Nutritional deficiencies that may predispose to long COVID
et al., Inflammopharmacology, doi:10.1007/s10787-023-01183-3, Mar 2023
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
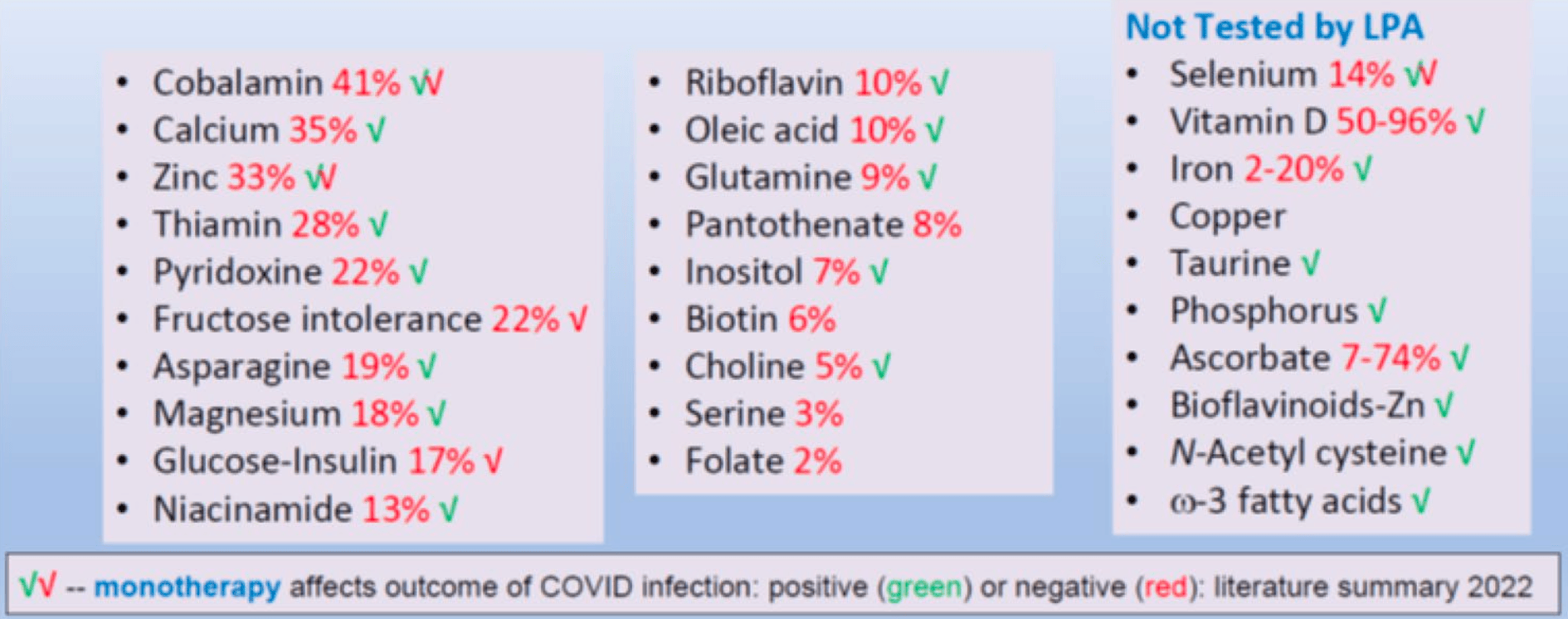
Review of 22 nutritional factors that have been linked to COVID-19 outcomes, the role of nutrients in COVID-19 infection, and the prevalence of multiple nutritional deficiencies in the population.
1.
Jaurrieta-Largo et al., A Machine Learning Approach to Understanding the Genetic Role in COVID-19 Prognosis: The Influence of Gene Polymorphisms Related to Inflammation, Vitamin D, and ACE2, International Journal of Molecular Sciences, doi:10.3390/ijms26167975.
2.
Al-Khrasani et al., Do vitamins halt the COVID-19-evoked pro-inflammatory cytokines involved in the development of neuropathic pain?, Biomedicine & Pharmacotherapy, doi:10.1016/j.biopha.2025.118346.
3.
Kow et al., Vitamin D and COVID‐19: How much more evidence do we need?, Nutrition in Clinical Practice, doi:10.1002/ncp.11349.
4.
Bigman et al., A Comprehensive Scoping Review on Diet and Nutrition in Relation to Long COVID-19 Symptoms and Recovery, Nutrients, doi:10.3390/nu17111802.
5.
Hewison, M., COVID-19 and our understanding of vitamin D and immune function, The Journal of Steroid Biochemistry and Molecular Biology, doi:10.1016/j.jsbmb.2025.106710.
6.
Wimalawansa, S., Vitamin D Deficiency Meets Hill’s Criteria for Causation in SARS-CoV-2 Susceptibility, Complications, and Mortality: A Systematic Review, Nutrients, doi:10.3390/nu17030599.
7.
Sanduzzi Zamparelli et al., Immune-Boosting and Antiviral Effects of Antioxidants in COVID-19 Pneumonia: A Therapeutic Perspective, Life, doi:10.3390/life15010113.
8.
Fazli et al., Possible Link between Gut Microbiota, Diet, and COVID-19 Infection, Journal of Medical Bacteriology, 12:4, jmb.tums.ac.ir/index.php/jmb/article/view/525.
9.
Wojciulik et al., The impact of genetic polymorphism on course and severity of the SARS-CoV-2 infection and COVID-19 disease, Przeglad Epidemiologiczny, doi:10.32394/pe/194862.
10.
Wimalawansa (B), S., Unveiling the Interplay—Vitamin D and ACE-2 Molecular Interactions in Mitigating Complications and Deaths from SARS-CoV-2, Biology, doi:10.3390/biology13100831.
11.
Santa et al., Comparative analysis of COVID-19 responses in Japan and Africa: diet, phytochemicals, vitamin D, and gut microbiota in reducing mortality—A systematic review and meta-analysis, Frontiers in Nutrition, doi:10.3389/fnut.2024.1465324.
12.
Kaushal, A., Nutraceuticals and pharmacological to balance the transitional microbiome to extend immunity during COVID-19 and other viral infections, Journal of Translational Medicine, doi:10.1186/s12967-024-05587-9.
13.
Mu et al., Anti-inflammatory and Nutritional Interventions Against SARS-CoV-2: A Comprehensive Review, Journal of Agriculture and Food Research, doi:10.1016/j.jafr.2024.101422.
14.
Wimalawansa (C), S., Unlocking Insights: Navigating COVID-19 Challenges and Emulating Future Pandemic Resilience Strategies with Strengthening Natural Immunity, Heliyon, doi:10.1016/j.heliyon.2024.e34691.
15.
Imran et al., Therapeutic Role of Vitamin D in COVID-19 Patients, Clinical Nutrition Open Science, doi:10.1016/j.nutos.2024.07.004.
16.
Grant, W., Vitamin D and viral infections: Infectious diseases, autoimmune diseases, and cancers, Advances in Food and Nutrition Research, doi:10.1016/bs.afnr.2023.12.007.
17.
Polonowita et al., Molecular Quantum and Logic Process of Consciousness—Vitamin D Big-Data in COVID-19—A Case for Incorporating Machine Learning In Medicine, European Journal of Biomedical and Pharmaceutical sciences, doi:10.5281/zenodo.10435649.
18.
Gomaa et al., Pharmacological evaluation of vitamin D in COVID-19 and long COVID-19: recent studies confirm clinical validation and highlight metformin to improve VDR sensitivity and efficacy, Inflammopharmacology, doi:10.1007/s10787-023-01383-x.
19.
Gotelli et al., Understanding the immune-endocrine effects of vitamin D in SARS-CoV-2 infection: a role in protecting against neurodamage?, Neuroimmunomodulation, doi:10.1159/000533286.
20.
Cutolo et al., Involvement of the secosteroid vitamin D in autoimmune rheumatic diseases and COVID-19, Nature Reviews Rheumatology, doi:10.1038/s41584-023-00944-2.
21.
Schloss et al., Nutritional deficiencies that may predispose to long COVID, Inflammopharmacology, doi:10.1007/s10787-023-01183-3.
22.
Arora et al., Global Dietary and Herbal Supplement Use during COVID-19—A Scoping Review, Nutrients, doi:10.3390/nu15030771.
23.
Nicoll et al., COVID-19 Prevention: Vitamin D Is Still a Valid Remedy, Journal of Clinical Medicine, doi:10.3390/jcm11226818.
24.
Foshati et al., Antioxidants and clinical outcomes of patients with coronavirus disease 2019: A systematic review of observational and interventional studies, Food Science & Nutrition, doi:10.1002/fsn3.3034.
25.
Quesada-Gomez et al., Vitamin D Endocrine System and COVID-19: Treatment with Calcifediol, Nutrients, doi:10.3390/nu14132716.
26.
DiGuilio et al., Micronutrient Improvement of Epithelial Barrier Function in Various Disease States: A Case for Adjuvant Therapy, International Journal of Molecular Sciences, doi:10.3390/ijms23062995.
27.
Grant (B) et al., A Narrative Review of the Evidence for Variations in Serum 25-Hydroxyvitamin D Concentration Thresholds for Optimal Health, Nutrients, doi:10.3390/nu14030639.
28.
Shah Alam et al., The role of vitamin D in reducing SARS-CoV-2 infection: An update, International Immunopharmacology, doi:10.1016/j.intimp.2021.107686.
29.
Griffin et al., Perspective: Vitamin D supplementation prevents rickets and acute respiratory infections when given as daily maintenance but not as intermittent bolus: implications for COVID-19, Clinical Medicine, doi:10.7861/clinmed.2021-0035.
30.
Kohlmeier et al., When Mendelian randomisation fails, BMJ Nutrition, Prevention & Health, doi:10.1136/bmjnph-2021-000265.
31.
Brenner, H., Vitamin D Supplementation to Prevent COVID-19 Infections and Deaths—Accumulating Evidence from Epidemiological and Intervention Studies Calls for Immediate Action, Nutrients, doi:10.3390/nu13020411.
32.
Mercola et al., Evidence Regarding Vitamin D and Risk of COVID-19 and Its Severity, Nutrients 2020, 12:11, 3361, doi:10.3390/nu12113361.
33.
Basha et al., Is the shielding effect of cholecalciferol in SARS CoV-2 infection dependable? An evidence based unraveling, Clinical Epidemiology and Global Health, doi:10.1016/j.cegh.2020.10.005.
34.
Xu et al., The importance of vitamin d metabolism as a potential prophylactic, immunoregulatory and neuroprotective treatment for COVID-19, Journal of Translational Medicine, doi:10.1186/s12967-020-02488-5.
35.
Alexander et al., Early Nutritional Interventions with Zinc, Selenium and Vitamin D for Raising Anti-Viral Resistance Against Progressive COVID-19, Nutrients, doi:10.3390/nu12082358.
36.
Andrade et al., Vitamin A and D deficiencies in the prognosis of respiratory tract infections: A systematic review with perspectives for COVID-19 and a critical analysis on supplementation, SciELO preprints, doi:10.1590/SciELOPreprints.839.
37.
Grant (C) et al., Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths, Nutrients, 12:4, 988, doi:10.3390/nu12040988.
38.
McCullough et al., Daily oral dosing of vitamin D3 using 5000 TO 50,000 international units a day in long-term hospitalized patients: Insights from a seven year experience, The Journal of Steroid Biochemistry and Molecular Biology, doi:10.1016/j.jsbmb.2018.12.010.
39.
EFSA, Scientific Opinion on the substantiation of health claims related to vitamin D and normal function of the immune system and inflammatory response (ID 154, 159), maintenance of normal muscle function (ID 155) and maintenance of normal cardiovascular function (ID 159) pursuant to Article 13(1) of Regulation (E, EFSA Journal, doi:10.2903/j.efsa.2010.1468.
40.
EFSA (B), Scientific Opinion on the substantiation of a health claim related to vitamin D and contribution to the normal function of the immune system pursuant to Article 14 of Regulation (EC) No 1924/2006, EFSA Journal, doi:10.2903/j.efsa.2015.4096.
Schloss et al., 15 Mar 2023, peer-reviewed, 1 author.
Nutritional deficiencies that may predispose to long COVID
Inflammopharmacology, doi:10.1007/s10787-023-01183-3
Multiple nutritional deficiencies (MND) confound studies designed to assess the role of a single nutrient in contributing to the initiation and progression of disease states. Despite the perception of many healthcare practitioners, up to 25% of Americans are deficient in five-or-more essential nutrients. Stress associated with the COVID-19 pandemic further increases the prevalence of deficiency states. Viral infections compete for crucial nutrients with immune cells. Viral replication and proliferation of immunocompetent cells critical to the host response require these essential nutrients, including zinc. Clinical studies have linked levels of more than 22 different dietary components to the likelihood of COVID-19 infection and the severity of the disease. People at higher risk of infection due to MND are also more likely to have long-term sequelae, known as Long COVID.
Declarations Conflict of interest The author declares that he has no conflict of interest, financial or otherwise. Consent for publication Not applicable.
References
Akasov, Khaydukov, Andreyuk, Sholina, Sheremeta et al., Riboflavin for COVID-19 adjuvant treatment in patients with mental health disorders: observational study, Front Pharmacol, doi:10.3389/fphar.2022.755745
Alexander, Davidson, Intranasal zinc and anosmia: the zinc-induced anosmia syndrome, Laryngoscope, doi:10.1097/01.mlg.0000191549.17796.13
Alexander, Debiec, Razzaque, He, Inorganic phosphate-induced cytotoxicity, IUBMB Life, doi:10.1002/iub.2561
Alfano, Ferrari, Fontana, Perrone, Mori et al., Hypokalemia in patients with COVID-19, Clin Exp Nephrol, doi:10.1007/s10157-020-01996-4
Alker, Schwerdtle, Schomburg, Haase, A Zinpyr-1-based fluorimetric microassay for free zinc in human serum, Int J Mol Sci, doi:10.3390/ijms20164006
Andreou, None
Andreou, Trantza, Filippou, Sipsas, Tsiodras, COVID-19: The potential role of copper and N-acetylcysteine (NAC) in a combination of candidate antiviral treatments against SARS-CoV-2, Vivo, doi:10.21873/invivo.11946
Aratani, Myeloperoxidase: Its role for host defense, inflammation, and neutrophil function, Arch Biochem Biophys, doi:10.1016/j.abb.2018.01.004
Ardestani, Azizi, Targeting glucose metabolism for treatment of COVID-19, Signal Transduct Target Ther, doi:10.1038/s41392-021-00532-4
Assimakopoulos, Komninos, Dimitropoulou, Lagadinou, Leonidou et al., N-acetyl-cysteine reduces the risk for mechanical ventilation and mortality in patients with COVID-19 pneumonia: a twocenter retrospective cohort study, Infect Dis (lond), doi:10.1080/23744235.2021.1945675
Barceloux, Selenium, J Toxicol Clin Toxicol, doi:10.1081/clt-100102417
Belikov, Schraven, Simeoni, T cells and reactive oxygen species, J Biomed Sci, doi:10.1186/s12929-015-0194-3
Biancatelli, Berrill, Catravas, Marik, Quercetin and vitamin C: an experimental, synergistic therapy for the prevention and treatment of SARS-CoV-2 related disease (COVID-19), Front Immunol, doi:10.3389/fimmu.2020.01451
Bioflavonoids (derosa, None
Bird, Risk of deficiency in multiple concurrent micronutrients in children and adults in the United States, Nutrients, doi:10.3390/nu9070655
Bizzarri, Laganà, Aragona, Unfer, Inositol and pulmonary function. Could myo-inositol treatment downregulate inflammation and cytokine release syndrome in SARS-CoV-2?, Eur Rev Med Pharmacol Sci, doi:10.26355/eurrev_202003_20715
Bizzarri, None
Branco De Oliveira, Irikura, Lourenço, Shinsato, Irikura et al., Encephalopathy responsive to thiamine in severe COVID-19 patients, Brain Behav Immun Health, doi:10.1016/j.bbih.2021.100252
Branco De Oliveira, Kumrungsee et al
Bucci, A functional analytical technique for monitoring nutrient status and repletion. Part 3: clinical experience, Am Clin Lab
Camp, Bai, Gonullu, Nayak, Hm, Melatonin interferes with COVID-19 at several distinct ROS-related steps, J Inorg Biochem, doi:10.1016/j.jinorgbio.2021.111546
Carr, Hawkins, Thomas, Stocker, Frei, Relative reactivities of N-chloramines and hypochlorous acid with human plasma constituents, Free Radic Biol Med, doi:10.1016/s0891-5849(00)00495-0
Carr, Winterbourn, Oxidation of neutrophil glutathione and protein thiols by myeloperoxidase-derived hypochlorous acid, Biochem J, doi:10.1042/bj3270275
Cengiz, Uysal, Ikitimur, Ozcan, Islamoğlu et al., Effect of oral L-glutamine supplementation on Covid-19 treatment, Clin Nutr Exp, doi:10.1016/j.yclnex.2020.07.003
Chen, An original discovery: selenium deficiency and Keshan disease (an endemic heart disease), Asia Pac J Clin Nutr
Chillon, Maares, Demircan, Hackler, Sun et al., Serum free zinc is associated with vaccination response to SARS-CoV-2, Front Immunol, doi:10.3389/fimmu.2022.906551
Cholecalciferol/Vitamin D (galmés, None
Cory, Cory, Critical roles of glutamine as nitrogen donors in purine and pyrimidine nucleotide synthesis: asparaginase treatment in childhood acute lymphoblastic leukemia, Vivo
Cysteine, Shi, Assimakopoulos, None
Dabbagh-Bazarbachi, Clergeaud, Quesada, Ortiz, Sullivan et al., Zinc ionophore activity of quercetin and epigallocatechin-gallate: from Hepa 1-6 cells to a liposome model, J Agric Food Chem, doi:10.1021/jf5014633
Dalbeni, Bevilacqua, Teani, Normelli, Mazzaferri et al., Excessive vitamin B12 and poor outcome in COVID-19 pneumonia, Nutr Metab Cardiovasc Dis, doi:10.1016/j.numecd.2020.12.005
Das, Can bioactive lipids inactivate coronavirus (COVID-19)?, Arch Med Res, doi:10.1016/j.arcmed.2020.03.004
De Alencar, Clemente-Suárez et al
De Alencar, Moreira, Müller, Chaves, Fukuhara et al., Double-blind, randomized, placebocontrolled trial with N-acetylcysteine for treatment of severe acute respiratory syndrome caused by Coronavirus disease 2019 (COVID-19), Clin Infect Dis, doi:10.1093/cid/ciaa1443
Derosa, Maffioli, Angelo, Pierro, A role for quercetin in coronavirus disease 2019 (COVID-19), Phytother Res, doi:10.1002/ptr.6887
Dharmalingam, Birdi, Tomo, Sreenivasulu, Charan et al., Trace elements as immunoregulators in SARS-CoV-2 and other viral infections, Indian J Clin Biochem, doi:10.1007/s12291-021-00961-6
Dharmalingam, phosphorus (van Kempen and Deixler
Doaei, Gholami, Rastgoo, Gholamalizadeh, Bourbour et al., The effect of omega-3 fatty acid supplementation on clinical and biochemical parameters of critically ill patients with COVID-19: a randomized clinical trial, J Transl Med, doi:10.1186/s12967-021-02795-5
Drakesmith, None
Drakesmith, Pasricha, Cabantchik, Hershko, Weiss et al., Vaccine efficacy and iron deficiency: an intertwined pair?, Lancet Haematol, doi:10.1016/S2352-3026(21)00201-5
Du, Luo, Ni, Hussain, Selenium and hazardous elements distribution in plant-soil-water system and human health risk assessment of lower Cambrian, Southern Shaanxi, China, Environ Geochem Health, doi:10.1007/s10653-018-0082-3
El-Kurdi, Khatua, Rood, Snozek, Cartin-Ceba et al., Mortality from coronavirus disease 2019 increases with unsaturated fat and may be reduced by early calcium and albumin supplementation, Gastroenterology, doi:10.1053/j.gastro.2020.05.057
Elham, Vitamin B12 deficiency in COVID-19 recovered patients: case report, Int J Pharma Res
Engström, Zetterberg, Phosphate and the regulation of DNA replication in normal and virus-transformed 3T3 cells, Biochem J, doi:10.1042/bj2140695
Eskander, Razzaque, Can maintaining optimal magnesium balance reduce the disease severity of COVID-19 patients?, Front Endocrinol, doi:10.3389/fendo.2022.843152
Españo, Kim, Lee, Kim, Phytochemicals for the treatment of COVID-19, J Microbiol, doi:10.1007/s12275-021-1467-z
Españo, None
Espinola, Bertelli, Bizzarri, Unfer, Laganà et al., Inositol and vitamin D may naturally protect human reproduction and women undergoing assisted reproduction from covid-19 risk, J Reprod Immunol, doi:10.1016/j.jri.2021.103271
Evanics, Maurmann, Yang, Bose, Nuclear magnetic resonance structures of the zinc finger domain of human DNA polymerase-alpha, Biochim Biophys Acta, doi:10.1016/s1570-9639(03)00266-8
Fairweather-Tait, Bao, Broadley, Collings, Ford et al., Selenium in human health and disease, Antioxid Redox Signal, doi:10.1089/ars.2010.3275
Fakhrolmobasheri, Mazaheri-Tehrani, Kieliszek, Zeinalian, Abbasi et al., COVID-19 and selenium deficiency: a systematic review, Biol Trace Elem Res, doi:10.1007/s12011-021-02997-4
Flora, Balansky, Maestra, Rationale for the use of N-acetylcysteine in both prevention and adjuvant therapy of COVID-19, FASEB J, doi:10.1096/fj.202001807
Flora, None
Fosmire, Zinc toxicity, Am J Clin Nutr, doi:10.1093/ajcn/51.2.225
Freedman, Hunter, Law, 'alessandro, Noonan et al., Maternal choline and respiratory coronavirus effects on fetal brain development, J Psychiatr Res, doi:10.1016/j.jpsychires.2020.05.019
Freedman, selenium
Fröhlich, Wahl, Physiological role and use of thyroid hormone metabolites -potential utility in COVID-19 patients, Front Endocrinol, doi:10.3389/fendo.2021.587518
Galmés, None
Galmés, Serra, Palou, Current state of evidence: influence of nutritional and nutrigenetic factors on immunity in the COVID-19 pandemic framework, Nutrients, doi:10.3390/nu12092738
Galmés, iodine
Gheorghe, Ilie, Bungau, Stoian, Bacalbasa et al., Is there a relationship between COVID-19 and hyponatremia?, Medicina (kaunas), doi:10.3390/medicina57010055
Glover, Basa, Moore, Laurence, Sreedhara, Metal ion interactions with mAbs: part 1, Mabs, doi:10.1080/19420862.2015.1062193
Goc, Niedzwiecki, Rath, Polyunsaturated ω-3 fatty acids inhibit ACE2-controlled SARS-CoV-2 binding and cellular entry, Sci Rep, doi:10.1038/s41598-021-84850-1
Goc, retinoic acid/vitamin A (Galmés et al
Goud, Bai, Hm, A multiple-hit hypothesis involving reactive oxygen species and myeloperoxidase explains clinical deterioration and fatality in COVID-19, Int J Biol Sci, doi:10.7150/ijbs.51811
Goyal, Basak, Human catalase: looking for complete identity, Protein Cell, doi:10.1007/s13238-010-0113-z
Grant, Lahore, Mcdonnell, Baggerly, French et al., Evidence that Vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths, Nutrients, doi:10.3390/nu12040988
Grant, None
Haase, Rink, Zinc signals and immune function, BioFactors, doi:10.1002/biof.1114
Habib, Ibrahim, Zaim, Ibrahim, The role of iron in the pathogenesis of COVID-19 and possible treatment with lactoferrin and other iron chelators, Biomed Pharmacother, doi:10.1016/j.biopha.2021.111228
Hackbarth, Islam, Šubr, Etrych, Fang, Singlet oxygen in vivo: It is all about intensity, J Pers Med, doi:10.3390/jpm12060891
Hariharan, Dharmaraj, Selenium and selenoproteins: it's role in regulation of inflammation, Inflammopharmacology, doi:10.1007/s10787-020-00690-x
Heller, Sun, Hackler, Seelig, Seibert et al., Prediction of survival odds in COVID-19 by zinc, age and selenoprotein P as composite biomarker, Redox Biol, doi:10.1016/j.redox.2020.101764
Hemila, De Man, Vitamin C and COVID-19, Front Med (lausanne), doi:10.3389/fmed.2020.559811
Hemilä, De Man, Holford, None
Holford, Carr, Jovic, Ali, Whitaker et al., Vitamin C-an adjunctive therapy for respiratory infection, sepsis and COVID-19, Nutrients, doi:10.3390/nu12123760
Holick, Sunlight, UV radiation, vitamin D, and skin cancer: how much sunlight do we need?, Adv Exp Med Biol, doi:10.1007/978-3-030-46227-7_2
Houillier, Salles, Biochemical assessment of phosphate homeostasis, Arch Pediatr, doi:10.1016/j.arcped.2021.09.001
Im, Je, Baek, Chung, Kwon et al., Nutritional status of patients with COVID-19, Int J Infect Dis, doi:10.1016/j.ijid.2020.08.018
Iwegbulem, Wang, Pfirrmann, Redmond, The role of taurine derivatives in the putative therapy of COVID-19-induced inflammation, Ir J Med Sci, doi:10.1007/s11845-021-02522-5
Jose, Magoon, Kapoor, Magnesium: the neglected cation in COVID-19?, J Anaesthesiol Clin Pharmacol, doi:10.4103/joacp.JOACP_628_20
Kanofsky, Singlet oxygen production by biological systems, Chem Biol Interact, doi:10.1016/0009-2797(89)90059-8
Kapur, Sharma, Sageena, Therapeutic potential of N-acetyl cysteine during COVID-19 epoch, World J Virol, doi:10.5501/wjv.v11.i2.104
Kaya, None
Kaya, Pamukçu, Yakar, The role of vitamin D deficiency on COVID-19: a systematic review and meta-analysis of observational studies, Epidemiol Health, doi:10.4178/epih.e2021074
Khatiwada, Subedi, A mechanistic link between selenium and coronavirus disease 2019 (COVID-19), Curr Nutr Rep, doi:10.1007/s13668-021-00354-4
Kim, Cha, Taurine chloramine produced from taurine under inflammation provides anti-inflammatory and cytoprotective effects, Amino Acids, doi:10.1007/s00726-013-1545-6
Kogan, Sood, Garnick, Zinc and wound healing: a review of zinc physiology and clinical applications, Wounds
Krishnaven, Maternal B12, Folate and homocysteine concentrations and offspring cortisol and cardiovascular responses to stress, J Clin Endocrinol Metab, doi:10.1210/clinem/dgz114
Kumrungsee, Zhang, Chartkul, Yanaka, Kato, Potential role of vitamin B6 in ameliorating the severity of COVID-19 and its complications, Front Nutr, doi:10.3389/fnut.2020.562051
Laganà, Unfer, Garzon, Bizzarri, Role of inositol to improve surfactant functions and reduce IL-6 levels: a potential adjuvant strategy for SARS-CoV-2 pneumonia?, Med Hypotheses, doi:10.1016/j.mehy.2020.110262
Laing, None
Laing, Petrovic, Lachat, Boevre, Klingenberg et al., Course and survival of COVID-19 patients with comorbidities in relation to the trace element status at hospital admission, Nutrients, doi:10.3390/nu13103304
Landis, Getachew, Tizabi, Therapeutic potential of flavonoids and zinc in COVID-19, Medpress Nutr Food Sci
Liu, Zhang, Weng, Yang, Fan et al., Association between average plasma potassium levels and 30-day mortality during hospitalization in patients with COVID-19 in Wuhan, China Int J Med Sci, doi:10.7150/ijms.50965
Liu, Zhu, Zhang, Li, Peng, Intravenous high-dose vitamin C for the treatment of severe COVID-19: study protocol for a multicentre randomised controlled trial, BMJ Open, doi:10.1136/bmjopen-2020-039519
Lopresti, The effects of psychological and environmental stress on micronutrient concentrations in the body: a review of the evidence, Adv Nutr, doi:10.1093/advances/nmz082
Luzzatto, Ally, Notaro, Glucose-6-phosphate dehydrogenase deficiency, Blood, doi:10.1182/blood.2019000944
Maares, Hackler, Haupt, Heller, Bachmann et al., Free zinc as a predictive marker for COVID-19 mortality risk, Nutrients, doi:10.3390/nu14071407
Magnani, Nenci, Fananas, Ceccon, Romero et al., Crystal structures and atomic model of NADPH oxidase, Proc Natl Acad Sci U S A, doi:10.1073/pnas.1702293114
Maitra, Shaeib, Abdulhamid, Abdulridha, Saed et al., Myeloperoxidase acts as a source of free iron during steady-state catalysis by a feedback inhibitory pathway, Free Radic Biol Med, doi:10.1016/j.freeradbiomed.2013.04.009
Mallouh, Yk, Bacterial infections in children with glucose-6-phosphate dehydrogenase deficiency, J Pediatr, doi:10.1016/s0022-3476(87)80202-0
Marcinkiewicz, Kontny, Taurine and inflammatory diseases, Amino Acids, doi:10.1007/s00726-012-1361-4
Martinez, Huang, Acuna, Laverde, Trujillo et al., Role of selenium in viral infections with a major focus on SARS-CoV-2, Int J Mol Sci, doi:10.3390/ijms23010280
Mascio, Devasagayam, Kaiser, Sies, Carotenoids, tocopherols and thiols as biological singlet molecular oxygen quenchers, Biochem Soc Trans, doi:10.1042/bst0181054
Mascio, Martinez, Miyamoto, Ronsein, Medeiros et al., Singlet molecular oxygen reactions with nucleic acids, lipids, and proteins, Chem Rev, doi:10.1021/acs.chemrev.8b00554
Matsushita, Freigang, Schneider, Conrad, Bornkamm et al., T cell lipid peroxidation induces ferroptosis and prevents immunity to infection, J Exp Med, doi:10.1084/jem.20140857
Matsuyama, Yoshinaga, Shibue, Mak, Comorbidity-associated glutamine deficiency is a predisposition to severe COVID-19, Cell Death Differ, doi:10.1038/s41418-021-00892-y
Mayadas, Cullere, Lowell, The multifaceted functions of neutrophils, Annu Rev Pathol, doi:10.1146/annurev-pathol-020712-164023
Mehta, Flores, Walters, Sreedhara, Metal ion interactions with mAbs: Part 2. Zinc-mediated aggregation of IgG1 monoclonal antibodies, Pharm Res, doi:10.1007/s11095-021-03089-7
Meisel, Efros, Bleier, Halevi, Segal et al., Folate levels in patients hospitalized with coronavirus disease, Nutrients, doi:10.3390/nu13030812
Miyamoto, Ronsein, Prado, Uemi, Corrêa et al., Biological hydroperoxides and singlet molecular oxygen generation, IUBMB Life, doi:10.1080/15216540701242508
Moghaddam, Heller, Sun, Seelig, Cherkezov et al., Selenium deficiency is associated with mortality, Nutrients, doi:10.3390/nu12072098
Mohanty, Padhy, Das, Meher, Therapeutic potential of N-acetyl cysteine (NAC) in preventing cytokine storm in COVID-19 review of current evidence, Eur Rev Med Pharmacol Sci, doi:10.26355/eurrev_202103_25442
Mp, N-acetylcysteine as a potential treatment for COVID-19, Future Microbiol, doi:10.2217/fmb-2020-0074
Muller, Lustgarten, Jang, Richardson, Van Remmen, Trends in oxidative aging theories, Free Radic Biol Med, doi:10.1016/j.freeradbiomed.2007.03.034
Muri, Heer, Matsushita, Pohlmeier, Tortola et al., The thioredoxin-1 system is essential for fueling DNA synthesis during T-cell metabolic reprogramming and proliferation, Nat Commun, doi:10.1038/s41467-018-04274-w
Nagarkoti, Dubey, Sadaf, Awasthi, Chandra et al., Catalase S-glutathionylation by NOX2 and mitochondrial-derived ROS adversely affects mice and human neutrophil survival, Inflammation, doi:10.1007/s10753-019-01093-z
Nai, Lorè, Pagani, Lorenzo, Modica et al., Hepcidin levels predict Covid-19 severity and mortality in a cohort of hospitalized Italian patients, Am J Hematol, doi:10.1002/ajh.26027
Nauseef, Myeloperoxidase deficiency, Hematol Oncol Clin North Am
Neiers, Jarriault, Menetrier, Briand, Heydel, The odorant metabolizing enzyme UGT2A1: immunolocalization and impact of the modulation of its activity on the olfactory response, PLoS ONE, doi:10.1371/journal.pone.0249029
Noori, Nejadghaderi, Sullman, Carson-Chahhoud, Kolahi et al., Epidemiology, prognosis and management of potassium disorders in covid-19, Rev Med Virol, doi:10.1002/rmv.2262
Noori, None
Noreng, Ota, Sun, Ho, Johnson et al., Structure of the core human NADPH oxidase NOX2, Nat Commun, doi:10.1038/s41467-022-33711-0
Notz, Herrmann, Schlesinger, Helmer, Sudowe et al., Clinical significance of micronutrient supplementation in critically ill COVID-19 patients with severe ARDS, Nutrients, doi:10.3390/nu13062113
Nowak, Szewczyk, Pilc, Zinc and depression. An update, Pharmacol Rep
Nutt, Hodgkin, Tarlinton, Corcoran, The generation of antibody-secreting plasma cells, Nat Rev Immunol, doi:10.1038/nri3795
Olivari, Riccardi, Rodari, Angheben, Artioli et al., COVID-19 pneumonia: increased choline uptake with 18F-choline PET/CT, Eur J Nucl Med Mol Imaging, doi:10.1007/s00259-020-04870-3
Osman, Fahdi, Salmi, Khalili, Gokhale et al., Serum calcium and vitamin D levels: correlation with severity of COVID-19 in hospitalized patients in royal hospital, Oman, Int J Infect Dis, doi:10.1016/j.ijid.2021.04.050
Panchariya, Khan, Kuila, Sonkar, Sahoo et al., Zinc 2+ ion inhibits SARS-CoV-2 main protease and viral replication in vitro, Chem Commun (camb), doi:10.1039/d1cc03563k
Petrucco, Percudani, Structural recognition of DNA by poly(ADP-ribose)polymerase-like zinc finger families, FEBS J, doi:10.1111/j.1742-4658.2008.06259.x
Peyneau, Granger, Wicky, Khelifi-Touhami, Timsit et al., Innate immune deficiencies are associated with severity and poor prognosis in patients with COVID-19, Sci Rep, doi:10.1038/s41598-021-04705-7
Pierro, Khan, Bertuccioli, Maffioli, Derosa et al., Quercetin phytosome® as a potential candidate for managing COVID-19, doi:10.23736/S2724-5985.20.02771-3
Pisano, Hilas, Zinc and taste disturbances in older adults: a review of the literature, Consult Pharm, doi:10.4140/TCP.n.2016.267
Prasad, Discovery of human zinc deficiency: its impact on human health and disease, Nutrition, doi:10.3945/an.112.003210
Raines, Ganatra, Nissaisorakarn, Pandit, Morales et al., Niacinamide may be associated with improved outcomes in COVID-19-related acute kidney injury: an observational study, Kidney, doi:10.34067/KID.0006452020
Raines, niacinamide/vitamin B 3
Read, Obeid, Ahlenstiel, Ahlenstiel, The role of zinc in antiviral immunity, Adv Nutr, doi:10.1093/advances/nmz013
Reusch, Domenico, Bonaguro, Schulte-Schrepping, Baßler et al., Neutrophils in COVID-19, Front Immunol, doi:10.3389/fimmu.2021.652470
Rosenblum, Wessler, Gupta, Maurer, Bikdeli, Zinc deficiency and heart failure: a systematic review of the current literature, J Card Fail, doi:10.1016/j.cardfail.2020.01.005
Schomburg, Selenium deficiency in COVID-19-a possible long-lasting toxic relationship, Nutrients, doi:10.3390/nu14020283
Schuller-Levis, Park, Taurine: new implications for an old amino acid, FEMS Microbiol Lett, doi:10.1016/S0378-1097(03)00611-6
Schöllhammer, Poll, Bickel, Liver microsomal beta-glucuronidase and UDP-glucuronyltransferase, Enzyme, doi:10.1159/000458949
Seers, Davenport, Phosphate metabolism and respiratory alkalosis: a forgotten lesson in COVID-19, Age Ageing, doi:10.1093/ageing/afaa176
Sengupta, Holmgren, Thioredoxin and glutaredoxinmediated redox regulation of ribonucleotide reductase, World J Biol Chem, doi:10.4331/wjbc.v5.i1.68
Shauly-Aharonov, Shafrir, Paltiel, Calderon-Margalit, Safadi et al., Both high and low pre-infection glucose levels associated with increased risk for severe COVID-19: new insights from a population-based study, PLoS ONE, doi:10.1371/journal.pone.0254847
Shelton, Shastri, Fletez-Brant, Aslibekyan, Auton, The UGT2A1/UGT2A2 locus is associated with COVID-19-related loss of smell or taste, Nat Genet, doi:10.1038/s41588-021-00986-w
Shi, Puyo, N-Acetylcysteine to combat COVID-19: An evidence review, Ther Clin Risk Manag, doi:10.2147/TCRM.S273700
Shive, Pinkerton, Humphreys, Johnson, Hamilton et al., Development of a chemically defined serum-and protein-free medium for growth of human peripheral lymphocytes, Proc Natl Acad Sci, doi:10.1073/pnas.83.1.9
Shrivastava, Chelluboina, Jedge, Doke, Palkar et al., Elevated levels of neutrophil activated proteins, alpha-defensins (DEFA1), calprotectin (S100A8/A9) and myeloperoxidase (MPO) are associated with disease severity in COVID-19 patients, Front Cell Infect Microbiol, doi:10.3389/fcimb.2021.751232
Singh, Chhabra, Patel, Chang, Ahmad, Dietary phytochemicals in zinc homeostasis: a strategy for prostate cancer management, Nutrients, doi:10.3390/nu13061867
Skesters, Kustovs, Lece, Moreino, Petrosina et al., Selenium, selenoprotein P, and oxidative stress levels in SARS-CoV-2 patients during illness and recovery, Inflammopharmacology, doi:10.1007/s10787-022-00925-z
Skovsen, Snyder, Lambert, Ogilby, Lifetime and diffusion of singlet oxygen in a cell, J Phys Chem B, doi:10.1021/jp051163i
Skrajnowska, Bobrowska-Korczak, Role of zinc in immune system and anti-cancer defense mechanisms, Nutrients, doi:10.3390/nu11102273
Sodium ; Gheorghe, Olfactory disturbances as presenting manifestation among Egyptian patients with COVID-19: possible role of zinc, Biol Trace Elem Res, doi:10.1007/s12011-020-02546-5
Soliman, None
Soliman, Thabet, Abudahab, Kamel, The impact of glutamine supplementation on the short-term mortality of COVID-19 diseased patients admitted to the ICU: A single-blind randomized clinical trial, Egypt J Anaesth, doi:10.1080/11101849.2022.2031811
Stief, Singlet oxygen potentiates thrombolysis, Clin Appl Thromb Hemost, doi:10.1177/1076029607302404
Stief, The physiology and pharmacology of singlet oxygen, Med Hypotheses, doi:10.1016/s0306-9877(03)00026-4
Stockwell, Jiang, Gu, Emerging mechanisms and disease relevance of ferroptosis, Trends Cell Biol, doi:10.1016/j.tcb.2020.02.009
Sulaiman, Aljuhani, Dossari, Alshahrani, Alharbi et al., Evaluation of thiamine as adjunctive therapy in COVID-19 critically ill patients: a two-center propensity score matched study, Crit Care, doi:10.1186/s13054-021-03648-9
Taneri, Gómez-Ochoa, Llanaj, Raguindin, Rojas et al., Anemia and iron metabolism in COVID-19: a systematic review and meta-analysis, Eur J Epidemiol, doi:10.1007/s10654-020-00678-5
Tom ; Dieck, Döring, Roth, Daniel, Changes in rat hepatic gene expression in response to zinc deficiency as assessed by DNA arrays, J Nutr, doi:10.1093/jn/133.4.1004
Trapani, Rosanoff, Baniasadi, Barbagallo, Castiglioni et al., Deixler E (2021) SARS-CoV-2: influence of phosphate and magnesium, moderated by vitamin D, on energy (ATP) metabolism and on severity of COVID-19, Am J Physiol Endocrinol Metab, doi:10.1152/ajpendo.00474.2020
Van Eijk, Offringa, Bernal, Bourgonje, Van Goor et al., The disease-modifying role of taurine and its therapeutic potential in coronavirus disease 2019 (COVID-19), Adv Exp Med Biol, doi:10.1007/978-3-030-93337-1_1
Van Kempen, Deixler, None, Ardestani and Azizi
Van Kempen, Deixler, Weir, None
Vazirani, COVID-19, an incentive to tackle sugar in hospitals and at home, J Endocr Soc, doi:10.1210/jendso/bvab037
Vick, Glucose-6-phosphate dehydrogenase deficiency and COVID-19 infection, Mayo Clin Proc, doi:10.1016/j.mayocp.2020.05.035
Vj, Ramos-Campo, Mielgo-Ayuso, Dalamitros, Nikolaidis et al., Nutrition in the actual COVID-19 pandemic, Narrat Rev Nutr, doi:10.3390/nu13061924
Vucić, Gavella, Bozikov, Ashcroft, Rocić, Superoxide dismutase activity in lymphocytes and polymorphonuclear cells of diabetic patients, Eur J Clin Chem Clin Biochem, doi:10.1515/cclm.1997.35.7.517
Wang, Shen, Tao, Fairley, Zhong et al., Elevated glucose level leads to rapid COVID-19 progression and high fatality, BMC Pulm Med, doi:10.1186/s12890-021-01413-w
Wee, COVID-19's toll on the elderly and those with diabetes mellitus -is vitamin B12 deficiency an accomplice?, Med Hypotheses, doi:10.1016/j.mehy.2020.110374
Weir, Thenappan, Bhargava, Chen, Does vitamin D deficiency increase the severity of COVID-19?, Clin Med (lond), doi:10.7861/clinmed.2020-0301
Wessels, Maywald, Rink, Zinc as a gatekeeper of immune function, Nutrients, doi:10.3390/nu9121286
Williams, Winterbourn, Biochemical individuality, the basis for the genetotrophic concept, Annu Rev Biochem, doi:10.1146/annurev-biochem-060815-014442
Witter, Okunnu, Berg, The essential role of neutrophils during infection with the intracellular bacterial pathogen Listeria monocytogenes, J Immunol, doi:10.4049/jimmunol.1600599
Wong, Lee, Kua, N-Acetylcysteine as adjuvant therapy for COVID-19 -a perspective on the current state of the evidence, J Inflamm Res, doi:10.2147/JIR.S306849
Wong, None
Xu, Liu, Zou, Luo, Wu et al., Hypozincemia in COVID-19 patients correlates with stronger antibody response, Front Immunol, doi:10.3389/fimmu.2021.785599
Yamaguchi, Mori, Suketa, Effects of Ca2+, Zn2+ and Cd2+ on uridine diphosphate-glucuronyltransferase and beta-glucuronidase activities in rat liver microsomes, Chem Pharm Bull (tokyo), doi:10.1248/cpb.38.159
Yamanaka, Matsugano, Yoshikawa, Orino, Binding analysis of human immunoglobulin G as a zinc-binding protein, Antibodies, doi:10.3390/antib5020013
Yang, Ma, Wu, Han, Zheng et al., Low serum calcium and phosphorus and their clinical performance in detecting COVID-19 patients, J Med Virol, doi:10.1002/jmv.26515
Yang, Stockwell, Ferroptosis: death by lipid peroxidation, Trends Cell Biol, doi:10.1016/j.tcb.2015.10.014
Yin, Mao, Luan, Shen, Shen et al., Structural basis for inhibition of the RNA-dependent RNA polymerase from SARS-CoV-2 by remdesivir, Science, doi:10.1126/science.abc1560
Zahra, Iddawela, Pillai, Choudhury, Harky, Can symptoms of anosmia and dysgeusia be diagnostic for COVID-19?, Brain Behav, doi:10.1002/brb3.1839
Zeng, Yang, Yuan, Wang, Cheng, Associations of essential and toxic metals/metalloids in whole blood with both disease severity and mortality in patients with COVID-19, FASEB J, doi:10.1096/fj.202002346RR
Zetterberg, Engström, Glutamine and the regulation of DNA replication and cell multiplication in fibroblasts, J Cell Physiol, doi:10.1002/jcp.1041080310
Zhang, Taylor, Bennett, Saad, Rayman, Association between regional selenium status and reported outcome of COVID-19 cases in China, Am J Clin Nutr, doi:10.1093/ajcn/nqaa095
Zhou, Chen, Wang, Zhao, Wei et al., Low serum calcium: a new, important indicator of COVID-19 patients from mild/moderate to severe/critical, Biosci Rep, doi:10.1042/BSR20202690
Zhou, Yang, Huang, Chen, The potential mechanism of N-acetylcysteine in treating COVID-19, Curr Pharm Biotechnol, doi:10.2174/1389201021999201228212043
schloss
