Quercetin inhibited LPS-induced cytokine storm by interacting with the AKT1-FoxO1 and Keap1-Nrf2 signaling pathway in macrophages
et al., Scientific Reports, doi:10.1038/s41598-024-71569-y, Sep 2024
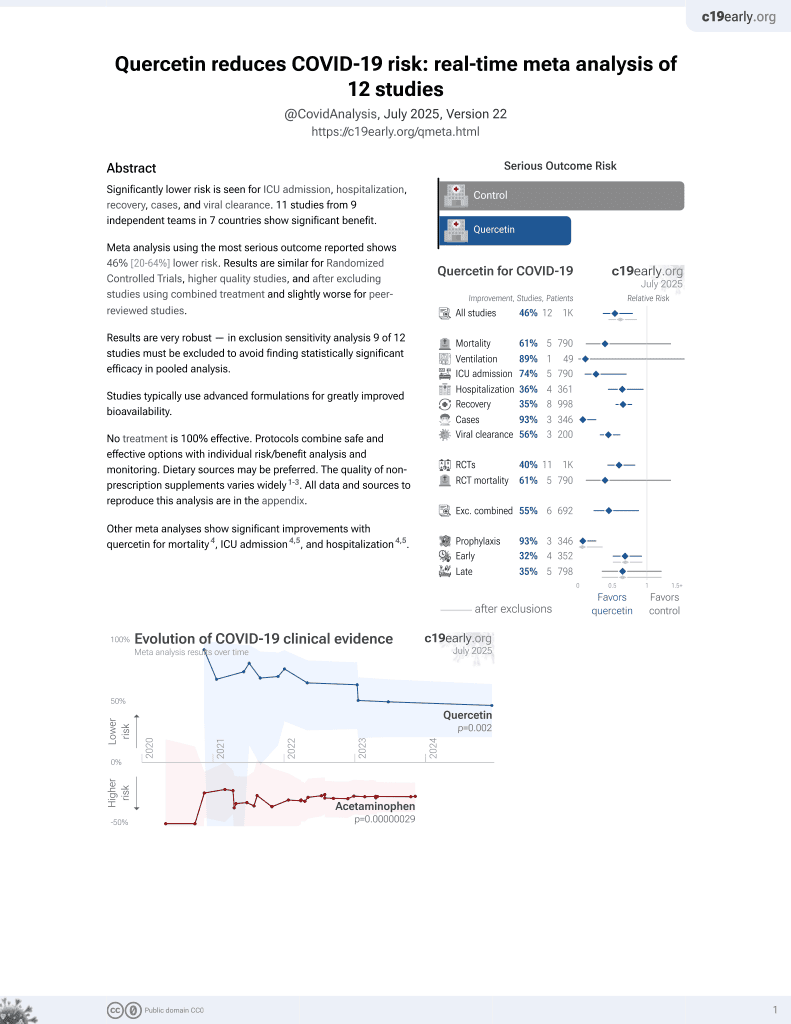
Quercetin for COVID-19
36th treatment shown to reduce risk in
January 2022, now with p = 0.0018 from 9 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
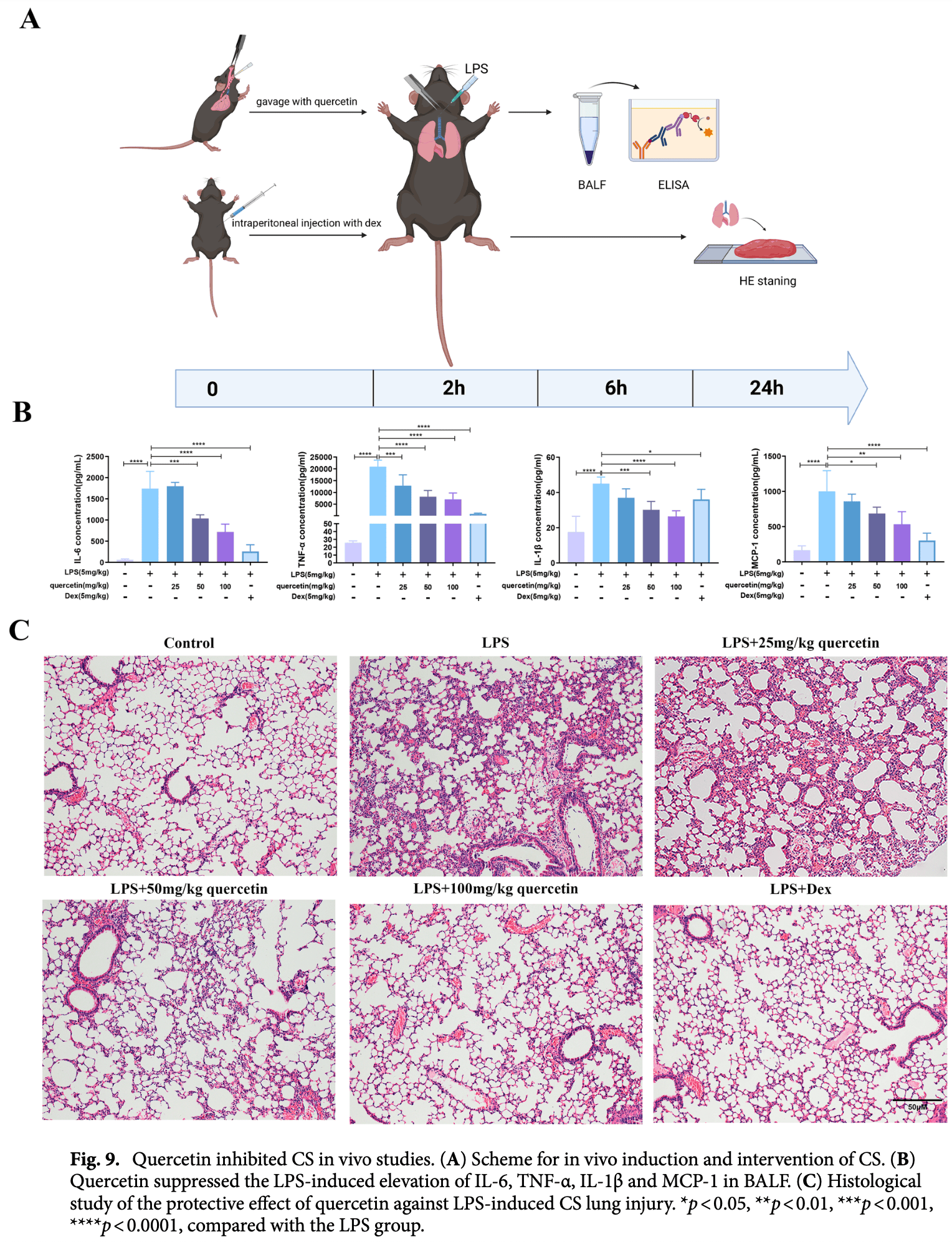
In silico, in vitro, and mouse study showing that quercetin inhibits LPS-induced cytokine storm by interacting with the AKT1-FoxO1 and Keap1-Nrf2 signaling pathways in macrophages. Authors found quercetin effectively suppressed the overexpression of pro-inflammatory mediators like IL-6, TNF-α, IL-1β, and MCP-1 in LPS-stimulated Raw264.7 cells and in vivo in C57BL/6 mice. Quercetin regulated the AKT1-FoxO1 pathway by increasing AKT1 phosphorylation and inhibiting FoxO1 nuclear translocation, thereby reducing inflammatory gene expression. It also activated the Keap1-Nrf2 pathway, decreasing intracellular reactive oxygen species (ROS) levels and oxidative stress. Molecular docking showed quercetin had the strongest binding affinity to AKT1 among potential targets. In mice, quercetin pretreatment reduced inflammatory factors in bronchoalveolar lavage fluid and ameliorated LPS-induced lung tissue damage. The study suggests quercetin's potential as a therapeutic agent for cytokine storm, by modulating key inflammatory and antioxidant pathways in macrophages.
Bioavailability. Quercetin has low bioavailability and studies typically use advanced formulations to improve bioavailability which may be required to reach therapeutic concentrations.
91 preclinical studies support the efficacy of quercetin for COVID-19:
In silico studies predict inhibition of SARS-CoV-2, or minimization of side effects, with quercetin or metabolites via binding to the spikeA,11,12,18,19,32,34,35,37,40,48,49,51,52,75 (and specifically the receptor binding domainB,8), MproC,7,8,11,12,16,18,20,22,24,26,28,30,33,34,37,40,44,46-48,52-55,72 , RNA-dependent RNA polymeraseD,8,10-12,18,42 , PLproE,12,47,55 , ACE2F,27,32,33,37,38,47,51 , TMPRSS2G,32, nucleocapsidH,12, helicaseI,12,39,44 , endoribonucleaseJ,49, NSP16/10K,15, cathepsin LL,36, Wnt-3M,32, FZDN,32, LRP6O,32, ezrinP,50, ADRPQ,48, NRP1R,51, EP300S,25, PTGS2T,33, HSP90AA1U,25,33 , matrix metalloproteinase 9V,41, IL-6W,31,45 , IL-10X,31, VEGFAY,45, and RELAZ,45 proteins, and inhibition of spike-ACE2 interactionAA,9.
In vitro studies demonstrate inhibition of the MproC,24,58,63,71 protein, and inhibition of spike-ACE2 interactionAA,59.
In vitro studies demonstrate efficacy in Calu-3AB,62, A549AC,31, HEK293-ACE2+AD,70, Huh-7AE,35, Caco-2AF,61, Vero E6AG,29,52,61 , mTECAH,64, RAW264.7AI,64, and HLMECAJ,9 cells.
Animal studies demonstrate efficacy in K18-hACE2 miceAK,67, db/db miceAL,64,74 , BALB/c miceAM,73, and rats29.
Quercetin reduced proinflammatory cytokines and protected lung and kidney tissue against LPS-induced damage in mice73, inhibits LPS-induced cytokine storm by modulating key inflammatory and antioxidant pathways in macrophages14, may block ACE2-spike interaction and NLRP3 inflammasome, limiting viral entry and inflammation5, upregulates the SIRT1/AMPK axis to inhibit oxidative injury and accelerate viral clearance76, inhibits SARS-CoV-2 ORF3a ion channel activity, which contributes to viral pathogenicity and cytotoxicity66, may alleviate COVID-19 ARDS via inhibition of EGFR and JAK2 inflammatory targets1, may destabilize the Spike protein, IL-6R, and integrins via conserved residues, blocking viral entry, hyperinflammation, and platelet aggregation77, and may reduce COVID-19 neuroinflammation and cognitive dysfunction through anti-inflammatory mechanisms and neuroprotective effects78.
1.
Gupta et al., Harnessing phytoconstituents to treat COVID-19 triggered acute respiratory distress syndrome: Insights from network pharmacology, and molecular modeling, Phytochemistry Letters, doi:10.1016/j.phytol.2025.104105.
2.
Sun et al., Feasibility of the inhibitor development for SARS-CoV-2: a systematic approach for drug design, Journal of Molecular Modeling, doi:10.1007/s00894-025-06541-2.
3.
Torabfam et al., Improving quercetin solubility via structural modification enhances dual-target coronavirus entry: an integrated in-vitro and in-silico study, Scientific Reports, doi:10.1038/s41598-025-27374-2.
4.
Abdelhameed et al., Phytochemical and antiviral investigation of Cynanchum acutum L. extract and derived semi-synthetic analogs targeting SARS-CoV-2 main protease, Future Journal of Pharmaceutical Sciences, doi:10.1186/s43094-025-00907-2.
5.
Manikyam et al., INP-Guided Network Pharmacology Discloses Multi-Target Therapeutic Strategy Against Cytokine and IgE Storms in the SARS-CoV-2 NB.1.8.1 Variant, Research Square, doi:10.21203/rs.3.rs-6819274/v1.
6.
Makoana et al., Integration of metabolomics and chemometrics with in-silico and in-vitro approaches to unravel SARS-Cov-2 inhibitors from South African plants, PLOS ONE, doi:10.1371/journal.pone.0320415.
7.
Bano et al., Biochemical Screening of Phytochemicals and Identification of Scopoletin as a Potential Inhibitor of SARS-CoV-2 Mpro, Revealing Its Biophysical Impact on Structural Stability, Viruses, doi:10.3390/v17030402.
8.
Rajamanickam et al., Exploring the Potential of Siddha Formulation MilagaiKudineer-Derived Phytotherapeutics Against SARS-CoV-2: An In-Silico Investigation for Antiviral Intervention, Journal of Pharmacy and Pharmacology Research, doi:10.26502/fjppr.0105.
9.
Moharram et al., Secondary metabolites of Alternaria alternate appraisal of their SARS-CoV-2 inhibitory and anti-inflammatory potentials, PLOS ONE, doi:10.1371/journal.pone.0313616.
10.
Metwaly et al., Integrated study of Quercetin as a potent SARS-CoV-2 RdRp inhibitor: Binding interactions, MD simulations, and In vitro assays, PLOS ONE, doi:10.1371/journal.pone.0312866.
11.
Al balawi et al., Assessing multi-target antiviral and antioxidant activities of natural compounds against SARS-CoV-2: an integrated in vitro and in silico study, Bioresources and Bioprocessing, doi:10.1186/s40643-024-00822-z.
12.
Haque et al., Exploring potential therapeutic candidates against COVID-19: a molecular docking study, Discover Molecules, doi:10.1007/s44345-024-00005-5.
13.
Pan et al., Decoding the mechanism of Qingjie formula in the prevention of COVID-19 based on network pharmacology and molecular docking, Heliyon, doi:10.1016/j.heliyon.2024.e39167.
14.
Xu et al., Quercetin inhibited LPS-induced cytokine storm by interacting with the AKT1-FoxO1 and Keap1-Nrf2 signaling pathway in macrophages, Scientific Reports, doi:10.1038/s41598-024-71569-y.
15.
Tamil Selvan et al., Computational Investigations to Identify Potent Natural Flavonoid Inhibitors of the Nonstructural Protein (NSP) 16/10 Complex Against Coronavirus, Cureus, doi:10.7759/cureus.68098.
16.
Sunita et al., Characterization of Phytochemical Inhibitors of the COVID-19 Primary Protease Using Molecular Modelling Approach, Asian Journal of Microbiology and Biotechnology, doi:10.56557/ajmab/2024/v9i28800.
17.
Wu et al., Biomarkers Prediction and Immune Landscape in Covid-19 and “Brain Fog”, Elsevier BV, doi:10.2139/ssrn.4897774.
18.
Raman et al., Phytoconstituents of Citrus limon (Lemon) as Potential Inhibitors Against Multi Targets of SARS‐CoV‐2 by Use of Molecular Modelling and In Vitro Determination Approaches, ChemistryOpen, doi:10.1002/open.202300198.
19.
Asad et al., Exploring the antiviral activity of Adhatoda beddomei bioactive compounds in interaction with coronavirus spike protein, Archives of Medical Reports, 1:1, archmedrep.com/index.php/amr/article/view/3.
20.
Irfan et al., Phytoconstituents of Artemisia Annua as potential inhibitors of SARS CoV2 main protease: an in silico study, BMC Infectious Diseases, doi:10.1186/s12879-024-09387-w.
21.
Yuan et al., Network pharmacology and molecular docking reveal the mechanisms of action of Panax notoginseng against post-COVID-19 thromboembolism, Review of Clinical Pharmacology and Pharmacokinetics - International Edition, doi:10.61873/DTFA3974.
22.
Nalban et al., Targeting COVID-19 (SARS-CoV-2) main protease through phytochemicals of Albizia lebbeck: molecular docking, molecular dynamics simulation, MM–PBSA free energy calculations, and DFT analysis, Journal of Proteins and Proteomics, doi:10.1007/s42485-024-00136-w.
23.
Zhou et al., Bioinformatics and system biology approaches to determine the connection of SARS-CoV-2 infection and intrahepatic cholangiocarcinoma, PLOS ONE, doi:10.1371/journal.pone.0300441.
24.
Waqas et al., Discovery of Novel Natural Inhibitors Against SARS-CoV-2 Main Protease: A Rational Approach to Antiviral Therapeutics, Current Medicinal Chemistry, doi:10.2174/0109298673292839240329081008.
25.
Hasanah et al., Decoding the therapeutic potential of empon-empon: a bioinformatics expedition unraveling mechanisms against COVID-19 and atherosclerosis, International Journal of Applied Pharmaceutics, doi:10.22159/ijap.2024v16i2.50128.
26.
Shaik et al., Computational identification of selected bioactive compounds from Cedrus deodara as inhibitors against SARS-CoV-2 main protease: a pharmacoinformatics study, Indian Drugs, doi:10.53879/id.61.02.13859.
27.
Wang et al., Investigating the Mechanism of Qu Du Qiang Fei 1 Hao Fang Formula against Coronavirus Disease 2019 Based on Network Pharmacology Method, World Journal of Traditional Chinese Medicine, doi:10.4103/2311-8571.395061.
28.
Singh et al., Unlocking the potential of phytochemicals in inhibiting SARS-CoV-2 M Pro protein - An in-silico and cell-based approach, Research Square, doi:10.21203/rs.3.rs-3888947/v1.
29.
El-Megharbel et al., Chemical and spectroscopic characterization of (Artemisinin/Quercetin/ Zinc) novel mixed ligand complex with assessment of its potent high antiviral activity against SARS-CoV-2 and antioxidant capacity against toxicity induced by acrylamide in male rats, PeerJ, doi:10.7717/peerj.15638.
30.
Akinwumi et al., Evaluation of therapeutic potentials of some bioactive compounds in selected African plants targeting main protease (Mpro) in SARS-CoV-2: a molecular docking study, Egyptian Journal of Medical Human Genetics, doi:10.1186/s43042-023-00456-4.
31.
Yang et al., Active ingredient and mechanistic analysis of traditional Chinese medicine formulas for the prevention and treatment of COVID-19: Insights from bioinformatics and in vitro experiments, Medicine, doi:10.1097/MD.0000000000036238.
32.
Chandran et al., Molecular docking analysis of quercetin with known CoVid-19 targets, Bioinformation, doi:10.6026/973206300191081.
33.
Qin et al., Exploring the bioactive compounds of Feiduqing formula for the prevention and management of COVID-19 through network pharmacology and molecular docking, Medical Data Mining, doi:10.53388/MDM202407003.
34.
Moschovou et al., Exploring the Binding Effects of Natural Products and Antihypertensive Drugs on SARS-CoV-2: An In Silico Investigation of Main Protease and Spike Protein, International Journal of Molecular Sciences, doi:10.3390/ijms242115894.
35.
Pan (B) et al., Quercetin: A promising drug candidate against the potential SARS-CoV-2-Spike mutants with high viral infectivity, Computational and Structural Biotechnology Journal, doi:10.1016/j.csbj.2023.10.029.
36.
Ahmed et al., Evaluation of the Effect of Zinc, Quercetin, Bromelain and Vitamin C on COVID-19 Patients, International Journal of Diabetes Management, doi:10.61797/ijdm.v2i2.259.
37.
Thapa et al., In-silico Approach for Predicting the Inhibitory Effect of Home Remedies on Severe Acute Respiratory Syndrome Coronavirus-2, Makara Journal of Science, doi:10.7454/mss.v27i3.1609.
38.
Alkafaas et al., A study on the effect of natural products against the transmission of B.1.1.529 Omicron, Virology Journal, doi:10.1186/s12985-023-02160-6.
39.
Singh (B) et al., Flavonoids as Potent Inhibitor of SARS-CoV-2 Nsp13 Helicase: Grid Based Docking Approach, Middle East Research Journal of Pharmaceutical Sciences, doi:10.36348/merjps.2023.v03i04.001.
40.
Mandal et al., In silico anti-viral assessment of phytoconstituents in a traditional (Siddha Medicine) polyherbal formulation – Targeting Mpro and pan-coronavirus post-fusion Spike protein, Journal of Traditional and Complementary Medicine, doi:10.1016/j.jtcme.2023.07.004.
41.
Sai Ramesh et al., Computational analysis of the phytocompounds of Mimusops elengi against spike protein of SARS CoV2 – An Insilico model, International Journal of Biological Macromolecules, doi:10.1016/j.ijbiomac.2023.125553.
42.
Corbo et al., Inhibitory potential of phytochemicals on five SARS-CoV-2 proteins: in silico evaluation of endemic plants of Bosnia and Herzegovina, Biotechnology & Biotechnological Equipment, doi:10.1080/13102818.2023.2222196.
43.
Azmi et al., Utilization of quercetin flavonoid compounds in onion (Allium cepa L.) as an inhibitor of SARS-CoV-2 spike protein against ACE2 receptors, 11th International Seminar on New Paradigm and Innovation on Natural Sciences and its Application, doi:10.1063/5.0140285.
44.
Alanzi et al., Structure-based virtual identification of natural inhibitors of SARS-CoV-2 and its Delta and Omicron variant proteins, Future Virology, doi:10.2217/fvl-2022-0184.
45.
Yang (B) et al., In silico evidence implicating novel mechanisms of Prunella vulgaris L. as a potential botanical drug against COVID-19-associated acute kidney injury, Frontiers in Pharmacology, doi:10.3389/fphar.2023.1188086.
46.
Wang (B) et al., Computational Analysis of Lianhua Qingwen as an Adjuvant Treatment in Patients with COVID-19, Society of Toxicology Conference, 2023, www.researchgate.net/publication/370491709_Y_Wang_A_E_Tan_O_Chew_A_Hsueh_and_D_E_Johnson_2023_Computational_Analysis_of_Lianhua_Qingwen_as_an_Adjuvant_Treatment_in_Patients_with_COVID-19_Toxicologist_1921_507.
47.
Ibeh et al., Computational studies of potential antiviral compounds from some selected Nigerian medicinal plants against SARS-CoV-2 proteins, Informatics in Medicine Unlocked, doi:10.1016/j.imu.2023.101230.
48.
Nguyen et al., The Potential of Ameliorating COVID-19 and Sequelae From Andrographis paniculata via Bioinformatics, Bioinformatics and Biology Insights, doi:10.1177/11779322221149622.
49.
Alavi et al., Interaction of Epigallocatechin Gallate and Quercetin with Spike Glycoprotein (S-Glycoprotein) of SARS-CoV-2: In Silico Study, Biomedicines, doi:10.3390/biomedicines10123074.
50.
Chellasamy et al., Docking and molecular dynamics studies of human ezrin protein with a modelled SARS-CoV-2 endodomain and their interaction with potential invasion inhibitors, Journal of King Saud University - Science, doi:10.1016/j.jksus.2022.102277.
51.
Şimşek et al., In silico identification of SARS-CoV-2 cell entry inhibitors from selected natural antivirals, Journal of Molecular Graphics and Modelling, doi:10.1016/j.jmgm.2021.108038.
52.
Kandeil et al., Bioactive Polyphenolic Compounds Showing Strong Antiviral Activities against Severe Acute Respiratory Syndrome Coronavirus 2, Pathogens, doi:10.3390/pathogens10060758.
53.
Rehman et al., Natural Compounds as Inhibitors of SARS-CoV-2 Main Protease (3CLpro): A Molecular Docking and Simulation Approach to Combat COVID-19, Current Pharmaceutical Design, doi:10.2174/1381612826999201116195851.
54.
Sekiou et al., In-Silico Identification of Potent Inhibitors of COVID-19 Main Protease (Mpro) and Angiotensin Converting Enzyme 2 (ACE2) from Natural Products: Quercetin, Hispidulin, and Cirsimaritin Exhibited Better Potential Inhibition than Hydroxy-Chloroquine Against COVID-19 Main Protease Active Site and ACE2, ChemRxiv, doi:10.26434/chemrxiv.12181404.v1.
55.
Zhang et al., In silico screening of Chinese herbal medicines with the potential to directly inhibit 2019 novel coronavirus, Journal of Integrative Medicine, doi:10.1016/j.joim.2020.02.005.
56.
Sisti et al., Evaluation of respiratory virus transmissibility and resilience from fomites: the case of 11 SARS-CoV-2 clinical isolates, Applied and Environmental Microbiology, doi:10.1128/aem.00774-25.
57.
Spinelli et al., Amphibian‐Derived Peptides as Natural Inhibitors of SARS‐CoV‐2 Main Protease (Mpro): A Combined In Vitro and In Silico Approach, Chemistry & Biodiversity, doi:10.1002/cbdv.202403202.
58.
Aguilera-Rodriguez et al., Inhibition of SARS-CoV-2 3CLpro by chemically modified tyrosinase from Agaricus bisporus, RSC Medicinal Chemistry, doi:10.1039/D4MD00289J.
59.
Emam et al., Establishment of in-house assay for screening of anti-SARS-CoV-2 protein inhibitors, AMB Express, doi:10.1186/s13568-024-01739-8.
60.
Fang et al., Development of nanoparticles incorporated with quercetin and ACE2-membrane as a novel therapy for COVID-19, Journal of Nanobiotechnology, doi:10.1186/s12951-024-02435-2.
61.
Roy et al., Quercetin inhibits SARS-CoV-2 infection and prevents syncytium formation by cells co-expressing the viral spike protein and human ACE2, Virology Journal, doi:10.1186/s12985-024-02299-w.
62.
DiGuilio et al., Quercetin improves and protects Calu-3 airway epithelial barrier function, Frontiers in Cell and Developmental Biology, doi:10.3389/fcell.2023.1271201.
63.
Zhang (B) et al., Discovery of the covalent SARS‐CoV‐2 Mpro inhibitors from antiviral herbs via integrating target‐based high‐throughput screening and chemoproteomic approaches, Journal of Medical Virology, doi:10.1002/jmv.29208.
64.
Wu (B) et al., SARS-CoV-2 N protein induced acute kidney injury in diabetic db/db mice is associated with a Mincle-dependent M1 macrophage activation, Frontiers in Immunology, doi:10.3389/fimmu.2023.1264447.
65.
Xu (B) et al., Bioactive compounds from Huashi Baidu decoction possess both antiviral and anti-inflammatory effects against COVID-19, Proceedings of the National Academy of Sciences, doi:10.1073/pnas.2301775120.
66.
Fam et al., Channel activity of SARS-CoV-2 viroporin ORF3a inhibited by adamantanes and phenolic plant metabolites, Scientific Reports, doi:10.1038/s41598-023-31764-9.
67.
Aguado et al., Senolytic therapy alleviates physiological human brain aging and COVID-19 neuropathology, bioRxiv, doi:10.1101/2023.01.17.524329.
68.
Goc et al., Inhibitory effects of specific combination of natural compounds against SARS-CoV-2 and its Alpha, Beta, Gamma, Delta, Kappa, and Mu variants, European Journal of Microbiology and Immunology, doi:10.1556/1886.2021.00022.
69.
Munafò et al., Quercetin and Luteolin Are Single-digit Micromolar Inhibitors of the SARS-CoV-2 RNA-dependent RNA Polymerase, Research Square, doi:10.21203/rs.3.rs-1149846/v1.
70.
Singh (C) et al., The spike protein of SARS-CoV-2 virus induces heme oxygenase-1: Pathophysiologic implications, Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease, doi:10.1016/j.bbadis.2021.166322.
71.
Bahun et al., Inhibition of the SARS-CoV-2 3CLpro main protease by plant polyphenols, Food Chemistry, doi:10.1016/j.foodchem.2021.131594.
72.
Abian et al., Structural stability of SARS-CoV-2 3CLpro and identification of quercetin as an inhibitor by experimental screening, International Journal of Biological Macromolecules, doi:10.1016/j.ijbiomac.2020.07.235.
73.
Shaker et al., Anti-cytokine Storm Activity of Fraxin, Quercetin, and their Combination on Lipopolysaccharide-Induced Cytokine Storm in Mice: Implications in COVID-19, Iranian Journal of Medical Sciences, doi:10.30476/ijms.2023.98947.3102.
74.
Wu (C) et al., Treatment with Quercetin inhibits SARS-CoV-2 N protein-induced acute kidney injury by blocking Smad3-dependent G1 cell cycle arrest, Molecular Therapy, doi:10.1016/j.ymthe.2022.12.002.
75.
Azmi (B) et al., The role of vitamin D receptor and IL‐6 in COVID‐19, Molecular Genetics & Genomic Medicine, doi:10.1002/mgg3.2172.
76.
Shokri-Afra et al., Targeting SIRT1: A Potential Strategy for Combating Severe COVID‐19, BioMed Research International, doi:10.1155/bmri/9507417.
a.
The trimeric spike (S) protein is a glycoprotein that mediates viral entry by binding to the host ACE2 receptor, is critical for SARS-CoV-2's ability to infect host cells, and is a target of neutralizing antibodies. Inhibition of the spike protein prevents viral attachment, halting infection at the earliest stage.
b.
The receptor binding domain is a specific region of the spike protein that binds ACE2 and is a major target of neutralizing antibodies. Focusing on the precise binding site allows highly specific disruption of viral attachment with reduced potential for off-target effects.
c.
The main protease or Mpro, also known as 3CLpro or nsp5, is a cysteine protease that cleaves viral polyproteins into functional units needed for replication. Inhibiting Mpro disrupts the SARS-CoV-2 lifecycle within the host cell, preventing the creation of new copies.
d.
RNA-dependent RNA polymerase (RdRp), also called nsp12, is the core enzyme of the viral replicase-transcriptase complex that copies the positive-sense viral RNA genome into negative-sense templates for progeny RNA synthesis. Inhibiting RdRp blocks viral genome replication and transcription.
e.
The papain-like protease (PLpro) has multiple functions including cleaving viral polyproteins and suppressing the host immune response by deubiquitination and deISGylation of host proteins. Inhibiting PLpro may block viral replication and help restore normal immune responses.
f.
The angiotensin converting enzyme 2 (ACE2) protein is a host cell transmembrane protein that serves as the cellular receptor for the SARS-CoV-2 spike protein. ACE2 is expressed on many cell types, including epithelial cells in the lungs, and allows the virus to enter and infect host cells. Inhibition may affect ACE2's physiological function in blood pressure control.
g.
Transmembrane protease serine 2 (TMPRSS2) is a host cell protease that primes the spike protein, facilitating cellular entry. TMPRSS2 activity helps enable cleavage of the spike protein required for membrane fusion and virus entry. Inhibition may especially protect respiratory epithelial cells, buy may have physiological effects.
h.
The nucleocapsid (N) protein binds and encapsulates the viral genome by coating the viral RNA. N enables formation and release of infectious virions and plays additional roles in viral replication and pathogenesis. N is also an immunodominant antigen used in diagnostic assays.
i.
The helicase, or nsp13, protein unwinds the double-stranded viral RNA, a crucial step in replication and transcription. Inhibition may prevent viral genome replication and the creation of new virus components.
j.
The endoribonuclease, also known as NendoU or nsp15, cleaves specific sequences in viral RNA which may help the virus evade detection by the host immune system. Inhibition may hinder the virus's ability to mask itself from the immune system, facilitating a stronger immune response.
k.
The NSP16/10 complex consists of non-structural proteins 16 and 10, forming a 2'-O-methyltransferase that modifies the viral RNA cap structure. This modification helps the virus evade host immune detection by mimicking host mRNA, making NSP16/10 a promising antiviral target.
l.
Cathepsin L is a host lysosomal cysteine protease that can prime the spike protein through an alternative pathway when TMPRSS2 is unavailable. Dual targeting of cathepsin L and TMPRSS2 may maximize disruption of alternative pathways for virus entry.
m.
Wingless-related integration site (Wnt) ligand 3 is a host signaling molecule that activates the Wnt signaling pathway, which is important in development, cell growth, and tissue repair. Some studies suggest that SARS-CoV-2 infection may interfere with the Wnt signaling pathway, and that Wnt3a is involved in SARS-CoV-2 entry.
n.
The frizzled (FZD) receptor is a host transmembrane receptor that binds Wnt ligands, initiating the Wnt signaling cascade. FZD serves as a co-receptor, along with ACE2, in some proposed mechanisms of SARS-CoV-2 infection. The virus may take advantage of this pathway as an alternative entry route.
o.
Low-density lipoprotein receptor-related protein 6 is a cell surface co-receptor essential for Wnt signaling. LRP6 acts in tandem with FZD for signal transduction and has been discussed as a potential co-receptor for SARS-CoV-2 entry.
p.
The ezrin protein links the cell membrane to the cytoskeleton (the cell's internal support structure) and plays a role in cell shape, movement, adhesion, and signaling. Drugs that occupy the same spot on ezrin where the viral spike protein would bind may hindering viral attachment, and drug binding could further stabilize ezrin, strengthening its potential natural capacity to impede viral fusion and entry.
q.
The Adipocyte Differentiation-Related Protein (ADRP, also known as Perilipin 2 or PLIN2) is a lipid droplet protein regulating the storage and breakdown of fats in cells. SARS-CoV-2 may hijack the lipid handling machinery of host cells and ADRP may play a role in this process. Disrupting ADRP's interaction with the virus may hinder the virus's ability to use lipids for replication and assembly.
r.
Neuropilin-1 (NRP1) is a cell surface receptor with roles in blood vessel development, nerve cell guidance, and immune responses. NRP1 may function as a co-receptor for SARS-CoV-2, facilitating viral entry into cells. Blocking NRP1 may disrupt an alternative route of viral entry.
s.
EP300 (E1A Binding Protein P300) is a transcriptional coactivator involved in several cellular processes, including growth, differentiation, and apoptosis, through its acetyltransferase activity that modifies histones and non-histone proteins. EP300 facilitates viral entry into cells and upregulates inflammatory cytokine production.
t.
Prostaglandin G/H synthase 2 (PTGS2, also known as COX-2) is an enzyme crucial for the production of inflammatory molecules called prostaglandins. PTGS2 plays a role in the inflammatory response that can become severe in COVID-19 and inhibitors (like some NSAIDs) may have benefits in dampening harmful inflammation, but note that prostaglandins have diverse physiological functions.
u.
Heat Shock Protein 90 Alpha Family Class A Member 1 (HSP90AA1) is a chaperone protein that helps other proteins fold correctly and maintains their stability. HSP90AA1 plays roles in cell signaling, survival, and immune responses. HSP90AA1 may interact with numerous viral proteins, but note that it has diverse physiological functions.
v.
Matrix metalloproteinase 9 (MMP9), also called gelatinase B, is a zinc-dependent enzyme that breaks down collagen and other components of the extracellular matrix. MMP9 levels increase in severe COVID-19. Overactive MMP9 can damage lung tissue and worsen inflammation. Inhibition of MMP9 may prevent excessive tissue damage and help regulate the inflammatory response.
w.
The interleukin-6 (IL-6) pro-inflammatory cytokine (signaling molecule) has a complex role in the immune response and may trigger and perpetuate inflammation. Elevated IL-6 levels are associated with severe COVID-19 cases and cytokine storm. Anti-IL-6 therapies may be beneficial in reducing excessive inflammation in severe COVID-19 cases.
x.
The interleukin-10 (IL-10) anti-inflammatory cytokine helps regulate and dampen immune responses, preventing excessive inflammation. IL-10 levels can also be elevated in severe COVID-19. IL-10 could either help control harmful inflammation or potentially contribute to immune suppression.
y.
Vascular Endothelial Growth Factor A (VEGFA) promotes the growth of new blood vessels (angiogenesis) and has roles in inflammation and immune responses. VEGFA may contribute to blood vessel leakiness and excessive inflammation associated with severe COVID-19.
z.
RELA is a transcription factor subunit of NF-kB and is a key regulator of inflammation, driving pro-inflammatory gene expression. SARS-CoV-2 may hijack and modulate NF-kB pathways.
aa.
The interaction between the SARS-CoV-2 spike protein and the human ACE2 receptor is a primary method of viral entry, inhibiting this interaction can prevent the virus from attaching to and entering host cells, halting infection at an early stage.
ab.
Calu-3 is a human lung adenocarcinoma cell line with moderate ACE2 and TMPRSS2 expression and SARS-CoV-2 susceptibility. It provides a model of the human respiratory epithelium, but many not be ideal for modeling early stages of infection due to the moderate expression levels of ACE2 and TMPRSS2.
ac.
A549 is a human lung carcinoma cell line with low ACE2 expression and SARS-CoV-2 susceptibility. Viral entry/replication can be studied but the cells may not replicate all aspects of lung infection.
ad.
HEK293-ACE2+ is a human embryonic kidney cell line engineered for high ACE2 expression and SARS-CoV-2 susceptibility.
ae.
Huh-7 cells were derived from a liver tumor (hepatoma).
af.
Caco-2 cells come from a colorectal adenocarcinoma (cancer). They are valued for their ability to form a polarized cell layer with properties similar to the intestinal lining.
ag.
Vero E6 is an African green monkey kidney cell line with low/no ACE2 expression and high SARS-CoV-2 susceptibility. The cell line is easy to maintain and supports robust viral replication, however the monkey origin may not accurately represent human responses.
ah.
mTEC is a mouse tubular epithelial cell line.
ai.
RAW264.7 is a mouse macrophage cell line.
aj.
HLMEC (Human Lung Microvascular Endothelial Cells) are primary endothelial cells derived from the lung microvasculature. They are used to study endothelial function, inflammation, and viral interactions, particularly in the context of lung infections such as SARS-CoV-2. HLMEC express ACE2 and are susceptible to SARS-CoV-2 infection, making them a relevant model for studying viral entry and endothelial responses in the lung.
ak.
A mouse model expressing the human ACE2 receptor under the control of the K18 promoter.
al.
A mouse model of obesity and severe insulin resistance leading to type 2 diabetes due to a mutation in the leptin receptor gene that impairs satiety signaling.
am.
A mouse model commonly used in infectious disease and cancer research due to higher immune response and susceptibility to infection.
Xu et al., 8 Sep 2024, China, peer-reviewed, 11 authors.
Contact: yicheng6834@126.com, lzjradiotherapy@163.com, huangying68@163.com.
Quercetin inhibited LPS-induced cytokine storm by interacting with the AKT1-FoxO1 and Keap1-Nrf2 signaling pathway in macrophages
Scientific Reports, doi:10.1038/s41598-024-71569-y
Cytokine storm (CS) emerges as an exacerbated inflammatory response triggered by various factors such as pathogens and excessive immunotherapy, posing a significant threat to life if left unchecked. Quercetin, a monomer found in traditional Chinese medicine, exhibits notable anti-inflammatory and antiviral properties. This study endeavors to explore whether quercetin intervention could mitigate CS through a combination of network pharmacology analysis and experimental validation. First, common target genes and potential mechanisms affected by quercetin and CS were identified through network pharmacology, and molecular docking experiments confirmed quercetin and core targets. Subsequently, in vitro experiments of Raw264.7 cells stimulated by lipopolysaccharide (LPS) showed that quercetin could effectively inhibit the overexpression of pro-inflammatory mediators and regulate the AKT1-FoxO1 signaling pathway. At the same time, quercetin can reduce ROS through the Keap1-Nrf2 signaling pathway. In addition, in vivo studies of C57BL/6 mice injected with LPS further confirmed quercetin's inhibitory effect on CS. In conclusion, this investigation elucidated novel target genes and signaling pathways implicated in the therapeutic effects of quercetin on CS. Moreover, it provided compelling evidence supporting the efficacy of quercetin in reversing LPS-induced CS, primarily through the regulation of the AKT1-FoxO1 and Keap1-Nrf2 signaling pathways.
Author contributions Xu, Li, Yang, Li, Xiao, You, Li, Zheng, Li, Yi, and Huang contributed to this study. Xu, Li,ang contributed equally to this study. Yi, Li andHuang directed the design of this study, supervised its implementation and revised draft.
Competing interests The authors declare no competing interests.
References
Addeo, Obeid, Friedlaender, COVID-19 and lung cancer: Risks, mechanisms and treatment interactions, J. Immuno-Therapy Cancer
Ansari, Abdul, Joshi, Opii, Butterfield, Protective effect of quercetin in primary neurons against Aβ(1-42): Relevance to Alzheimer's disease, J. Nutr. Biochem
Arranz, Akt1 and Akt2 protein kinases differentially contribute to macrophage polarization, Proc. Natl. Acad. Sci
Brahmer, Management of immune-related adverse events in patients treated with immune checkpoint inhibitor therapy: American society of clinical oncology clinical practice guideline, J. Clin. Oncol
Cai, The neutrophil-to-lymphocyte ratio determines clinical efficacy of corticosteroid therapy in patients with COVID-19, Cell Metabol
Chan, Murphy, Reactive oxygen species mediate endotoxin-induced human dermal endothelial NF-κB Activation, J. Surg. Res
Cheng, Gu, CircRNA_09505 aggravates inflammation and joint damage in collagen-induced arthritis mice via miR-6089/AKT1/NF-κBaxis, Cell Death & Disease, doi:10.1038/s41419-020-03038-z
Das, Quercetin alleviates inflammation after short-term treatment in high-fat-fed mice, Food Funct
Fajgenbaum, Longo, June, Cytokine storm, N. Engl. J. Med
Fan, FoxO1 regulates Tlr4 inflammatory pathway signalling in macrophages, EMBO J
Granato, Quercetin induces apoptosis and autophagy in primary effusion lymphoma cells by inhibiting PI3K/AKT/mTOR and STAT3 signaling pathways, J. Nutr. Biochem
Han, FoxO1 regulates TLR4/MyD88/MD2-NF-κB inflammatory signalling in mucosal barrier injury of inflammatory bowel disease, J. Cell Mol. Med
Ip, Hydroxychloroquine and tocilizumab therapy in COVID-19 patients-An observational study, Plos One
Jarczak, Nierhaus, Cytokine storm-definition, causes, and implications, Int. J. Mol. Sci
Kanehisa, Furumichi, Sato, Kawashima, Ishiguro-Watanabe, KEGG for taxonomy-based analysis of pathways and genomes, Nucleic Acids Res
Kanehisa, Goto, KEGG: Kyoto encyclopedia of genes and genomes, Nucleic Acids Res
Kanehisa, Toward understanding the origin and evolution of cellular organisms, Scientific Reports, doi:10.1038/s41598-024-71569-ywww.nature.com/scientificreports/
Kang, Melatonin attenuates LPS-induced pyroptosis in acute lung injury by inhibiting NLRP3-GSDMD pathway via activating Nrf2/HO-1 signaling axis, Int. Immunopharmacol
Karki, Kanneganti, The 'cytokine storm': Molecular mechanisms and therapeutic prospects, Trends Immunol
Kim, Rengyolone inhibits inducible nitric oxide synthase expression and nitric oxide production by down-regulation of NF-κB and p38 MAP kinase activity in LPS-stimulated RAW 264.7 cells, Biochem. Pharmacol
Knoll, Schultze, Schulte-Schrepping, Monocytes and Macrophages in COVID-19, Front. Immunol
Lee, Current concepts in the diagnosis and management of cytokine release syndrome, Blood
Lee, Jang, Park, Yang, An update on the role of Nrf2 in respiratory disease: Molecular mechanisms and therapeutic approaches, Int. J. Mol. Sci
Li, Glycyrrhetinic acid: A potential drug for the treatment of COVID-19 cytokine storm, Phytomedicine
Lin, Curcumin attenuates oxidative stress in RAW264.7 cells by increasing the activity of antioxidant enzymes and activating the Nrf2-Keap1 pathway, PloS one
Lin, Zhao, Fu, Xiong, Zhang et al., ISOC1 Modulates Inflammatory Responses in Macrophages through the AKT1/PEX11B/Peroxisome Pathway, Molecules
Liu, Cheng, Roberts, Zhao, Targeting the phosphoinositide 3-kinase pathway in cancer, Nat. Rev. Drug Discov
Liu, Mollugin prevents CLP-induced sepsis in mice by inhibiting TAK1-NF-κB/MAPKs pathways and activating Keap1-Nrf2 pathway in macrophages, Int. Immunopharmacol
Luo, Astaxanthin attenuates ferroptosis via Keap1-Nrf2/HO-1 signaling pathways in LPS-induced acute lung injury, Scientific Reports, doi:10.1038/s41598-024-71569-ywww.nature.com/scientificreports/
Martin, Toll-like receptor-mediated cytokine production is differentially regulated by glycogen synthase kinase 3, Nat. Immunol
Poojary, Penberthy, Buckley, Arandjelovic, Ravichandran, Ex vivo modulation of the Foxo1 phosphorylation state does not lead to dysfunction of T regulatory cells, Plos One
Pooladanda, Thatikonda, Muvvala, Devabattula, Godugu, BRD4 targeting nanotherapy prevents lipopolysaccharide induced acute respiratory distress syndrome, Int. J. Pharmaceut
Prescott, Rice, Corticosteroids in COVID-19 ARDS: Evidence and hope during the pandemic, Jama
Puzanov, Managing toxicities associated with immune checkpoint inhibitors: Consensus recommendations from the Society for Immunotherapy of Cancer (SITC) Toxicity Management Working Group, J. ImmunoTherapy Cancer
Ramos-Casals, Immune-related adverse events of checkpoint inhibitors, Nat. Rev. Dis. Prim
Riol-Blanco, Immunological synapse formation inhibits, via NF-κB and FOXO1, the apoptosis of dendritic cells, Nat. Immunol
Rosas, Tocilizumab in hospitalized patients with severe Covid-19 pneumonia, N. Engl. J. Med
Savai, Pro-proliferative and inflammatory signaling converge on FoxO1 transcription factor in pulmonary hypertension, Nat. Med
Seiler, FOXO transcription factors regulate innate immune mechanisms in respiratory epithelial cells, J. Immunol
Shapouri-Moghaddam, Macrophage plasticity, polarization, and function in health and disease, J. Cell. Physiol
Simon, Fernández, Early lipopolysaccharide-induced reactive oxygen species production evokes necrotic cell death in human umbilical vein endothelial cells, J. Hypertens
Su, FoxO1 links insulin resistance to proinflammatory cytokine IL-1β production in macrophages, Diabetes
Sul, Ra, Quercetin prevents LPS-induced oxidative stress and inflammation by modulating NOX2/ROS/NF-kB in lung epithelial cells, Molecules, doi:10.3390/molecules26226949
Sullivan, FoxO1 integrates direct and indirect effects of insulin on hepatic glucose production and glucose utilization, Nat. Commun
Sun, Schisandrin attenuates lipopolysaccharide-induced lung injury by regulating TLR-4 and Akt/FoxO1 signaling pathways, Front. Physiol
Suryavanshi, Zaiachuk, Pryimak, Kovalchuk, Kovalchuk, Cannabinoids alleviate the LPS-induced cytokine storm via attenuating NLRP3 inflammasome signaling and TYK2-mediated STAT3 signaling pathways in vitro, Cells
Tan, The reactive oxygen species in macrophage polarization: Reflecting its dual role in progression and treatment of human diseases, Oxid. Med. Cell. Longevity
Tay, Cytokine release syndrome in cancer patients receiving immune checkpoint inhibitors: A case series of 25 patients and review of the literature, Front. Immunol
Wang, Wu, Zhang, Resveratrol Targets AKT1 to Inhibit Inflammasome Activation in Cardiomyocytes Under Acute Sympathetic Stress, Frontiers in Pharmacology, doi:10.3389/fphar.2022.818127
Webb, Brunet, FOXO transcription factors: Key regulators of cellular quality control, Trends Biochem. Sci
Wu, Quercetin as an antiviral agent inhibits influenza A virus (IAV) entry, Viruses
Xu, Yang, None
Yamamoto, Kensler, Motohashi, The KEAP1-NRF2 system: A thiol-based sensor-effector apparatus for maintaining redox homeostasis, Physiol. Rev
Yang, Myrsine seguinii ethanolic extract and its active component quercetin inhibit macrophage activation and peritonitis induced by LPS by targeting to Syk/Src/IRAK-1, J. Ethnopharmacol
Yang, TLR3-triggered reactive oxygen species contribute to inflammatory responses by activating signal transducer and activator of transcription-1, J. Immunol
You, Inspiration for COVID-19 treatment: Network analysis and experimental validation of baicalin for cytokine storm, Front. Pharmacol
Zhu, Brd4 inhibition ameliorates Pyocyanin-mediated macrophage dysfunction via transcriptional repression of reactive oxygen and nitrogen free radical pathways, Cell Death Dis
Zhu, Clinical value of immune-inflammatory parameters to assess the severity of coronavirus disease 2019, Int. J. Infect. Dis
DOI record:
{
"DOI": "10.1038/s41598-024-71569-y",
"ISSN": [
"2045-2322"
],
"URL": "http://dx.doi.org/10.1038/s41598-024-71569-y",
"alternative-id": [
"71569"
],
"article-number": "20913",
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "10 May 2024"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "29 August 2024"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "8 September 2024"
},
{
"group": {
"label": "Competing interests",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1,
"value": "The authors declare no competing interests."
}
],
"author": [
{
"affiliation": [],
"family": "Xu",
"given": "Jingyi",
"sequence": "first"
},
{
"affiliation": [],
"family": "Li",
"given": "Yue",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yang",
"given": "Xi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Li",
"given": "Hong",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Xiao",
"given": "Xi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "You",
"given": "Jia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Li",
"given": "Huawei",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zheng",
"given": "Lingnan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yi",
"given": "Cheng",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Li",
"given": "Zhaojun",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Huang",
"given": "Ying",
"sequence": "additional"
}
],
"container-title": "Scientific Reports",
"container-title-short": "Sci Rep",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2024,
9,
8
]
],
"date-time": "2024-09-08T11:01:49Z",
"timestamp": 1725793309000
},
"deposited": {
"date-parts": [
[
2024,
9,
8
]
],
"date-time": "2024-09-08T12:04:11Z",
"timestamp": 1725797051000
},
"funder": [
{
"DOI": "10.13039/501100013365",
"award": [
"2022NSFSC1379",
"HX-2019-nCoV-069"
],
"doi-asserted-by": "publisher",
"id": [
{
"asserted-by": "publisher",
"id": "10.13039/501100013365",
"id-type": "DOI"
}
],
"name": "West China Hospital, Sichuan University"
},
{
"award": [
"2022YFSY0054"
],
"name": "四川大学华西医院,中国"
},
{
"award": [
"NO.82260490"
],
"name": "Hainan Affiliated Hospital of Hainan Medical University, China"
},
{
"award": [
"NO.821QN394"
],
"name": "Hainan Affiliated Hospital of Hainan Medical University"
},
{
"DOI": "10.13039/501100004912",
"award": [
"2020-YF05-00059-SN"
],
"doi-asserted-by": "publisher",
"id": [
{
"asserted-by": "publisher",
"id": "10.13039/501100004912",
"id-type": "DOI"
}
],
"name": "Sichuan University"
}
],
"indexed": {
"date-parts": [
[
2024,
9,
9
]
],
"date-time": "2024-09-09T00:22:36Z",
"timestamp": 1725841356755
},
"is-referenced-by-count": 0,
"issue": "1",
"issued": {
"date-parts": [
[
2024,
9,
8
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2024,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by-nc-nd/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
9,
8
]
],
"date-time": "2024-09-08T00:00:00Z",
"timestamp": 1725753600000
}
},
{
"URL": "https://creativecommons.org/licenses/by-nc-nd/4.0",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
9,
8
]
],
"date-time": "2024-09-08T00:00:00Z",
"timestamp": 1725753600000
}
}
],
"link": [
{
"URL": "https://www.nature.com/articles/s41598-024-71569-y.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.nature.com/articles/s41598-024-71569-y",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.nature.com/articles/s41598-024-71569-y.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1038",
"published": {
"date-parts": [
[
2024,
9,
8
]
]
},
"published-online": {
"date-parts": [
[
2024,
9,
8
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1056/NEJMra2026131",
"author": "DC Fajgenbaum",
"doi-asserted-by": "publisher",
"first-page": "2255",
"issue": "23",
"journal-title": "N. Engl. J. Med.",
"key": "71569_CR1",
"unstructured": "Fajgenbaum, D. C., Longo, D. L. & June, C. H. Cytokine storm. N. Engl. J. Med. 383(23), 2255–2273 (2020).",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.1016/j.it.2021.06.001",
"author": "R Karki",
"doi-asserted-by": "publisher",
"first-page": "681",
"issue": "8",
"journal-title": "Trends Immunol.",
"key": "71569_CR2",
"unstructured": "Karki, R. & Kanneganti, T.-D. The ‘cytokine storm’: Molecular mechanisms and therapeutic prospects. Trends Immunol. 42(8), 681–705 (2021).",
"volume": "42",
"year": "2021"
},
{
"DOI": "10.1002/jcp.26429",
"author": "A Shapouri-Moghaddam",
"doi-asserted-by": "publisher",
"first-page": "6425",
"issue": "9",
"journal-title": "J. Cell. Physiol.",
"key": "71569_CR3",
"unstructured": "Shapouri-Moghaddam, A. et al. Macrophage plasticity, polarization, and function in health and disease. J. Cell. Physiol. 233(9), 6425–6440 (2018).",
"volume": "233",
"year": "2018"
},
{
"DOI": "10.1016/j.jnutbio.2008.03.002",
"author": "MA Ansari",
"doi-asserted-by": "publisher",
"first-page": "269",
"issue": "4",
"journal-title": "J. Nutr. Biochem.",
"key": "71569_CR4",
"unstructured": "Ansari, M. A., Abdul, H. M., Joshi, G., Opii, W. O. & Butterfield, D. A. Protective effect of quercetin in primary neurons against Aβ(1–42): Relevance to Alzheimer’s disease. J. Nutr. Biochem. 20(4), 269–275 (2009).",
"volume": "20",
"year": "2009"
},
{
"DOI": "10.1039/c3fo30241e",
"author": "N Das",
"doi-asserted-by": "publisher",
"first-page": "6",
"journal-title": "Food Funct.",
"key": "71569_CR5",
"unstructured": "Das, N. et al. Quercetin alleviates inflammation after short-term treatment in high-fat-fed mice. Food Funct. 4, 6 (2013).",
"volume": "4",
"year": "2013"
},
{
"DOI": "10.1016/j.jnutbio.2016.12.011",
"author": "M Granato",
"doi-asserted-by": "publisher",
"first-page": "124",
"journal-title": "J. Nutr. Biochem.",
"key": "71569_CR6",
"unstructured": "Granato, M. et al. Quercetin induces apoptosis and autophagy in primary effusion lymphoma cells by inhibiting PI3K/AKT/mTOR and STAT3 signaling pathways. J. Nutr. Biochem. 41, 124–136 (2017).",
"volume": "41",
"year": "2017"
},
{
"DOI": "10.3390/v8010006",
"author": "W Wu",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Viruses",
"key": "71569_CR7",
"unstructured": "Wu, W. et al. Quercetin as an antiviral agent inhibits influenza A virus (IAV) entry. Viruses 8, 1 (2015).",
"volume": "8",
"year": "2015"
},
{
"author": "WS Yang",
"first-page": "1165",
"journal-title": "J. Ethnopharmacol.",
"key": "71569_CR8",
"unstructured": "Yang, W. S. et al. Myrsine seguinii ethanolic extract and its active component quercetin inhibit macrophage activation and peritonitis induced by LPS by targeting to Syk/Src/IRAK-1. J. Ethnopharmacol. 15, 1165–1174 (2015).",
"volume": "15",
"year": "2015"
},
{
"DOI": "10.3390/molecules26226949",
"author": "OA-O Sul",
"doi-asserted-by": "publisher",
"first-page": "6949",
"journal-title": "Molecules",
"key": "71569_CR9",
"unstructured": "Sul, O.A.-O. & Ra, S.A.-O. Quercetin prevents LPS-induced oxidative stress and inflammation by modulating NOX2/ROS/NF-kB in lung epithelial cells. Molecules 26, 6949. https://doi.org/10.3390/molecules26226949 (2021).",
"volume": "26",
"year": "2021"
},
{
"author": "IO Sullivan",
"first-page": "1",
"journal-title": "Nat. Commun.",
"key": "71569_CR10",
"unstructured": "Sullivan, I. O. et al. FoxO1 integrates direct and indirect effects of insulin on hepatic glucose production and glucose utilization. Nat. Commun. 6, 1 (2015).",
"volume": "6",
"year": "2015"
},
{
"DOI": "10.1038/nm.3695",
"author": "R Savai",
"doi-asserted-by": "publisher",
"first-page": "1289",
"issue": "11",
"journal-title": "Nat. Med.",
"key": "71569_CR11",
"unstructured": "Savai, R. et al. Pro-proliferative and inflammatory signaling converge on FoxO1 transcription factor in pulmonary hypertension. Nat. Med. 20(11), 1289–1300 (2014).",
"volume": "20",
"year": "2014"
},
{
"author": "VK Poojary",
"first-page": "3",
"journal-title": "Plos One",
"key": "71569_CR12",
"unstructured": "Poojary, V. K., Penberthy, K. K., Buckley, M. W., Arandjelovic, S. & Ravichandran, K. Ex vivo modulation of the Foxo1 phosphorylation state does not lead to dysfunction of T regulatory cells. Plos One 12, 3 (2017).",
"volume": "12",
"year": "2017"
},
{
"DOI": "10.1016/j.tibs.2014.02.003",
"author": "AE Webb",
"doi-asserted-by": "publisher",
"first-page": "159",
"journal-title": "Trends Biochem. Sci.",
"key": "71569_CR13",
"unstructured": "Webb, A. E. & Brunet, A. FOXO transcription factors: Key regulators of cellular quality control. Trends Biochem. Sci. 39, 159–169 (2014).",
"volume": "39",
"year": "2014"
},
{
"DOI": "10.1038/ni.1750",
"author": "L Riol-Blanco",
"doi-asserted-by": "publisher",
"first-page": "753",
"issue": "7",
"journal-title": "Nat. Immunol.",
"key": "71569_CR14",
"unstructured": "Riol-Blanco, L. et al. Immunological synapse formation inhibits, via NF-κB and FOXO1, the apoptosis of dendritic cells. Nat. Immunol. 10(7), 753–760 (2009).",
"volume": "10",
"year": "2009"
},
{
"DOI": "10.1111/jcmm.15075",
"author": "C Han",
"doi-asserted-by": "publisher",
"first-page": "3712",
"issue": "6",
"journal-title": "J. Cell Mol. Med.",
"key": "71569_CR15",
"unstructured": "Han, C. et al. FoxO1 regulates TLR4/MyD88/MD2-NF-κB inflammatory signalling in mucosal barrier injury of inflammatory bowel disease. J. Cell Mol. Med. 24(6), 3712–3723 (2020).",
"volume": "24",
"year": "2020"
},
{
"DOI": "10.2337/db09-0232",
"author": "D Su",
"doi-asserted-by": "publisher",
"first-page": "2624",
"issue": "11",
"journal-title": "Diabetes",
"key": "71569_CR16",
"unstructured": "Su, D. et al. FoxO1 links insulin resistance to proinflammatory cytokine IL-1β production in macrophages. Diabetes 58(11), 2624–2633 (2009).",
"volume": "58",
"year": "2009"
},
{
"DOI": "10.1038/emboj.2010.268",
"author": "W Fan",
"doi-asserted-by": "publisher",
"first-page": "4223",
"issue": "24",
"journal-title": "EMBO J.",
"key": "71569_CR17",
"unstructured": "Fan, W. et al. FoxO1 regulates Tlr4 inflammatory pathway signalling in macrophages. EMBO J. 29(24), 4223–4236 (2010).",
"volume": "29",
"year": "2010"
},
{
"DOI": "10.1152/physrev.00023.2017",
"author": "MA-O Yamamoto",
"doi-asserted-by": "publisher",
"first-page": "1169",
"issue": "3",
"journal-title": "Physiol. Rev.",
"key": "71569_CR18",
"unstructured": "Yamamoto, M.A.-O., Kensler, T. W. & Motohashi, H. The KEAP1-NRF2 system: A thiol-based sensor-effector apparatus for maintaining redox homeostasis. Physiol. Rev. 98(3), 1169–1203 (2018).",
"volume": "98",
"year": "2018"
},
{
"DOI": "10.1093/nar/28.1.27",
"author": "M Kanehisa",
"doi-asserted-by": "publisher",
"first-page": "27",
"journal-title": "Nucleic Acids Res.",
"key": "71569_CR19",
"unstructured": "Kanehisa, M. & Goto, S. KEGG: Kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 28, 27–30 (2000).",
"volume": "28",
"year": "2000"
},
{
"DOI": "10.1002/pro.3715",
"author": "MA-OX Kanehisa",
"doi-asserted-by": "publisher",
"first-page": "1947",
"journal-title": "Protein Sci.",
"key": "71569_CR20",
"unstructured": "Kanehisa, M.A.-O.X. Toward understanding the origin and evolution of cellular organisms. Protein Sci. 28, 1947–1951 (2019).",
"volume": "28",
"year": "2019"
},
{
"DOI": "10.1093/nar/gkac963",
"author": "MA-OX Kanehisa",
"doi-asserted-by": "publisher",
"first-page": "D587",
"journal-title": "Nucleic Acids Res.",
"key": "71569_CR21",
"unstructured": "Kanehisa, M.A.-O.X., Furumichi, M., Sato, Y., Kawashima, M. & Ishiguro-Watanabe, M. KEGG for taxonomy-based analysis of pathways and genomes. Nucleic Acids Res. 51, D587–D592 (2023).",
"volume": "51",
"year": "2023"
},
{
"author": "V Pooladanda",
"first-page": "601",
"journal-title": "Int. J. Pharmaceut.",
"key": "71569_CR22",
"unstructured": "Pooladanda, V., Thatikonda, S., Muvvala, S. P., Devabattula, G. & Godugu, C. BRD4 targeting nanotherapy prevents lipopolysaccharide induced acute respiratory distress syndrome. Int. J. Pharmaceut. 2021, 601 (2021).",
"volume": "2021",
"year": "2021"
},
{
"DOI": "10.1016/S0022-4804(03)00050-7",
"author": "EL Chan",
"doi-asserted-by": "publisher",
"first-page": "120",
"issue": "1",
"journal-title": "J. Surg. Res.",
"key": "71569_CR23",
"unstructured": "Chan, E. L. & Murphy, J. T. Reactive oxygen species mediate endotoxin-induced human dermal endothelial NF-κB Activation. J. Surg. Res. 111(1), 120–126 (2003).",
"volume": "111",
"year": "2003"
},
{
"DOI": "10.1097/HJH.0b013e328329e31c",
"author": "F Simon",
"doi-asserted-by": "publisher",
"first-page": "1202",
"issue": "6",
"journal-title": "J. Hypertens.",
"key": "71569_CR24",
"unstructured": "Simon, F. & Fernández, R. Early lipopolysaccharide-induced reactive oxygen species production evokes necrotic cell death in human umbilical vein endothelial cells. J. Hypertens. 27(6), 1202–1216 (2009).",
"volume": "27",
"year": "2009"
},
{
"DOI": "10.1155/2016/2795090",
"author": "H-Y Tan",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Oxid. Med. Cell. Longevity",
"key": "71569_CR25",
"unstructured": "Tan, H.-Y. et al. The reactive oxygen species in macrophage polarization: Reflecting its dual role in progression and treatment of human diseases. Oxid. Med. Cell. Longevity 2016, 1–16 (2016).",
"volume": "2016",
"year": "2016"
},
{
"DOI": "10.1038/s41419-020-2672-0",
"author": "F Zhu",
"doi-asserted-by": "publisher",
"first-page": "459",
"journal-title": "Cell Death Dis.",
"key": "71569_CR26",
"unstructured": "Zhu, F. et al. Brd4 inhibition ameliorates Pyocyanin-mediated macrophage dysfunction via transcriptional repression of reactive oxygen and nitrogen free radical pathways. Cell Death Dis. 11, 459 (2020).",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1038/nrd2926",
"author": "P Liu",
"doi-asserted-by": "publisher",
"first-page": "627",
"issue": "8",
"journal-title": "Nat. Rev. Drug Discov.",
"key": "71569_CR27",
"unstructured": "Liu, P., Cheng, H., Roberts, T. M. & Zhao, J. J. Targeting the phosphoinositide 3-kinase pathway in cancer. Nat. Rev. Drug Discov. 8(8), 627–644 (2009).",
"volume": "8",
"year": "2009"
},
{
"DOI": "10.4049/jimmunol.1202574",
"author": "C-S Yang",
"doi-asserted-by": "publisher",
"first-page": "6368",
"issue": "12",
"journal-title": "J. Immunol.",
"key": "71569_CR28",
"unstructured": "Yang, C.-S. et al. TLR3-triggered reactive oxygen species contribute to inflammatory responses by activating signal transducer and activator of transcription-1. J. Immunol. 190(12), 6368–6377 (2013).",
"volume": "190",
"year": "2013"
},
{
"DOI": "10.3390/ijms231911740",
"author": "D Jarczak",
"doi-asserted-by": "publisher",
"first-page": "19",
"journal-title": "Int. J. Mol. Sci.",
"key": "71569_CR29",
"unstructured": "Jarczak, D. & Nierhaus, A. Cytokine storm—definition, causes, and implications. Int. J. Mol. Sci. 23, 19 (2022).",
"volume": "23",
"year": "2022"
},
{
"DOI": "10.1136/jitc-2020-000892",
"author": "A Addeo",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "J. ImmunoTherapy Cancer",
"key": "71569_CR30",
"unstructured": "Addeo, A., Obeid, M. & Friedlaender, A. COVID-19 and lung cancer: Risks, mechanisms and treatment interactions. J. ImmunoTherapy Cancer 8, 1 (2020).",
"volume": "8",
"year": "2020"
},
{
"author": "R Knoll",
"first-page": "12",
"journal-title": "Front. Immunol.",
"key": "71569_CR31",
"unstructured": "Knoll, R., Schultze, J. L. & Schulte-Schrepping, J. Monocytes and Macrophages in COVID-19. Front. Immunol. 2021, 12 (2021).",
"volume": "2021",
"year": "2021"
},
{
"DOI": "10.1182/blood-2014-05-552729",
"author": "DW Lee",
"doi-asserted-by": "publisher",
"first-page": "188",
"issue": "2",
"journal-title": "Blood",
"key": "71569_CR32",
"unstructured": "Lee, D. W. et al. Current concepts in the diagnosis and management of cytokine release syndrome. Blood 124(2), 188–195 (2014).",
"volume": "124",
"year": "2014"
},
{
"author": "SH Tay",
"first-page": "13",
"journal-title": "Front. Immunol.",
"key": "71569_CR33",
"unstructured": "Tay, S. H. et al. Cytokine release syndrome in cancer patients receiving immune checkpoint inhibitors: A case series of 25 patients and review of the literature. Front. Immunol. 2022, 13 (2022).",
"volume": "2022",
"year": "2022"
},
{
"DOI": "10.1016/j.ijid.2020.04.041",
"author": "Z Zhu",
"doi-asserted-by": "publisher",
"first-page": "332",
"journal-title": "Int. J. Infect. Dis.",
"key": "71569_CR34",
"unstructured": "Zhu, Z. et al. Clinical value of immune-inflammatory parameters to assess the severity of coronavirus disease 2019. Int. J. Infect. Dis. 95, 332–339 (2020).",
"volume": "95",
"year": "2020"
},
{
"DOI": "10.1200/JCO.2017.77.6385",
"author": "JR Brahmer",
"doi-asserted-by": "publisher",
"first-page": "1714",
"issue": "17",
"journal-title": "J. Clin. Oncol.",
"key": "71569_CR35",
"unstructured": "Brahmer, J. R. et al. Management of immune-related adverse events in patients treated with immune checkpoint inhibitor therapy: American society of clinical oncology clinical practice guideline. J. Clin. Oncol. 36(17), 1714–1768 (2018).",
"volume": "36",
"year": "2018"
},
{
"DOI": "10.1186/s40425-017-0300-z",
"author": "I Puzanov",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "J. ImmunoTherapy Cancer",
"key": "71569_CR36",
"unstructured": "Puzanov, I. et al. Managing toxicities associated with immune checkpoint inhibitors: Consensus recommendations from the Society for Immunotherapy of Cancer (SITC) Toxicity Management Working Group. J. ImmunoTherapy Cancer 5, 1 (2017).",
"volume": "5",
"year": "2017"
},
{
"DOI": "10.1038/s41572-019-0135-7",
"author": "M Ramos-Casals",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Nat. Rev. Dis. Prim.",
"key": "71569_CR37",
"unstructured": "Ramos-Casals, M. et al. Immune-related adverse events of checkpoint inhibitors. Nat. Rev. Dis. Prim. 6, 1 (2020).",
"volume": "6",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.16747",
"author": "HC Prescott",
"doi-asserted-by": "publisher",
"first-page": "1292",
"journal-title": "Jama",
"key": "71569_CR38",
"unstructured": "Prescott, H. C. & Rice, T. W. Corticosteroids in COVID-19 ARDS: Evidence and hope during the pandemic. Jama 324, 1292–1295 (2020).",
"volume": "324",
"year": "2020"
},
{
"DOI": "10.1016/j.cmet.2021.01.002",
"author": "J Cai",
"doi-asserted-by": "publisher",
"first-page": "258",
"issue": "2",
"journal-title": "Cell Metabol.",
"key": "71569_CR39",
"unstructured": "Cai, J. et al. The neutrophil-to-lymphocyte ratio determines clinical efficacy of corticosteroid therapy in patients with COVID-19. Cell Metabol. 33(2), 258-269.e3 (2021).",
"volume": "33",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2028700",
"author": "IO Rosas",
"doi-asserted-by": "publisher",
"first-page": "1503",
"issue": "16",
"journal-title": "N. Engl. J. Med.",
"key": "71569_CR40",
"unstructured": "Rosas, I. O. et al. Tocilizumab in hospitalized patients with severe Covid-19 pneumonia. N. Engl. J. Med. 384(16), 1503–1516 (2021).",
"volume": "384",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0237693",
"author": "A Ip",
"doi-asserted-by": "publisher",
"first-page": "8",
"journal-title": "Plos One",
"key": "71569_CR41",
"unstructured": "Ip, A. et al. Hydroxychloroquine and tocilizumab therapy in COVID-19 patients-An observational study. Plos One 15, 8 (2020).",
"volume": "15",
"year": "2020"
},
{
"author": "J-Y Kang",
"first-page": "109",
"journal-title": "Int. Immunopharmacol.",
"key": "71569_CR42",
"unstructured": "Kang, J.-Y. et al. Melatonin attenuates LPS-induced pyroptosis in acute lung injury by inhibiting NLRP3-GSDMD pathway via activating Nrf2/HO-1 signaling axis. Int. Immunopharmacol. 2022, 109 (2022).",
"volume": "2022",
"year": "2022"
},
{
"DOI": "10.1016/j.bcp.2005.12.031",
"author": "JH Kim",
"doi-asserted-by": "publisher",
"first-page": "1198",
"issue": "8",
"journal-title": "Biochem. Pharmacol.",
"key": "71569_CR43",
"unstructured": "Kim, J. H. et al. Rengyolone inhibits inducible nitric oxide synthase expression and nitric oxide production by down-regulation of NF-κB and p38 MAP kinase activity in LPS-stimulated RAW 264.7 cells. Biochem. Pharmacol. 71(8), 1198–1205 (2006).",
"volume": "71",
"year": "2006"
},
{
"DOI": "10.3390/cells11091391",
"author": "SV Suryavanshi",
"doi-asserted-by": "publisher",
"first-page": "9",
"journal-title": "Cells",
"key": "71569_CR44",
"unstructured": "Suryavanshi, S. V., Zaiachuk, M., Pryimak, N., Kovalchuk, I. & Kovalchuk, O. Cannabinoids alleviate the LPS-induced cytokine storm via attenuating NLRP3 inflammasome signaling and TYK2-mediated STAT3 signaling pathways in vitro. Cells 11, 9 (2022).",
"volume": "11",
"year": "2022"
},
{
"author": "H Li",
"first-page": "102",
"journal-title": "Phytomedicine",
"key": "71569_CR45",
"unstructured": "Li, H. et al. Glycyrrhetinic acid: A potential drug for the treatment of COVID-19 cytokine storm. Phytomedicine 2022, 102 (2022).",
"volume": "2022",
"year": "2022"
},
{
"author": "J You",
"first-page": "13",
"journal-title": "Front. Pharmacol.",
"key": "71569_CR46",
"unstructured": "You, J. et al. Inspiration for COVID-19 treatment: Network analysis and experimental validation of baicalin for cytokine storm. Front. Pharmacol. 2022, 13 (2022).",
"volume": "2022",
"year": "2022"
},
{
"DOI": "10.3390/molecules27185896",
"doi-asserted-by": "crossref",
"key": "71569_CR47",
"unstructured": "Lin. X, Zhao. Q, Fu. B, Xiong. Y, Zhang. S, Xu. S, Wu. H. ISOC1 Modulates Inflammatory Responses in Macrophages through the AKT1/PEX11B/Peroxisome Pathway. Molecules 27(18), 5896 (2022)."
},
{
"DOI": "10.3389/fphar.2022.818127",
"doi-asserted-by": "publisher",
"key": "71569_CR48",
"unstructured": "Wang. R, Wang. Y, Wu. J, Guo. Y, Xiao. H, Zhang. Y, & Ma. K. Resveratrol Targets AKT1 to Inhibit Inflammasome Activation in Cardiomyocytes Under Acute Sympathetic Stress. Frontiers in Pharmacology 13, https://doi.org/10.3389/fphar.2022.818127 (2022)."
},
{
"DOI": "10.1038/s41419-020-03038-z",
"doi-asserted-by": "publisher",
"key": "71569_CR49",
"unstructured": "Yang. J, Cheng. M, Gu. B, & Wang. J. CircRNA_09505 aggravates inflammation and joint damage in collagen-induced arthritis mice via miR-6089/AKT1/NF-κBaxis, Cell Death & Disease 11(10), https://doi.org/10.1038/s41419-020-03038-z (2020)."
},
{
"DOI": "10.1073/pnas.1119038109",
"author": "A Arranz",
"doi-asserted-by": "publisher",
"first-page": "9517",
"issue": "24",
"journal-title": "Proc. Natl. Acad. Sci.",
"key": "71569_CR50",
"unstructured": "Arranz, A. et al. Akt1 and Akt2 protein kinases differentially contribute to macrophage polarization. Proc. Natl. Acad. Sci. 109(24), 9517–9522 (2012).",
"volume": "109",
"year": "2012"
},
{
"DOI": "10.1038/ni1221",
"author": "M Martin",
"doi-asserted-by": "publisher",
"first-page": "777",
"journal-title": "Nat. Immunol.",
"key": "71569_CR51",
"unstructured": "Martin, M. et al. Toll-like receptor-mediated cytokine production is differentially regulated by glycogen synthase kinase 3. Nat. Immunol. 6, 777–784 (2005).",
"volume": "6",
"year": "2005"
},
{
"DOI": "10.4049/jimmunol.1200596",
"author": "F Seiler",
"doi-asserted-by": "publisher",
"first-page": "1603",
"issue": "4",
"journal-title": "J. Immunol.",
"key": "71569_CR52",
"unstructured": "Seiler, F. et al. FOXO transcription factors regulate innate immune mechanisms in respiratory epithelial cells. J. Immunol. 190(4), 1603–1613 (2013).",
"volume": "190",
"year": "2013"
},
{
"author": "K Sun",
"first-page": "9",
"journal-title": "Front. Physiol.",
"key": "71569_CR53",
"unstructured": "Sun, K. et al. Schisandrin attenuates lipopolysaccharide-induced lung injury by regulating TLR-4 and Akt/FoxO1 signaling pathways. Front. Physiol. 2018, 9 (2018).",
"volume": "2018",
"year": "2018"
},
{
"author": "J Lee",
"first-page": "16",
"journal-title": "Int. J. Mol. Sci.",
"key": "71569_CR54",
"unstructured": "Lee, J., Jang, J., Park, S.-M. & Yang, S.-R. An update on the role of Nrf2 in respiratory disease: Molecular mechanisms and therapeutic approaches. Int. J. Mol. Sci. 22, 16 (2021).",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0216711",
"author": "X Lin",
"doi-asserted-by": "publisher",
"first-page": "e0216711",
"journal-title": "PloS one",
"key": "71569_CR55",
"unstructured": "Lin, X. et al. Curcumin attenuates oxidative stress in RAW264.7 cells by increasing the activity of antioxidant enzymes and activating the Nrf2-Keap1 pathway. PloS one 14, e0216711 (2019).",
"volume": "14",
"year": "2019"
},
{
"DOI": "10.1016/j.intimp.2023.111079",
"author": "X Liu",
"doi-asserted-by": "publisher",
"first-page": "111079",
"journal-title": "Int. Immunopharmacol.",
"key": "71569_CR56",
"unstructured": "Liu, X. et al. Mollugin prevents CLP-induced sepsis in mice by inhibiting TAK1-NF-κB/MAPKs pathways and activating Keap1-Nrf2 pathway in macrophages. Int. Immunopharmacol. 125, 111079 (2023).",
"volume": "125",
"year": "2023"
},
{
"DOI": "10.1016/j.lfs.2022.121091",
"author": "L Luo",
"doi-asserted-by": "publisher",
"first-page": "121091",
"journal-title": "Life Sci.",
"key": "71569_CR57",
"unstructured": "Luo, L. et al. Astaxanthin attenuates ferroptosis via Keap1-Nrf2/HO-1 signaling pathways in LPS-induced acute lung injury. Life Sci. 311, 121091 (2022).",
"volume": "311",
"year": "2022"
}
],
"reference-count": 57,
"references-count": 57,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.nature.com/articles/s41598-024-71569-y"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Quercetin inhibited LPS-induced cytokine storm by interacting with the AKT1-FoxO1 and Keap1-Nrf2 signaling pathway in macrophages",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "14"
}