Vitamin D 25OH deficiency in COVID-19 patients admitted to a tertiary referral hospital
et al., Clinical Nutrition (Edinburgh, Scotland), doi:10.1016/j.clnu.2020.10.055, Nov 2020
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
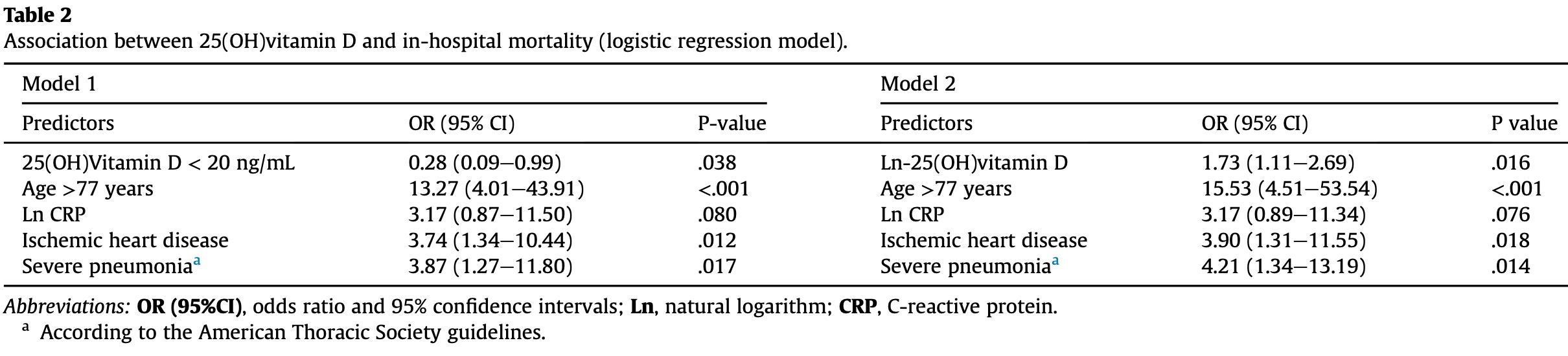
Prospective cohort study of 129 adult hospitalized COVID-19 patients finding patients with vitamin D levels >20ng/mL had increased mortality after adjustment. This study does not account for the risk of having a serious enough case to be hospitalized, and adjustments for factors correlated with vitamin D levels could obscure a potential association with vitamin D levels.
This is the 25th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
risk of death, 120.0% higher, RR 2.20, p = 0.04, high D levels 10 of 30 (33.3%), low D levels 24 of 99 (24.2%), inverted to make RR<1 favor high D levels, odds ratio converted to relative risk, >20ng/mL.
|
|
risk of ICU admission, 86.7% lower, RR 0.13, p = 0.59, high D levels 0 of 30 (0.0%), low D levels 5 of 99 (5.1%), NNT 20, relative risk is not 0 because of continuity correction due to zero events (with reciprocal of the contrasting arm).
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Cereda et al., 1 Nov 2020, prospective, Italy, peer-reviewed, 13 authors.
Vitamin D 25OH deficiency in COVID-19 patients admitted to a tertiary referral hospital
doi:10.1016/j.clnu.2020.10.055
Since January 2020 Elsevier has created a COVID-19 resource centre with free information in English and Mandarin on the novel coronavirus COVID-19. The COVID-19 resource centre is hosted on Elsevier Connect, the company's public news and information website. Elsevier hereby grants permission to make all its COVID-19-related research that is available on the COVID-19 resource centre -including this research content -immediately available in PubMed Central and other publicly funded repositories, such as the WHO COVID database with rights for unrestricted research re-use and analyses in any form or by any means with acknowledgement of the original source. These permissions are granted for free by Elsevier for as long as the COVID-19 resource centre remains active.
Author contributions Caccialanza, Cereda and Bogliolo had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of data analysis. Caccialanza is chief investigators and act as guarantors for this work. Concept and design: Caccialanza, Cereda, Bogliolo, Klersy. Acquisition, analysis, or interpretation of data: Caccialanza, Cereda, Bogliolo, Klersy, Lobascio, Masi, Crotti, De Stefano, Mariani, Ludovisi, Muggia, Croce, Barteselli, Mambella, Di Terlizzi, Belliato. Drafting of the manuscript: Caccialanza, Cereda, Bogliolo, Klersy. Critical revision of the manuscript for important intellectual content: Montecucco, Di Sabatino, Corsico, Perlini, Bruno. Statistical analysis: Klersy. Administrative, technical, or material support: Ferrari. Supervision: Caccialanza. Other -Research facilitator responsible for data collection from participants: Mariani, Ludovisi, Muggia, Croce, Barteselli, Mambella, Di Terlizzi. Other -Trial management: Cereda, Bogliolo, Masi, Crotti, De Stefano, Lobascio.
Additional contributions We are grateful to all the employees of the Fondazione IRCCS Policlinico San Matteo for their courageous efforts in struggling against the clinical and social COVID-19 emergency.
Conflict of interest None of the authors have conflicts of interest to disclose.
References
Castillo, Costa, Barrios, Díaz, Opez Miranda et al., Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: a pilot randomized clinical study, J Steroid Biochem Mol Biol
Daneshkhah, Agrawal, Eshein, Subramanian, Roy et al., Evidence for possible association of vitamin D status with cytokine storm and unregulated inflammation in COVID-19 patients, Aging Clin Exp Res
Duncan, Talwar, Mcmillan, Stefanowicz, Reilly, Quantitative data on the magnitude of the systemic inflammatory response and its effect on micronutrient status based on plasma measurements, Am J Clin Nutr
Mardani, Alamdary, Nasab, Gholami, Ahmadi et al., Association of vitamin D with the modulation of the disease severity in COVID-19, Virus Res
Merad, Martin, Pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages, Nat Rev Immunol
Montazeri, Nasiri, Shirvani, Holick, Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection, PloS One
Panagiotou, Tee, Ihsan, Athar, Marchitelli et al., Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalized with COVID-19 are associated with greater disease severity, Clin Endocrinol, doi:10.1111/cen.14276
Radujkovic, Hippchen, Tiwari-Heckler, Dreher, Boxberger, Vitamin D deficiency and outcome of COVID-19 patients, Nutrients
Reijven, Soeters, Vitamin D: a magic bullet or a myth?, Clin Nutr
Rhodes, Subramanian, Laird, Griffin, Kenny, Perspective: vitamin D deficiency and COVID-19 severity -plausibly linked by latitude, ethnicity, impacts on cytokines, ACE2 and thrombosis, J Intern Med, doi:10.1111/joim.13149
DOI record:
{
"DOI": "10.1016/j.clnu.2020.10.055",
"ISSN": [
"0261-5614"
],
"URL": "http://dx.doi.org/10.1016/j.clnu.2020.10.055",
"alternative-id": [
"S0261561420306014"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Vitamin D 25OH deficiency in COVID-19 patients admitted to a tertiary referral hospital"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Clinical Nutrition"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.clnu.2020.10.055"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2020 Elsevier Ltd and European Society for Clinical Nutrition and Metabolism. All rights reserved."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-0747-1951",
"affiliation": [],
"authenticated-orcid": false,
"family": "Cereda",
"given": "Emanuele",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-1661-0482",
"affiliation": [],
"authenticated-orcid": false,
"family": "Bogliolo",
"given": "Laura",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Klersy",
"given": "Catherine",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lobascio",
"given": "Federica",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Masi",
"given": "Sara",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Crotti",
"given": "Silvia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "De Stefano",
"given": "Ludovico",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bruno",
"given": "Raffaele",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8716-4694",
"affiliation": [],
"authenticated-orcid": false,
"family": "Corsico",
"given": "Angelo Guido",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Di Sabatino",
"given": "Antonio",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0320-8574",
"affiliation": [],
"authenticated-orcid": false,
"family": "Perlini",
"given": "Stefano",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Montecucco",
"given": "Carlomaurizio",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Caccialanza",
"given": "Riccardo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Belliato",
"given": "Mirko",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ludovisi",
"given": "Serena",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mariani",
"given": "Francesca",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ferrari",
"given": "Alessandra",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Musella",
"given": "Valeria",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Muggia",
"given": "Chiara",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Croce",
"given": "Gabriele",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Barteselli",
"given": "Chiara",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mambella",
"given": "Jacopo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Di Terlizzi",
"given": "Francesco",
"sequence": "additional"
}
],
"container-title": "Clinical Nutrition",
"container-title-short": "Clinical Nutrition",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.jp",
"clinicalkey.com",
"clinicalkey.es",
"clinicalkey.fr",
"clinicalkey.com.au",
"clinicalnutritionjournal.com",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2020,
11,
2
]
],
"date-time": "2020-11-02T22:59:04Z",
"timestamp": 1604357944000
},
"deposited": {
"date-parts": [
[
2021,
11,
11
]
],
"date-time": "2021-11-11T03:05:41Z",
"timestamp": 1636599941000
},
"indexed": {
"date-parts": [
[
2024,
2,
12
]
],
"date-time": "2024-02-12T18:09:16Z",
"timestamp": 1707761356034
},
"is-referenced-by-count": 57,
"issue": "4",
"issued": {
"date-parts": [
[
2021,
4
]
]
},
"journal-issue": {
"issue": "4",
"published-print": {
"date-parts": [
[
2021,
4
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
4,
1
]
],
"date-time": "2021-04-01T00:00:00Z",
"timestamp": 1617235200000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S0261561420306014?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S0261561420306014?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "2469-2472",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2021,
4
]
]
},
"published-print": {
"date-parts": [
[
2021,
4
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"article-title": "Perspective: vitamin D deficiency and COVID-19 severity - plausibly linked by latitude, ethnicity, impacts on cytokines, ACE2 and thrombosis",
"author": "Rhodes",
"journal-title": "J Intern Med",
"key": "10.1016/j.clnu.2020.10.055_bib1",
"year": "2020"
},
{
"DOI": "10.1016/j.clnu.2019.12.028",
"article-title": "Vitamin D: a magic bullet or a myth?",
"author": "Reijven",
"doi-asserted-by": "crossref",
"first-page": "2663",
"issue": "9",
"journal-title": "Clin Nutr",
"key": "10.1016/j.clnu.2020.10.055_bib2",
"volume": "39",
"year": "2020"
},
{
"DOI": "10.3390/nu12092757",
"article-title": "Vitamin D deficiency and outcome of COVID-19 patients",
"author": "Radujkovic",
"doi-asserted-by": "crossref",
"first-page": "E2757",
"issue": "9",
"journal-title": "Nutrients",
"key": "10.1016/j.clnu.2020.10.055_bib3",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1007/s40520-020-01677-y",
"article-title": "Evidence for possible association of vitamin D status with cytokine storm and unregulated inflammation in COVID-19 patients",
"author": "Daneshkhah",
"doi-asserted-by": "crossref",
"first-page": "2141",
"issue": "10",
"journal-title": "Aging Clin Exp Res",
"key": "10.1016/j.clnu.2020.10.055_bib4",
"volume": "32",
"year": "2020"
},
{
"article-title": "Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalized with COVID-19 are associated with greater disease severity",
"author": "Panagiotou",
"journal-title": "Clin Endocrinol (Oxf)",
"key": "10.1016/j.clnu.2020.10.055_bib5",
"year": "2020"
},
{
"article-title": "Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection",
"author": "Montazeri",
"issue": "9",
"journal-title": "PloS One",
"key": "10.1016/j.clnu.2020.10.055_bib6",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1016/j.virusres.2020.198148",
"article-title": "Association of vitamin D with the modulation of the disease severity in COVID-19",
"author": "Mardani",
"doi-asserted-by": "crossref",
"first-page": "198148",
"journal-title": "Virus Res",
"key": "10.1016/j.clnu.2020.10.055_bib7",
"volume": "289",
"year": "2020"
},
{
"DOI": "10.1016/j.jsbmb.2020.105751",
"article-title": "Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: a pilot randomized clinical study",
"author": "Entrenas Castillo",
"doi-asserted-by": "crossref",
"first-page": "105751",
"journal-title": "J Steroid Biochem Mol Biol",
"key": "10.1016/j.clnu.2020.10.055_bib8",
"volume": "203",
"year": "2020"
},
{
"DOI": "10.1038/s41577-020-0331-4",
"article-title": "Pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages",
"author": "Merad",
"doi-asserted-by": "crossref",
"first-page": "355",
"journal-title": "Nat Rev Immunol",
"key": "10.1016/j.clnu.2020.10.055_bib9",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.3945/ajcn.111.023812",
"article-title": "Quantitative data on the magnitude of the systemic inflammatory response and its effect on micronutrient status based on plasma measurements",
"author": "Duncan",
"doi-asserted-by": "crossref",
"first-page": "64",
"journal-title": "Am J Clin Nutr",
"key": "10.1016/j.clnu.2020.10.055_bib10",
"volume": "95",
"year": "2012"
}
],
"reference-count": 10,
"references-count": 10,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S0261561420306014"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Critical Care and Intensive Care Medicine",
"Nutrition and Dietetics"
],
"subtitle": [],
"title": "Vitamin D 25OH deficiency in COVID-19 patients admitted to a tertiary referral hospital",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "40"
}
