25-hydroxyvitamin D is a predictor of COVID-19 severity of hospitalized patients
et al., PLOS ONE, doi:10.1371/journal.pone.0268038, May 2022
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 88 COVID-19 hospitalized patients and 122 controls, showing higher mortality, ventilation, and length of stay with vitamin D deficiency.
This is the 132nd of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
risk of death, 81.1% lower, OR 0.19, p = 0.008, cutoff 20ng/mL, adjusted per study, inverted to make OR<1 favor high D levels (≥20ng/mL), 25-OH-D3, multivariable, RR approximated with OR.
|
|
risk of mechanical ventilation, 52.8% lower, OR 0.47, p = 0.13, cutoff 20ng/mL, adjusted per study, inverted to make OR<1 favor high D levels (≥20ng/mL), 25-OH-D3, multivariable, RR approximated with OR.
|
|
risk of no hospital discharge, 74.0% lower, HR 0.26, p < 0.001, cutoff 20ng/mL, 25-OH-D3, Cox proportional hazards.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Nguyen et al., 3 May 2022, retrospective, USA, peer-reviewed, 11 authors, study period 15 July, 2020 - 15 October, 2020.
Contact: nguyen.nguyen2@bswhealth.org.
25-hydroxyvitamin D is a predictor of COVID-19 severity of hospitalized patients
PLOS ONE, doi:10.1371/journal.pone.0268038
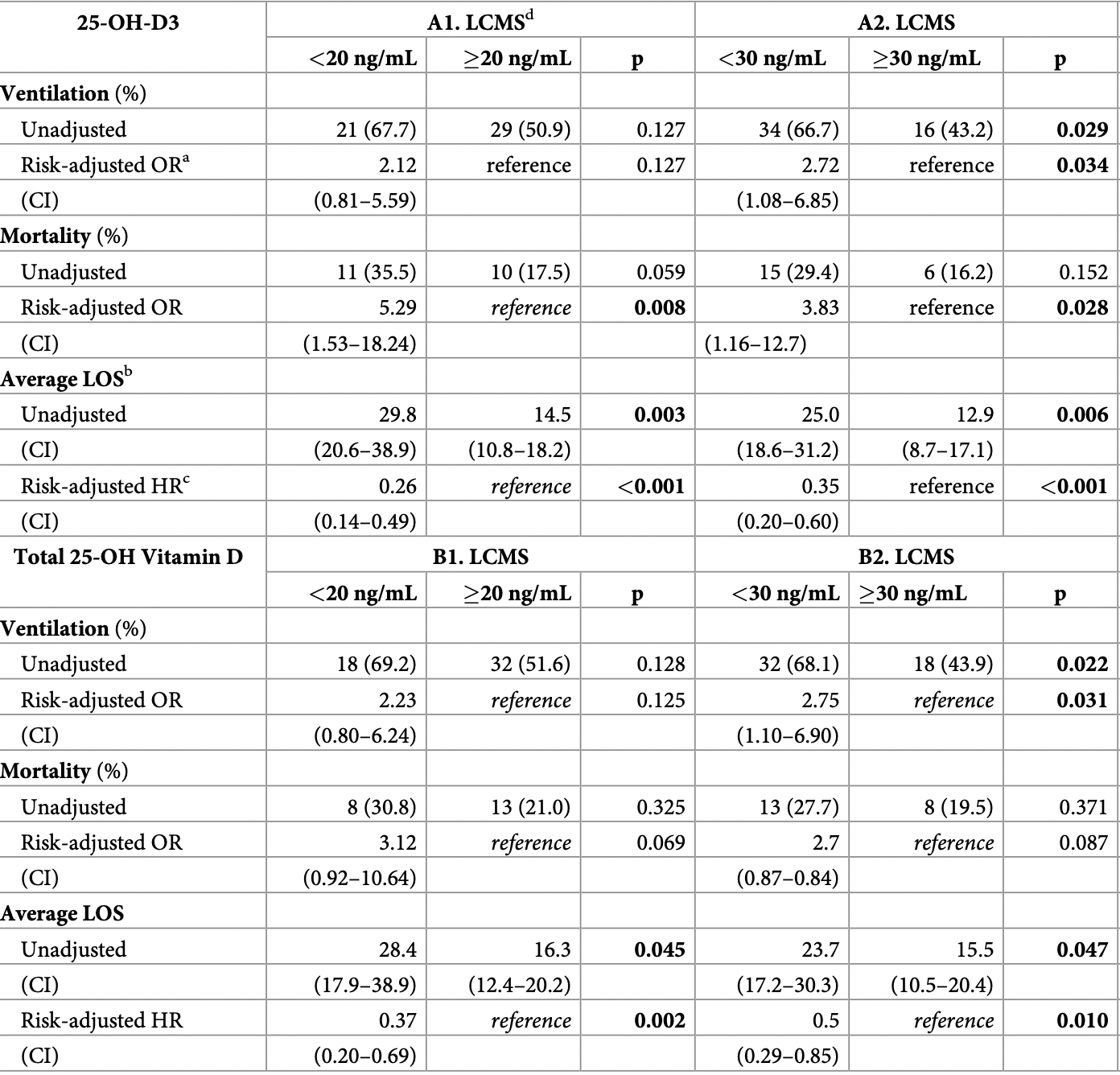
Objectives Studies investigating the association between vitamin D and severity of COVID-19 have mixed results perhaps due to immunoassay assessment of total 25-hydroxyvitamin D (tD) (the sum of 25-hydroxyvitamin-D2 [25-OH-D2] and 25-hydroxyvitamin-D3 [25-OH-D3]). Liquid chromatography tandem mass spectrometry (LC-MS/MS) has high analytical specificity and sensitivity for 25-OH-D2 and 25-OH-D3, and thus enables a more accurate assessment of impact on COVID-19 outcomes. Methods We established reference intervals for 25-OH-D3 and tD using LC-MS/MS. 25-OH-D2, 25-OH-D3 and tD were quantitated for 88 COVID-19 positive and 122 COVID-19 negative specimens. Chi-square or Fisher's exact tests were used to test associations in binary variables. T-Tests or Wilcoxon rank sum tests were used for continuous variables. Cox proportional hazards were used to test associations between 25-OH-D3 or tD levels and length of stay (LOS). For mortality and ventilation, logistic regression models were used.
Results COVID-19 patients with deficient (<20 ng/mL) levels of 25-OH-D3 had significantly longer LOS by 15.3 days. COVID-19 P patients with deficient (<20 ng/mL) and insufficient (<30 ng/ mL) of tD had significantly longer LOS by 12.1 and 8.2 days, respectively. Patients with insufficient levels of tD had significantly longer LOS by 13.7 days. COVID-19 patients with deficient serum 25-OH-D3 levels had significantly increased risk-adjusted odds of in-hospital mortality (OR [95% CI]: 5.29 [1.53-18.24]); those with insufficient 25-OH-D3 had significantly increased risk for requiring ventilation during hospitalization was found at LCMS insufficient cutoff (OR [95%
Supporting information
S1 Table. Full models for adjusted evaluation of mortality, need for ventilation, and LOS. Full models for adjusted evaluation of mortality, need for ventilation, and LOS for COVID-19 positive patients at deficiency and insufficiency cutoffs for 25-OH-D3 and tD. Logistic regression was used for mortality and ventilation, and Cox proportional hazards was used for LOS.
References
Annweiler, Corvaisier, Gautier, Dube ´e, Legrand et al., Vitamin D supplementation associated to better survival in hospitalized frail elderly COVID-19 patients: the GERIA-COVID quasi-experimental study, Nutrients, doi:10.3390/nu12113377
Benton, Tetteh, Needham, Mu ¨cke, Sheppard et al., Evaluation of the 25-hydroxy vitamin D assay on a fully automated liquid chromatography mass spectrometry system, the Thermo Scientific Cascadion SM Clinical Analyzer with the Cascadion 25-hydroxy vitamin D assay in a routine clinical laboratory, Clin Chem Lab Med, doi:10.1515/cclm-2019-0834
Cascadiontm, 25-Hydroxy Vitamin D Assay
Castillo, Costa, Barrios, Alcala ´dı ´az, Lo ´pez Miranda et al., Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study, J Steroid Biochem Mol Biol, doi:10.1016/j.jsbmb.2020.105751
Daneshkhah, Agrawal, Eshein, Subramanian, Roy et al., Evidence for possible association of vitamin D status with cytokine storm and unregulated inflammation in COVID-19 patients, Aging Clin Exp Res, doi:10.1007/s40520-020-01677-y
Gauzzi, Purificato, Donato, Suppressive effect of 1alpha,25-dihydroxyvitamin D3 on type I IFN-mediated monocyte differentiation into dendritic cells: impairment of functional activities and chemotaxis, J Immunol, doi:10.4049/jimmunol.174.1.270
Giustina, Adler, Binkley, Consensus statement from 2 nd International Conference on Controversies in Vitamin D, Rev Endocr Metab Disord, doi:10.1007/s11154-019-09532-w
Gombart, Pierre, Maggini, A Review of Micronutrients and the Immune System-Working in Harmony to Reduce the Risk of Infection, Nutrients
Grant, Lahore, Mcdonnell, Baggerly, French et al., Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths, Nutrients
Heaney, Dowell, Hale, Bendich, Calcium absorption varies within the reference range for serum 25-hydroxyvitamin D, J Am Coll Nutr, doi:10.1080/07315724.2003.10719287
Herna, Nan, Fernandez-Ayala, Garcı ´a-Unzueta, Herna ´ndez-Herna ´ndez et al., Vitamin D status in hospitalized patients with SARS-CoV-2 infection, The Journal of clinical endocrinology and metabolism
Hossein-Nezhad, Holick, Vitamin D for health: a global perspective, Mayo Clin Proc, doi:10.1016/j.mayocp.2013.05.011
Hossein-Nezhad, Spira, Holick, Influence of vitamin D status and vitamin D 3 supplementation on genome wide expression of white blood cells: a randomized double-blind clinical trial, PLoS One, doi:10.1371/journal.pone.0058725
Kaufman, Niles, Kroll, Bi, Holick, SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels, PLoS One, doi:10.1371/journal.pone.0239252
Lemire, Archer, Beck, Spiegelberg, Immunosuppressive actions of 1,25-dihydroxyvitamin D3: preferential inhibition of Th1 functions, J Nutr, doi:10.1093/jn/125.suppl%5F6.1704S
Meltzer, Best, Zhang, Vokes, Arora et al., Association of Vitamin D Status and Other Clinical Characteristics With COVID-19 Test Results, JAMA Netw Open, doi:10.1001/jamanetworkopen.2020.19722
Mohan, Cherian, Sharma, Exploring links between vitamin D deficiency and COVID-19, PLoS Pathog, doi:10.1371/journal.ppat.1008874
Murai, Fernandes, Sales, Pinto, Goessler et al., Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: a randomized clinical trial, Jama, doi:10.1001/jama.2020.26848
Nowson, Mcgrath, Ebeling, Vitamin D and health in adults in Australia and New Zealand: a position statement, Med J Australia, doi:10.5694/mja11.10301
Nurminen, Seuter, Carlberg, Primary Vitamin D Target Genes of Human Monocytes, Front Physiol, doi:10.3389/fphys.2019.00194
Radujkovic, Hippchen, Tiwari-Heckler, Dreher, Boxberger, Vitamin D deficiency and outcome of COVID-19 patients, Nutrients
Thacher, Clarke, Vitamin D Insufficiency, Mayo Clin Proc, doi:10.4065/mcp.2010.0567
DOI record:
{
"DOI": "10.1371/journal.pone.0268038",
"ISSN": [
"1932-6203"
],
"URL": "http://dx.doi.org/10.1371/journal.pone.0268038",
"abstract": "<jats:sec id=\"sec001\">\n<jats:title>Objectives</jats:title>\n<jats:p>Studies investigating the association between vitamin D and severity of COVID-19 have mixed results perhaps due to immunoassay assessment of total 25-hydroxyvitamin D (tD) (the sum of 25-hydroxyvitamin-D2 [25-OH-D2] and 25-hydroxyvitamin-D3 [25-OH-D3]). Liquid chromatography tandem mass spectrometry (LC-MS/MS) has high analytical specificity and sensitivity for 25-OH-D2 and 25-OH-D3, and thus enables a more accurate assessment of impact on COVID-19 outcomes.</jats:p>\n</jats:sec>\n<jats:sec id=\"sec002\">\n<jats:title>Methods</jats:title>\n<jats:p>We established reference intervals for 25-OH-D3 and tD using LC-MS/MS. 25-OH-D2, 25-OH-D3 and tD were quantitated for 88 COVID-19 positive and 122 COVID-19 negative specimens. Chi-square or Fisher’s exact tests were used to test associations in binary variables. T-Tests or Wilcoxon rank sum tests were used for continuous variables. Cox proportional hazards were used to test associations between 25-OH-D3 or tD levels and length of stay (LOS). For mortality and ventilation, logistic regression models were used.</jats:p>\n</jats:sec>\n<jats:sec id=\"sec003\">\n<jats:title>Results</jats:title>\n<jats:p>COVID-19 patients with deficient (<20 ng/mL) levels of 25-OH-D3 had significantly longer LOS by 15.3 days. COVID-19 P patients with deficient (<20 ng/mL) and insufficient (<30 ng/mL) of tD had significantly longer LOS by 12.1 and 8.2 days, respectively. Patients with insufficient levels of tD had significantly longer LOS by 13.7 days. COVID-19 patients with deficient serum 25-OH-D3 levels had significantly increased risk-adjusted odds of in-hospital mortality (OR [95% CI]: 5.29 [1.53–18.24]); those with insufficient 25-OH-D3 had significantly increased risk for requiring ventilation during hospitalization was found at LCMS insufficient cutoff (OR [95% CI]: 2.75 [1.10–6.90]).</jats:p>\n</jats:sec>\n<jats:sec id=\"sec004\">\n<jats:title>Conclusions</jats:title>\n<jats:p>There is an inverse relationship of 25-hydroxyvitamin D levels and hospital LOS for COVID-19 patients. Vitamin D status is a predictor for severity of outcomes. LCMS results are useful for assessing the odds of mortality and the need for ventilation during hospitalization.</jats:p>\n</jats:sec>",
"author": [
{
"ORCID": "http://orcid.org/0000-0002-9362-1994",
"affiliation": [],
"authenticated-orcid": true,
"family": "Nguyen",
"given": "Nguyen N.",
"sequence": "first"
},
{
"affiliation": [],
"family": "Raju",
"given": "Muppala N. P.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "da Graca",
"given": "Briget",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wang",
"given": "Dapeng",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mohamed",
"given": "Nada A.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mutnal",
"given": "Manohar B.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rao",
"given": "Arundhati",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bennett",
"given": "Monica",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gokingco",
"given": "Matthew",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pham",
"given": "Huy",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mohammad",
"given": "Amin A.",
"sequence": "additional"
}
],
"container-title": "PLOS ONE",
"container-title-short": "PLoS ONE",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"www.plosone.org"
]
},
"created": {
"date-parts": [
[
2022,
5,
3
]
],
"date-time": "2022-05-03T17:28:39Z",
"timestamp": 1651598919000
},
"deposited": {
"date-parts": [
[
2022,
5,
3
]
],
"date-time": "2022-05-03T17:28:57Z",
"timestamp": 1651598937000
},
"editor": [
{
"affiliation": [],
"family": "Szecsi",
"given": "Pal Bela",
"sequence": "first"
}
],
"indexed": {
"date-parts": [
[
2022,
5,
4
]
],
"date-time": "2022-05-04T14:40:45Z",
"timestamp": 1651675245514
},
"is-referenced-by-count": 0,
"issue": "5",
"issued": {
"date-parts": [
[
2022,
5,
3
]
]
},
"journal-issue": {
"issue": "5",
"published-online": {
"date-parts": [
[
2022,
5,
3
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
5,
3
]
],
"date-time": "2022-05-03T00:00:00Z",
"timestamp": 1651536000000
}
}
],
"link": [
{
"URL": "https://dx.plos.org/10.1371/journal.pone.0268038",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "340",
"original-title": [],
"page": "e0268038",
"prefix": "10.1371",
"published": {
"date-parts": [
[
2022,
5,
3
]
]
},
"published-online": {
"date-parts": [
[
2022,
5,
3
]
]
},
"publisher": "Public Library of Science (PLoS)",
"reference": [
{
"DOI": "10.1371/journal.pone.0058725",
"article-title": "Influence of vitamin D status and vitamin D3 supplementation on genome wide expression of white blood cells: a randomized double-blind clinical trial",
"author": "A Hossein-nezhad",
"doi-asserted-by": "crossref",
"first-page": "e58725",
"journal-title": "PLoS One",
"key": "pone.0268038.ref001",
"volume": "8",
"year": "2013"
},
{
"DOI": "10.3390/nu12010236",
"article-title": "A Review of Micronutrients and the Immune System-Working in Harmony to Reduce the Risk of Infection",
"author": "AF Gombart",
"doi-asserted-by": "crossref",
"journal-title": "Nutrients",
"key": "pone.0268038.ref002",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1016/j.mayocp.2013.05.011",
"article-title": "Vitamin D for health: a global perspective",
"author": "A Hossein-nezhad",
"doi-asserted-by": "crossref",
"first-page": "720",
"journal-title": "Mayo Clin Proc",
"key": "pone.0268038.ref003",
"volume": "88",
"year": "2013"
},
{
"DOI": "10.4065/mcp.2010.0567",
"article-title": "Vitamin D Insufficiency",
"author": "TD Thacher",
"doi-asserted-by": "crossref",
"first-page": "50",
"journal-title": "Mayo Clin Proc",
"key": "pone.0268038.ref004",
"volume": "86",
"year": "2011"
},
{
"DOI": "10.1016/j.jsbmb.2020.105751",
"article-title": "Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study",
"author": "M Entrenas Castillo",
"doi-asserted-by": "crossref",
"first-page": "105751",
"journal-title": "J Steroid Biochem Mol Biol",
"key": "pone.0268038.ref005",
"volume": "203",
"year": "2020"
},
{
"DOI": "10.3390/nu12092757",
"article-title": "Vitamin D deficiency and outcome of COVID-19 patients",
"author": "A. Radujkovic",
"doi-asserted-by": "crossref",
"first-page": "2757",
"issue": "9",
"journal-title": "Nutrients",
"key": "pone.0268038.ref006",
"volume": "12",
"year": "2020"
},
{
"article-title": "Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths",
"author": "WB Grant",
"journal-title": "Nutrients",
"key": "pone.0268038.ref007",
"volume": "12",
"year": "2020"
},
{
"article-title": "Vitamin D status in hospitalized patients with SARS-CoV-2 infection",
"author": "J. L. Hernández",
"journal-title": "The Journal of clinical endocrinology and metabolism",
"key": "pone.0268038.ref008",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.26848",
"article-title": "Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: a randomized clinical trial",
"author": "I. H. Murai",
"doi-asserted-by": "crossref",
"first-page": "1053",
"issue": "11",
"journal-title": "Jama",
"key": "pone.0268038.ref009",
"volume": "325",
"year": "2021"
},
{
"DOI": "10.1515/cclm-2019-0834",
"article-title": "Evaluation of the 25- hydroxy vitamin D assay on a fully automated liquid chromatography mass spectrometry system, the Thermo Scientific Cascadion SM Clinical Analyzer with the Cascadion 25-hydroxy vitamin D assay in a routine clinical laboratory",
"author": "SC Benton",
"doi-asserted-by": "crossref",
"first-page": "1010",
"journal-title": "Clin Chem Lab Med",
"key": "pone.0268038.ref010",
"volume": "58",
"year": "2020"
},
{
"key": "pone.0268038.ref011",
"unstructured": "CascadionTM SM 25-Hydroxy Vitamin D Assay [Internet]. [cited 2021 Jan 21]. Available from: https://www.thermofisher.com/order/catalog/product/10026927"
},
{
"key": "pone.0268038.ref012",
"unstructured": "Practical Nonparametric Statistics, 3rd Edition | Wiley [Internet]. Wiley.com. [cited 2021 Jan 21]. Available from: https://www.wiley.com/en-us/Practical+Nonparametric+Statistics%2C+3rd+Edition-p-9780471160687"
},
{
"DOI": "10.1007/s11154-019-09532-w",
"article-title": "Consensus statement from 2nd International Conference on Controversies in Vitamin D",
"author": "A Giustina",
"doi-asserted-by": "crossref",
"first-page": "89",
"issue": "1",
"journal-title": "Rev Endocr Metab Disord",
"key": "pone.0268038.ref013",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.1080/07315724.2003.10719287",
"article-title": "Calcium absorption varies within the reference range for serum 25‐hydroxyvitamin D",
"author": "RP Heaney",
"doi-asserted-by": "crossref",
"first-page": "142",
"issue": "2",
"journal-title": "J Am Coll Nutr",
"key": "pone.0268038.ref014",
"volume": "22",
"year": "2003"
},
{
"DOI": "10.5694/mja11.10301",
"article-title": "Vitamin D and health in adults in Australia and New Zealand: a position statement",
"author": "CA Nowson",
"doi-asserted-by": "crossref",
"first-page": "686",
"issue": "11",
"journal-title": "Med J Australia",
"key": "pone.0268038.ref015",
"volume": "196",
"year": "2012"
},
{
"key": "pone.0268038.ref016",
"unstructured": "Ilex Medical, specializes in medical diagnostics Manufacture and sale of medical equipment—[Internet]. [cited 2021 Jan 22]. Available from: https://www.ilexmedical.com/"
},
{
"DOI": "10.1371/journal.ppat.1008874",
"article-title": "Exploring links between vitamin D deficiency and COVID-19",
"author": "M Mohan",
"doi-asserted-by": "crossref",
"first-page": "e1008874",
"journal-title": "PLoS Pathog",
"key": "pone.0268038.ref017",
"volume": "16",
"year": "2020"
},
{
"DOI": "10.3390/nu12113377",
"article-title": "Vitamin D supplementation associated to better survival in hospitalized frail elderly COVID-19 patients: the GERIA-COVID quasi-experimental study",
"author": "G. Annweiler",
"doi-asserted-by": "crossref",
"first-page": "3377",
"issue": "11",
"journal-title": "Nutrients",
"key": "pone.0268038.ref018",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0239252",
"article-title": "SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels",
"author": "H. W. Kaufman",
"doi-asserted-by": "crossref",
"first-page": "e0239252",
"issue": "9",
"journal-title": "PLoS One",
"key": "pone.0268038.ref019",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1007/s40520-020-01677-y",
"article-title": "Evidence for possible association of vitamin D status with cytokine storm and unregulated inflammation in COVID-19 patients",
"author": "A Daneshkhah",
"doi-asserted-by": "crossref",
"first-page": "2141",
"issue": "10",
"journal-title": "Aging Clin Exp Res",
"key": "pone.0268038.ref020",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.4049/jimmunol.174.1.270",
"article-title": "Suppressive effect of 1alpha,25-dihydroxyvitamin D3 on type I IFN-mediated monocyte differentiation into dendritic cells: impairment of functional activities and chemotaxis",
"author": "MC Gauzzi",
"doi-asserted-by": "crossref",
"first-page": "270",
"issue": "1",
"journal-title": "J Immunol",
"key": "pone.0268038.ref021",
"volume": "174",
"year": "2005"
},
{
"DOI": "10.3389/fphys.2019.00194",
"article-title": "Primary Vitamin D Target Genes of Human Monocytes",
"author": "V Nurminen",
"doi-asserted-by": "crossref",
"first-page": "194",
"journal-title": "Front Physiol",
"key": "pone.0268038.ref022",
"volume": "10",
"year": "2019"
},
{
"DOI": "10.1001/jamanetworkopen.2020.19722",
"article-title": "Association of Vitamin D Status and Other Clinical Characteristics With COVID-19 Test Results",
"author": "DO Meltzer",
"doi-asserted-by": "crossref",
"first-page": "e2019722",
"journal-title": "JAMA Netw Open",
"key": "pone.0268038.ref023",
"volume": "3",
"year": "2020"
},
{
"article-title": "Immunosuppressive actions of 1,25-dihydroxyvitamin D3: preferential inhibition of Th1 functions",
"author": "JM Lemire",
"first-page": "1704S",
"issue": "6",
"journal-title": "J Nutr",
"key": "pone.0268038.ref024",
"volume": "125",
"year": "1995"
}
],
"reference-count": 24,
"references-count": 24,
"relation": {},
"resource": {
"primary": {
"URL": "https://dx.plos.org/10.1371/journal.pone.0268038"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Multidisciplinary"
],
"subtitle": [],
"title": "25-hydroxyvitamin D is a predictor of COVID-19 severity of hospitalized patients",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1371/journal.pone.corrections_policy",
"volume": "17"
}
