Association Between Preoperative 25-Hydroxyvitamin D Level and Hospital-Acquired Infections Following Roux-en-Y Gastric Bypass Surgery
et al., JAMA Surgery, doi:10.1001/jamasurg.2013.3176, Feb 2014
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
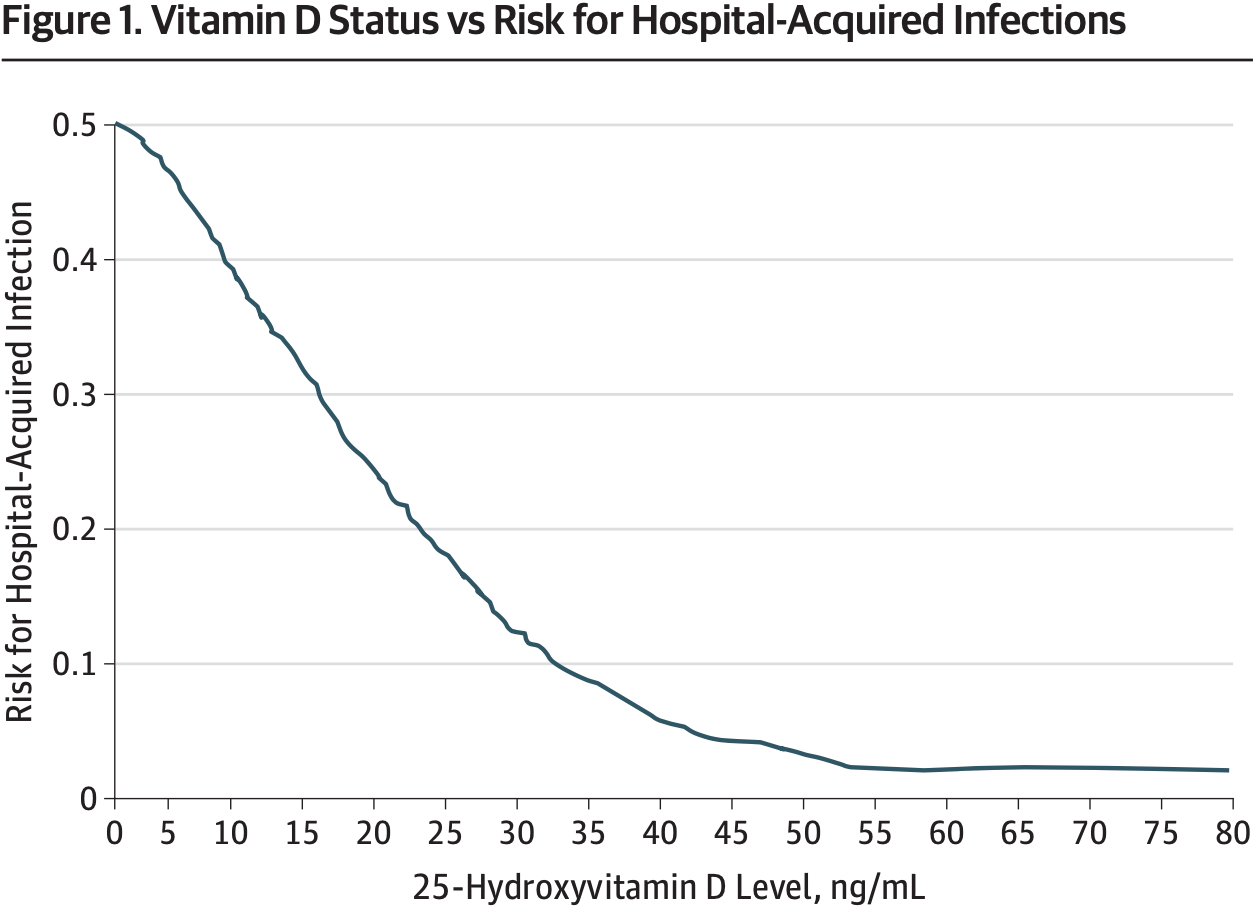
Retrospective 770 gastric bypass surgery patients showing a strong relationship between pre-operative vitamin D levels and the risk of hospital acquired infections.
Quraishi et al., 1 Feb 2014, peer-reviewed, 5 authors.
Association Between Preoperative 25-Hydroxyvitamin D Level and Hospital-Acquired Infections Following Roux-en-Y Gastric Bypass Surgery
JAMA Surgery, doi:10.1001/jamasurg.2013.3176
Postoperative hospital-acquired infections (HAIs) may result from disruption of natural barrier sites. Recent studies have linked vitamin D status and barrier site integrity. OBJECTIVE To investigate the association between preoperative vitamin D status and the risk for HAIs.
DESIGN, SETTING, AND PARTICIPANTS A retrospective analysis was performed using propensity score methods to construct a matched-pairs cohort to reduce baseline differences between patients with 25-hydroxyvitamin D (25[OH]D) levels less than 30 ng/mL vs 30 ng/mL or greater. Multivariable logistic regression analysis was then performed to examine the association between 25(OH)D levels and HAIs while adjusting for additional perioperative factors. Locally weighted scatterplot smoothing was used to depict the relationship between increasing 25(OH)D levels and the risk for HAIs. This study was conducted in a single, teaching hospital in Boston, Massachusetts, and involved 770 gastric bypass surgery patients between January 1, 2007, and December 31, 2011.
EXPOSURES Preoperative 25(OH)D levels. MAIN OUTCOMES AND MEASURES Association between preoperative 25(OH)D levels and the risk for postoperative HAIs.
RESULTS The risk for HAIs was 3-fold greater (adjusted odds ratio, 3.05; 95% CI, 1.34-6.94) in patients with 25(OH)D levels less than 30 ng/mL vs 30 ng/mL or greater. Further adjustment for additional perioperative factors did not materially change this association. Locally weighted scatterplot smoothing analysis depicted a near inverse linear relationship between vitamin D status and the risk for HAIs for 25(OH)D levels around 30 ng/mL.
CONCLUSIONS AND RELEVANCE In our patient cohort, a significant inverse association was observed between preoperative 25(OH)D levels and the risk for HAIs. These results suggest that preoperative 25(OH)D levels may be a modifiable risk factor for postoperative nosocomial infections. Prospective studies must determine whether there is a potential benefit to preoperative optimization of vitamin D status.
References
Acheson, Brookes, Spahn, Effects of allogeneic red blood cell transfusions on clinical outcomes in patients undergoing colorectal cancer surgery: a systematic review and meta-analysis, Ann Surg
Adams, Hewison, Unexpected actions of vitamin D: new perspectives on the regulation of innate and adaptive immunity, Nat Clin Pract Endocrinol Metab
Anderson, Surgical site infections, Infect Dis Clin North Am
Ata, Lee, Bestle, Desemone, Stain, Postoperative hyperglycemia and surgical site infection in general surgery patients, Arch Surg
Beltramini, Salata, Ray, Thermoregulation and risk of surgical site infection, Infect Control Hosp Epidemiol
Bhan, Camargo, Jr, Wenger, Circulating levels of 25-hydroxyvitamin D and human cathelicidin in healthy adults, J Allergy Clin Immunol
Cardinale, Mastrototaro, Cappiello, Immunological modifications induced from products used during the perioperative period, Int J Immunopathol Pharmacol
Chang, Lin, Lin, Lin, Anesthetic management and surgical site infections in total hip or knee replacement: a population-based study, Anesthesiology
Cleveland, Devlin, Locally weighted regression: an approach to regression analysis by local fitting, J Am Stat Assoc, doi:10.1080/01621459.1988.10478639
Cleveland, Robust locally weighted regression and smoothing scatterplots, J Am Stat Assoc, doi:10.1080/01621459.1979.10481038
Dixon, Barker, Mckinnon, Positive correlation between circulating cathelicidin antimicrobial peptide (hCAP18/LL-37) and 25-hydroxyvitamin D levels in healthy adults, BMC Res Notes
Dürr, Sudheendra, Ramamoorthy, LL-37, the only human member of the cathelicidin family of antimicrobial peptides, Biochim Biophys Acta
Fabri, Stenger, Shin, Vitamin D is required for IFN-gamma-mediated antimicrobial activity of human macrophages, Sci Transl Med
Fish, Beverstein, Olson, Reinhardt, Garren et al., Vitamin D status of morbidly obese bariatric surgery patients, J Surg Res
Flancbaum, Belsley, Drake, Colarusso, Tayler, Preoperative nutritional status of patients undergoing Roux-en-Y gastric bypass for morbid obesity, J Gastrointest Surg
Guggenbichler, Assadian, Boeswald, Kramer, Incidence and clinical implication of nosocomial infections associated with implantable biomaterials: catheters, ventilator-associated pneumonia, urinary tract infections, GMS Krankenhhyg Interdiszip
Holick, Binkley, Bischoff-Ferrari, Endocrine Society. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline, J Clin Endocrinol Metab
Holick, Vitamin D deficiency, N Engl J Med
Hooton, Bradley, Cardenas, None
Horan, Andrus, Dudeck, CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting, Am J Infect Control
Huttunen, Syrjänen, Obesity and the risk and outcome of infection, Int J Obes (Lond)
Infectious, Society, America, Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America, Clin Infect Dis
Jeng, Yamshchikov, Judd, Alterations in vitamin D status and anti-microbial peptide levels in patients in the intensive care unit with sepsis, J Transl Med
Kawasaki, Sata, Perioperative innate immunity and its modulation, J UOEH
Klevens, Edwards, Richards, Jr, Estimating health care-associated infections and deaths in U.S. hospitals, Public Health Rep
Liu, Stenger, Li, Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response, Science
Martone, Nichols, Recognition, prevention, surveillance, and management of surgical site infections: introduction to the problem and symposium overview, Clin Infect Dis
Nandipati, Lin, Husain, Factors predicting the increased risk for return to the operating room in bariatric patients: a NSQIP database study, Surg Endosc
Nguyen, Paya, Stevens, Mavandadi, Zainabadi et al., The relationship between hospital volume and outcome in bariatric surgery at academic medical centers, Ann Surg
Qadan, Akça, Mahid, Hornung, Polk, Perioperative supplemental oxygen therapy and surgical site infection: a meta-analysis of randomized controlled trials, Arch Surg
Qadan, Gardner, Vitale, Lominadze, Joshua et al., Hypothermia and surgery: immunologic mechanisms for current practice, Ann Surg
Quraishi, Camargo, Vitamin D and major chronic illness, J Restor Med
Quraishi, Camargo, Vitamin D in acute stress and critical illness, Curr Opin Clin Nutr Metab Care
Ranji, Shetty, Posley, Closing the Quality Gap: A Critical Analysis of Quality Improvement Strategies
Rassen, Shelat, Myers, Glynn, Rothman et al., One-to-many propensity score matching in cohort studies, Pharmacoepidemiol Drug Saf
Roberts, Scott, Ii, Hota, Costs attributable to healthcare-acquired infection in hospitalized adults and a comparison of economic methods, Med Care
Rubin, Estimating causal effects from large data sets using propensity scores, Ann Intern Med
Salkind, Rao, Antiobiotic prophylaxis to prevent surgical site infections, Am Fam Physician
Scott, The Direct Medical Costs of Healthcare-Associated Infections in US Hospitals and the Benefits of Prevention
Shokoohi, Stanworth, Mistry, Lamb, Staves et al., The risks of red cell transfusion for hip fracture surgery in the elderly, Vox Sang
Staehr, Meyhoff, Rasmussen, Group, Inspiratory oxygen fraction and postoperative complications in obese patients: a subgroup analysis of the PROXI trial, Anesthesiology
Steiner, Guo, Fraser, Propensity score analysis: statistical methods and applications, Psychometrika, doi:10.1007/s11336-010-9170-8
Thoracic, Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilatorassociated, and healthcare-associated pneumonia, Am J Respir Crit Care Med
Tollin, Bergman, Svenberg, Jörnvall, Gudmundsson et al., Antimicrobial peptides in the first line defence of human colon mucosa, Peptides
Von Dossow, Sander, Macgill, Spies, Perioperative cell-mediated immune response, Front Biosci
Welsh, Flanagan, Hoke, Doebbeling, Herwaldt, Agency for Healthcare Research and Quality Hospital-Acquired Infections Collaborative. Reducing health care-associated infections (HAIs): lessons learned from a national collaborative of regional HAI programs, Am J Infect Control
Youssef, Miller, El-Abbassi, Antimicrobial implications of vitamin D, Dermatoendocrinol
Youssef, Ranasinghe, Grant, Peiris, Vitamin D's potential to reduce the risk of hospital-acquired infections, Dermatoendocrinol
DOI record:
{
"DOI": "10.1001/jamasurg.2013.3176",
"ISSN": [
"2168-6254"
],
"URL": "http://dx.doi.org/10.1001/jamasurg.2013.3176",
"author": [
{
"affiliation": [
{
"name": "Massachusetts General Hospital, Harvard Medical School, Boston, Massachusetts"
}
],
"family": "Quraishi",
"given": "Sadeq A.",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Massachusetts General Hospital, Harvard Medical School, Boston, Massachusetts"
}
],
"family": "Bittner",
"given": "Edward A.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Massachusetts General Hospital, Harvard Medical School, Boston, Massachusetts"
}
],
"family": "Blum",
"given": "Livnat",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Massachusetts General Hospital, Harvard Medical School, Boston, Massachusetts"
}
],
"family": "Hutter",
"given": "Mathew M.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Massachusetts General Hospital, Harvard Medical School, Boston, Massachusetts"
}
],
"family": "Camargo",
"given": "Carlos A.",
"sequence": "additional",
"suffix": "Jr"
}
],
"container-title": "JAMA Surgery",
"container-title-short": "JAMA Surg",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2013,
11,
28
]
],
"date-time": "2013-11-28T00:06:35Z",
"timestamp": 1385597195000
},
"deposited": {
"date-parts": [
[
2016,
12,
15
]
],
"date-time": "2016-12-15T16:57:57Z",
"timestamp": 1481821077000
},
"indexed": {
"date-parts": [
[
2024,
3,
12
]
],
"date-time": "2024-03-12T16:31:06Z",
"timestamp": 1710261066545
},
"is-referenced-by-count": 52,
"issue": "2",
"issued": {
"date-parts": [
[
2014,
2,
1
]
]
},
"journal-issue": {
"issue": "2",
"published-print": {
"date-parts": [
[
2014,
2,
1
]
]
}
},
"language": "en",
"link": [
{
"URL": "http://jamanetwork.com/journals/jamasurgery/fullarticle/1782085",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "10",
"original-title": [],
"page": "112",
"prefix": "10.1001",
"published": {
"date-parts": [
[
2014,
2,
1
]
]
},
"published-print": {
"date-parts": [
[
2014,
2,
1
]
]
},
"publisher": "American Medical Association (AMA)",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "http://archsurg.jamanetwork.com/article.aspx?doi=10.1001/jamasurg.2013.3176"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Association Between Preoperative 25-Hydroxyvitamin D Level and Hospital-Acquired Infections Following Roux-en-Y Gastric Bypass Surgery",
"type": "journal-article",
"volume": "149"
}
