Vitamin D Endocrine System and COVID-19: Treatment with Calcifediol
et al., Nutrients, doi:10.3390/nu14132716, Jun 2022
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
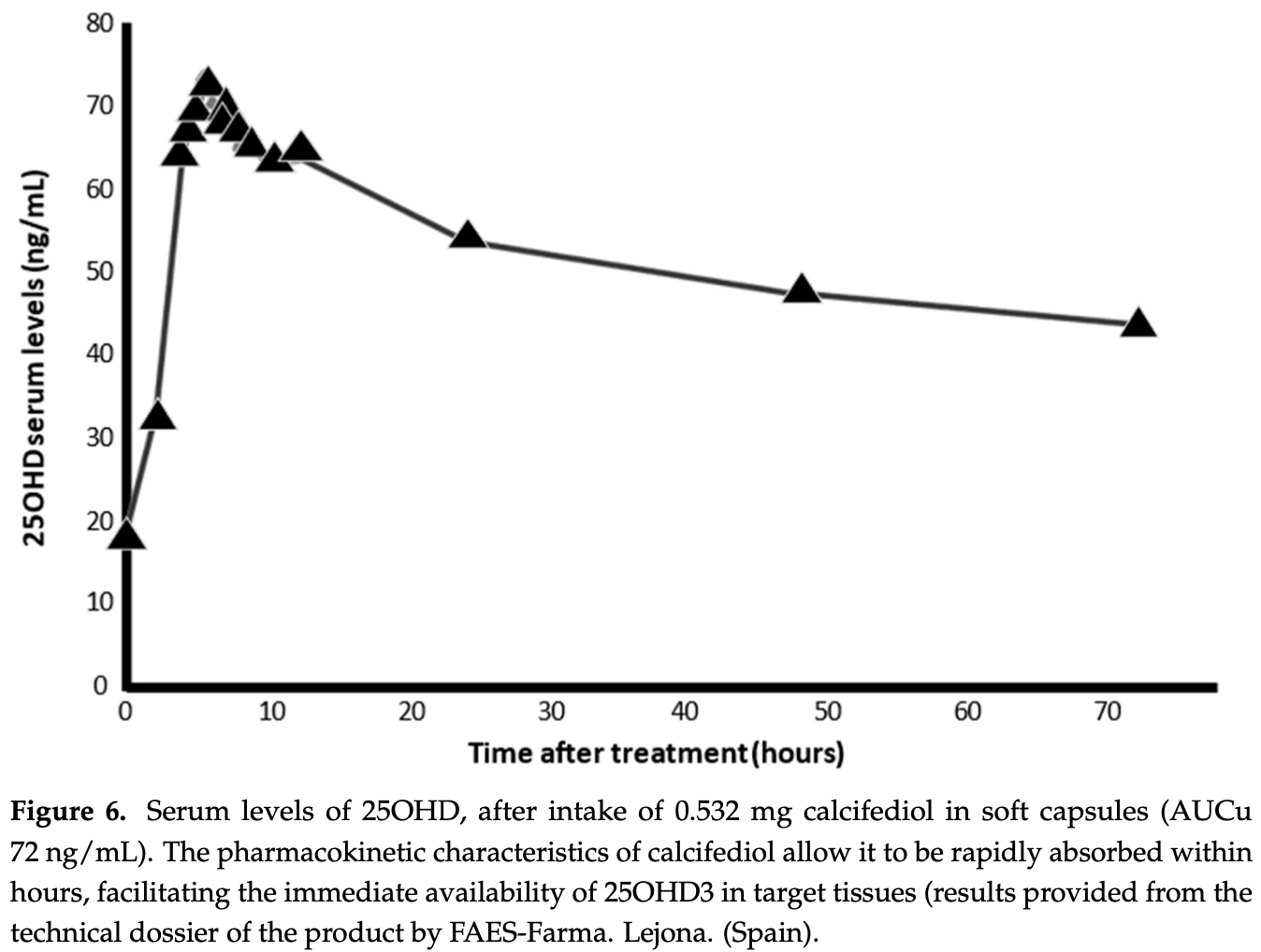
Review of the use of calcifediol for COVID-19. Authors note several advantages of calcifediol vs. cholecalciferol: calcifediol induces a more rapid increase in circulating 250HD; calcifediol is more potent than cholecalciferol; calcifediol has a higher rate of intestinal absorption; and calcifediol has a linear dose-response curve, independent of initial serum levels.
Authors note that the available data strongly and consistently suggest that treatment with calcifediol can reduce the severity of COVID-19; and that calcifediol is cost-effective and widely available, without significant adverse effects. Authors propose to use calcifediol for the rapid correction of vitamin D deficiency in all patients in the early stages of COVID-19.
1.
Jaurrieta-Largo et al., A Machine Learning Approach to Understanding the Genetic Role in COVID-19 Prognosis: The Influence of Gene Polymorphisms Related to Inflammation, Vitamin D, and ACE2, International Journal of Molecular Sciences, doi:10.3390/ijms26167975.
2.
Al-Khrasani et al., Do vitamins halt the COVID-19-evoked pro-inflammatory cytokines involved in the development of neuropathic pain?, Biomedicine & Pharmacotherapy, doi:10.1016/j.biopha.2025.118346.
3.
Kow et al., Vitamin D and COVID‐19: How much more evidence do we need?, Nutrition in Clinical Practice, doi:10.1002/ncp.11349.
4.
Bigman et al., A Comprehensive Scoping Review on Diet and Nutrition in Relation to Long COVID-19 Symptoms and Recovery, Nutrients, doi:10.3390/nu17111802.
5.
Hewison, M., COVID-19 and our understanding of vitamin D and immune function, The Journal of Steroid Biochemistry and Molecular Biology, doi:10.1016/j.jsbmb.2025.106710.
6.
Wimalawansa, S., Vitamin D Deficiency Meets Hill’s Criteria for Causation in SARS-CoV-2 Susceptibility, Complications, and Mortality: A Systematic Review, Nutrients, doi:10.3390/nu17030599.
7.
Sanduzzi Zamparelli et al., Immune-Boosting and Antiviral Effects of Antioxidants in COVID-19 Pneumonia: A Therapeutic Perspective, Life, doi:10.3390/life15010113.
8.
Fazli et al., Possible Link between Gut Microbiota, Diet, and COVID-19 Infection, Journal of Medical Bacteriology, 12:4, jmb.tums.ac.ir/index.php/jmb/article/view/525.
9.
Wojciulik et al., The impact of genetic polymorphism on course and severity of the SARS-CoV-2 infection and COVID-19 disease, Przeglad Epidemiologiczny, doi:10.32394/pe/194862.
10.
Wimalawansa (B), S., Unveiling the Interplay—Vitamin D and ACE-2 Molecular Interactions in Mitigating Complications and Deaths from SARS-CoV-2, Biology, doi:10.3390/biology13100831.
11.
Santa et al., Comparative analysis of COVID-19 responses in Japan and Africa: diet, phytochemicals, vitamin D, and gut microbiota in reducing mortality—A systematic review and meta-analysis, Frontiers in Nutrition, doi:10.3389/fnut.2024.1465324.
12.
Kaushal, A., Nutraceuticals and pharmacological to balance the transitional microbiome to extend immunity during COVID-19 and other viral infections, Journal of Translational Medicine, doi:10.1186/s12967-024-05587-9.
13.
Mu et al., Anti-inflammatory and Nutritional Interventions Against SARS-CoV-2: A Comprehensive Review, Journal of Agriculture and Food Research, doi:10.1016/j.jafr.2024.101422.
14.
Wimalawansa (C), S., Unlocking Insights: Navigating COVID-19 Challenges and Emulating Future Pandemic Resilience Strategies with Strengthening Natural Immunity, Heliyon, doi:10.1016/j.heliyon.2024.e34691.
15.
Imran et al., Therapeutic Role of Vitamin D in COVID-19 Patients, Clinical Nutrition Open Science, doi:10.1016/j.nutos.2024.07.004.
16.
Grant, W., Vitamin D and viral infections: Infectious diseases, autoimmune diseases, and cancers, Advances in Food and Nutrition Research, doi:10.1016/bs.afnr.2023.12.007.
17.
Polonowita et al., Molecular Quantum and Logic Process of Consciousness—Vitamin D Big-Data in COVID-19—A Case for Incorporating Machine Learning In Medicine, European Journal of Biomedical and Pharmaceutical sciences, doi:10.5281/zenodo.10435649.
18.
Gomaa et al., Pharmacological evaluation of vitamin D in COVID-19 and long COVID-19: recent studies confirm clinical validation and highlight metformin to improve VDR sensitivity and efficacy, Inflammopharmacology, doi:10.1007/s10787-023-01383-x.
19.
Gotelli et al., Understanding the immune-endocrine effects of vitamin D in SARS-CoV-2 infection: a role in protecting against neurodamage?, Neuroimmunomodulation, doi:10.1159/000533286.
20.
Cutolo et al., Involvement of the secosteroid vitamin D in autoimmune rheumatic diseases and COVID-19, Nature Reviews Rheumatology, doi:10.1038/s41584-023-00944-2.
21.
Schloss et al., Nutritional deficiencies that may predispose to long COVID, Inflammopharmacology, doi:10.1007/s10787-023-01183-3.
22.
Arora et al., Global Dietary and Herbal Supplement Use during COVID-19—A Scoping Review, Nutrients, doi:10.3390/nu15030771.
23.
Nicoll et al., COVID-19 Prevention: Vitamin D Is Still a Valid Remedy, Journal of Clinical Medicine, doi:10.3390/jcm11226818.
24.
Foshati et al., Antioxidants and clinical outcomes of patients with coronavirus disease 2019: A systematic review of observational and interventional studies, Food Science & Nutrition, doi:10.1002/fsn3.3034.
25.
Quesada-Gomez et al., Vitamin D Endocrine System and COVID-19: Treatment with Calcifediol, Nutrients, doi:10.3390/nu14132716.
26.
DiGuilio et al., Micronutrient Improvement of Epithelial Barrier Function in Various Disease States: A Case for Adjuvant Therapy, International Journal of Molecular Sciences, doi:10.3390/ijms23062995.
27.
Grant (B) et al., A Narrative Review of the Evidence for Variations in Serum 25-Hydroxyvitamin D Concentration Thresholds for Optimal Health, Nutrients, doi:10.3390/nu14030639.
28.
Shah Alam et al., The role of vitamin D in reducing SARS-CoV-2 infection: An update, International Immunopharmacology, doi:10.1016/j.intimp.2021.107686.
29.
Griffin et al., Perspective: Vitamin D supplementation prevents rickets and acute respiratory infections when given as daily maintenance but not as intermittent bolus: implications for COVID-19, Clinical Medicine, doi:10.7861/clinmed.2021-0035.
30.
Kohlmeier et al., When Mendelian randomisation fails, BMJ Nutrition, Prevention & Health, doi:10.1136/bmjnph-2021-000265.
31.
Brenner, H., Vitamin D Supplementation to Prevent COVID-19 Infections and Deaths—Accumulating Evidence from Epidemiological and Intervention Studies Calls for Immediate Action, Nutrients, doi:10.3390/nu13020411.
32.
Mercola et al., Evidence Regarding Vitamin D and Risk of COVID-19 and Its Severity, Nutrients 2020, 12:11, 3361, doi:10.3390/nu12113361.
33.
Basha et al., Is the shielding effect of cholecalciferol in SARS CoV-2 infection dependable? An evidence based unraveling, Clinical Epidemiology and Global Health, doi:10.1016/j.cegh.2020.10.005.
34.
Xu et al., The importance of vitamin d metabolism as a potential prophylactic, immunoregulatory and neuroprotective treatment for COVID-19, Journal of Translational Medicine, doi:10.1186/s12967-020-02488-5.
35.
Alexander et al., Early Nutritional Interventions with Zinc, Selenium and Vitamin D for Raising Anti-Viral Resistance Against Progressive COVID-19, Nutrients, doi:10.3390/nu12082358.
36.
Andrade et al., Vitamin A and D deficiencies in the prognosis of respiratory tract infections: A systematic review with perspectives for COVID-19 and a critical analysis on supplementation, SciELO preprints, doi:10.1590/SciELOPreprints.839.
37.
Grant (C) et al., Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths, Nutrients, 12:4, 988, doi:10.3390/nu12040988.
38.
McCullough et al., Daily oral dosing of vitamin D3 using 5000 TO 50,000 international units a day in long-term hospitalized patients: Insights from a seven year experience, The Journal of Steroid Biochemistry and Molecular Biology, doi:10.1016/j.jsbmb.2018.12.010.
39.
EFSA, Scientific Opinion on the substantiation of health claims related to vitamin D and normal function of the immune system and inflammatory response (ID 154, 159), maintenance of normal muscle function (ID 155) and maintenance of normal cardiovascular function (ID 159) pursuant to Article 13(1) of Regulation (E, EFSA Journal, doi:10.2903/j.efsa.2010.1468.
40.
EFSA (B), Scientific Opinion on the substantiation of a health claim related to vitamin D and contribution to the normal function of the immune system pursuant to Article 14 of Regulation (EC) No 1924/2006, EFSA Journal, doi:10.2903/j.efsa.2015.4096.
Quesada-Gomez et al., 29 Jun 2022, peer-reviewed, 7 authors.
Contact: jmquesada@uco.es (corresponding author), md1lomij@uco.es, bb1cadia@uco.es, xnogues@psmar.cat, marenca@gmail.com, joseluismansur@yahoo.com.ar, roger.bouillon@kuleuven.be.
Vitamin D Endocrine System and COVID-19: Treatment with Calcifediol
Nutrients, doi:10.3390/nu14132716
The COVID-19 pandemic is the greatest challenge facing modern medicine and public health systems. The viral evolution of SARS-CoV-2, with the emergence of new variants with in-creased infectious potential, is a cause for concern. In addition, vaccination coverage remains in-sufficient worldwide. Therefore, there is a need to develop new therapeutic options, and/or to optimize the repositioning of drugs approved for other indications for COVID-19. This may include the use of calcifediol, the prohormone of the vitamin D endocrine system (VDES) as it may have potential useful effects for the treatment of COVID-19. We review the aspects associating COVID-19 with VDES and the potential use of calcifediol in COVID-19. VDES/VDR stimulation may enhance innate antiviral effector mechanisms, facilitating the induction of antimicrobial peptides/autophagy, with a critical modulatory role in the subsequent host reactive hyperinflammatory phase during COVID-19: By decreasing the cytokine/chemokine storm, regulating the renin-angiotensin-bradykinin system (RAAS), modulating neutrophil activity and maintaining the integrity of the pulmonary epithelial barrier, stimulating epithelial repair, and directly and indirectly decreasing the increased coagulability and prothrombotic tendency associated with severe COVID-19 and its complications. Available evidence suggests that VDES/VDR stimulation, while maintaining optimal serum 25OHD status, in patients with SARS-CoV-2 infection may significantly reduce the risk of acute respiratory distress syndrome (ARDS) and severe COVID-19, with possible beneficial effects on the need for mechanical ventilation and/or intensive care unit (ICU) admission, as well as deaths in the course of the disease. The pharmacokinetic and functional characteristics of calcifediol give it superiority in rapidly optimizing 25OHD levels in COVID-19. A pilot study and several observational intervention studies using high doses of calcifediol (0.532 mg on day 1 and 0.266 mg on days 3, 7, 14, 21, and 28) dramatically decreased the need for ICU admission and the mortality rate. We, therefore, propose to use calcifediol at the doses described for the rapid correction of 25OHD deficiency in all patients in the early stages of COVID-19, in association, if necessary, with the new oral antiviral agents.
Funding: From the Fundación para la investigación biomédica de Córdoba (FIBICO) and FAES Farma, Bilbao, Spain.
Institutional Review Board Statement: Not applicable. Informed Consent Statement: Not applicable.
References
Ahmed, A Network-Based Analysis Reveals the Mechanism Underlying Vitamin D in Suppressing Cytokine Storm and Virus in SARS-CoV-2 Infection, Front. Immunol, doi:10.3389/fimmu.2020.590459
Aihara, Azuma, Akaike, Ikeda, Yamashita et al., Disruption of nuclear vitamin D receptor gene causes enhanced thrombogenicity in mice, J. Biol. Chem
Alcala-Diaz, Limia-Perez, Gomez-Huelgas, Martin-Escalante, Cortes-Rodriguez et al., Calcifediol treatment and hospital mortality due to COVID-19: A cohort study, Nutrients, doi:10.3390/nu13061760
Andújar-Espinosa, Salinero-González, Illán-Gómez, Castilla-Martínez, Hu-Yang et al., Effect of vitamin D supplementation on asthma control in patients with vitamin D deficiency: The ACVID randomised clinical trial, Thorax, doi:10.1136/thoraxjnl-2019-213936
Anonim, COVID Live-Coronavirus Statistics-Worldometer
Bassatne, Basbous, Chakhtoura, El Zein, Rahme et al., The link between COVID-19 and VItamin D (VIVID): A systematic review and meta-analysis, Metabolism, doi:10.1016/j.metabol.2021.154753
Bikle, Vitamin, Production, Metabolism and Mechanisms of Action
Bilezikian, Bikle, Hewison, Lazaretti-Castro, Formenti et al., MECHANISMS in ENDOCRINOLOGY Vitamin D and COVID-19, Eur. J. Endocrinol
Bischoff-Ferrari, Dawson-Hughes, Stöcklin, Sidelnikov, Willett et al., Oral supplementation with 25(OH)D3 versus vitamin D3: Effects on 25(OH)D levels, lower extremity function, blood pressure, and markers of innate immunity, J. Bone Miner. Res, doi:10.1002/jbmr.551
Bishop, Ismailova, Dimeloe, Hewison, White, Vitamin D and Immune Regulation: Antibacterial, Antiviral, Anti-Inflammatory, JBMR Plus, doi:10.1002/jbm4.10405
Blanco-Melo, Nilsson-Payant, Liu, Uhl, Hoagland et al., Imbalanced Host Response to SARS-CoV-2 Drives Development of COVID-19, Cell, doi:10.1016/j.cell.2020.04.026
Boban, Novel coronavirus disease (COVID-19) update on epidemiology, pathogenicity, clinical course and treatments, Int. J. Clin. Pract, doi:10.1111/ijcp.13868
Bouillon, Antonio, Olarte, Calcifediol (25OH Vitamin D3) Deficiency: A Risk Factor from Early to Old Age, Nutrients, doi:10.3390/nu14061168
Bouillon, Bikle, Vitamin D Metabolism Revised: Fall of Dogmas, J. Bone Miner. Res, doi:10.1002/jbmr.3884
Bouillon, Marcocci, Carmeliet, Bikle, White et al., Skeletal and Extraskeletal Actions of Vitamin D: Current Evidence and Outstanding Questions, Endocr. Rev, doi:10.1210/er.2018-00126
Bouillon, Quesada-Gomez, Vitamin D Endocrine System and COVID-19, JBMR Plus, doi:10.1002/jbm4.10576
Bouillon, Vitamin D and cardiovascular disorders, Osteoporos. Int, doi:10.1007/s00198-019-05098-0
Campbell, Spector, Vitamin D inhibits human immunodeficiency virus type 1 and Mycobacterium tuberculosis infection in macrophages through the induction of autophagy, PLoS Pathog, doi:10.1371/journal.ppat.1002689
Cantorna, Snyder, Lin, Yang, Vitamin D and 1,25(OH)2D regulation of T cells, Nutrients
Castillo, Entrenas Costa, Vaquero Barrios, Alcalá Díaz, López Miranda et al., Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study, J. Steroid Biochem. Mol. Biol, doi:10.1016/j.jsbmb.2020.105751
Cele, Jackson, Khoury, Khan, Moyo-Gwete et al., Omicron extensively but incompletely escapes Pfizer BNT162b2 neutralization, Nature, doi:10.1038/s41586-021-04387-1
Cesareo, Falchetti, Attanasio, Tabacco, Naciu et al., Is it time to consider the use of calcifediol?, Nutrients, doi:10.3390/nu11051016
Chang, Nie, Ge, Du, Liu et al., Vitamin D suppresses bleomycin-induced pulmonary fibrosis by targeting the local renin-angiotensin system in the lung, Sci. Rep, doi:10.1038/s41598-021-96152-7
Charoenngam, Holick, Immunologic effects of vitamin d on human health and disease, Nutrients
Charoenngam, Kalajian, Shirvani, Yoon, Desai et al., A pilotrandomized, double-blind crossover trial to evaluate the pharmacokinetics of orally administered 25-hydroxyvitamin D3 and vitamin D3 in healthy adults with differing BMI and in adults with intestinal malabsorption, Am. J. Clin. Nutr, doi:10.1093/ajcn/nqab123
Chen, Lu, Zhang, Sun, Vitamin D Receptor Deletion Leads to the Destruction of Tight and Adherens Junctions in Lungs, Tissue Barriers, doi:10.1080/21688370.2018.1540904
Chen, Yang, Nissen, Chen, Wang et al., Dysregulated renin-AngioteNsin system contributes to acute lung injury caused by hind-limb ischemia-reperfusion in mice, Shock, doi:10.1097/SHK.0b013e3182a6953e
Chiodini, Gatti, Soranna, Merlotti, Mingiano et al., Vitamin D Status and SARS-CoV-2 Infection and COVID-19 Clinical Outcomes, Front. Public Health
Colotta, Jansson, Bonelli, Modulation of inflammatory and immune responses by vitamin D, J. Autoimmun, doi:10.1016/j.jaut.2017.07.007
Damascena, Azevedo, De Oliveira, Da Mota Santana, Pereira, Addendum to vitamin D deficiency aggravates COVID-19: Systematic review and meta-analysis, Crit. Rev. Food Sci. Nutr, doi:10.1080/10408398.2021.1951652
Deluca, History of the discovery of vitamin D and its active metabolites, Bonekey Rep, doi:10.1038/bonekey.2013.213
Dimitrov, Barbier, Ismailova, Wang, Dmowski et al., Vitamin D-regulated Gene Expression Profiles: Species-specificity and Cell-specific Effects on Metabolism and Immunity, Endocrinology, doi:10.1210/endocr/bqaa218
Dissanayake, De Silva, Sumanatilleke, De Silva, Gamage et al., Prognostic and Therapeutic Role of Vitamin D in COVID-19: Systematic Review and Meta-analysis, J. Clin. Endocrinol. Metab, doi:10.1210/clinem/dgab892
Duchow, Sibilska-Kaminski, Plum, Deluca, Vitamin D esters are the major form of vitamin D produced by UV irradiation in mice, Photochem. Photobiol. Sci, doi:10.1007/s43630-022-00230-2
Fernández, Sebti, Wei, Zou, Shi et al., Disruption of the beclin 1-BCL2 autophagy regulatory complex promotes longevity in mice, Nature, doi:10.1038/s41586-018-0162-7
Gayan-Ramirez, Janssens, Vitamin D Actions: The Lung Is a Major Target for Vitamin D, FGF23, and Klotho, JBMR Plus, doi:10.1002/jbm4.10569
George, Amjesh, Paul, Santhoshkumar, Pillai et al., Evidence of a dysregulated vitamin D endocrine system in SARS-CoV-2 infected patient's lung cells, Sci. Rep, doi:10.1038/s41598-021-87703-z
Ginde, Mansbach, Camargo, Association between Serum 25-hydroxyvitamin D level and upper respiratory tract infection in the Third National Health and Nutrition Examination Survey, Arch. Intern. Med, doi:10.1001/archinternmed.2008.560
Giustina, Adler, Binkley, Bollerslev, Bouillon et al., Consensus statement from 2nd International Conference on Controversies in Vitamin D, Rev. Endocr. Metab. Disord, doi:10.1007/s11154-019-09532-w
Grant, Lahore, Mcdonnell, Baggerly, French et al., Evidence that vitamin d supplementation could reduce risk of influenza and COVID-19 infections and deaths, Nutrients, doi:10.3390/nu12040988
Greiller, Martineau, Modulation of the immune response to respiratory viruses by vitamin D, Nutrients, doi:10.3390/nu7064240
Guan, Ni, Hu, Liang, Ou et al., Clinical Characteristics of Coronavirus Disease 2019 in China, N. Engl. J. Med, doi:10.1056/NEJMoa2002032
Hartmann, Riedel, Jör, Loddenkemper, Steinmeyer et al., Vitamin D receptor activation improves allergen-triggered eczema in mice, J. Invest Dermatol, doi:10.1038/jid.2011.296
Hilger, Friedel, Herr, Rausch, Roos et al., A systematic review of vitamin D status in populations worldwide, Br. J. Nutr, doi:10.1017/S0007114513001840
Holick, Binkley, Bischoff-Ferrari, Gordon, Hanley et al., Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline, J. Clin. Endocrinol. Metab, doi:10.1210/jc.2011-0385
Holick, The CO-VID D-Lemma: A Call for Action, Nutrients, doi:10.3390/nu14050963
Holick, Vitamin, Deficiency, None, N. Engl. J. Med, doi:10.1056/NEJMra070553
Jain, Micinski, Vitamin D upregulates glutamate cysteine ligase and glutathione reductase, and GSH formation, and decreases ROS and MCP-1 and IL-8 secretion in high-glucose exposed U937 monocytes, Biochem. Biophys. Res. Commun, doi:10.1016/j.bbrc.2013.06.004
Jiang, Yang, Xue, Li, Zhang, 1α, 25-dihydroxyvitamin D3 attenuates TGF-β-induced pro-fibrotic effects in human lung epithelial cells through inhibition of epithelial-mesenchymal transition, Nutrients, doi:10.3390/nu9090980
Jolliffe, Camargo, Sluyter, Aglipay, Aloia et al., Vitamin D supplementation to prevent acute respiratory infections: A systematic review and meta-analysis of aggregate data from randomised controlled trials, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(21)00051-6
Jolliffe, Stefanidis, Wang, Kermani, Dimitrov et al., Vitamin d metabolism is dysregulated in asthma and chronic obstructive pulmonary disease, Am. J. Respir. Crit. Care Med, doi:10.1164/rccm.201909-1867OC
Jones, Kaufmann, Diagnostic Aspects of Vitamin D: Clinical Utility of Vitamin D Metabolite Profiling, JBMR Plus, doi:10.1002/jbm4.10581
Kaya, Pamukcu, Yakar, The role of vitamin D deficiency on COVID-19: A systematic review and meta-Analysis of observational studies, Epidemiol. Health, doi:10.4178/epih.e2021074
Kazemi, Mohammadi, Aghababaee, Golzarand, Clark et al., Association of Vitamin D Status with SARS-CoV-2 Infection or COVID-19 Severity: A Systematic Review and Meta-analysis, Adv. Nutr, doi:10.1093/advances/nmab012
Khademvatani, Seyyed-Mohammadzad, Akbari, Rezaei, Eskandari et al., The relationship between vitamin D status and idiopathic lower-extremity deep vein thrombosis, Int. J. Gen. Med, doi:10.2147/IJGM.S64812
Kong, Zhang, Musch, Ning, Sun et al., Novel role of the vitamin D receptor in maintaining the integrity of the intestinal mucosal barrier, Am. J. Physiol. -Gastrointest. Liver Physiol, doi:10.1152/ajpgi.00398.2007
Li, Chang, Chen, Wang, Yau et al., Genomic Feature Analysis of Betacoronavirus Provides Insights Into SARS and COVID-19 Pandemics, Front. Microbiol, doi:10.3389/fmicb.2021.614494
Lips, Worldwide status of vitamin D nutrition, J. Steroid Biochem. Mol. Biol, doi:10.1016/j.jsbmb.2010.02.021
Liu, Sun, Wang, Zhang, Zhao et al., Low vitamin D status is associated with coronavirus disease 2019 outcomes: A systematic review and meta-analysis, Int. J. Infect. Dis, doi:10.1016/j.ijid.2020.12.077
Loucera, Esteban-Medina, Rian, Falco, Dopazo et al., Drug repurposing for COVID-19 using machine learning and mechanistic models of signal transduction circuits related to SARS-CoV-2 infection, Signal Transduct. Target. Ther, doi:10.1038/s41392-020-00417-y
Loucera, Peña-Chilet, Esteban-Medina, Muñoyerro-Muñiz, Villegas et al., Real world evidence of calcifediol or vitamin D prescription and mortality rate of COVID-19 in a retrospective cohort of hospitalized Andalusian patients, Sci. Rep, doi:10.1038/s41598-021-02701-5
Maestro, Molnár, Carlberg, Vitamin D and its synthetic analogs, J. Med. Chem, doi:10.1021/acs.jmedchem.9b00208
Maghbooli, Sahraian, Jamalimoghadamsiahkali, Asadi, Zarei et al., Treatment With 25-Hydroxyvitamin D3 (Calcifediol) Is Associated With a Reduction in the Blood Neutrophil-to-Lymphocyte Ratio Marker of Disease Severity in Hospitalized Patients With COVID-19: A Pilot Multicenter, Randomized, Placebo-Controlled, Double-Bli, Endocr. Pract, doi:10.1016/j.eprac.2021.09.016
Mansur, Tajer, Mariani, Inserra, Ferder et al., Vitamin D high doses supplementation could represent a promising alternative to prevent or treat COVID-19 infection, Clin. E Investig. En Arterioscler, doi:10.1016/j.arteri.2020.05.003
Martineau, Jolliffe, Hooper, Greenberg, Aloia et al., Vitamin D supplementation to prevent acute respiratory tract infections: Systematic review and meta-analysis of individual participant data, BMJ, doi:10.1136/bmj.i6583
Martinez-Moreno, Herencia, De Oca, Muñoz-Castañeda, Rodríguez-Ortiz et al., Vitamin D modulates tissue factor and protease-activated receptor 2 expression in vascular smooth muscle cells, FASEB J, doi:10.1096/fj.15-272872
Martucci, Mcnally, Parekh, Zajic, Tuzzolino et al., Trying to identify who may benefit most from future vitamin D intervention trials: A post hoc analysis from the VITDAL-ICU study excluding the early deaths, Crit. Care, doi:10.1186/s13054-019-2472-z
Mohammad, Mishra, Ashraf, Emerging role of vitamin d and its associated molecules in pathways related to pathogenesis of thrombosis, Biomolecules, doi:10.3390/biom9110649
Molin, Wiedemann, Demers, Kaufmann, Do Cao et al., Vitamin D-Dependent Rickets Type 1B (25-Hydroxylase Deficiency): A Rare Condition or a Misdiagnosed Condition?, J. Bone Miner. Res, doi:10.1002/jbmr.3181
Nalbandian, Sehgal, Gupta, Madhavan, Mcgroder et al., Post-acute COVID-19 syndrome, Nat. Med, doi:10.1038/s41591-021-01283-z
Nogues, Ovejero, Pineda-Moncusí, Bouillon, Arenas et al., Calcifediol treatment and COVID-19-related outcomes, J. Clin. Endocrinol. Metab, doi:10.1210/clinem/dgab405
Norman, From vitamin D to hormone D: Fundamentals of the vitamin D endocrine system essential for good health, Am. J. Clin. Nutr, doi:10.1093/ajcn/88.2.491S
Okoye, Calsolaro, Niccolai, Calabrese, Franchi et al., Open-Label Study to Assess Efficacy of Weekly Assumption of Cholecalciferol versus Calcifediol in Older Patients with Hypovitaminosis D, Geriatrics, doi:10.3390/geriatrics7010013
Oristrell, Oliva, Subirana, Casado, Domínguez et al., Association of calcitriol supplementation with reduced COVID19 mortality in patients with chronic kidney disease: A populationbased study, Biomedicines, doi:10.3390/biomedicines9050509
Oscanoa, Amado, Vidal, Laird, Ghashut et al., The relationship between the severity and mortality of SARS-CoV-2 infection and 25-hydroxyvitamin D concentration-A metaanalysis, Adv. Respir. Med, doi:10.5603/ARM.a2021.0037
Osuchowski, Winkler, Skirecki, Cajander, Shankar-Hari et al., The COVID-19 puzzle: Deciphering pathophysiology and phenotypes of a new disease entity, Lancet Respir. Med, doi:10.1016/S2213-2600(21)00218-6
Pereira, Dantas Damascena, Galvão Azevedo, De Almeida Oliveira, Da Mota Santana, Vitamin D deficiency aggravates COVID-19: Systematic review and meta-analysis, Crit. Rev. Food Sci. Nutr, doi:10.1080/10408398.2020.1841090
Pilz, Verheyen, Grübler, Tomaschitz, März, Vitamin D and cardiovascular disease prevention, Nat. Rev. Cardiol, doi:10.1038/nrcardio.2016.73
Pérez-Castrillón, Dueñas-Laita, Brandi, Jódar, Del Pino-Montes et al., Calcifediol is superior to cholecalciferol in improving vitamin D status in postmenopausal women: A randomized trial, J. Bone Miner. Res, doi:10.1002/jbmr.4387
Quesada-Gomez, Bouillon, Is calcifediol better than cholecalciferol for vitamin D supplementation?, Osteoporos. Int, doi:10.1007/s00198-018-4520-y
Quesada-Gomez, Entrenas-Castillo, Bouillon, Vitamin D receptor stimulation to reduce acute respiratory distress syndrome (ARDS) in patients with coronavirus SARS-CoV-2 infections: Revised Ms SBMB 2020_166, J. Steroid Biochem. Mol. Biol, doi:10.1016/j.jsbmb.2020.105719
Roth, Jones, Prosser, Robinson, Vohra, Vitamin D receptor polymorphisms and the risk of acute lower respiratory tract infection in early childhood, J. Infect. Dis, doi:10.1086/527488
Sariol, Perlman, Lessons for COVID-19 Immunity from Other Coronavirus Infections, Immunity, doi:10.1016/j.immuni.2020.07.005
Sengupta, Majumder, Majumder, Role of vitamin D in treating COVID-19-associated coagulopathy: Problems and perspectives, Mol. Cell. Biochem, doi:10.1007/s11010-021-04093-6
Solanki, Singh, Kashyap, Sansi, Ali, Promising role of defensins peptides as therapeutics to combat against viral infection, Microb. Pathog, doi:10.1016/j.micpath.2021.104930
Thorne, Bouhaddou, Reuschl, Zuliani-Alvarez, Polacco et al., Evolution of enhanced innate immune evasion by SARS-CoV-2, Nature, doi:10.1038/s41586-021-04352-y
Tzilas, Bouros, Barbayianni, Karampitsakos, Kourtidou et al., Vitamin D prevents experimental lung fibrosis and predicts survival in patients with idiopathic pulmonary fibrosis, Pulm. Pharmacol. Ther, doi:10.1016/j.pupt.2019.01.003
Vanherwegen, Gysemans, Mathieu, Vitamin D endocrinology on the cross-road between immunity and metabolism, Mol. Cell. Endocrinol, doi:10.1016/j.mce.2017.04.018
Vieth, Vitamin D supplementation: Cholecalciferol, calcifediol, and calcitriol, Eur. J. Clin. Nutr, doi:10.1038/s41430-020-0697-1
Visser, Dofferhoff, Van Den Ouweland, Van Daal, Kramers et al., Effects of Vitamin D and K on Interleukin-6 in COVID-19, Front. Nutr, doi:10.3389/fnut.2021.761191
Vitiello, Ferrara, Auti, Di Domenico, Boccellino, Advances in the Omicron variant development, J. Intern. Med, doi:10.1111/joim.13478
Wagner, Saad-Roy, Morris, Baker, Mina et al., Vaccine nationalism and the dynamics and control of SARS-CoV-2, Science, doi:10.1126/science.abj7364
Wang, Joshi, Leopold, Jackson, Christensen et al., Association of Vitamin D Deficiency with COVID-19 Infection Severity: Systematic Review and Meta-analysis, Clin. Endocrinol, doi:10.1111/cen.14540
Wen, Chen, Tang, Wang, Zhou et al., Efficacy and safety of three new oral antiviral treatment (molnupiravir, fluvoxamine and Paxlovid) for COVID-19: A meta-analysis, Ann. Med, doi:10.1080/07853890.2022.2034936
Wu, He, Low Vitamin D Levels Are Associated With the Development of Deep Venous Thromboembolic Events in Patients With Ischemic Stroke, Clin. Appl. Thromb, doi:10.1177/1076029618786574
Wu, Peng, Huang, Ding, Wang et al., Genome Composition and Divergence of the Novel Coronavirus (2019-nCoV) Originating in China, Cell. Host Microbe, doi:10.1016/j.chom.2020.02.001
Xu, Yang, Chen, Luo, Zhang et al., Vitamin D alleviates lipopolysaccharide-induced acute lung injury via regulation of the renin-angiotensin system, Mol. Med. Rep, doi:10.3892/mmr.2017.7546
Yang, Xie, Tu, Fu, Xu et al., The signal pathways and treatment of cytokine storm in COVID-19, Signal Transduct. Target. Ther, doi:10.1038/s41392-021-00679-0
Yoshimoto, The Proteins of Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2 or n-COV19), the Cause of COVID-19, Protein J, doi:10.1007/s10930-020-09901-4
Yuk, Shin, Lee, Yang, Jin et al., Vitamin D3 Induces Autophagy in Human Monocytes/Macrophages via Cathelicidin, Cell. Host Microbe, doi:10.1016/j.chom.2009.08.004
Zdrenghea, Makrinioti, Bagacean, Bush, Johnston et al., Vitamin D modulation of innate immune responses to respiratory viral infections, Rev. Med. Virol, doi:10.1002/rmv.1909
Zhang, Ai, Chen, Liu, Gong et al., Associations of immunological features with COVID-19 severity: A systematic review and meta-analysis, BMC Infect. Dis, doi:10.1186/s12879-021-06457-1
Zhou, Lu, Cao, Xu, Goltzman et al., Calcium-independent and 1,25(OH)2D3-dependent regulation of the renin-angiotensin system in 1α-hydroxylase knockout mice, Kidney Int, doi:10.1038/ki.2008.101
Zhou, Yu, Du, Fan, Liu et al., Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study, Lancet
DOI record:
{
"DOI": "10.3390/nu14132716",
"ISSN": [
"2072-6643"
],
"URL": "http://dx.doi.org/10.3390/nu14132716",
"abstract": "<jats:p>The COVID-19 pandemic is the greatest challenge facing modern medicine and public health systems. The viral evolution of SARS-CoV-2, with the emergence of new variants with in-creased infectious potential, is a cause for concern. In addition, vaccination coverage remains in-sufficient worldwide. Therefore, there is a need to develop new therapeutic options, and/or to optimize the repositioning of drugs approved for other indications for COVID-19. This may include the use of calcifediol, the prohormone of the vitamin D endocrine system (VDES) as it may have potential useful effects for the treatment of COVID-19. We review the aspects associating COVID-19 with VDES and the potential use of calcifediol in COVID-19. VDES/VDR stimulation may enhance innate antiviral effector mechanisms, facilitating the induction of antimicrobial peptides/autophagy, with a critical modulatory role in the subsequent host reactive hyperinflammatory phase during COVID-19: By decreasing the cytokine/chemokine storm, regulating the renin–angiotensin–bradykinin system (RAAS), modulating neutrophil activity and maintaining the integrity of the pulmonary epithelial barrier, stimulating epithelial repair, and directly and indirectly decreasing the increased coagulability and prothrombotic tendency associated with severe COVID-19 and its complications. Available evidence suggests that VDES/VDR stimulation, while maintaining optimal serum 25OHD status, in patients with SARS-CoV-2 infection may significantly reduce the risk of acute respiratory distress syndrome (ARDS) and severe COVID-19, with possible beneficial effects on the need for mechanical ventilation and/or intensive care unit (ICU) admission, as well as deaths in the course of the disease. The pharmacokinetic and functional characteristics of calcifediol give it superiority in rapidly optimizing 25OHD levels in COVID-19. A pilot study and several observational intervention studies using high doses of calcifediol (0.532 mg on day 1 and 0.266 mg on days 3, 7, 14, 21, and 28) dramatically decreased the need for ICU admission and the mortality rate. We, therefore, propose to use calcifediol at the doses described for the rapid correction of 25OHD deficiency in all patients in the early stages of COVID-19, in association, if necessary, with the new oral antiviral agents.</jats:p>",
"alternative-id": [
"nu14132716"
],
"author": [
{
"affiliation": [],
"family": "Quesada-Gomez",
"given": "Jose Manuel",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-8844-0718",
"affiliation": [],
"authenticated-orcid": false,
"family": "Lopez-Miranda",
"given": "José",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Entrenas-Castillo",
"given": "Marta",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8520-8278",
"affiliation": [],
"authenticated-orcid": false,
"family": "Casado-Díaz",
"given": "Antonio",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5537-1859",
"affiliation": [],
"authenticated-orcid": false,
"family": "Nogues y Solans",
"given": "Xavier",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8383-9543",
"affiliation": [],
"authenticated-orcid": false,
"family": "Mansur",
"given": "José Luis",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bouillon",
"given": "Roger",
"sequence": "additional"
}
],
"container-title": "Nutrients",
"container-title-short": "Nutrients",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
6,
30
]
],
"date-time": "2022-06-30T02:43:28Z",
"timestamp": 1656557008000
},
"deposited": {
"date-parts": [
[
2022,
7,
5
]
],
"date-time": "2022-07-05T01:27:04Z",
"timestamp": 1656984424000
},
"indexed": {
"date-parts": [
[
2022,
7,
5
]
],
"date-time": "2022-07-05T01:42:10Z",
"timestamp": 1656985330387
},
"is-referenced-by-count": 0,
"issue": "13",
"issued": {
"date-parts": [
[
2022,
6,
29
]
]
},
"journal-issue": {
"issue": "13",
"published-online": {
"date-parts": [
[
2022,
7
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
6,
29
]
],
"date-time": "2022-06-29T00:00:00Z",
"timestamp": 1656460800000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2072-6643/14/13/2716/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "2716",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2022,
6,
29
]
]
},
"published-online": {
"date-parts": [
[
2022,
6,
29
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1111/ijcp.13868",
"doi-asserted-by": "publisher",
"key": "ref1"
},
{
"key": "ref2",
"unstructured": "COVID Live—Coronavirus Statistics—Worldometer\nhttps://www.worldometers.info/coronavirus/"
},
{
"key": "ref3",
"unstructured": "COVID-19 Map—Johns Hopkins Coronavirus Resource Center\nhttps://coronavirus.jhu.edu/map.html"
},
{
"DOI": "10.1038/s41586-021-04352-y",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.1038/s41586-021-04387-1",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.1126/science.abj7364",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.1038/s41392-020-00417-y",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.1002/jbm4.10576",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"DOI": "10.3390/nu12040988",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"DOI": "10.3389/fmicb.2021.614494",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.1016/j.chom.2020.02.001",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.1007/s10930-020-09901-4",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.1016/j.immuni.2020.07.005",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"article-title": "Coronavirus Disease 2019 (COVID-19) Treatment Guidelines",
"author": "NIH Clinical Spectrum",
"key": "ref14"
},
{
"DOI": "10.1056/NEJMoa2002032",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.1038/s41591-021-01283-z",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.1016/j.cell.2020.04.026",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.1021/acs.jmedchem.9b00208",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.1038/s41430-020-0697-1",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.1038/bonekey.2013.213",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"DOI": "10.1093/ajcn/88.2.491S",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"DOI": "10.1056/NEJMra070553",
"doi-asserted-by": "publisher",
"key": "ref23"
},
{
"article-title": "Vitamin D: Production, Metabolism and Mechanisms of Action",
"key": "ref24",
"year": "2000"
},
{
"DOI": "10.1002/jbm4.10581",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"DOI": "10.17226/13050",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.1210/jc.2011-0385",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.1210/er.2018-00126",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.1016/j.mce.2017.04.018",
"doi-asserted-by": "publisher",
"key": "ref29"
},
{
"DOI": "10.1210/endocr/bqaa218",
"doi-asserted-by": "publisher",
"key": "ref30"
},
{
"DOI": "10.1002/jbm4.10405",
"doi-asserted-by": "publisher",
"key": "ref31"
},
{
"DOI": "10.1002/jbm4.10569",
"doi-asserted-by": "publisher",
"key": "ref32"
},
{
"DOI": "10.1038/nrcardio.2016.73",
"doi-asserted-by": "publisher",
"key": "ref33"
},
{
"DOI": "10.1007/s00198-019-05098-0",
"doi-asserted-by": "publisher",
"key": "ref34"
},
{
"DOI": "10.1007/s11010-021-04093-6",
"doi-asserted-by": "publisher",
"key": "ref35"
},
{
"DOI": "10.1016/S2213-2600(21)00218-6",
"doi-asserted-by": "publisher",
"key": "ref36"
},
{
"DOI": "10.1017/S0007114513001840",
"doi-asserted-by": "publisher",
"key": "ref37"
},
{
"DOI": "10.1016/j.jsbmb.2010.02.021",
"doi-asserted-by": "publisher",
"key": "ref38"
},
{
"DOI": "10.3390/nu14061168",
"doi-asserted-by": "publisher",
"key": "ref39"
},
{
"DOI": "10.1007/s11154-019-09532-w",
"doi-asserted-by": "publisher",
"key": "ref40"
},
{
"DOI": "10.2147/IJGM.S64812",
"doi-asserted-by": "publisher",
"key": "ref41"
},
{
"DOI": "10.1038/s41598-021-87703-z",
"doi-asserted-by": "publisher",
"key": "ref42"
},
{
"DOI": "10.3389/fimmu.2020.590459",
"doi-asserted-by": "publisher",
"key": "ref43"
},
{
"DOI": "10.1001/archinternmed.2008.560",
"doi-asserted-by": "publisher",
"key": "ref44"
},
{
"DOI": "10.3390/nu7064240",
"doi-asserted-by": "publisher",
"key": "ref45"
},
{
"DOI": "10.1086/527488",
"doi-asserted-by": "publisher",
"key": "ref46"
},
{
"DOI": "10.1136/bmj.i6583",
"doi-asserted-by": "publisher",
"key": "ref47"
},
{
"DOI": "10.1016/S2213-8587(21)00051-6",
"doi-asserted-by": "publisher",
"key": "ref48"
},
{
"DOI": "10.3390/nu12072097",
"doi-asserted-by": "publisher",
"key": "ref49"
},
{
"DOI": "10.1002/rmv.1909",
"doi-asserted-by": "publisher",
"key": "ref50"
},
{
"DOI": "10.1530/EJE-20-0665",
"doi-asserted-by": "publisher",
"key": "ref51"
},
{
"DOI": "10.1016/j.arteri.2020.05.003",
"doi-asserted-by": "publisher",
"key": "ref52"
},
{
"DOI": "10.1016/j.jsbmb.2020.105719",
"doi-asserted-by": "publisher",
"key": "ref53"
},
{
"DOI": "10.1016/j.micpath.2021.104930",
"doi-asserted-by": "publisher",
"key": "ref54"
},
{
"DOI": "10.1016/j.bbrc.2013.06.004",
"doi-asserted-by": "publisher",
"key": "ref55"
},
{
"DOI": "10.1371/journal.ppat.1002689",
"doi-asserted-by": "publisher",
"key": "ref56"
},
{
"DOI": "10.1016/j.chom.2009.08.004",
"doi-asserted-by": "publisher",
"key": "ref57"
},
{
"DOI": "10.1038/s41586-018-0162-7",
"doi-asserted-by": "publisher",
"key": "ref58"
},
{
"DOI": "10.1152/ajpgi.00398.2007",
"doi-asserted-by": "publisher",
"key": "ref59"
},
{
"DOI": "10.1038/jid.2011.296",
"doi-asserted-by": "publisher",
"key": "ref60"
},
{
"DOI": "10.1080/21688370.2018.1540904",
"doi-asserted-by": "publisher",
"key": "ref61"
},
{
"DOI": "10.1038/s41392-021-00679-0",
"doi-asserted-by": "publisher",
"key": "ref62"
},
{
"DOI": "10.3390/nu7043011",
"doi-asserted-by": "publisher",
"key": "ref63"
},
{
"DOI": "10.1016/j.jaut.2017.07.007",
"doi-asserted-by": "publisher",
"key": "ref64"
},
{
"DOI": "10.1038/ki.2008.101",
"doi-asserted-by": "publisher",
"key": "ref65"
},
{
"DOI": "10.3892/mmr.2017.7546",
"doi-asserted-by": "publisher",
"key": "ref66"
},
{
"DOI": "10.1097/SHK.0b013e3182a6953e",
"doi-asserted-by": "publisher",
"key": "ref67"
},
{
"DOI": "10.3390/biom9110649",
"doi-asserted-by": "publisher",
"key": "ref68"
},
{
"DOI": "10.1074/jbc.M404865200",
"doi-asserted-by": "publisher",
"key": "ref69"
},
{
"DOI": "10.1096/fj.15-272872",
"doi-asserted-by": "publisher",
"key": "ref70"
},
{
"DOI": "10.1177/1076029618786574",
"doi-asserted-by": "publisher",
"key": "ref71"
},
{
"DOI": "10.3390/nu9090980",
"doi-asserted-by": "publisher",
"key": "ref72"
},
{
"DOI": "10.1038/s41598-021-96152-7",
"doi-asserted-by": "publisher",
"key": "ref73"
},
{
"DOI": "10.1016/j.pupt.2019.01.003",
"doi-asserted-by": "publisher",
"key": "ref74"
},
{
"DOI": "10.1080/10408398.2020.1841090",
"doi-asserted-by": "publisher",
"key": "ref75"
},
{
"DOI": "10.1080/10408398.2021.1951652",
"doi-asserted-by": "publisher",
"key": "ref76"
},
{
"DOI": "10.5603/ARM.a2021.0037",
"doi-asserted-by": "publisher",
"key": "ref77"
},
{
"DOI": "10.1016/j.metabol.2021.154753",
"doi-asserted-by": "publisher",
"key": "ref78"
},
{
"DOI": "10.1093/advances/nmab012",
"doi-asserted-by": "publisher",
"key": "ref79"
},
{
"DOI": "10.4178/epih.e2021074",
"doi-asserted-by": "publisher",
"key": "ref80"
},
{
"DOI": "10.1111/cen.14540",
"doi-asserted-by": "publisher",
"key": "ref81"
},
{
"DOI": "10.1016/j.ijid.2020.12.077",
"doi-asserted-by": "publisher",
"key": "ref82"
},
{
"DOI": "10.3389/fpubh.2021.736665",
"doi-asserted-by": "publisher",
"key": "ref83"
},
{
"DOI": "10.1210/clinem/dgab892",
"doi-asserted-by": "publisher",
"key": "ref84"
},
{
"DOI": "10.1186/s13054-019-2472-z",
"doi-asserted-by": "publisher",
"key": "ref85"
},
{
"DOI": "10.3390/nu11051016",
"doi-asserted-by": "publisher",
"key": "ref86"
},
{
"DOI": "10.1002/jbmr.4387",
"doi-asserted-by": "publisher",
"key": "ref87"
},
{
"DOI": "10.3390/nu14050963",
"doi-asserted-by": "publisher",
"key": "ref88"
},
{
"DOI": "10.1007/s00198-018-4520-y",
"doi-asserted-by": "publisher",
"key": "ref89"
},
{
"DOI": "10.1007/s43630-022-00230-2",
"doi-asserted-by": "publisher",
"key": "ref90"
},
{
"DOI": "10.1002/jbmr.3181",
"doi-asserted-by": "publisher",
"key": "ref91"
},
{
"DOI": "10.1002/jbmr.3884",
"doi-asserted-by": "publisher",
"key": "ref92"
},
{
"DOI": "10.1093/ajcn/nqab123",
"doi-asserted-by": "publisher",
"key": "ref93"
},
{
"DOI": "10.1164/rccm.201909-1867OC",
"doi-asserted-by": "publisher",
"key": "ref94"
},
{
"DOI": "10.1136/thoraxjnl-2019-213936",
"doi-asserted-by": "publisher",
"key": "ref95"
},
{
"DOI": "10.1002/jbmr.551",
"doi-asserted-by": "publisher",
"key": "ref96"
},
{
"DOI": "10.1186/s12879-021-06457-1",
"doi-asserted-by": "publisher",
"key": "ref97"
},
{
"DOI": "10.3390/geriatrics7010013",
"doi-asserted-by": "publisher",
"key": "ref98"
},
{
"DOI": "10.3390/biomedicines9050509",
"doi-asserted-by": "publisher",
"key": "ref99"
},
{
"DOI": "10.1038/s41598-021-02701-5",
"doi-asserted-by": "publisher",
"key": "ref100"
},
{
"DOI": "10.1016/j.jsbmb.2020.105751",
"doi-asserted-by": "publisher",
"key": "ref101"
},
{
"DOI": "10.3390/nu13061760",
"doi-asserted-by": "publisher",
"key": "ref102"
},
{
"DOI": "10.1210/clinem/dgab405",
"doi-asserted-by": "publisher",
"key": "ref103"
},
{
"DOI": "10.1016/j.eprac.2021.09.016",
"doi-asserted-by": "publisher",
"key": "ref104"
},
{
"DOI": "10.3389/fnut.2021.761191",
"doi-asserted-by": "publisher",
"key": "ref105"
},
{
"DOI": "10.1080/07853890.2022.2034936",
"doi-asserted-by": "publisher",
"key": "ref106"
},
{
"DOI": "10.1111/joim.13478",
"doi-asserted-by": "publisher",
"key": "ref107"
}
],
"reference-count": 107,
"references-count": 107,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2072-6643/14/13/2716"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Food Science",
"Nutrition and Dietetics"
],
"subtitle": [],
"title": "Vitamin D Endocrine System and COVID-19: Treatment with Calcifediol",
"type": "journal-article",
"volume": "14"
}
