Vitamin-D levels and intensive care unit outcomes of a cohort of critically ill COVID-19 patients
et al., Clin Chem Lab Med, doi:10.1515/cclm-2020-1567, Jan 2021
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
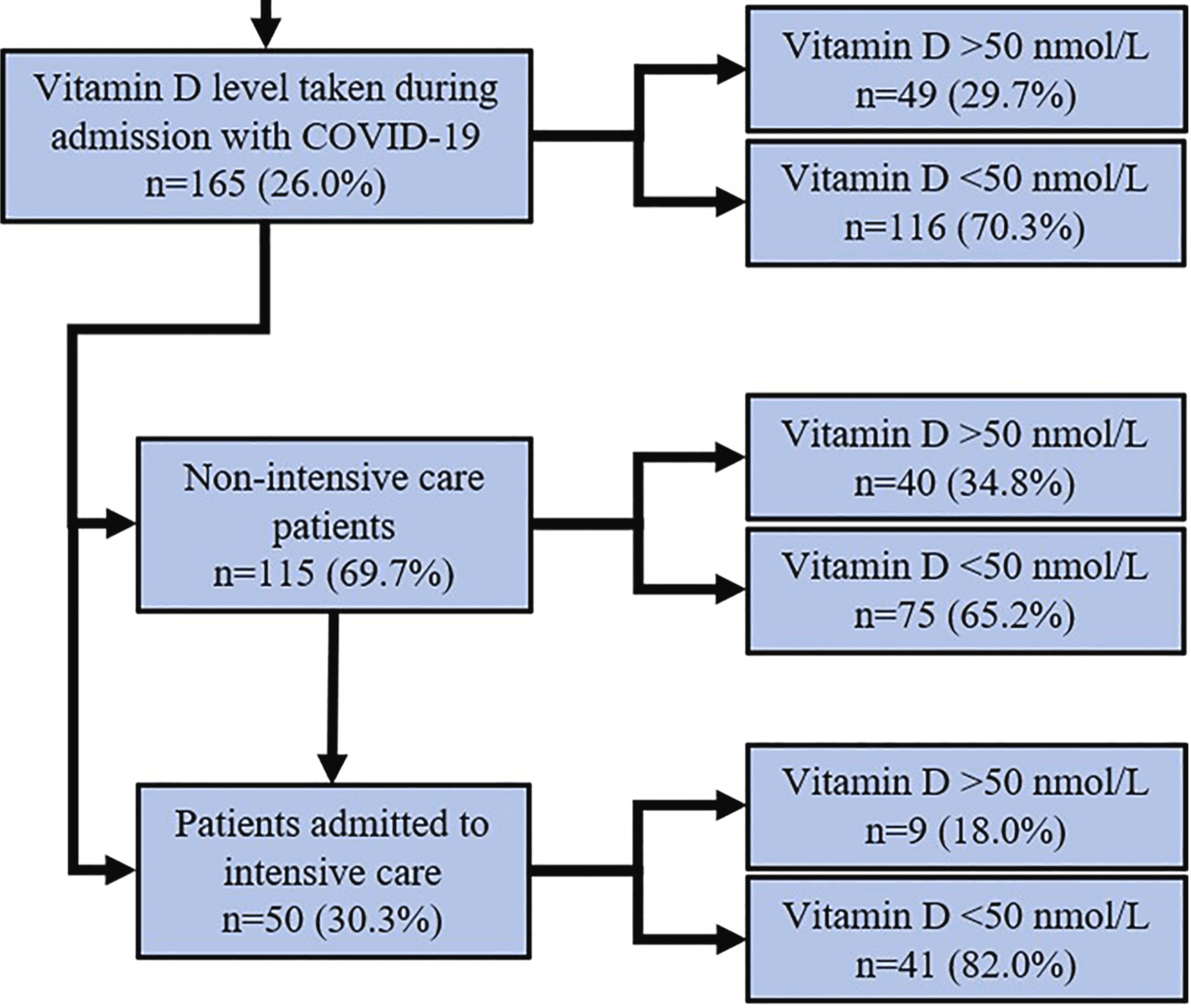
Retrospective 165 hospitalized patients with known vitamin D levels, showing an associated between vitamin D deficiency and ICU admission. There was no statistically significant difference in clinical outcomes for ICU patients. It's unclear why authors do not provide clinical outcomes for all patients rather than ICU only.
This is the 42nd of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
Standard of Care (SOC) for COVID-19 in the study country,
the United Kingdom, is very poor with very low average efficacy for approved treatments1.
The United Kingdom focused on expensive high-profit treatments, approving only one low-cost early treatment, which required a prescription and had limited adoption. The high-cost prescription treatment strategy reduces the probability of early treatment due to access and cost barriers, and eliminates complementary and synergistic benefits seen with many low-cost treatments.
|
risk of ICU admission, 58.8% lower, RR 0.41, p = 0.001, high D levels 9 of 40 (22.5%), low D levels 41 of 75 (54.7%), NNT 3.1, all hospitalized patients, >50 nmol/L.
|
|
risk of death, 24.1% lower, RR 0.76, p = 1.00, high D levels 1 of 9 (11.1%), low D levels 6 of 41 (14.6%), NNT 28, ICU patients only, >50 nmol/L.
|
|
risk of mechanical ventilation, 8.9% lower, RR 0.91, p = 0.70, high D levels 6 of 9 (66.7%), low D levels 30 of 41 (73.2%), NNT 15, ICU patients only, >50 nmol/L.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Orchard et al., 19 Jan 2021, retrospective, United Kingdom, peer-reviewed, 7 authors.
Vitamin-D levels and intensive care unit outcomes of a cohort of critically ill COVID-19 patients
Clinical Chemistry and Laboratory Medicine (CCLM), doi:10.1515/cclm-2020-1567
Objectives: The pattern of global COVID-19 has caused many to propose a possible link between susceptibility, severity and vitamin-D levels. Vitamin-D has known immune modulatory effects and deficiency has been linked to increased severity of viral infections. Methods: We evaluated patients admitted with confirmed SARS-COV-2 to our hospital between March-June 2020. Demographics and outcomes were assessed for those admitted to the intensive care unit (ICU) with normal (>50 nmol/L) and low (<50 nmol/L) vitamin-D. Results: There were 646 SARS-COV-2 PCR positive hospitalisations and 165 (25.5%) had plasma vitamin-D levels. Fifty patients were admitted to ICU. There was no difference in vitamin-D levels of those hospitalised (34, IQR 18.5-66 nmol/L) and those admitted to the ICU (31.5, IQR 21-42 nmol/L). Higher proportion of vitamin-D deficiency (<50 nmol/L) noted in the ICU group (82.0 vs. 65.2%). Among the ICU patients, low vitamin D level (<50 nmol/L) was associated with younger age (57 vs. 67 years, p=0.04) and lower cycle threshold (CT) real time polymerase chain reaction values (RT-PCR) (26.96 vs. 33.6, p=0.02) analogous to higher viral loads. However, there were no significant differences in ICU clinical outcomes (invasive and non-invasive mechanical ventilation, acute kidney injury and mechanical ventilation and hospital days) between patients with low and normal vitamin-D levels. Conclusions: Despite the association of low vitamin-D levels with low CT values, there is no difference in clinical outcomes in this small cohort of critically ill COVID-19 patients. The complex relationship between vitamin-D levels and COVID-19 infection needs further exploration with large scale randomized controlled trials.
References
Adams, Ren, Liu, Chun, Lagishetty et al., Vitamin D-directed rheostatic regulation of monocyte antibacterial responses, J Immunol
Almerighi, Sinistro, Cavazza, Ciaprini, Rocchi et al., 1alpha,25-dihydroxyvitamin D3 inhibits CD40L-induced pro-inflammatory and immunomodulatory activity in human monocytes, Cytokine
Anwar, Hamdy, Taher, Fawzy, Abdulattif et al., Burden and outcome of vitamin D deficiency among critically ill patients: a prospective study, Nutr Clin Pract
Aygun, Vitamin D can prevent COVID-19 infection-induced multiple organ damage, Naunyn-Schmiedeberg's Arch Pharmacol
Baktash, Hosack, Patel, Shah, Kandiah et al., Vitamin D status and outcomes for hospitalised older patients with COVID-19, Postgrad Med J, doi:10.1136/postgradmedj-2020-138712
Barlow, Svoboda, Mackellar, Nash, York et al., Antiviral activity and increased host defense against influenza infection elicited by the human cathelicidin LL-37, PloS One
Bates, Lennox, Prentice, Bates, Swan, National diet and nutrition survey
Chandran, Maung, Mithal, Parameswaran, Vitamin D in COVID-19: dousing the fire or averting the storm? -a perspective from the Asia-Pacific, Osteoporos Sarcopenia, doi:10.1016/j.afos.2020.07.003
Charoenngam, Holick, Immunologic effects of vitamin D on human health and disease, Nutrients, doi:10.3390/nu12072097
D'avolio, Avataneo, Manca, Cusato, Nicolò et al., 25-hhydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2, Nutrients, doi:10.3390/nu12051359
Dancer, Parekh, Lax, Souza, Zheng et al., Vitamin D deficiency contributes directly to the acute respiratory distress syndrome (ARDS), Thorax
Group, Dexamethasone in hospitalized patients with Covid-19 -preliminary report, N Engl J Med, doi:10.1056/NEJMoa2021436
Hastie, Mackay, Ho, Celis-Morales, Katikireddi et al., Vitamin D concentrations and COVID-19 infection in UK Biobank, Diabetes Metab Syndr
Hastie, Pell, Sattar, Vitamin D and COVID-19 infection and mortality in UK Biobank, Eur J Nutr, doi:10.1007/s00394-020-02372-4
Huang, Ran, Lv, Feng, Ran et al., Chronological changes of viral shedding in adult inpatients with COVID-19 in Wuhan, China, Clin Infect Dis, doi:10.1093/cid/ciaa631
Im, Je, Baek, Chung, Kwon et al., Nutritional status of patients with coronavirus disease 2019 (COVID-19), Int J Infect Dis, doi:10.1016/j.ijid.2020.08.018
Kellum, Lameire, Aspelin, Barsoum, Burdmann et al., Kidney disease: improving global outcomes (KDIGO) acute kidney injury work group. KDIGO clinical practice guideline for acute kidney injury, Kidney Int Suppl
Lofgren, Fefferman, Naumov, Gorski, Naumova, Influenza seasonality: underlying causes and modeling theories, J Virol
Meltzer, Best, Zhang, Vokes, Arora et al., Association of vitamin D deficiency and treatment with COVID-19 incidence, medRxiv, doi:10.1101/2020.05.08.20095893
Merzon, Tworowski, Gorohovski, Vinker, Cohen et al., Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli populationbased study, FEBS J, doi:10.1111/febs.15495
Mitchell, Vitamin-D and COVID-19: do deficient risk a poorer outcome?, Lancet Diabetes Endocrinol
Nice, COVID-19 rapid evidence summary: vitamin D for COVID-19 advice NICE
Panagiotou, Tee, Ihsan, Athar, Marchitelli et al., Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalised with COVID-19 are associated with greater disease severity, Clin Endocrinol, doi:10.1111/cen.14276
Pham, Rahman, Majidi, Waterhouse, Neale, Acute respiratory tract infection and 25-hydroxyvitamin D concentration: a systematic review and meta-analysis, Int J Environ Res Publ Health
Quesada-Gomez, Entrenas-Castillo, Bouillon, Vitamin D receptor stimulation to reduce acute respiratory distress syndrome (ARDS) in patients with coronavirus SARS-CoV-2 infections: revised Ms SBMB 2020_166, J Steroid Biochem Mol Biol
Raisi-Estabragh, Mccracken, Bethell, Cooper, Cooper et al., Greater risk of severe COVID-19 in Black, Asian and Minority Ethnic populations is not explained by cardiometabolic, socioeconomic or behavioural factors, or by 25(OH)-vitamin D status: study of 1,326 cases from the UK Biobank, J Public Health, doi:10.1093/pubmed/fdaa095
Rao, Manissero, Steele, Pareja, A narrative systematic review of the clinical utility of cycle threshold values in the context of COVID-19, Infect Dis Ther
Rech, Hunsaker, Rodriguez, Deficiency in 25-hydroxyvitamin D and 30-day mortality in patients with severe sepsis and septic shock, Am J Crit Care
Rosa, Malaguarnera, Nicoletti, Malaguarnera, Vitamin D3: a helpful immuno-modulator, Immunology
Tabary, Khanmohammadi, Araghi, Dadkhahfar, Tavangar, Pathologic features of COVID-19: a concise review, Pathol Res Pract
Weir, Thenappan, Bhargava, Chen, Does vitamin D deficiency increase the severity of COVID-19?, Clin Med
Xu, Yang, Chen, Luo, Zhang et al., Vitamin D alleviates lipopolysaccharide-induced acute lung injury via regulation of the renin-angiotensin system, Mol Med Rep
Yu, Yan, Wang, Yang, Wang et al., Quantitative detection and viral load analysis of SARS-CoV-2 in infected patients, Clin Infect Dis, doi:10.1093/cid/ciaa345
Yuki, Fujiogi, Koutsogiannaki, COVID-19 pathophysiology: a review, Clin Immunol
Zhang, Leung, Richers, Liu, Remigio et al., Vitamin D inhibits monocyte/macrophage proinflammatory cytokine production by targeting MAPK phosphatase-1, J Immunol
DOI record:
{
"DOI": "10.1515/cclm-2020-1567",
"ISSN": [
"1434-6621",
"1437-4331"
],
"URL": "http://dx.doi.org/10.1515/cclm-2020-1567",
"abstract": "<jats:title>Abstract</jats:title>\n <jats:sec id=\"j_cclm-2020-1567_abs_001\">\n <jats:title>Objectives</jats:title>\n <jats:p>The pattern of global COVID-19 has caused many to propose a possible link between susceptibility, severity and vitamin-D levels. Vitamin-D has known immune modulatory effects and deficiency has been linked to increased severity of viral infections.</jats:p>\n </jats:sec>\n <jats:sec id=\"j_cclm-2020-1567_abs_002\">\n <jats:title>Methods</jats:title>\n <jats:p>We evaluated patients admitted with confirmed SARS-COV-2 to our hospital between March-June 2020. Demographics and outcomes were assessed for those admitted to the intensive care unit (ICU) with normal (>50 nmol/L) and low (<50 nmol/L) vitamin-D.</jats:p>\n </jats:sec>\n <jats:sec id=\"j_cclm-2020-1567_abs_003\">\n <jats:title>Results</jats:title>\n <jats:p>There were 646 SARS-COV-2 PCR positive hospitalisations and 165 (25.5%) had plasma vitamin-D levels. Fifty patients were admitted to ICU. There was no difference in vitamin-D levels of those hospitalised (34, IQR 18.5–66 nmol/L) and those admitted to the ICU (31.5, IQR 21–42 nmol/L). Higher proportion of vitamin-D deficiency (<50 nmol/L) noted in the ICU group (82.0 vs. 65.2%). Among the ICU patients, low vitamin D level (<50 nmol/L) was associated with younger age (57 vs. 67 years, p=0.04) and lower cycle threshold (CT) real time polymerase chain reaction values (RT-PCR) (26.96 vs. 33.6, p=0.02) analogous to higher viral loads. However, there were no significant differences in ICU clinical outcomes (invasive and non-invasive mechanical ventilation, acute kidney injury and mechanical ventilation and hospital days) between patients with low and normal vitamin-D levels.</jats:p>\n </jats:sec>\n <jats:sec id=\"j_cclm-2020-1567_abs_004\">\n <jats:title>Conclusions</jats:title>\n <jats:p>Despite the association of low vitamin-D levels with low CT values, there is no difference in clinical outcomes in this small cohort of critically ill COVID-19 patients. The complex relationship between vitamin-D levels and COVID-19 infection needs further exploration with large scale randomized controlled trials.</jats:p>\n </jats:sec>",
"alternative-id": [
"10.1515/cclm-2020-1567"
],
"author": [
{
"affiliation": [
{
"name": "General Intensive Care Unit , University Hospital Southampton NHS Foundation Trust , Southampton , UK"
}
],
"family": "Orchard",
"given": "Laurence",
"sequence": "first"
},
{
"affiliation": [
{
"name": "General Intensive Care Unit , University Hospital Southampton NHS Foundation Trust , Southampton , UK"
}
],
"family": "Baldry",
"given": "Matthew",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "General Intensive Care Unit , University Hospital Southampton NHS Foundation Trust , Southampton , UK"
}
],
"family": "Nasim-Mohi",
"given": "Myra",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Southampton Specialist Virology Centre , University of Southampton School of Medicine, University Hospital Southampton NHS Foundation Trust , Southampton , UK"
}
],
"family": "Monck",
"given": "Chantelle",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Microbiology Innovation and Research Unit, Department of Microbiology , University Hospital Southampton NHS Foundation Trust , Southampton , UK"
},
{
"name": "Faculty of Medicine , University of Southampton University, Hospital Southampton , Southampton , UK"
}
],
"family": "Saeed",
"given": "Kordo",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "General Intensive Care Unit , University Hospital Southampton NHS Foundation Trust , Southampton , UK"
},
{
"name": "Faculty of Medicine , University of Southampton University, Hospital Southampton , Southampton , UK"
},
{
"name": "NIHR Southampton Clinical Research Facility and NIHR Southampton Biomedical Research Centre , University Hospital Southampton/University of Southampton , Southampton , UK"
}
],
"family": "Grocott",
"given": "Michael P. W.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "General Intensive Care Unit , University Hospital Southampton NHS Foundation Trust , Southampton , UK"
},
{
"name": "Faculty of Medicine , University of Southampton University, Hospital Southampton , Southampton , UK"
},
{
"name": "NIHR Southampton Clinical Research Facility and NIHR Southampton Biomedical Research Centre , University Hospital Southampton/University of Southampton , Southampton , UK"
}
],
"family": "Ahilanandan",
"given": "Dushianthan",
"sequence": "additional"
}
],
"container-title": "Clinical Chemistry and Laboratory Medicine (CCLM)",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
1,
23
]
],
"date-time": "2021-01-23T06:33:46Z",
"timestamp": 1611383626000
},
"deposited": {
"date-parts": [
[
2021,
8,
22
]
],
"date-time": "2021-08-22T02:04:42Z",
"timestamp": 1629597882000
},
"indexed": {
"date-parts": [
[
2024,
2,
21
]
],
"date-time": "2024-02-21T09:44:19Z",
"timestamp": 1708508659716
},
"is-referenced-by-count": 30,
"issue": "6",
"issued": {
"date-parts": [
[
2021,
1,
19
]
]
},
"journal-issue": {
"issue": "6",
"published-online": {
"date-parts": [
[
2021,
1,
15
]
]
},
"published-print": {
"date-parts": [
[
2021,
5,
26
]
]
}
},
"language": "en",
"link": [
{
"URL": "https://www.degruyter.com/view/journals/cclm/ahead-of-print/article-10.1515-cclm-2020-1567/article-10.1515-cclm-2020-1567.xml",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.degruyter.com/document/doi/10.1515/cclm-2020-1567/xml",
"content-type": "application/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.degruyter.com/document/doi/10.1515/cclm-2020-1567/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "374",
"original-title": [],
"page": "1155-1163",
"prefix": "10.1515",
"published": {
"date-parts": [
[
2021,
1,
19
]
]
},
"published-online": {
"date-parts": [
[
2021,
1,
19
]
]
},
"published-print": {
"date-parts": [
[
2021,
5,
26
]
]
},
"publisher": "Walter de Gruyter GmbH",
"reference": [
{
"DOI": "10.1016/j.prp.2020.153097",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_001",
"unstructured": "Tabary, M, Khanmohammadi, S, Araghi, F, Dadkhahfar, S, Tavangar, S. Pathologic features of COVID-19: a concise review. Pathol Res Pract 2020;216:153097. https://doi.org/10.1016/j.prp.2020.153097."
},
{
"DOI": "10.1056/NEJMoa2021436",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_002",
"unstructured": "Group, TRC. Dexamethasone in hospitalized patients with Covid-19 — preliminary report. N Engl J Med 2020 Jul 17. https://doi.org/10.1056/NEJMoa2021436 [Epub ahead of print]."
},
{
"DOI": "10.1016/j.clim.2020.108427",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_003",
"unstructured": "Yuki, K, Fujiogi, M, Koutsogiannaki, S. COVID-19 pathophysiology: a review. Clin Immunol 2020;215:108427. https://doi.org/10.1016/j.clim.2020.108427."
},
{
"DOI": "10.1016/j.afos.2020.07.003",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_004",
"unstructured": "Chandran, M, Maung, AC, Mithal, A, Parameswaran, R. Vitamin D in COVID-19: dousing the fire or averting the storm? – a perspective from the Asia-Pacific. Osteoporos Sarcopenia 2020 Jul 23. https://doi.org/10.1016/j.afos.2020.07.003 [Epub ahead of print]."
},
{
"DOI": "10.1016/j.ijid.2020.08.018",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_005",
"unstructured": "Im, JH, Je, YS, Baek, J, Chung, MH, Kwon, HY, Lee, JS. Nutritional status of patients with coronavirus disease 2019 (COVID-19). Int J Infect Dis 2020 Aug 11. https://doi.org/10.1016/j.ijid.2020.08.018 [Epub ahead of print]."
},
{
"DOI": "10.1016/S2213-8587(20)30183-2",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_006",
"unstructured": "Mitchell, F. Vitamin-D and COVID-19: do deficient risk a poorer outcome? Lancet Diabetes Endocrinol 2020;8:570. https://doi.org/10.1016/s2213-8587(20)30183-2."
},
{
"DOI": "10.7861/clinmed.2020-0301",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_007",
"unstructured": "Weir, EK, Thenappan, T, Bhargava, M, Chen, Y. Does vitamin D deficiency increase the severity of COVID-19? Clin Med 2020;20:e107–8. https://doi.org/10.7861/clinmed.2020-0301."
},
{
"DOI": "10.3390/ijerph16173020",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_008",
"unstructured": "Pham, H, Rahman, A, Majidi, A, Waterhouse, M, Neale, RE. Acute respiratory tract infection and 25-hydroxyvitamin D concentration: a systematic review and meta-analysis. Int J Environ Res Publ Health 2019;16:3020. https://doi.org/10.3390/ijerph16173020."
},
{
"DOI": "10.1128/JVI.01680-06",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_009",
"unstructured": "Lofgren, E, Fefferman, NH, Naumov, YN, Gorski, J, Naumova, EN. Influenza seasonality: underlying causes and modeling theories. J Virol 2007;81:5429–36. https://doi.org/10.1128/jvi.01680-06."
},
{
"key": "2021082201593403749_j_cclm-2020-1567_ref_010",
"unstructured": "NICE. COVID-19 rapid evidence summary: vitamin D for COVID-19 advice NICE. Available from: https://www.nice.org.uk/advice/es28/chapter/Key-messages [Accessed 7 Sep 2020]."
},
{
"DOI": "10.1038/kisup.2012.1",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_011",
"unstructured": "Kellum, JA, Lameire, N, Aspelin, P, Barsoum, RS, Burdmann, EA, Goldstein, SL, et al.. Kidney disease: improving global outcomes (KDIGO) acute kidney injury work group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl 2012;2:1–138. https://doi.org/10.1038/kisup.2012.1."
},
{
"key": "2021082201593403749_j_cclm-2020-1567_ref_012",
"unstructured": "Bates, B, Lennox, A, Prentice, A, Bates, C, Swan, G. National diet and nutrition survey; 2011. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/207708/NDNS-Y3-report_All-TEXT-docs-combined.pdf."
},
{
"DOI": "10.1111/cen.14276",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_013",
"unstructured": "Panagiotou, G, Tee, SA, Ihsan, Y, Athar, W, Marchitelli, G, Kelly, D, et al.. Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalised with COVID-19 are associated with greater disease severity. Clin Endocrinol 2020 Jul 3. https://doi.org/10.1111/cen.14276 [Epub ahead of print]."
},
{
"DOI": "10.1136/thoraxjnl-2014-206680",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_014",
"unstructured": "Dancer, RCA, Parekh, D, Lax, S, D’Souza, V, Zheng, S, Bassford, CR, et al.. Vitamin D deficiency contributes directly to the acute respiratory distress syndrome (ARDS). Thorax 2015;70:617–24. https://doi.org/10.1136/thoraxjnl-2014-206680."
},
{
"DOI": "10.4037/ajcc2014723",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_015",
"unstructured": "Rech, MA, Hunsaker, T, Rodriguez, J. Deficiency in 25-hydroxyvitamin D and 30-day mortality in patients with severe sepsis and septic shock. Am J Crit Care 2014;23:e72–9. https://doi.org/10.4037/ajcc2014723."
},
{
"DOI": "10.1177/0884533616671741",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_016",
"unstructured": "Anwar, E, Hamdy, G, Taher, E, Fawzy, E, Abdulattif, S, Attia, MH. Burden and outcome of vitamin D deficiency among critically ill patients: a prospective study. Nutr Clin Pract 2017;32:378–84. https://doi.org/10.1177/0884533616671741."
},
{
"DOI": "10.21203/rs.3.rs-41867/v1",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_017",
"unstructured": "Rao, SN, Manissero, D, Steele, VR, Pareja, J. A narrative systematic review of the clinical utility of cycle threshold values in the context of COVID-19. Infect Dis Ther 2020;9:1–14. https://doi.org/10.1007/s40121-020-00324-3."
},
{
"DOI": "10.1093/cid/ciaa631",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_018",
"unstructured": "Huang, J-T, Ran, R-X, Lv, Z-H, Feng, LN, Ran, CY, Tong, YQ, et al.. Chronological changes of viral shedding in adult inpatients with COVID-19 in Wuhan, China. Clin Infect Dis 2020 May 23. https://doi.org/10.1093/cid/ciaa631 [Epub ahead of print]."
},
{
"DOI": "10.1093/cid/ciaa345",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_019",
"unstructured": "Yu, F, Yan, L, Wang, N, Yang, S, Wang, L, Tang, Y, et al.. Quantitative detection and viral load analysis of SARS-CoV-2 in infected patients. Clin Infect Dis 2020 Mar 28. https://doi.org/10.1093/cid/ciaa345 [Epub ahead of print]."
},
{
"DOI": "10.1007/s00210-020-01911-4",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_020",
"unstructured": "Aygun, H. Vitamin D can prevent COVID-19 infection-induced multiple organ damage. Naunyn-Schmiedeberg’s Arch Pharmacol 2020;393:1157–60. https://doi.org/10.1007/s00210-020-01911-4."
},
{
"DOI": "10.3892/mmr.2017.7546",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_021",
"unstructured": "Xu, J, Yang, J, Chen, J, Luo, Q, Zhang, Q, Zhang, H. Vitamin D alleviates lipopolysaccharide-induced acute lung injury via regulation of the renin-angiotensin system. Mol Med Rep 2017;16:7432. https://doi.org/10.3892/mmr.2017.7546."
},
{
"DOI": "10.1016/j.jsbmb.2020.105719",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_022",
"unstructured": "Quesada-Gomez, JM, Entrenas-Castillo, M, Bouillon, R. Vitamin D receptor stimulation to reduce acute respiratory distress syndrome (ARDS) in patients with coronavirus SARS-CoV-2 infections: revised Ms SBMB 2020_166. J Steroid Biochem Mol Biol 2020;202:105719. https://doi.org/10.1016/j.jsbmb.2020.105719."
},
{
"DOI": "10.3390/nu12072097",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_023",
"unstructured": "Charoenngam, N, Holick, MF. Immunologic effects of vitamin D on human health and disease. Nutrients 2020 Jul 15;12. https://doi.org/10.3390/nu12072097 [Epub ahead of print]."
},
{
"DOI": "10.4049/jimmunol.0803736",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_024",
"unstructured": "Adams, JS, Ren, S, Liu, PT, Chun, RF, Lagishetty, V, Gombart, AF, et al.. Vitamin D-directed rheostatic regulation of monocyte antibacterial responses. J Immunol 2009;182:4289–95. https://doi.org/10.4049/jimmunol.0803736."
},
{
"DOI": "10.1016/j.cyto.2008.12.009",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_025",
"unstructured": "Almerighi, C, Sinistro, A, Cavazza, A, Ciaprini, C, Rocchi, G, Bergamini, A, et al.. 1alpha,25-dihydroxyvitamin D3 inhibits CD40L-induced pro-inflammatory and immunomodulatory activity in human monocytes. Cytokine 2009;45:190–7. https://doi.org/10.1016/j.cyto.2008.12.009."
},
{
"DOI": "10.4049/jimmunol.1102412",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_026",
"unstructured": "Zhang, Y, Leung, DYM, Richers, BN, Liu, Y, Remigio, LK, Riches, DW, et al.. Vitamin D inhibits monocyte/macrophage proinflammatory cytokine production by targeting MAPK phosphatase-1. J Immunol 2012;188:2127–35. https://doi.org/10.4049/jimmunol.1102412."
},
{
"DOI": "10.1111/j.1365-2567.2011.03482.x",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_027",
"unstructured": "Di Rosa, M, Malaguarnera, M, Nicoletti, F, Malaguarnera, L. Vitamin D3: a helpful immuno-modulator. Immunology 2011;134:123–39. https://doi.org/10.1111/j.1365-2567.2011.03482.x."
},
{
"DOI": "10.1371/journal.pone.0025333",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_028",
"unstructured": "Barlow, PG, Svoboda, P, Mackellar, A, Nash, AA, York, I, Pohl, J, et al.. Antiviral activity and increased host defense against influenza infection elicited by the human cathelicidin LL-37. PloS One 2011;6:e25333. https://doi.org/10.1371/journal.pone.0025333."
},
{
"DOI": "10.1101/2020.05.08.20095893",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_029",
"unstructured": "Meltzer, DO, Best, TJ, Zhang, H, Vokes, T, Arora, V, Solway, J. Association of vitamin D deficiency and treatment with COVID-19 incidence. medRxiv 2020 May 13. https://doi.org/10.1101/2020.05.08.20095893 [Epub ahead of print]."
},
{
"DOI": "10.3390/nu12051359",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_030",
"unstructured": "D’Avolio, A, Avataneo, V, Manca, A, Cusato, J, De Nicolò, A, Lucchini, R, et al.. 25-hhydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2. Nutrients 2020 May 9;12. https://doi.org/10.3390/nu12051359 [Epub ahead of print]."
},
{
"DOI": "10.1101/2020.07.01.20144329",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_031",
"unstructured": "Merzon, E, Tworowski, D, Gorohovski, A, Vinker, S, Cohen, AG, Green, I, et al.. Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study. FEBS J 2020 Jul 23. https://doi.org/10.1111/febs.15495 [Epub ahead of print]."
},
{
"DOI": "10.1016/j.dsx.2020.07.021",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_032",
"unstructured": "Hastie, CE, Mackay, DF, Ho, F, Celis-Morales, CA, Katikireddi, SV, Niedzwiedz, CL, et al.. Vitamin D concentrations and COVID-19 infection in UK Biobank. Diabetes Metab Syndr 2020;14:561–5. https://doi.org/10.1016/j.dsx.2020.04.050."
},
{
"DOI": "10.1101/2020.06.26.20140921",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_033",
"unstructured": "Hastie, CE, Pell, JP, Sattar, N. Vitamin D and COVID-19 infection and mortality in UK Biobank. Eur J Nutr 2020 Aug 26. https://doi.org/10.1007/s00394-020-02372-4 [Epub ahead of print]."
},
{
"DOI": "10.1101/2020.06.01.20118943",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_034",
"unstructured": "Raisi-Estabragh, Z, McCracken, C, Bethell, MS, Cooper, J, Cooper, C, Caulfield, MJ, et al.. Greater risk of severe COVID-19 in Black, Asian and Minority Ethnic populations is not explained by cardiometabolic, socioeconomic or behavioural factors, or by 25(OH)-vitamin D status: study of 1,326 cases from the UK Biobank. J Public Health 2020 Jun 19. https://doi.org/10.1093/pubmed/fdaa095 [Epub ahead of print]."
},
{
"DOI": "10.1136/postgradmedj-2020-138712",
"doi-asserted-by": "crossref",
"key": "2021082201593403749_j_cclm-2020-1567_ref_035",
"unstructured": "Baktash, V, Hosack, T, Patel, N, Shah, S, Kandiah, P, Van Den Abbeele, K, et al.. Vitamin D status and outcomes for hospitalised older patients with COVID-19. Postgrad Med J 2020 Aug 27. https://doi.org/10.1136/postgradmedj-2020-138712 [Epub ahead of print]."
}
],
"reference-count": 35,
"references-count": 35,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.degruyter.com/document/doi/10.1515/cclm-2020-1567/html"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Biochemistry (medical)",
"Clinical Biochemistry",
"General Medicine"
],
"subtitle": [],
"title": "Vitamin-D levels and intensive care unit outcomes of a cohort of critically ill COVID-19 patients",
"type": "journal-article",
"volume": "59"
}
