Vitamin D on COVID-19 Patients During the Pandemic, 2022. A Systematic Review and Meta-Analysis
et al., Current Research in Nutrition and Food Science Journal, doi:10.12944/CRNFSJ.11.1.3, Apr 2023
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
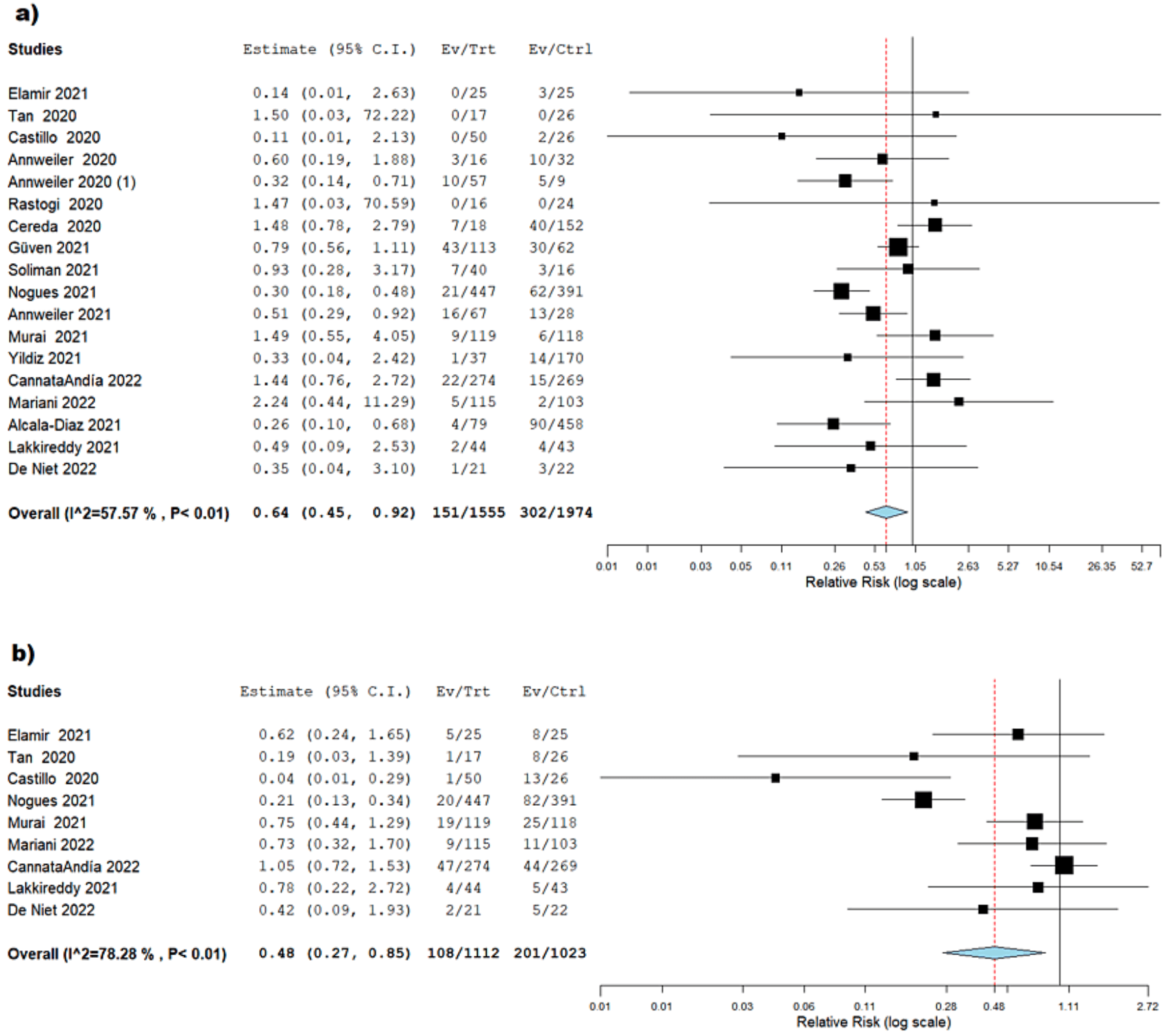
Systematic review and meta-analysis of 42 studies with 8,001 COVID-19 patients showing vitamin D deficiency associated with higher mortality, and vitamin D supplementation associated with lower mortality, ICU admission, mechanical ventilation, and length of hospitalization, especially when administered after COVID-19 diagnosis. Doses of 50,000 to 100,000IU showed the greatest benefits for mortality. The Figure 4 caption is incorrectly duplicated from Figure 5.
20 meta-analyses show significant improvements with vitamin D treatment for mortality1-14,
mechanical ventilation1,5,6,11,15-17 ,
ICU admission1,3,5,6,9,11,13,15-19 ,
hospitalization11,
severity2,4,5,10,20 , and
cases7,19,20 .
Currently there are 135 vitamin D treatment for COVID-19 studies, showing 39% lower mortality [32‑45%], 17% lower ventilation [-5‑35%], 45% lower ICU admission [28‑57%], 22% lower hospitalization [13‑30%], and 17% fewer cases [9‑25%].
|
risk of death, 36.0% lower, RR 0.64, p = 0.01.
|
|
risk of mechanical ventilation, 30.0% lower, RR 0.70, p < 0.001.
|
|
risk of ICU admission, 52.0% lower, RR 0.48, p = 0.02.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Shah et al., Does vitamin D supplementation reduce COVID-19 severity? - a systematic review, QJM: An International Journal of Medicine, doi:10.1093/qjmed/hcac040.
2.
Nikniaz et al., The impact of vitamin D supplementation on mortality rate and clinical outcomes of COVID-19 patients: A systematic review and meta-analysis, Pharmaceutical Sciences, doi:10.34172/PS.2021.13.
3.
Hosseini et al., Effects of Vitamin D Supplementation on COVID-19 Related Outcomes: A Systematic Review and Meta-Analysis, Nutrients, doi:10.3390/nu14102134.
4.
D’Ecclesiis et al., Vitamin D and SARS-CoV2 infection, severity and mortality: A systematic review and meta-analysis, PLOS ONE, doi:10.1371/journal.pone.0268396.
5.
Xie et al., Micronutrient perspective on COVID-19: Umbrella review and reanalysis of meta-analyses, Critical Reviews in Food Science and Nutrition, doi:10.1080/10408398.2023.2174948.
6.
Hariyanto et al., Vitamin D supplementation and Covid‐19 outcomes: A systematic review, meta‐analysis and meta‐regression, Reviews in Medical Virology, doi:10.1002/rmv.2269.
7.
Begum et al., The Role of Vitamin D in COVID-19 Survival and Prevention: A Meta-analysis, Sudan Journal of Medical Sciences, doi:10.18502/sjms.v19i1.15776.
8.
Jamilian et al., The role of vitamin D in outcomes of critical care in COVID-19 patients: Evidence from an umbrella meta-analysis of interventional and observational studies, Public Health Nutrition, doi:10.1017/S1368980024000934.
9.
Sobczak et al., Effect of Vitamin D3 Supplementation on Severe COVID-19: A Meta-Analysis of Randomized Clinical Trials, Nutrients, doi:10.3390/nu16101402.
10.
Petrelli et al., Therapeutic and prognostic role of vitamin D for COVID-19 infection: A systematic review and meta-analysis of 43 observational studies, The Journal of Steroid Biochemistry and Molecular Biology, doi:10.1016/j.jsbmb.2021.105883.
11.
Asla et al., Vitamin D on COVID-19 Patients During the Pandemic, 2022. A Systematic Review and Meta-Analysis, Current Research in Nutrition and Food Science Journal, doi:10.12944/CRNFSJ.11.1.3.
12.
Kow et al., The impact of vitamin D administration on mortality in COVID-19 patients: a systematic review and meta-analysis of randomized controlled trials, Inflammopharmacology, doi:10.1007/s10787-024-01564-2.
13.
Zhang et al., The impact of supplementing vitamin D through different methods on the prognosis of COVID-19 patients: a systematic review and meta-analysis, Frontiers in Nutrition, doi:10.3389/fnut.2024.1441847.
14.
Doustmohammadian et al., Impact of vitamin D supplementation on COVID-19 mortality: A systematic review and meta-analysis, Nutrition Clinique et Métabolisme, doi:10.1016/j.nupar.2025.12.001.
15.
Meng et al., The role of vitamin D in the prevention and treatment of SARS-CoV-2 infection: A meta-analysis of randomized controlled trials, Clinical Nutrition, doi:10.1016/j.clnu.2023.09.008.
16.
Yang et al., Therapeutic effects of vitamin D supplementation on COVID-19 aggravation: a systematic review and meta-analysis of randomized controlled trials, Frontiers in Pharmacology, doi:10.3389/fphar.2024.1367686.
17.
Szarpak et al., Vitamin D supplementation to treat SARS-CoV-2 positive patients. Evidence from meta-analysis, Cardiology Journal, doi:10.5603/CJ.a2021.0122.
18.
Tentolouris et al., The effect of vitamin D supplementation on mortality and intensive care unit admission of COVID-19 patients. A systematic review, meta-analysis and meta-regression, Diabetes/Metabolism Research and Reviews, doi:10.1002/dmrr.3517.
Asla et al., 25 Apr 2023, peer-reviewed, 8 authors.
Contact: dr_samar11@yahoo.com.
Vitamin D on COVID-19 Patients During the Pandemic, 2022. A Systematic Review and Meta-Analysis
Current Research in Nutrition and Food Science Journal, doi:10.12944/crnfsj.11.1.3
Numerous connections between the level of vitamin D (Vit-D) and the novel coronavirus disease -19 (COVID-19) have surfaced during the pandemic. So, we conducted this systematic review and meta-analysis to explore the effect of Vit-D deficiency and its supplementation on the clinical outcomes of COVID-19 patients. We looked for relevant articles in Cochrane Library, Scopus, Web Science, PubMed, and EBSCO up until the end of 2022. The Open Meta Analyst software was used to analyze the extracted data. We classified them into two main categories based on their objectives. First, the studies that evaluated the effects of Vit-D deficiency in patients, and lastly, the studies that evaluated Vit-D as a supplement, both on mortality rate, hospitalization duration, ICU admission rate, and mechanical ventilation rate. A total of 8001 COVID-19 patients from 42 studies were included. A high serum Vit-D concentration compared to those with lower levels was associated with a significantly lower mortality rate (RR = 1.5, 95% CI = 1.11: 2.02, p = 0.01). According to the estimated effect of 18 studies, those who took Vit-D supplements had a significantly lower mortality rate, hospitalization duration, ICU admission rate, and mechanical ventilation rate than those who did not. The group receiving Vit-D doses
Authors Contributions The manuscript has been read and approved by all the authors, that the requirements for authorship have been met, and that each author has substantial contributions to each of the three components mentioned below: 1. Concept and design of study or acquisition of data or analysis and interpretation of data.
2. Drafting the article or revising it critically for important intellectual content, and 3. Final approval of the version to be published.
Conflicts of interests The authors have declared no conflicts of interest.
References
A K B A R M R , W I B O W O A , P R A N A T A R , S E T I, a b u d i a w a n B . L o w s e r u m 25-hydroxyvitamin D (vitamin D) level is associated with susceptibility to COVID-19, severity, and mortality: a systematic review and meta-analysis, Frontiers in nutrition
Annweiler, Beaudenon, Gautier, Gonsard, Boucher et al., High-dose versus standard-dose vitamin D supplementation in older adults with COVID-19 (COVIT-TRIAL): A multicenter, open-label, randomized controlled superiority trial, PLoS Medicine
Annweiler, Corvaisier, Gautier, Dubée, Legrand et al., Vitamin D supplementation associated to better survival in hospitalized frail elderly COVID-19 patients: the GERIA-COVID quasi-experimental study, Nutrients
Annweiler, Hanotte, De L'eprevier, Sabatier, Lafaie et al., Vitamin D and survival in COVID-19 patients: A quasi-experimental study, The Journal of steroid biochemistry and molecular biology
Baktash, Hosack, Patel, Shah, Kandiah et al., Vitamin D status and outcomes for hospitalised older patients with COVID-19, Postgraduate medical journal
Bandeira, Lazaretti-Castro, Binkley, Clinical aspects of SARS-CoV-2 infection and vitamin D, Reviews in Endocrine and Metabolic Disorders
Bassatne, Basbous, Chakhtoura, El Zein, Rahme et al., The link between COVID-19 and VItamin D (VIVID): a systematic review and meta-analysis, Metabolism
Bilezikian, Bikle, Hewison, Lazaretti-Castro, Formenti et al., Mechanisms in endocrinology: vitamin D and COVID-19, European journal of endocrinology
Binkley, Ramamurthy, Krueger, Low vitamin D status: definition, prevalence, consequences, and correction, Endocrinology and Metabolism Clinics
Brice, Diamond, Antiviral activities of human host defense peptides, Current medicinal chemistry
Campi, Gennari, Merlotti, Mingiano, Frosali et al., Vitamin D and COVID-19 severity and related mortality: a prospective study in Italy, BMC Infectious Diseases
Cannata-Andía, Díaz-Sottolano, Fernández, Palomo-Antequera, Herrero-Puente et al., A single-oral bolus of 100,000 IU of cholecalciferol at hospital admission did not improve outcomes in the COVID-19 disease: the COVID-VIT-D-a randomised multicentre international clinical trial, BMC medicine
Castillo, Costa, Barrios, Díaz, Miranda et al., Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study, The Journal of steroid biochemistry and molecular biology
Cereda, Bogliolo, Lobascio, Barichella, Zecchinelli et al., Vitamin D supplementation and outcomes in coronavirus disease 2019 (COVID-19) patients from the outbreak area of Lombardy, Italy. Nutrition
Demir, Demir, Aygun, Vitamin D deficiency is associated with COVID-19 positivity and severity of the disease, Journal of Medical Virology
Elamir, Amir, Lim, Rana, Lopez et al., A randomized pilot study using calcitriol in hospitalized COVID-19 patients, Bone
Giannini, Passeri, Tripepi, Sella, Fusaro et al., Effectiveness of in-hospital cholecalciferol use on clinical outcomes in comorbid COVID-19 patients: a hypothesis-generating study, Nutrients
Gold, Sehayek, Gabrielli, Zhang, Mccusker et al., COVID-19 and comorbidities: a systematic review and meta-analysis, Postgraduate Medicine
Gombart, Pierre, Maggini, A Review of Micronutrients and the Immune System-Working in Harmony to Reduce the Risk of Infection, Nutrients
Grant, Lahore, Mcdonnell, Baggerly, French et al., Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths, Nutrients
Grant, Lahore, Rockwell, The benefits of vitamin D supplementation for athletes: better performance and reduced risk of COVID-19, Nutrients
Griffin, Hewison, Hopkin, Kenny, Quinton et al., Perspective: Vitamin D supplementation prevents rickets and acute respiratory infections when given as daily maintenance but not as intermittent bolus: implications for COVID-19, Clinical Medicine
Heaney, Guidelines for optimizing design and analysis of clinical studies of nutrient effects, Nutrition reviews
Higgins, Sterne, Savovic, Page, Hróbjartsson et al., A revised tool for assessing risk of bias in randomized trials, Cochrane database of systematic reviews
Higgins, Thompson, Deeks, Altman, Measuring inconsistency in metaanalyses, Bmj
Holick, Vitamin D Deficiency, New England Journal of Medicine
Iversen, Bjertnaes, Skudal, Patient evaluation of hospital outcomes: an analysis of open-ended comments from extreme clusters in a national survey, BMJ open
Jevalikar, Mithal, Singh, Sharma, Farooqui et al., Lack of association of baseline 25-hydroxyvitamin D levels with disease severity and mortality in Indian patients hospitalized for COVID-19, Scientific reports
Jolliffe, Jr, Sluyter, Aglipay, Aloia et al., Vitamin D supplementation to prevent acute respiratory infections: a systematic review and meta-analysis of aggregate data from randomised controlled trials, The lancet Diabetes & endocrinology
Kaufman, Niles, Kroll, Bi, Holick, SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels, PloS one
Ketha, Thacher, Oberhelman, Fischer, Singh et al., Comparison of the effect of daily versus bolus dose maternal vitamin D3 supplementation on the 24, 25-dihydroxyvitamin D3 to 25-hydroxyvitamin D3 ratio, Bone
Lakkireddy, Gadiga, Malathi, Karra, Raju et al., Impact of daily high dose oral vitamin D therapy on the inflammatory markers in patients with COVID 19 disease, Scientific Reports
Lei, Zhang, Cheng, Lee, Mechanisms of Action of Vitamin D as Supplemental Therapy for Pneumocystis Pneumonia, Antimicrobial Agents and Chemotherapy
Li, Huang, Zou, Yang, Hui et al., Epidemiology of COVID-19: A systematic review and meta-analysis of clinical characteristics, risk factors, and outcomes, Journal of Medical Virology
Liberati, Altman, Tetzlaff, Mulrow, Gøtzsche et al., The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration, Journal of clinical epidemiology
Ling, Broad, Murphy, Pappachan, Pardesi-Newton et al., High-dose cholecalciferol booster therapy is associated with a reduced risk of mortality in patients with COVID-19: a cross-sectional multi-centre observational study, Nutrients
Maghbooli, Sahraian, Ebrahimi, Pazoki, Kafan et al., Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection, PloS one
Mahdavi, A brief review of interplay between vitamin D and angiotensinconverting enzyme 2: Implications for a potential treatment for COVID-19, Reviews in medical virology
Mariani, Antonietti, Tajer, Ferder, Inserra et al., High-dose vitamin D versus placebo to prevent complications in COVID-19 patients: Multicentre randomized controlled clinical trial, PLoS ONE
Mariani, Giménez, Bergam, Tajer, Antonietti et al., Association between vitamin D deficiency and COVID-19 incidence, complications, and mortality in 46 countries: an ecological study, Health security
Meltzer, Best, Zhang, Vokes, Arora et al., Association of vitamin D status and other clinical characteristics with COVID-19 test results, JAMA network open
Mohammad, Ashraf, Emerging Role of Vitamin D and its Associated Molecules in Pathways Related to Pathogenesis of Thrombosis, Biomolecules
Munshi, Hussein, Toraih, Elshazli, Jardak et al., Vitamin D insufficiency as a potential culprit in critical COVID-19 patients, Journal of Medical Virology
Murai, Fernandes, Sales, Pinto, Goessler et al., Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: a randomized clinical trial, Jama
Niet, Trémège, Coffiner, Rousseau, Calmes et al., Positive effects of vitamin D supplementation in patients hospitalized for COVID-19: a randomized, double-blind, placebocontrolled trial, Nutrients
Nogues, Ovejero, Pineda-Moncusí, Bouillon, Arenas et al., Calcifediol treatment and COVID-19r e l a t e d o u t c o m e s, T h e J o u r n a l o f Clinical Endocrinology & Metabolism
Nogues, Ovejero, Pineda-Moncusí, Bouillon, Arenas et al., Calcifediol treatment and COVID-19r e l a t e d o u t c o m e s, T h e J o u r n a l o f Clinical Endocrinology & Metabolism
Pacha, Sallman, Evans, COVID-19: a case for inhibiting IL-17?, Nature Reviews Immunology
Pal, Bhansali, COVID-19, diabetes mellitus and ACE2: the conundrum, Diabetes research and clinical practice
Pal, Ram, Zohmangaihi, Biswas, Suri et al., High prevalence of hypocalcemia in non-severe COVID-19 patients: a retrospective case-control study, Frontiers in medicine
Pereira, Damascena, Azevedo, De Almeida Oliveira, Da et al., Vitamin D deficiency aggravates COVID-19: systematic review and metaanalysis, Critical Reviews in Food Science and Nutrition
Petrilli, Jones, Yang, Rajagopalan, Donnell et al., Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study, BMJ
Radujkovic, Hippchen, Tiwari-Heckler, Dreher, Boxberger, Vitamin D deficiency and outcome of COVID-19 patients, Nutrients
Rake, Gilham, Bukasa, Ostler, Newton et al., High-dose oral vitamin D supplementation and mortality in people aged 65-84 years: the VIDAL cluster feasibility RCT of open versus double-blind individual randomisation, Health Technology Assessment
Rastogi, Bhansali, Khare, Suri, Yaddanapudi et al., Short term, high-dose vitamin D supplementation for COVID-19 disease: A randomised, p l a c e b o -c o n t r o l l e d , s t u d y ( S H A D E study), Postgraduate Medical Journal
Raucci, Mansour, Casillo, Saviano, Caso et al., Interleukin-17A (IL-17A), a key molecule of innate and adaptive immunity, and its potential involvement in COVID-19-related thrombotic and vascular mechanisms, Autoimmunity Reviews
Reis, Fernandes, Sales, Santos, Santos et al., Influence of vitamin D status on hospital length of stay and prognosis in hospitalized patients with moderate to severe COVID-19: a multicenter prospective cohort study, American Journal of Clinical Nutrition
Slim, Nini, Forestier, Kwiatkowski, Panis et al., Methodological i n d e x f o r n o n -r a n d o m i z e d s t u d i e s (MINORS): development and validation of a new instrument, ANZ journal of surgery
Soliman, Abdelaziz, Fathy, Impact of Vitamin D Therapy on the Progress COVID-19: Six Weeks Follow-Up Study of Vitamin D Deficient Elderly Diabetes Patients, Proceedings of Singapore Healthcare
Suhail, Zajac, Fossum, Lowater, Mccracken et al., Role of Oxidative Stress on SARS-CoV (SARS) and SARS-CoV-2 (COVID-19) Infection: A Review, The Protein Journal
Teshome, Adane, Girma, Mekonnen, The impact of vitamin D level on COVID-19 infection: systematic review and meta-analysis, Frontiers in public health
Torres, Casado, Vigón, Rodríguez-Mora, Mateos et al., Changes in the immune response against SARS-CoV-2 in individuals with severe COVID-19 treated with high dose of vitamin D, Biomedicine & Pharmacotherapy
Vassiliou, Jahaj, Pratikaki, Keskinidou, Detsika et al., Vitamin D deficiency correlates with a reduced number of natural killer cells in intensive care unit (ICU) and non-ICU patients with COVID-19 pneumonia, Hellenic Journal of Cardiology
Weir, Thenappan, Bhargava, Chen, Does vitamin D deficiency increase the severity of COVID-19?, Clinical Medicine
Who, Coronavirus (COVID-19) dashboard
Yildiz, Senel, Kavurgaci, Ozturk, Ozturk, The prognostic significance of vitamin D deficiency in patients with COVID-19 pneumonia, Bratislavske Lekarske Listy
Zhou, Du, Fan, Liu, Liu, Clinical course and risk factors for mortality of adult inpatients with COVID19 in Wuhan, China: a retrospective cohort study, Lancet
Zou, Yan, Shu, Gao, Sun et al., Angiotensin-converting enzyme 2 protects from lethal avian influenza A H5N1 infections, Nature communications
DOI record:
{
"DOI": "10.12944/crnfsj.11.1.3",
"ISSN": [
"2322-0007",
"2347-467X"
],
"URL": "http://dx.doi.org/10.12944/CRNFSJ.11.1.3",
"abstract": "<jats:p>Numerous connections between the level of vitamin D (Vit-D) and the novel coronavirus disease -19 (COVID-19) have surfaced during the pandemic. So, we conducted this systematic review and meta-analysis to explore the effect of Vit-D deficiency and its supplementation on the clinical outcomes of COVID-19 patients. We looked for relevant articles in Cochrane Library, Scopus, Web Science, PubMed, and EBSCO up until the end of 2022. The Open Meta Analyst software was used to analyze the extracted data. We classified them into two main categories based on their objectives. First, the studies that evaluated the effects of Vit-D deficiency in patients, and lastly, the studies that evaluated Vit-D as a supplement, both on mortality rate, hospitalization duration, ICU admission rate, and mechanical ventilation rate. A total of 8001 COVID-19 patients from 42 studies were included. A high serum Vit-D concentration compared to those with lower levels was associated with a significantly lower mortality rate (RR = 1.5, 95% CI = 1.11: 2.02, p = 0.01). According to the estimated effect of 18 studies, those who took Vit-D supplements had a significantly lower mortality rate, hospitalization duration, ICU admission rate, and mechanical ventilation rate than those who did not. The group receiving Vit-D doses between 50 000 to 100 000 IU had a significantly better clinical outcome compared to lower and higher doses. COVID-19 patients with normal Vit-D levels had significantly lower death rates than those with hypovitaminosis. Vit-D supplements in COVID-19 significantly improved clinical outcomes. Vit-D supplementation between 50 000 to 100 000 IU, in patients with COVID-19 significantly outperformed other doses in terms of mortality.</jats:p>",
"assertion": [
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Published Print",
"name": "published_print",
"order": 0,
"value": "2023-4-25"
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-4837-5445",
"affiliation": [
{
"name": "1Faculty of Human Medicine, Zagazig University, Zagazig City, Sharkia, Egypt."
}
],
"authenticated-orcid": false,
"family": "Asla",
"given": "Moamen Mostafa",
"sequence": "first"
},
{
"affiliation": [
{
"name": "1Faculty of Human Medicine, Zagazig University, Zagazig City, Sharkia, Egypt."
}
],
"family": "Nawar",
"given": "Asmaa Ahmed",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6722-4365",
"affiliation": [
{
"name": "2Faculty of Medicine, Kafrelsheikh University, Kafrelsheikh, Egypt."
}
],
"authenticated-orcid": false,
"family": "Elsayed",
"given": "Esraa",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6263-0812",
"affiliation": [
{
"name": "5Department of Public Health and Community Medicine, Faculty of Medicine, Zagazig University, Zagazig City, Sharkia, Egypt."
}
],
"authenticated-orcid": false,
"family": "Farahat",
"given": "Ramadan Abdelmoez",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5905-5271",
"affiliation": [
{
"name": "6Membership at the Royal Colleague of General Practitioners[INT], London, United Kingdom."
}
],
"authenticated-orcid": false,
"family": "Abdulgadir",
"given": "Ayah",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7568-6383",
"affiliation": [
{
"name": "1Faculty of Human Medicine, Zagazig University, Zagazig City, Sharkia, Egypt."
}
],
"authenticated-orcid": false,
"family": "Alsharabasy",
"given": "Mostafa Abdullah",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9050-3888",
"affiliation": [
{
"name": "7Department of Mental Health Primary Care, Nova University, Lisbon"
}
],
"authenticated-orcid": false,
"family": "Elshahawy",
"given": "sraa Mohamed",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9475-6372",
"affiliation": [
{
"name": "4Faculty of Pharmacy, Zagazig University, Zagazig City, Sharkia, Egypt."
}
],
"authenticated-orcid": false,
"family": "Amer",
"given": "Samar A.",
"sequence": "additional"
}
],
"container-title": "Current Research in Nutrition and Food Science Journal",
"container-title-short": "Curr Res Nutr Food Sci",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
4,
27
]
],
"date-time": "2023-04-27T08:02:28Z",
"timestamp": 1682582548000
},
"deposited": {
"date-parts": [
[
2023,
4,
27
]
],
"date-time": "2023-04-27T08:02:59Z",
"timestamp": 1682582579000
},
"indexed": {
"date-parts": [
[
2024,
3,
2
]
],
"date-time": "2024-03-02T03:19:34Z",
"timestamp": 1709349574106
},
"is-referenced-by-count": 1,
"issue": "1",
"issued": {
"date-parts": [
[
2023,
4,
25
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2023,
4,
25
]
]
},
"published-print": {
"date-parts": [
[
2023,
4,
25
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
4,
24
]
],
"date-time": "2023-04-24T00:00:00Z",
"timestamp": 1682294400000
}
}
],
"link": [
{
"URL": "https://www.foodandnutritionjournal.org/volume11number1/vitamin-d-on-covid-19-patients-during-the-pandemic-2022-a-systematic-review-and-meta-analysis/",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "5089",
"original-title": [],
"page": "37-60",
"prefix": "10.12944",
"published": {
"date-parts": [
[
2023,
4,
25
]
]
},
"published-online": {
"date-parts": [
[
2023,
4,
25
]
]
},
"published-print": {
"date-parts": [
[
2023,
4,
25
]
]
},
"publisher": "Enviro Research Publishers",
"reference": [
{
"key": "ref0",
"unstructured": "1.\tWHO. Coronavirus (COVID-19) dashboard. s. f."
},
{
"DOI": "10.22541/au.160373214.44393120/v1",
"doi-asserted-by": "publisher",
"key": "ref1",
"unstructured": "2.\tRamasamy S, Subbian S. Critical Determinants of Cytokine Storm and Type I Interferon Response in COVID-19 Pathogenesis. Clinical Microbiology Reviews. 2021;34."
},
{
"DOI": "10.1016/s0140-6736(20)30566-3",
"doi-asserted-by": "publisher",
"key": "ref2",
"unstructured": "3.\tZhou F. Y u T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054-62."
},
{
"DOI": "10.1002/jmv.26424",
"doi-asserted-by": "crossref",
"key": "ref3",
"unstructured": "4.\tLi J, Huang DQ, Zou B, Yang H, Hui WZ, Rui F, et al. Epidemiology of COVID‐19: A systematic review and meta‐analysis of clinical characteristics, risk factors, and outcomes. Journal of Medical Virology. 2021;93:1449-58."
},
{
"DOI": "10.1080/00325481.2020.1786964",
"doi-asserted-by": "publisher",
"key": "ref4",
"unstructured": "5.\tGold MS, Sehayek D, Gabrielli S, Zhang X, McCusker C, Ben-Shoshan M. COVID-19 and comorbidities: a systematic review and meta-analysis. Postgraduate Medicine. 2020;132:749-55."
},
{
"DOI": "10.1136/bmj.m1966",
"doi-asserted-by": "publisher",
"key": "ref5",
"unstructured": "6.\tPetrilli CM, Jones SA, Yang J, Rajagopalan H, O’Donnell L, Chernyak Y, et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ. 2020:m1966."
},
{
"DOI": "10.1002/jmv.26360",
"doi-asserted-by": "publisher",
"key": "ref6",
"unstructured": "7.\tMunshi R, Hussein MH, Toraih EA, Elshazli RM, Jardak C, Sultana N, et al. Vitamin D insufficiency as a potential culprit in critical COVID‐19 patients. Journal of Medical Virology. 2021;93:733-40."
},
{
"DOI": "10.1080/10408398.2020.1841090",
"doi-asserted-by": "publisher",
"key": "ref7",
"unstructured": "8.\tPereira M, Dantas Damascena A, Galvão Azevedo LM, de Almeida Oliveira T, da Mota Santana J. Vitamin D deficiency aggravates COVID-19: systematic review and meta-analysis. Critical Reviews in Food Science and Nutrition. 2022;62:1308-16."
},
{
"DOI": "10.1056/NEJMra070553",
"doi-asserted-by": "crossref",
"key": "ref8",
"unstructured": "9.\tHolick MF. Vitamin D Deficiency. New England Journal of Medicine. 2007;357:266-81."
},
{
"DOI": "10.3390/nu12040988",
"doi-asserted-by": "publisher",
"key": "ref9",
"unstructured": "10.\tGrant W, Lahore H, McDonnell S, Baggerly C, French C, Aliano J, et al. Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths. Nutrients. 2020;12:988."
},
{
"DOI": "10.3390/nu12010236",
"doi-asserted-by": "publisher",
"key": "ref10",
"unstructured": "11.\tGombart AF, Pierre A, Maggini S. A Review of Micronutrients and the Immune System–Working in Harmony to Reduce the Risk of Infection. Nutrients. 2020;12:236."
},
{
"DOI": "10.7861/clinmed.2020-0301",
"doi-asserted-by": "publisher",
"key": "ref11",
"unstructured": "12.\tWeir EK, Thenappan T, Bhargava M, Chen Y. Does vitamin D deficiency increase the severity of COVID-19? Clinical Medicine. 2020;20:e107-8."
},
{
"DOI": "10.3390/biom9110649",
"doi-asserted-by": "publisher",
"key": "ref12",
"unstructured": "13.\tMohammad, Mishra, Ashraf. Emerging Role of Vitamin D and its Associated Molecules in Pathways Related to Pathogenesis of Thrombosis. Biomolecules. 2019;9:649."
},
{
"DOI": "10.1128/AAC.01226-17",
"doi-asserted-by": "crossref",
"key": "ref13",
"unstructured": "14.\tLei G-S, Zhang C, Cheng B-H, Lee C-H. Mechanisms of Action of Vitamin D as Supplemental Therapy for Pneumocystis Pneumonia. Antimicrobial Agents and Chemotherapy. 2017;61."
},
{
"DOI": "10.1007/s10930-020-09935-8",
"doi-asserted-by": "publisher",
"key": "ref14",
"unstructured": "15.\tSuhail S, Zajac J, Fossum C, Lowater H, McCracken C, Severson N, et al. Role of Oxidative Stress on SARS-CoV (SARS) and SARS-CoV-2 (COVID-19) Infection: A Review. The Protein Journal. 2020;39:644-56."
},
{
"DOI": "10.1016/j.jclinepi.2009.06.006",
"doi-asserted-by": "publisher",
"key": "ref15",
"unstructured": "16.\tLiberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Journal of clinical epidemiology. 2009;62:e1-34."
},
{
"DOI": "10.1186/s13643-016-0259-8",
"doi-asserted-by": "publisher",
"key": "ref16",
"unstructured": "17.\tHiggins JPT, Sterne JAC, Savovic J, Page MJ, Hróbjartsson A, Boutron I, et al. A revised tool for assessing risk of bias in randomized trials. Cochrane database of systematic reviews. 2016;10:29-31."
},
{
"DOI": "10.1046/j.1445-2197.2003.02748.x",
"doi-asserted-by": "publisher",
"key": "ref17",
"unstructured": "18.\tSlim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non‐randomized studies (MINORS): development and validation of a new instrument. ANZ journal of surgery. 2003;73:712-6."
},
{
"DOI": "10.1136/bmj.327.7414.557",
"doi-asserted-by": "crossref",
"key": "ref18",
"unstructured": "19.\tHiggins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Bmj. 2003;327:557-60."
},
{
"DOI": "10.1016/j.jsbmb.2020.105751",
"doi-asserted-by": "publisher",
"key": "ref19",
"unstructured": "20.\tCastillo ME, Costa LME, Barrios JMV, Díaz JFA, Miranda JL, Bouillon R, et al. Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study. The Journal of steroid biochemistry and molecular biology. 2020;203:105751."
},
{
"DOI": "10.1186/s13063-021-05073-3",
"doi-asserted-by": "publisher",
"key": "ref20",
"unstructured": "21.\tMariani J, Antonietti L, Tajer C, Ferder L, Inserra F, Cunto MS, et al. High-dose vitamin D versus placebo to prevent complications in COVID-19 patients: Multicentre randomized controlled clinical trial. PLoS ONE. 2022;17:1-16."
},
{
"DOI": "10.1001/jama.2020.26848",
"doi-asserted-by": "publisher",
"key": "ref21",
"unstructured": "22.\tMurai IH, Fernandes AL, Sales LP, Pinto AJ, Goessler KF, Duran CSC, et al. Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: a randomized clinical trial. Jama. 2021;325:1053-60."
},
{
"DOI": "10.3390/nu14153048",
"doi-asserted-by": "publisher",
"key": "ref22",
"unstructured": "23.\tDe Niet S, Trémège M, Coffiner M, Rousseau A-F, Calmes D, Frix A-N, et al. Positive effects of vitamin D supplementation in patients hospitalized for COVID-19: a randomized, double-blind, placebo-controlled trial. Nutrients. 2022;14:3048."
},
{
"DOI": "10.1016/j.biopha.2022.112965",
"doi-asserted-by": "crossref",
"key": "ref23",
"unstructured": "24.\tTorres M, Casado G, Vigón L, Rodríguez-Mora S, Mateos E, Ramos-Martín F, et al. Changes in the immune response against SARS-CoV-2 in individuals with severe COVID-19 treated with high dose of vitamin D. Biomedicine & Pharmacotherapy. 2022;150:112965."
},
{
"DOI": "10.1186/s12916-022-02290-8",
"doi-asserted-by": "publisher",
"key": "ref24",
"unstructured": "25.\tCannata-Andía JB, Díaz-Sottolano A, Fernández P, Palomo-Antequera C, Herrero-Puente P, Mouzo R, et al. A single-oral bolus of 100,000 IU of cholecalciferol at hospital admission did not improve outcomes in the COVID-19 disease: the COVID-VIT-D—a randomised multicentre international clinical trial. BMC medicine. 2022;20:1-13."
},
{
"DOI": "10.1371/journal.pmed.1003999",
"doi-asserted-by": "crossref",
"key": "ref25",
"unstructured": "26.\tAnnweiler C, Beaudenon M, Gautier J, Gonsard J, Boucher S, Chapelet G, et al. High-dose versus standard-dose vitamin D supplementation in older adults with COVID-19 (COVIT-TRIAL): A multicenter, open-label, randomized controlled superiority trial. PLoS Medicine. 2022;19:1-18."
},
{
"DOI": "10.1038/s41598-021-97181-y",
"doi-asserted-by": "publisher",
"key": "ref26",
"unstructured": "27.\tLakkireddy M, Gadiga SG, Malathi RD, Karra ML, Raju ISSVPM, Ragini, et al. Impact of daily high dose oral vitamin D therapy on the inflammatory markers in patients with COVID 19 disease. Scientific Reports. 2021;11:1-8."
},
{
"DOI": "10.1177/20101058211041405",
"doi-asserted-by": "publisher",
"key": "ref27",
"unstructured": "28.\tSoliman AR, Abdelaziz TS, Fathy A. Impact of Vitamin D Therapy on the Progress COVID-19: Six Weeks Follow-Up Study of Vitamin D Deficient Elderly Diabetes Patients. Proceedings of Singapore Healthcare. 2021;0:1-5."
},
{
"DOI": "10.1136/postgradmedj-2020-139065",
"doi-asserted-by": "publisher",
"key": "ref28",
"unstructured": "29.\tRastogi A, Bhansali A, Khare N, Suri V, Yaddanapudi N, Sachdeva N, et al. Short term, high-dose vitamin D supplementation for COVID-19 disease: A randomised, placebo-controlled, study (SHADE study). Postgraduate Medical Journal. 2022;98:87-90."
},
{
"DOI": "10.1016/j.bone.2021.116175",
"doi-asserted-by": "publisher",
"key": "ref29",
"unstructured": "30.\tElamir YM, Amir H, Lim S, Rana YP, Lopez CG, Feliciano NV, et al. A randomized pilot study using calcitriol in hospitalized COVID-19 patients. Bone. 2022;154."
},
{
"DOI": "10.1210/clinem/dgab405",
"doi-asserted-by": "publisher",
"key": "ref30",
"unstructured": "31.\tNogues X, Ovejero D, Pineda-Moncusí M, Bouillon R, Arenas D, Pascual J, et al. Calcifediol treatment and COVID-19–related outcomes. The Journal of Clinical Endocrinology & Metabolism. 2021;106:e4017-27."
},
{
"DOI": "10.4149/bll_2021_119",
"doi-asserted-by": "publisher",
"key": "ref31",
"unstructured": "32.\tYildiz M, Senel MU, Kavurgaci S, Ozturk FE, Ozturk A. The prognostic significance of vitamin D deficiency in patients with COVID-19 pneumonia. Bratislavske Lekarske Listy. 2021;122:744-7."
},
{
"DOI": "10.1038/s41598-021-85809-y",
"doi-asserted-by": "crossref",
"key": "ref32",
"unstructured": "33.\tJevalikar G, Mithal A, Singh A, Sharma R, Farooqui KJ, Mahendru S, et al. Lack of association of baseline 25-hydroxyvitamin D levels with disease severity and mortality in Indian patients hospitalized for COVID-19. Scientific reports. 2021;11:1-8."
},
{
"DOI": "10.1093/ajcn/nqab227",
"doi-asserted-by": "publisher",
"key": "ref33",
"unstructured": "34.\tReis BZ, Fernandes AL, Sales LP, Santos MD, Dos Santos CC, Pinto AJ, et al. Influence of vitamin D status on hospital length of stay and prognosis in hospitalized patients with moderate to severe COVID-19: a multicenter prospective cohort study. American Journal of Clinical Nutrition. 2021;114:598-604."
},
{
"DOI": "10.1016/j.hjc.2020.11.011",
"doi-asserted-by": "publisher",
"key": "ref34",
"unstructured": "35.\tVassiliou AG, Jahaj E, Pratikaki M, Keskinidou C, Detsika M, Grigoriou E, et al. Vitamin D deficiency correlates with a reduced number of natural killer cells in intensive care unit (ICU) and non-ICU patients with COVID-19 pneumonia. Hellenic Journal of Cardiology. 2021;62:381."
},
{
"DOI": "10.1210/clinem/dgab405",
"doi-asserted-by": "publisher",
"key": "ref35",
"unstructured": "36.\tNogues X, Ovejero D, Pineda-Moncusí M, Bouillon R, Arenas D, Pascual J, et al. Calcifediol treatment and COVID-19–related outcomes. The Journal of Clinical Endocrinology & Metabolism. 2021;106:e4017-27."
},
{
"DOI": "10.1186/s12879-021-06281-7",
"doi-asserted-by": "publisher",
"key": "ref36",
"unstructured": "37.\tCampi I, Gennari L, Merlotti D, Mingiano C, Frosali A, Giovanelli L, et al. Vitamin D and COVID-19 severity and related mortality: a prospective study in Italy. BMC Infectious Diseases. 2021;21:1-13."
},
{
"DOI": "10.1002/jmv.26832",
"doi-asserted-by": "publisher",
"key": "ref37",
"unstructured": "38.\tDemir M, Demir F, Aygun H. Vitamin D deficiency is associated with COVID-19 positivity and severity of the disease. Journal of Medical Virology. 2021;93:2992-9."
},
{
"DOI": "10.3390/nu12092757",
"doi-asserted-by": "publisher",
"key": "ref38",
"unstructured": "39.\tRadujkovic A, Hippchen T, Tiwari-Heckler S, Dreher S, Boxberger M, Merle U. Vitamin D deficiency and outcome of COVID-19 patients. Nutrients. 2020;12:2757."
},
{
"DOI": "10.1089/hs.2020.0137",
"doi-asserted-by": "publisher",
"key": "ref39",
"unstructured": "40.\tMariani J, Giménez VMM, Bergam I, Tajer C, Antonietti L, Inserra F, et al. Association between vitamin D deficiency and COVID-19 incidence, complications, and mortality in 46 countries: an ecological study. Health security. 2021;19:302-8."
},
{
"DOI": "10.1016/j.metabol.2021.154753",
"doi-asserted-by": "crossref",
"key": "ref40",
"unstructured": "41.\tBassatne A, Basbous M, Chakhtoura M, El Zein O, Rahme M, Fuleihan GE-H. The link between COVID-19 and VItamin D (VIVID): a systematic review and meta-analysis. Metabolism. 2021;119:154753."
},
{
"DOI": "10.3389/fpubh.2021.624559",
"doi-asserted-by": "publisher",
"key": "ref41",
"unstructured": "42.\tTeshome A, Adane A, Girma B, Mekonnen ZA. The impact of vitamin D level on COVID-19 infection: systematic review and meta-analysis. Frontiers in public health. 2021;9:624559."
},
{
"DOI": "10.3389/fnut.2021.660420",
"doi-asserted-by": "publisher",
"key": "ref42",
"unstructured": "43.\tAkbar MR, Wibowo A, Pranata R, Setiabudiawan B. Low serum 25-hydroxyvitamin D (vitamin D) level is associated with susceptibility to COVID-19, severity, and mortality: a systematic review and meta-analysis. Frontiers in nutrition. 2021;8:660420."
},
{
"DOI": "10.1371/journal.pone.0239252",
"doi-asserted-by": "publisher",
"key": "ref43",
"unstructured": "44.\tKaufman HW, Niles JK, Kroll MH, Bi C, Holick MF. SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels. PloS one. 2020;15:e0239252."
},
{
"DOI": "10.1111/nure.12090",
"doi-asserted-by": "publisher",
"key": "ref44",
"unstructured": "45.\tHeaney RP. Guidelines for optimizing design and analysis of clinical studies of nutrient effects. Nutrition reviews. 2014;72:48-54."
},
{
"DOI": "10.3389/fmed.2020.590805",
"doi-asserted-by": "publisher",
"key": "ref45",
"unstructured": "46.\tPal R, Ram S, Zohmangaihi D, Biswas I, Suri V, Yaddanapudi LN, et al. High prevalence of hypocalcemia in non-severe COVID-19 patients: a retrospective case-control study. Frontiers in medicine. 2021;7:590805."
},
{
"DOI": "10.1001/jamanetworkopen.2020.19722",
"doi-asserted-by": "publisher",
"key": "ref46",
"unstructured": "47.\tMeltzer DO, Best TJ, Zhang H, Vokes T, Arora V, Solway J. Association of vitamin D status and other clinical characteristics with COVID-19 test results. JAMA network open. 2020;3:e2019722-e2019722."
},
{
"DOI": "10.3390/nu12123741",
"doi-asserted-by": "publisher",
"key": "ref47",
"unstructured": "48.\tGrant WB, Lahore H, Rockwell MS. The benefits of vitamin D supplementation for athletes: better performance and reduced risk of COVID-19. Nutrients. 2020;12:3741."
},
{
"DOI": "10.2174/0929867326666190805151654",
"doi-asserted-by": "publisher",
"key": "ref48",
"unstructured": "49.\tBrice DC, Diamond G. Antiviral activities of human host defense peptides. Current medicinal chemistry. 2020;27:1420-43."
},
{
"DOI": "10.1016/j.autrev.2020.102572",
"doi-asserted-by": "publisher",
"key": "ref49",
"unstructured": "50.\tRaucci F, Mansour AA, Casillo GM, Saviano A, Caso F, Scarpa R, et al. Interleukin-17A (IL-17A), a key molecule of innate and adaptive immunity, and its potential involvement in COVID-19-related thrombotic and vascular mechanisms. Autoimmunity Reviews. 2020;19:102572."
},
{
"DOI": "10.1038/s41577-020-0328-z",
"doi-asserted-by": "publisher",
"key": "ref50",
"unstructured": "51.\tPacha O, Sallman MA, Evans SE. COVID-19: a case for inhibiting IL-17? Nature Reviews Immunology. 2020;20:345-6."
},
{
"DOI": "10.1530/eje-20-0665",
"doi-asserted-by": "publisher",
"key": "ref51",
"unstructured": "52.\tBilezikian JP, Bikle D, Hewison M, Lazaretti-Castro M, Formenti AM, Gupta A, et al. Mechanisms in endocrinology: vitamin D and COVID-19. European journal of endocrinology. 2020;183:R133-47."
},
{
"DOI": "10.1002/rmv.2119",
"doi-asserted-by": "publisher",
"key": "ref52",
"unstructured": "53.\tMalek Mahdavi A. A brief review of interplay between vitamin D and angiotensin‐converting enzyme 2: Implications for a potential treatment for COVID‐19. Reviews in medical virology. 2020;30:e2119."
},
{
"DOI": "10.1016/j.diabres.2020.108132",
"doi-asserted-by": "publisher",
"key": "ref53",
"unstructured": "54.\tPal R, Bhansali A. COVID-19, diabetes mellitus and ACE2: the conundrum. Diabetes research and clinical practice. 2020;162."
},
{
"DOI": "10.1038/ncomms4594",
"doi-asserted-by": "publisher",
"key": "ref54",
"unstructured": "55.\tZou Z, Yan Y, Shu Y, Gao R, Sun Y, Li X, et al. Angiotensin-converting enzyme 2 protects from lethal avian influenza A H5N1 infections. Nature communications. 2014;5:1-7."
},
{
"DOI": "10.1136/postgradmedj-2020-138712",
"doi-asserted-by": "publisher",
"key": "ref55",
"unstructured": "56.\tBaktash V, Hosack T, Patel N, Shah S, Kandiah P, Van den Abbeele K, et al. Vitamin D status and outcomes for hospitalised older patients with COVID-19. Postgraduate medical journal. 2021;97:442-7."
},
{
"DOI": "10.3390/nu13010219",
"doi-asserted-by": "publisher",
"key": "ref56",
"unstructured": "57.\tGiannini S, Passeri G, Tripepi G, Sella S, Fusaro M, Arcidiacono G, et al. Effectiveness of in-hospital cholecalciferol use on clinical outcomes in comorbid COVID-19 patients: a hypothesis-generating study. Nutrients. 2021;13:219."
},
{
"DOI": "10.3390/nu12123799",
"doi-asserted-by": "publisher",
"key": "ref57",
"unstructured": "58.\tLing SF, Broad E, Murphy R, Pappachan JM, Pardesi-Newton S, Kong M-F, et al. High-dose cholecalciferol booster therapy is associated with a reduced risk of mortality in patients with COVID-19: a cross-sectional multi-centre observational study. Nutrients. 2020;12:3799."
},
{
"DOI": "10.1016/j.jsbmb.2020.105771",
"doi-asserted-by": "crossref",
"key": "ref58",
"unstructured": "59.\tAnnweiler C, Hanotte B, de l’Eprevier CG, Sabatier J-M, Lafaie L, Célarier T. Vitamin D and survival in COVID-19 patients: A quasi-experimental study. The Journal of steroid biochemistry and molecular biology. 2020;204:105771."
},
{
"DOI": "10.3390/nu12113377",
"doi-asserted-by": "publisher",
"key": "ref59",
"unstructured": "60.\tAnnweiler G, Corvaisier M, Gautier J, Dubée V, Legrand E, Sacco G, et al. Vitamin D supplementation associated to better survival in hospitalized frail elderly COVID-19 patients: the GERIA-COVID quasi-experimental study. Nutrients. 2020;12:3377."
},
{
"DOI": "10.1016/j.nut.2020.111055",
"doi-asserted-by": "publisher",
"key": "ref60",
"unstructured": "61.\tCereda E, Bogliolo L, Lobascio F, Barichella M, Zecchinelli AL, Pezzoli G, et al. Vitamin D supplementation and outcomes in coronavirus disease 2019 (COVID-19) patients from the outbreak area of Lombardy, Italy. Nutrition (Burbank, Los Angeles County, Calif). 2021;82:111055."
},
{
"DOI": "10.1371/journal.pone.0239799",
"doi-asserted-by": "publisher",
"key": "ref61",
"unstructured": "62.\tMaghbooli Z, Sahraian MA, Ebrahimi M, Pazoki M, Kafan S, Tabriz HM, et al. Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection. PloS one. 2020;15:e0239799."
},
{
"DOI": "10.7861/clinmed.2021-0035",
"doi-asserted-by": "publisher",
"key": "ref62",
"unstructured": "63.\tGriffin G, Hewison M, Hopkin J, Kenny RA, Quinton R, Rhodes J, et al. Perspective: Vitamin D supplementation prevents rickets and acute respiratory infections when given as daily maintenance but not as intermittent bolus: implications for COVID-19. Clinical Medicine. 2021;21:e144."
},
{
"DOI": "10.1016/j.bone.2018.02.024",
"doi-asserted-by": "publisher",
"key": "ref63",
"unstructured": "64.\tKetha H, Thacher TD, Oberhelman SS, Fischer PR, Singh RJ, Kumar R. Comparison of the effect of daily versus bolus dose maternal vitamin D3 supplementation on the 24, 25-dihydroxyvitamin D3 to 25-hydroxyvitamin D3 ratio. Bone. 2018;110:321-5."
},
{
"DOI": "10.1136/thorax-2020-btsabstracts.105",
"doi-asserted-by": "publisher",
"key": "ref64",
"unstructured": "65.\tJolliffe DA, Camargo Jr CA, Sluyter JD, Aglipay M, Aloia JF, Ganmaa D, et al. Vitamin D supplementation to prevent acute respiratory infections: a systematic review and meta-analysis of aggregate data from randomised controlled trials. The lancet Diabetes & endocrinology. 2021;9:276-92."
},
{
"DOI": "10.1136/bmjopen-2014-004848",
"doi-asserted-by": "publisher",
"key": "ref65",
"unstructured": "66.\tIversen HH, Bjertnæs ØA, Skudal KE. Patient evaluation of hospital outcomes: an analysis of open-ended comments from extreme clusters in a national survey. BMJ open. 2014;4:e004848."
},
{
"DOI": "10.1016/j.ecl.2010.02.008",
"doi-asserted-by": "publisher",
"key": "ref66",
"unstructured": "67.\tBinkley N, Ramamurthy R, Krueger D. Low vitamin D status: definition, prevalence, consequences, and correction. Endocrinology and Metabolism Clinics. 2010;39:287-301."
},
{
"DOI": "10.3310/hta24100",
"doi-asserted-by": "publisher",
"key": "ref67",
"unstructured": "68.\tRake C, Gilham C, Bukasa L, Ostler R, Newton M, Wild JP, et al. High-dose oral vitamin D supplementation and mortality in people aged 65-84 years: the VIDAL cluster feasibility RCT of open versus double-blind individual randomisation. Health Technology Assessment (Winchester, England). 2020;24:1."
},
{
"DOI": "10.1007/s11154-021-09683-9",
"doi-asserted-by": "publisher",
"key": "ref68",
"unstructured": "69.\tBandeira L, Lazaretti-Castro M, Binkley N. Clinical aspects of SARS-CoV-2 infection and vitamin D. Reviews in Endocrine and Metabolic Disorders. 2021:1-5."
}
],
"reference-count": 69,
"references-count": 69,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.foodandnutritionjournal.org/volume11number1/vitamin-d-on-covid-19-patients-during-the-pandemic-2022-a-systematic-review-and-meta-analysis/"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Vitamin D on COVID-19 Patients During the Pandemic, 2022. A Systematic Review and Meta-Analysis",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.13003/0pyd3js",
"volume": "11"
}
