization (robvis): an R package and Shiny web app for visualizing risk‐of‐bias assessments",
"author": "McGuinness LA",
"journal-title": "Res Synthesis Methods",
"key": "e_1_2_11_36_1",
"year": "2020"
},
{
"DOI": "10.1136/bmj.i4919",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_37_1"
},
{
"author": "Higgins JPT",
"key": "e_1_2_11_38_1",
"volume-title": "Cochrane Handbook for Systematic Reviews of Interventions Version 6.2",
"year": "2021"
},
{
"key": "e_1_2_11_39_1",
"unstructured": "GRADEproGDT:GRADEpro Guideline Development Tool [Software].McMaster University and Evidence Prime 2021. Accessed 10/25/2021.https://gradepro.org/"
},
{
"DOI": "10.1098/rsos.201912",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_40_1"
},
{
"DOI": "10.1530/EJE-20-0665",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_41_1"
},
{
"DOI": "10.1016/j.hlc.2020.05.004",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_42_1"
},
{
"DOI": "10.7861/clinmed.2021-0035",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_43_1"
},
{
"author": "Bringhurst FR",
"first-page": "1211",
"key": "e_1_2_11_44_1",
"series-title": "Mineral Metabolism. Williams Textbook of Endocrinology",
"year": "2020"
},
{
"DOI": "10.1111/joim.13149",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_45_1"
},
{
"DOI": "10.1093/qjmed/hcab009",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_46_1"
},
{
"article-title": "The impact of vitamin D supplementation on mortality rate and clinical outcomes of COVID‐19 patients: a systematic review and meta‐analysis",
"author": "Nikniaz L",
"first-page": "21249219",
"journal-title": "medRxiv",
"key": "e_1_2_11_47_1",
"year": "2021"
},
{
"article-title": "Vitamin D supplementation and clinical outcomes in COVID‐19: a systematic review and meta‐analysis",
"author": "Pal R",
"first-page": "1",
"journal-title": "J Endocrinol Invest",
"key": "e_1_2_11_48_1",
"volume": "24",
"year": "2021"
},
{
"DOI": "10.1016/j.dsx.2021.102189",
"doi-asserted-by": "publisher",
"key": "e_1_2_11_49_1"
}
],
"reference-count": 48,
"references-count": 48,
"relation": {},
"resource": {
"primary": {
"URL": "https://onlinelibrary.wiley.com/doi/10.1002/dmrr.3517"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Endocrinology",
"Endocrinology, Diabetes and Metabolism",
"Internal Medicine"
],
"subtitle": [],
"title": "The effect of vitamin D supplementation on mortality and intensive care unit admission of COVID‐19 patients. A systematic review, meta‐analysis and meta‐regression",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1002/crossmark_policy",
"volume": "38"
}
