Low 25-Hydroxyvitamin D Levels on Admission to the Intensive Care Unit May Predispose COVID-19 Pneumonia Patients to a Higher 28-Day Mortality Risk: A Pilot Study on a Greek ICU Cohort
et al., Nutrients, doi:10.3390/nu12123773, Dec 2020
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
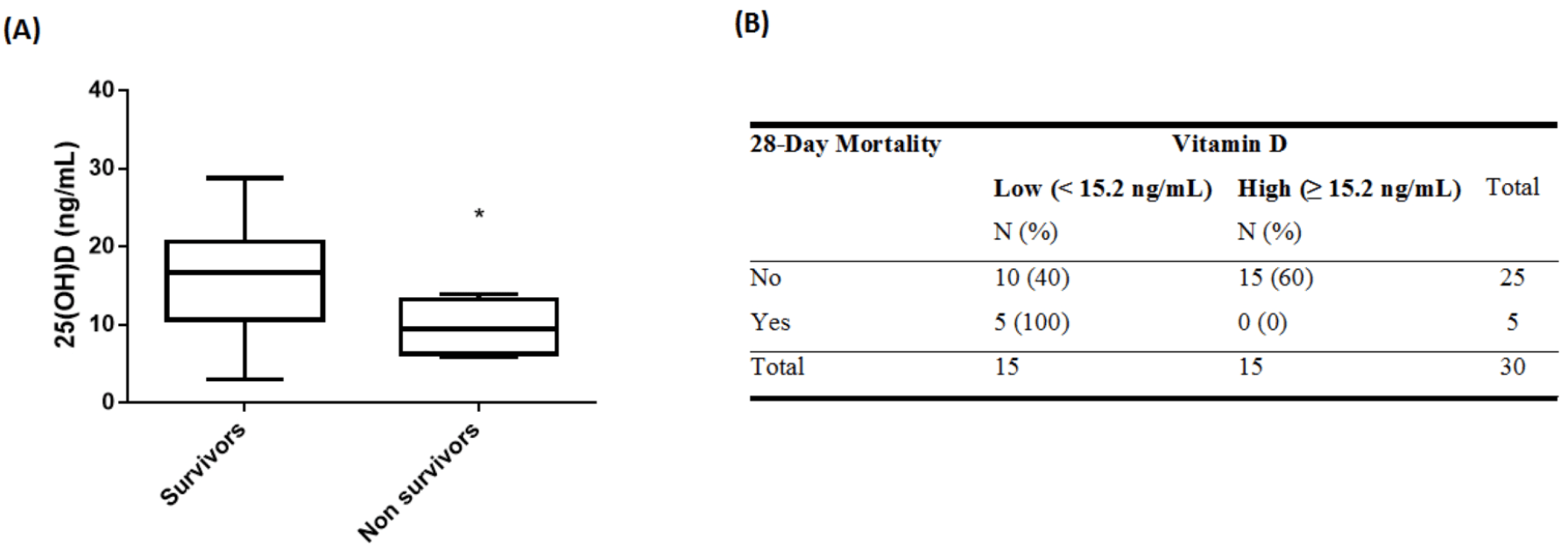
Small prospective study of 30 ICU patients, showing higher mortality risk for low vitamin D levels. When divided into two groups at the median level, there was 5 of 15 deaths for the low vitamin D group compared to 0 of 15 in the high vitamin D group.
This is the 32nd of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
risk of death, 90.9% lower, RR 0.09, p = 0.04, high D levels 0 of 15 (0.0%), low D levels 5 of 15 (33.3%), NNT 3.0, relative risk is not 0 because of continuity correction due to zero events (with reciprocal of the contrasting arm), >15.2ng/mL.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Vassiliou et al., 9 Dec 2020, prospective, Greece, peer-reviewed, 6 authors.
Abstract: Hellenic Journal of Cardiology 62 (2021) 381e383
Contents lists available at ScienceDirect
Hellenic Journal of Cardiology
journal homepage: http://www.journals.elsevier.com/
hellenic-journal-of-cardiology/
Correspondence
Vitamin D deficiency correlates with a reduced number of natural
killer cells in intensive care unit (ICU) and non-ICU patients with
COVID-19 pneumonia
Keywords:
COVID-19
Vitamin D
Natural killer cells
Regulation of immune function continues to be one of the most
well-recognised extra-skeletal actions of vitamin D. In vitro data
have shown that vitamin D modulates immune cells and induces
immune tolerance, while in vivo data from animal studies and
from vitamin D supplementation human studies have shown beneficial effects of vitamin D on immune function, particularly in the
context of autoimmunity.1 In the present study, we examined
whether vitamin D deficiency modulates the number of immune
cells in COVID-19 patients.
This observational, single-centre study included consecutive
COVID-19 intensive care unit (ICU) patients (N ¼ 29) and consecutive patients hospitalised in a specialised non-ICU COVID-19 ward
(N ¼ 10) who were discharged from the hospital without being
transferred to the ICU, from March 18th 2020 to May 25th 2020.
The study was approved by the Hospital's Research Ethics Committee (129/19-3-2020), and all procedures carried out on patients
were in compliance with the Helsinki Declaration. Informed written consent was obtained from all patients or patients' next-ofkin. Total 25-hydroxyvitamin D was measured on hospital admission using the electrochemiluminescence immunoassay method
(Cobas E602, Roche Diagnostics International Ltd). Immune phenotyping was performed by flow cytometric analysis (Navios EX flow
cytometer, Beckman Coulter).
Vitamin D levels positively correlated with subpopulations of
immune cells, namely, cytotoxic T cells (rs ¼ 0.344, p ¼ 0.032), natural killer (NK) cells (rs ¼ 0.496, p ¼ 0.001), NK-T cells (rs ¼ 0.325,
p ¼ 0.044) and regulatory T cells (rs ¼ 0.333, p ¼ 0.038). With
respect to all other clinical and laboratory parameters, vitamin D
levels correlated only with albumin (rs ¼ 0.387, p ¼ 0.018). To
further explore these associations, we divided our cohort into
two groups based on their vitamin D levels; we classified them as
vitamin D deficient (19.9 ng/ml, N ¼ 32) and vitamin D insufficient (20-29.9 ng/ml, N ¼ 7). Demographics, clinical and biochemical characteristics on hospital admission and important outcomes
Peer review under responsibility of Hellenic Society of Cardiology.
of the two patient groups are listed in Table 1. As expected, hypertension was the most common comorbidity.2 The two groups
differed only in the number of NK cells (Table 1 and Figure 1). Cytotoxic T cells, NK-T cells and regulatory T cells did not differ in the
two groups. It should also be noted that the two patient groups
did not differ with respect to hospital mortality or disease severity.
The beneficial effects of vitamin D on protective immunity are
due in part to its effects on the innate immune system. In vitro
studies have reported contradictory results on the role of vitamin
D on NK cell function, but whether vitamin D induces or inhibits
NK cell function in vivo remains unclear.3 NK cells are a type of
cytotoxic lymphocytes that are critical to the innate immune system and secrete many cytokines and chemokines. Despite their vital role in viral infections, the contribution of NK cells in..
DOI record:
{
"DOI": "10.3390/nu12123773",
"ISSN": [
"2072-6643"
],
"URL": "http://dx.doi.org/10.3390/nu12123773",
"abstract": "<jats:p>We aimed to examine whether low intensive care unit (ICU) admission 25-hydroxyvitamin D (25(OH)D) levels are associated with worse outcomes of COVID-19 pneumonia. This was a prospective observational study of SARS-CoV2 positive critically ill patients treated in a multidisciplinary ICU. Thirty (30) Greek patients were included, in whom 25(OH)D was measured on ICU admission. Eighty (80%) percent of patients had vitamin D deficiency, and the remaining insufficiency. Based on 25(OH)D levels, patients were stratified in two groups: higher and lower than the median value of the cohort (15.2 ng/mL). The two groups did not differ in their demographic or clinical characteristics. All patients who died within 28 days belonged to the low vitamin D group. Survival analysis showed that the low vitamin D group had a higher 28-day survival absence probability (log-rank test, p = 0.01). Critically ill COVID-19 patients who died in the ICU within 28 days appeared to have lower ICU admission 25(OH)D levels compared to survivors. When the cohort was divided at the median 25(OH)D value, the low vitamin D group had an increased risk of 28-day mortality. It seems plausible, therefore, that low 25(OH)D levels may predispose COVID-19 patients to an increased 28-day mortality risk.</jats:p>",
"alternative-id": [
"nu12123773"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-4984-0476",
"affiliation": [],
"authenticated-orcid": false,
"family": "Vassiliou",
"given": "Alice G.",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-7306-713X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Jahaj",
"given": "Edison",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pratikaki",
"given": "Maria",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Orfanos",
"given": "Stylianos E.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2219-7292",
"affiliation": [],
"authenticated-orcid": false,
"family": "Dimopoulou",
"given": "Ioanna",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2508-500X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Kotanidou",
"given": "Anastasia",
"sequence": "additional"
}
],
"container-title": "Nutrients",
"container-title-short": "Nutrients",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2020,
12,
9
]
],
"date-time": "2020-12-09T14:17:58Z",
"timestamp": 1607523478000
},
"deposited": {
"date-parts": [
[
2020,
12,
10
]
],
"date-time": "2020-12-10T06:40:30Z",
"timestamp": 1607582430000
},
"indexed": {
"date-parts": [
[
2024,
4,
2
]
],
"date-time": "2024-04-02T15:10:31Z",
"timestamp": 1712070631552
},
"is-referenced-by-count": 38,
"issue": "12",
"issued": {
"date-parts": [
[
2020,
12,
9
]
]
},
"journal-issue": {
"issue": "12",
"published-online": {
"date-parts": [
[
2020,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2020,
12,
9
]
],
"date-time": "2020-12-09T00:00:00Z",
"timestamp": 1607472000000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2072-6643/12/12/3773/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "3773",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2020,
12,
9
]
]
},
"published-online": {
"date-parts": [
[
2020,
12,
9
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1097/CCM.0b013e31829eb7af",
"doi-asserted-by": "publisher",
"key": "ref1"
},
{
"DOI": "10.1126/science.1123933",
"doi-asserted-by": "publisher",
"key": "ref2"
},
{
"DOI": "10.4049/jimmunol.179.4.2060",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.4049/jimmunol.173.5.2909",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.7861/clinmed.2020-0301",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.1016/j.cct.2020.106176",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.1001/jama.2012.5669",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.1210/jc.2010-2704",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"DOI": "10.1016/j.medidd.2020.100064",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"DOI": "10.1007/s40618-020-01370-x",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.1038/s41598-020-77093-z",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.3390/nu12092757",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.1002/jmv.26360",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"DOI": "10.1016/j.virusres.2020.198148",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.1111/cen.14276",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.3389/fpubh.2020.00513",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.1371/journal.pone.0239799",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.1007/s00394-020-02429-4",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.1016/j.jsbmb.2020.105771",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.3390/nu12113377",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.1111/febs.15495",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"DOI": "10.3390/nu12051359",
"doi-asserted-by": "publisher",
"key": "ref22"
}
],
"reference-count": 22,
"references-count": 22,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2072-6643/12/12/3773"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Food Science",
"Nutrition and Dietetics"
],
"subtitle": [],
"title": "Low 25-Hydroxyvitamin D Levels on Admission to the Intensive Care Unit May Predispose COVID-19 Pneumonia Patients to a Higher 28-Day Mortality Risk: A Pilot Study on a Greek ICU Cohort",
"type": "journal-article",
"volume": "12"
}
