Deficiency of vitamin D is a risk factor of mortality in patients with COVID-19
et al., Revista de Sanidad Militar, doi:10.35366/93773, Apr 2020
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
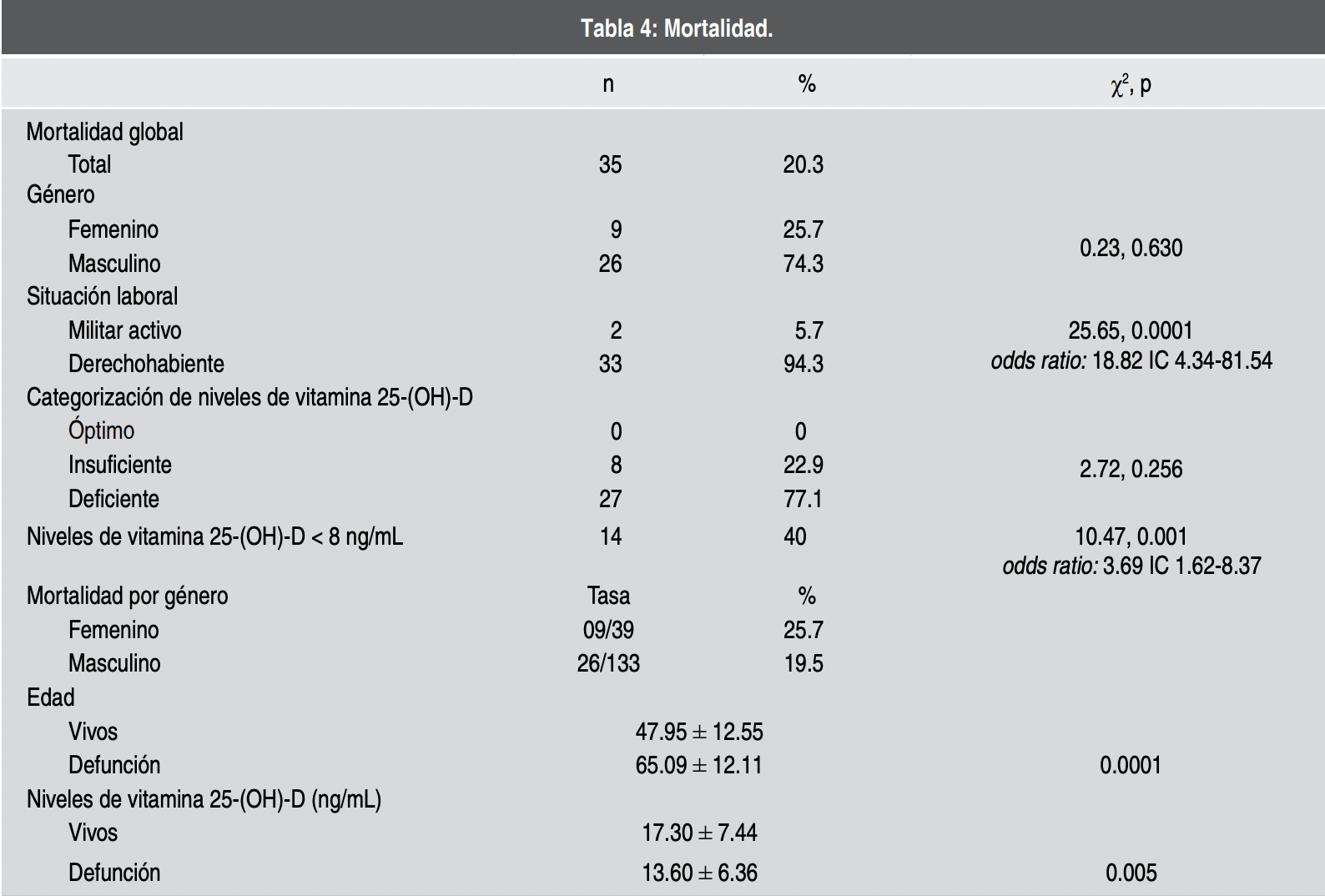
Retrospective 172 hospitalized COVID-19 patients in Mexico, reporting a very high prevalence of vitamin D deficiency, and significantly higher mortality with low vitamin D levels in unadjusted results.
This is the 2nd of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
This study is excluded in the after exclusion results of meta-analysis:
unadjusted results with no group details.
|
risk of death, 61.7% lower, RR 0.38, p = 0.006, high D levels (≥8ng/mL) 21 of 137 (15.3%), low D levels (<8ng/mL) 14 of 35 (40.0%), NNT 4.1, inverted to make RR<1 favor high D levels (≥8ng/mL), odds ratio converted to relative risk.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Reyes Pérez et al., 30 Apr 2020, retrospective, Mexico, peer-reviewed, 5 authors.
Contact: tort1822@gmail.com.
La deficiencia de vitamina D es un factor de riesgo de mortalidad en pacientes con COVID-19
Revista de Sanidad Militar, doi:10.35366/93773
Introduction: At this moment COVID-19 disease has no specific treatment and there is no vaccine available. This disease has an elevated morbidity-mortality not only in Mexico but worldwide, and it is the reason why it's essential to study factors that could modulate the course of the disease; the role of vitamin D seems to have a fundamental role in immunity when we talk about respiratory infections.
Objective: Determine the association between vitamin D levels and mortality in hospitalized patients with COVID-19 at the Hospital Central Militar México. Material and methods: This study included 172 patients diagnosed with COVID-19 whom serum levels of vitamin 25-(OH)-D were determined. Considering as a case the patients who died from COVID-19 and control patients who survived. Results: Vitamin 25-(OH)-D serum levels in hospitlized patients with COVID-19 were 16.54 ± 7.22 ng/mL. The 95.92% presented vitamin D levels below the ideal range. Patients with vitamin D serum levels bellow 8 ng/mL had 3.68 higher risk of dying from COVID-19. Conclusion: Patients with COVID-19 who require hospitalization were deficient in vitamin D and their serum levels were bellow 8 ng/mL. This is considered a risk factor and therefore increases mortality in the disease caused by COVID-19, reason enough to take several actions such as oral suplementation in order to improve vitamin D serum levels.
References
Amrein, Scherkl, Hoffmann, Neuwersch, Köstenberger et al., Vitamin D deficiency 2.0: an update on the current status worldwide, Eur J Clin Nutr, doi:10.1038/s41430-020-0558-y
Cannell, Vieth, Umhau, Epidemic influenza and vitamin D, Epidemiol Infect, doi:10.1017/S0950268806007175
Cruz, Cervantes, Juárez, COVID-19, a worldwide public health emergency
Cui, Xu, Li, Qiao, Han et al., Vitamin D receptor activation regulates microglia polarization and oxidative stress in spontaneously hypertensive rats and angiotensin II-exposed microglial cells: Role of renin-angiotensin system, Redox Biol, doi:10.1016/j.redox.2019.101295
Grant, Lahore, Mcdonnell, Baggerly, Francés et al., Evidencia de que la suplementación con vitamina D podría reducir el riesgo de influenza e infecciones y muertes por COVID-19, Nutri
Grant, Lahore, Mcdonnell, Baggerly, French et al., Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths, Nutrients, doi:10.3390/nu12040988
Holick, Medical progress: vitamin D deficiency, N Engl J Med, doi:10.1056/NEJMra070553
Hossein-Nezhad, Holick, Vitamin D for health: a global perspective, Mayo Clin Proc, doi:10.1016/j.mayocp.2013.05.011
Ianevski, Zusinaite, Shtaida, Kallio-Kokko, Valkonen et al., Low temperature and low UV indexes correlated with peaks of influenza virus activity in Northern Europe during 2010-2018, Viruses, doi:10.3390/v11030207
Ilie, Stefanescu, Smith, The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality
Kechichian, Ezzedine, Vitamin D and the skin: an update for dermatologists, Am J Clin Dermatol, doi:10.1007/s40257-017-0323-8
Khan, Fabian, How I treat vitamin d deficiency, J Oncol Pract
Lips, Cashman, Lamberg-Allardt, Bischoff-Ferrari, Obermayer-Pietsch et al., Current vitamin D status in European and Middle East countries and strategies to prevent vitamin D deficiency: a position statement of the European Calcified Tissue Society, Eur J Endocrinol, doi:10.1530/EJE-18-0736
Marik, Kory, Varon, Does vitamin D status impact mortality from SARS-CoV-2 infection?
Raharusun, Priambada, Budiarti, Agung, Budi, Patterns of COVID-19 Mortality and Vitamin D: An Indonesian Study
Rhodes, Subramanian, Laird, Kenny, Editorial: low population mortality from COVID-19 in countries south of latitude 35 degrees North supports vitamin D as a factor determining severity, Aliment Pharmacol Ther, doi:10.1111/apt.15777
Rhodes, Webb, Fraser, Kift, Durkin et al., Recommended summer sunlight exposure levels can produce sufficient (> or =20 ng ml(-1)) but not the proposed optimal (> or =32 ng ml(-1))
Richardson, Hirsch, Narasimhan, Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area, JAMA, doi:10.1001/jama.2020.6775
Soler, Lloveras, Batlle, Enzima conversiva de la angiotensina 2 y su papel emergente en la regulación del sistema renina-angiotensina, Medicina Clínica, doi:10.1157/13124619
Sowah, Fan, Dennett, Hagtvedt, Straube, Vitamin D levels and deficiency with different occupations: a systematic review, BMC Public Health, doi:10.1186/s12889-017-4436-z
Spiro, Buttriss, Vitamin D: an overview of vitamin D status and intake in Europe, Nutr Bull, doi:10.1111/nbu.12108
Teymoori-Rad, Shokri, Salimi, Marashi, The interplay between vitamin D and viral infections, Rev Med Virol, doi:10.1002/rmv.2032
Tikellis, Thomas, Angiotensin-converting enzyme 2 (ACE2) is a key modulator of the renin angiotensin system in health and disease, Int J Pept, doi:10.1155/2012/256294
Varsavskya, Rozas, Becerra, Luque, Quesada et al., Recomendaciones de vitamina D para la población general, Endocrinol Diabetes Nutr, doi:10.1016/j.endinu.2016.11.002
Zhou, Yu, Du, Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study [published correction appears, Lancet
DOI record:
{
"DOI": "10.35366/93773",
"ISSN": [
"0301-696X"
],
"URL": "http://dx.doi.org/10.35366/93773",
"alternative-id": [
"93773"
],
"author": [
{
"affiliation": [],
"family": "Reyes Pérez",
"given": "Rocío Adriana",
"sequence": "first"
},
{
"affiliation": [],
"family": "Puente Nieto",
"given": "Ana Victoria",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Martínez-Cuazitl",
"given": "Adriana",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Montelongo Mercado",
"given": "Edgardo Alonso",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rodríguez Tort",
"given": "Arturo",
"sequence": "additional"
}
],
"container-title": "Revista de Sanidad Militar",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2020,
6,
16
]
],
"date-time": "2020-06-16T23:45:07Z",
"timestamp": 1592351107000
},
"deposited": {
"date-parts": [
[
2022,
7,
1
]
],
"date-time": "2022-07-01T08:55:25Z",
"timestamp": 1656665725000
},
"indexed": {
"date-parts": [
[
2022,
7,
1
]
],
"date-time": "2022-07-01T09:11:21Z",
"timestamp": 1656666681876
},
"is-referenced-by-count": 6,
"issue": "1-2",
"issued": {
"date-parts": [
[
2020
]
]
},
"journal-issue": {
"issue": "1-2",
"published-print": {
"date-parts": [
[
2020
]
]
}
},
"language": "es",
"member": null,
"original-title": [],
"page": "106-113",
"prefix": "10.56443",
"published": {
"date-parts": [
[
2020
]
]
},
"published-print": {
"date-parts": [
[
2020
]
]
},
"publisher": null,
"reference-count": 27,
"references-count": 27,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.medigraphic.com/cgi-bin/new/resumen.cgi?IDARTICULO=93773"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "La deficiencia de vitamina D es un factor de riesgo de mortalidad en pacientes con COVID-19",
"type": "journal-article",
"volume": "74"
}
