Real world evidence of calcifediol or vitamin D prescription and mortality rate of COVID-19 in a retrospective cohort of hospitalized Andalusian patients
et al., Scientific Reports, doi:10.1038/s41598-021-02701-5, Apr 2021 (preprint)
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
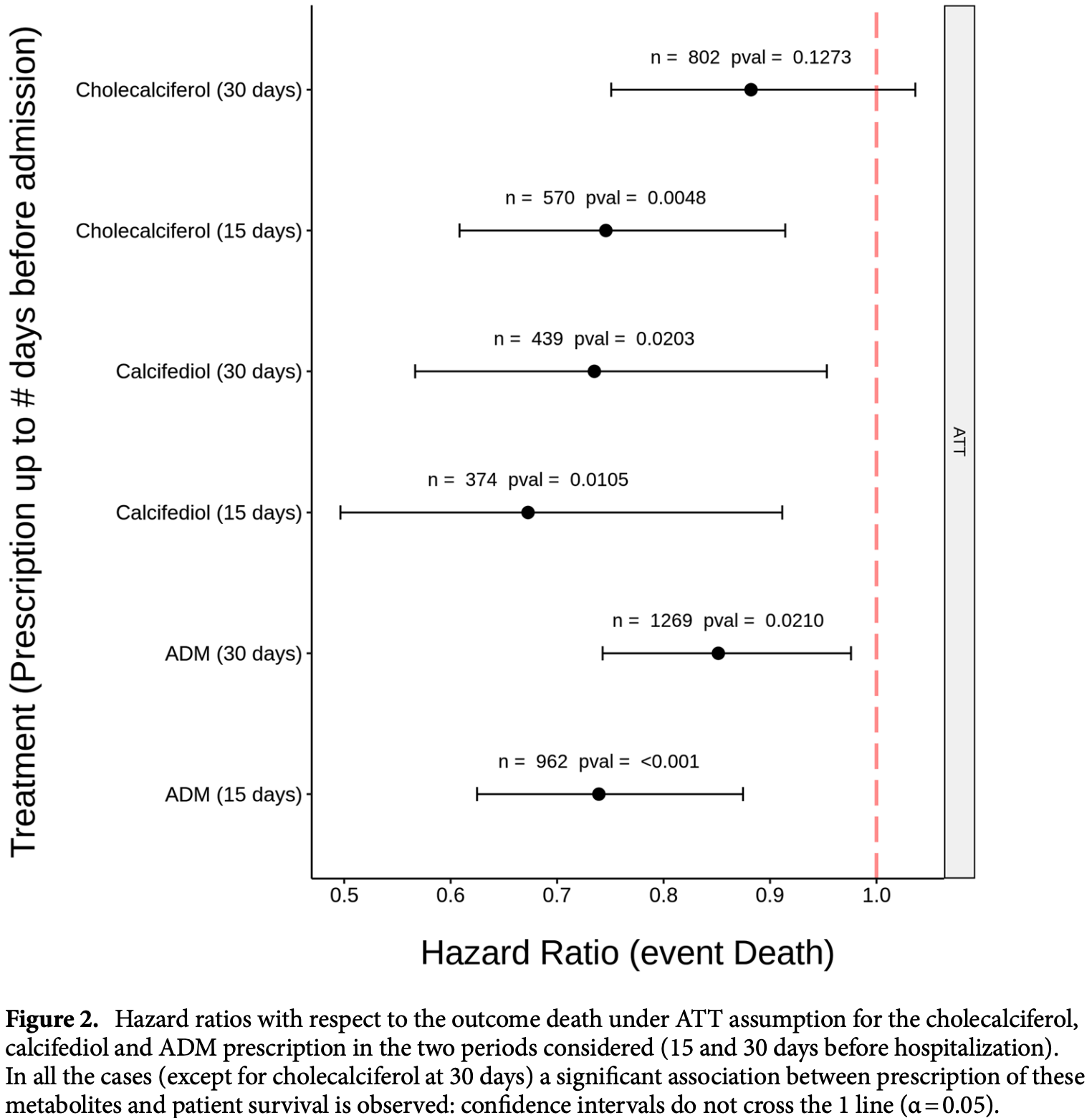
Retrospective 15,968 hospitalized patients in Spain showing a significant reduction in mortality associated with the prescription of vitamin D, especially calcifediol, within 15-30 days prior to hospitalization.
This is the 31st of 136 COVID-19 controlled studies for vitamin D, which collectively show efficacy with p<0.0000000001.
40 studies are RCTs, which show efficacy with p=0.0000001.
|
risk of death, 33.0% lower, HR 0.67, p = 0.009, treatment 374, control 374, calcifediol, <15 days before hospitalization, Cox model with inverse propensity weighting.
|
|
risk of death, 27.0% lower, HR 0.73, p = 0.02, treatment 439, control 439, calcifediol, <30 days before hospitalization, Cox model with inverse propensity weighting.
|
|
risk of death, 25.0% lower, HR 0.75, p = 0.005, treatment 570, control 570, cholecalciferol, <15 days before hospitalization, Cox model with inverse propensity weighting.
|
|
risk of death, 12.0% lower, HR 0.88, p = 0.11, treatment 802, control 802, cholecalciferol, <30 days before hospitalization, Cox model with inverse propensity weighting.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Loucera et al., 29 Apr 2021, retrospective, propensity score matching, Spain, peer-reviewed, 11 authors, dosage varies (calcifediol).
Real world evidence of calcifediol or vitamin D prescription and mortality rate of COVID-19 in a retrospective cohort of hospitalized Andalusian patients
Scientific Reports, doi:10.1038/s41598-021-02701-5
COVID-19 is a major worldwide health problem because of acute respiratory distress syndrome, and mortality. Several lines of evidence have suggested a relationship between the vitamin D endocrine system and severity of COVID-19. We present a survival study on a retrospective cohort of 15,968 patients, comprising all COVID-19 patients hospitalized in Andalusia between January and November 2020. Based on a central registry of electronic health records (the Andalusian Population Health Database, BPS), prescription of vitamin D or its metabolites within 15-30 days before hospitalization were recorded. The effect of prescription of vitamin D (metabolites) for other indication previous to the hospitalization was studied with respect to patient survival. Kaplan-Meier survival curves and hazard ratios support an association between prescription of these metabolites and patient survival. Such association was stronger for calcifediol (Hazard Ratio, HR = 0.67, with 95% confidence interval, CI, of [0.50-0.91]) than for cholecalciferol (HR = 0.75, with 95% CI of [0.61-0.91]), when prescribed 15 days prior hospitalization. Although the relation is maintained, there is a general decrease of this effect when a longer period of 30 days prior hospitalization is considered (calcifediol HR = 0.73, with 95% CI [0.57-0.95] and cholecalciferol HR = 0.88, with 95% CI [0.75, 1.03]), suggesting that association was stronger when the prescription was closer to the hospitalization.
Author contributions C.L.: Data curation, Formal Analysis, Investigation, Visualization; M.P.C.: Formal Analysis; M.E.M.: Formal Analysis; D.M.M.: Resources; R.V.: Resources; J.L.M.: Writing-review and editing; J.R.B.: Writing-review and editing; I.T.: Writing-review and editing; R.B.: Writing-review and editing; J.D.: Supervision, Project administration, Writing-original draft; J.M.Q.G.: Supervision, Writing-original draft. All authors reviewed the manuscript.
Competing interests RB declares payment of honoraria for lectures by FAES (Spain), Abiogen (Italy) and Fresenius (Germany). JMQ declares small consulting fees and small lecture fees from Amgen and FESE Farma (Spain). The rest of authors declare no competing interests.
Additional information
Supplementary Information The online version contains supplementary material available at https:// doi. org/ 10. 1038/ s41598-021-02701-5. Correspondence and requests for materials should be addressed to J.D. or J.M.Q.G. Reprints and permissions information is available at www.nature.com/reprints. Publisher's note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Alcala-Diaz, Calcifediol treatment and hospital mortality due to COVID-19: A cohort study, Nutrients
Austin, Variance estimation when using inverse probability of treatment weighting (IPTW) with survival analysis, Stat. Med
Baktash, Vitamin D status and outcomes for hospitalised older patients with COVID-19, Postgrad. Med. J
Bassatne, The link between COVID-19 and VItamin D (VIVID): A systematic review and meta-analysis, Metabolism
Benjamini, Hochberg, Controlling the false discovery rate: A practical and powerful approach to multiple testing, J. R. Stat. Soc. Ser. B
Bilezikian, Mechanisms in endocrinology: Vitamin D and COVID-19, Eur. J. Endocrinol
Blondon, Thrombin generation and fibrin clot structure after vitamin D supplementation, Endocr. Connect
Bothwell, Podolsky, The emergence of the randomized, controlled trial, N. Engl. J. Med
Bouillon, Skeletal and extraskeletal actions of vitamin D: Current evidence and outstanding questions, Endocr. Rev
Carrigan, Using electronic health records to derive control arms for early phase single-arm lung cancer trials: Proof-ofconcept in randomized controlled trials, Clin. Pharmacol. Ther
Castillo, Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study, J. Steroid Biochem. Mol. Biol
Charoenngam, A pilot-randomized, double-blind crossover trial to evaluate the pharmacokinetics of orally administered 25-hydroxyvitamin D3 and vitamin D3 in healthy adults with differing BMI and in adults with intestinal malabsorption, Am. J. Clin. Nutr
Corrigan-Curay, Sacks, Woodcock, Real-world evidence and real-world data for evaluating drug safety and effectiveness, J. Am. Med. Assoc, doi:10.1001/jama.2018.10136
Cowie, Electronic health records to facilitate clinical research, Clin. Res. Cardiol
Faul, Vitamin D deficiency and ARDS after SARS-CoV-2 infection, Ir. Med. J
González-Molero, Vitamin D deficiency in Spain: A population-based cohort study, Eur. J. Clin. Nutr
Grant, Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths, Nutrients
Gutiérrez-Gutiérrez, Identification and validation of clinical phenotypes with prognostic implications in patients admitted to hospital with COVID-19: A multicentre cohort study, Lancet Infect. Dis, doi:10.1016/S1473-3099(21)00019-0
Hajage, Closed-form variance estimator for weighted propensity score estimators with survival outcome, Biom. J
Hajage, Hripw, Hazard ratio estimation using Cox model weighted by the estimated propensity score
Hannan, Randomized clinical trials and observational studies: Guidelines for assessing respective strengths and limitations, JACC Cardiovasc. Interv
Hernández, Vitamin D status in hospitalized patients with SARS-CoV-2 infection, J. Clin. Endocrinol. Metab
Ho, Imai, King, Stuart, Matching as nonparametric preprocessing for reducing model dependence in parametric causal inference, Polit. Anal
Ilie, Stefanescu, Smith, The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality, Aging Clin. Exp. Res
Imbens, Nonparametric estimation of average treatment effects under exogeneity: A review, Rev. Econ. Stat
Jiang, Ge, Chen, The causal role of circulating vitamin D concentrations in human complex traits and diseases: A large-scale Mendelian randomization study, Sci. Rep
Jude, Ling, Allcock, Yeap, Pappachan, Vitamin D deficiency is associated with higher hospitalization risk from COVID-19: A retrospective case-control study, J. Clin. Endocrinol. Metab, doi:10.1210/clinem/dgab439
Kassambara, Kosinski, Biecek, Fabian, Package 'survminer, Scientific Reports
Kaufman, Niles, Kroll, Bi, Holick, SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels, PLoS One
Kong, VDR attenuates acute lung injury by blocking Ang-2-Tie-2 pathway and renin-angiotensin system, Mol. Endocrinol
Liao, Liu, Wu, Dynamic RMST curves for survival analysis in clinical trials, BMC Med. Res. Methodol
Liu, Low vitamin D status is associated with coronavirus disease 2019 outcomes: A systematic review and meta-analysis, Int. J. Infect. Dis
Loucera, Drug repurposing for COVID-19 using machine learning and mechanistic models of signal transduction circuits related to SARS-CoV-2 infection, Signal Transduct. Target. Ther, doi:10.1038/s41392-020-00417-y
Marik, Kory, Varon, Does vitamin D status impact mortality from SARS-CoV-2 infection?, Med. Drug Discov
Martineau, Vitamin D supplementation to prevent acute respiratory tract infections: Systematic review and meta-analysis of individual participant data, BMJ
Martinez-Moreno, Vitamin D modulates tissue factor and protease-activated receptor 2 expression in vascular smooth muscle cells, FASEB J
Meltzer, Association of vitamin D status and other clinical characteristics with COVID-19 test results, JAMA Netw. Open
Merzon, Low plasma 25 (OH) vitamin D level is associated with increased risk of COVID-19 infection: An Israeli population-based study, FEBS J
Murai, Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: A randomized clinical trial, J. Am. Med. Assoc
Muñoyerro-Muñiz, Health record linkage: Andalusian health population database, Gac. Sanit
Ng, Comorbidities in SARS-CoV-2 patients: A systematic review and meta-analysis, MBio
Nogues, Calcifediol treatment and COVID-19-related outcomes
Oristrell, Association of calcitriol supplementation with reduced COVID-19 mortality in patients with chronic kidney disease: A population-based study, Biomedicines
Oristrell, Vitamin D supplementation and COVID-19 risk: A population-based, cohort study, J. Endocrinol. Investig, doi:10.1007/s40618-021-01639
Ostaszewski, COVID-19 Disease Map, building a computational repository of SARS-CoV-2 virus-host interaction mechanisms, Sci. Data
Pereira, Dantas Damascena, Galvão Azevedo, De Almeida Oliveira, Da Mota Santana, Vitamin D deficiency aggravates COVID-19: Systematic review and meta-analysis, Crit. Rev. Food Sci. Nutr, doi:10.1080/10408398.2020.1841090
Pérez-Castrillón, Calcifediol is superior to cholecalciferol in improving vitamin D status in postmenopausal women: A randomized trial, J. Bone Miner. Res
Quesada-Gomez, Bouillon, Is calcifediol better than cholecalciferol for vitamin D supplementation?, Osteoporos. Int
Quesada-Gomez, Entrenas-Castillo, Bouillon, Vitamin D receptor stimulation to reduce acute respiratory distress syndrome (ARDS) in patients with coronavirus SARS-CoV-2 infections: Revised Ms SBMB 2020_166, J. Steroid Biochem. Mol. Biol
Radujkovic, Vitamin D deficiency and outcome of COVID-19 patients, Nutrients
Ramagopalan, Simpson, Sammon, Can real-world data really replace randomised clinical trials?, BMC Med
Rhodes, Subramanian, Laird, Kenny, low population mortality from COVID-19 in countries south of latitude 35 degrees North supports vitamin D as a factor determining severity, Aliment. Pharmacol. Ther
Rian, Mechanistic modeling of the SARS-CoV-2 disease map, BioData Min, doi:10.1186/s13040-021-00234-1
Sherman, Real-world evidence-What is it and what can it tell us, N. Engl. J. Med
Shi, Vitamin D/VDR signaling attenuates lipopolysaccharide-induced acute lung injury by maintaining the integrity of the pulmonary epithelial barrier, Mol. Med. Rep
Sterne, Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19: A meta-analysis, J. Am. Med. Assoc
Stroehlein, Vitamin D supplementation for the treatment of COVID-19: A living systematic review, Cochrane Database Syst. Rev
Stuart, King, Imai, Ho, MatchIt: Nonparametric preprocessing for parametric causal inference, J. Stat. Softw
Takano, Mitsuhashi, Ueno, 25-Dihydroxyvitamin D3 inhibits neutrophil recruitment in hamster model of acute lung injury, Steroids
Therneau, A package for survival analysis in R
Uno, survRM2: Comparing restricted mean survival time
Wang, Association of vitamin D deficiency with COVID-19 infection severity: Systematic review and meta-analysis, Clin. Endocrinol, doi:10.1111/cen.14540
Xu, Vitamin D alleviates lipopolysaccharide-induced acute lung injury via regulation of the renin-angiotensin system, Mol. Med. Rep
Zakrison, Austin, Mccredie, A systematic review of propensity score methods in the acute care surgery literature: Avoiding the pitfalls and proposing a set of reporting guidelines, Eur. J. Trauma Emerg. Surg
Zheng, Vitamin D attenuates lung injury via stimulating epithelial repair, reducing epithelial cell apoptosis and inhibits TGF-β induced epithelial to mesenchymal transition, Biochem. Pharmacol
DOI record:
{
"DOI": "10.1038/s41598-021-02701-5",
"ISSN": [
"2045-2322"
],
"URL": "http://dx.doi.org/10.1038/s41598-021-02701-5",
"abstract": "<jats:title>Abstract</jats:title><jats:p>COVID-19 is a major worldwide health problem because of acute respiratory distress syndrome, and mortality. Several lines of evidence have suggested a relationship between the vitamin D endocrine system and severity of COVID-19. We present a survival study on a retrospective cohort of 15,968 patients, comprising all COVID-19 patients hospitalized in Andalusia between January and November 2020. Based on a central registry of electronic health records (the Andalusian Population Health Database, BPS), prescription of vitamin D or its metabolites within 15–30 days before hospitalization were recorded. The effect of prescription of vitamin D (metabolites) for other indication previous to the hospitalization was studied with respect to patient survival. Kaplan–Meier survival curves and hazard ratios support an association between prescription of these metabolites and patient survival. Such association was stronger for calcifediol (Hazard Ratio, HR = 0.67, with 95% confidence interval, CI, of [0.50–0.91]) than for cholecalciferol (HR = 0.75, with 95% CI of [0.61–0.91]), when prescribed 15 days prior hospitalization. Although the relation is maintained, there is a general decrease of this effect when a longer period of 30 days prior hospitalization is considered (calcifediol HR = 0.73, with 95% CI [0.57–0.95] and cholecalciferol HR = 0.88, with 95% CI [0.75, 1.03]), suggesting that association was stronger when the prescription was closer to the hospitalization.</jats:p>",
"alternative-id": [
"2701"
],
"article-number": "23380",
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "3 September 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "19 November 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "3 December 2021"
},
{
"group": {
"label": "Competing interests",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1,
"value": "RB declares payment of honoraria for lectures by FAES (Spain), Abiogen (Italy) and Fresenius (Germany). JMQ declares small consulting fees and small lecture fees from Amgen and FESE Farma (Spain). The rest of authors declare no competing interests."
}
],
"author": [
{
"affiliation": [],
"family": "Loucera",
"given": "Carlos",
"sequence": "first"
},
{
"affiliation": [],
"family": "Peña-Chilet",
"given": "María",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Esteban-Medina",
"given": "Marina",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Muñoyerro-Muñiz",
"given": "Dolores",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Villegas",
"given": "Román",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lopez-Miranda",
"given": "Jose",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rodriguez-Baño",
"given": "Jesus",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Túnez",
"given": "Isaac",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bouillon",
"given": "Roger",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dopazo",
"given": "Joaquin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Quesada Gomez",
"given": "Jose Manuel",
"sequence": "additional"
}
],
"container-title": [
"Scientific Reports"
],
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2021,
12,
3
]
],
"date-time": "2021-12-03T11:03:41Z",
"timestamp": 1638529421000
},
"deposited": {
"date-parts": [
[
2021,
12,
3
]
],
"date-time": "2021-12-03T11:11:41Z",
"timestamp": 1638529901000
},
"funder": [
{
"award": [
"PAIDI2020-DOC_00350"
],
"name": "Consejería de Transformación Económica, Industria, Conocimiento y Universidades, Junta de Andalucía"
},
{
"award": [
"ACCI2018/29"
],
"name": "Centro de Investigación Biomédica en Red sobre Enfermedades Raras"
},
{
"DOI": "10.13039/501100004837",
"award": [
"PID2020-117979RB-I00"
],
"doi-asserted-by": "publisher",
"name": "Ministerio de Ciencia e Innovación"
},
{
"DOI": "10.13039/501100004587",
"award": [
"IMP/0019",
"PI19/00033"
],
"doi-asserted-by": "publisher",
"name": "Instituto de Salud Carlos III"
},
{
"DOI": "10.13039/100007406",
"award": [
"G999088Q"
],
"doi-asserted-by": "publisher",
"name": "Fundación BBVA"
},
{
"DOI": "10.13039/100010665",
"award": [
"813533"
],
"doi-asserted-by": "publisher",
"name": "H2020 Marie Skłodowska-Curie Actions"
},
{
"DOI": "10.13039/501100010566",
"award": [
"COVID-011-2020"
],
"doi-asserted-by": "publisher",
"name": "Consejería de Salud y Familias, Junta de Andalucía"
},
{
"DOI": "10.13039/100012619",
"award": [
"CB16/10/00245"
],
"doi-asserted-by": "publisher",
"name": "Centro de Investigación Biomédica en Red Fragilidad y Envejecimiento Saludable"
}
],
"indexed": {
"date-parts": [
[
2021,
12,
3
]
],
"date-time": "2021-12-03T13:47:16Z",
"timestamp": 1638539236404
},
"is-referenced-by-count": 0,
"issn-type": [
{
"type": "electronic",
"value": "2045-2322"
}
],
"issue": "1",
"issued": {
"date-parts": [
[
2021,
12
]
]
},
"journal-issue": {
"issue": "1",
"published-print": {
"date-parts": [
[
2021,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
12,
1
]
],
"date-time": "2021-12-01T00:00:00Z",
"timestamp": 1638316800000
}
},
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "vor",
"delay-in-days": 2,
"start": {
"date-parts": [
[
2021,
12,
3
]
],
"date-time": "2021-12-03T00:00:00Z",
"timestamp": 1638489600000
}
}
],
"link": [
{
"URL": "https://www.nature.com/articles/s41598-021-02701-5.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.nature.com/articles/s41598-021-02701-5",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.nature.com/articles/s41598-021-02701-5.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1038",
"published": {
"date-parts": [
[
2021,
12
]
]
},
"published-online": {
"date-parts": [
[
2021,
12,
3
]
]
},
"published-print": {
"date-parts": [
[
2021,
12
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1210/er.2018-00126",
"author": "R Bouillon",
"doi-asserted-by": "crossref",
"first-page": "1109",
"journal-title": "Endocr. Rev.",
"key": "2701_CR1",
"unstructured": "Bouillon, R. et al. Skeletal and extraskeletal actions of vitamin D: Current evidence and outstanding questions. Endocr. Rev. 40, 1109–1151 (2019).",
"volume": "40",
"year": "2019"
},
{
"DOI": "10.1038/s41598-020-79139-8",
"author": "X Jiang",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Sci. Rep.",
"key": "2701_CR2",
"unstructured": "Jiang, X., Ge, T. & Chen, C.-Y. The causal role of circulating vitamin D concentrations in human complex traits and diseases: A large-scale Mendelian randomization study. Sci. Rep. 11, 1–10 (2021).",
"volume": "11",
"year": "2021"
},
{
"author": "AR Martineau",
"journal-title": "BMJ",
"key": "2701_CR3",
"unstructured": "Martineau, A. R. et al. Vitamin D supplementation to prevent acute respiratory tract infections: Systematic review and meta-analysis of individual participant data. BMJ 356, i6583 (2017).",
"volume": "356",
"year": "2017"
},
{
"author": "HW Kaufman",
"journal-title": "PLoS One",
"key": "2701_CR4",
"unstructured": "Kaufman, H. W., Niles, J. K., Kroll, M. H., Bi, C. & Holick, M. F. SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels. PLoS One 15, e0239252 (2020).",
"volume": "15",
"year": "2020"
},
{
"author": "V Baktash",
"first-page": "442",
"journal-title": "Postgrad. Med. J.",
"key": "2701_CR5",
"unstructured": "Baktash, V. et al. Vitamin D status and outcomes for hospitalised older patients with COVID-19. Postgrad. Med. J. 97, 442–447 (2021).",
"volume": "97",
"year": "2021"
},
{
"author": "J Faul",
"first-page": "84",
"journal-title": "Ir. Med. J.",
"key": "2701_CR6",
"unstructured": "Faul, J. et al. Vitamin D deficiency and ARDS after SARS-CoV-2 infection. Ir. Med. J. 113, 84 (2020).",
"volume": "113",
"year": "2020"
},
{
"DOI": "10.3390/nu12092757",
"author": "A Radujkovic",
"doi-asserted-by": "crossref",
"first-page": "2757",
"journal-title": "Nutrients",
"key": "2701_CR7",
"unstructured": "Radujkovic, A. et al. Vitamin D deficiency and outcome of COVID-19 patients. Nutrients 12, 2757 (2020).",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1111/febs.15495",
"author": "E Merzon",
"doi-asserted-by": "crossref",
"first-page": "3693",
"journal-title": "FEBS J.",
"key": "2701_CR8",
"unstructured": "Merzon, E. et al. Low plasma 25 (OH) vitamin D level is associated with increased risk of COVID-19 infection: An Israeli population-based study. FEBS J. 287, 3693–3702 (2020).",
"volume": "287",
"year": "2020"
},
{
"DOI": "10.1001/jamanetworkopen.2020.19722",
"author": "DO Meltzer",
"doi-asserted-by": "crossref",
"journal-title": "JAMA Netw. Open",
"key": "2701_CR9",
"unstructured": "Meltzer, D. O. et al. Association of vitamin D status and other clinical characteristics with COVID-19 test results. JAMA Netw. Open 3, e2019722 (2020).",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1210/clinem/dgaa733",
"author": "JL Hernández",
"doi-asserted-by": "crossref",
"first-page": "e1343",
"journal-title": "J. Clin. Endocrinol. Metab.",
"key": "2701_CR10",
"unstructured": "Hernández, J. L. et al. Vitamin D status in hospitalized patients with SARS-CoV-2 infection. J. Clin. Endocrinol. Metab. 106, e1343–e1353 (2021).",
"volume": "106",
"year": "2021"
},
{
"DOI": "10.1080/10408398.2020.1841090",
"author": "M Pereira",
"doi-asserted-by": "publisher",
"journal-title": "Crit. Rev. Food Sci. Nutr.",
"key": "2701_CR11",
"unstructured": "Pereira, M., Dantas Damascena, A., Galvão Azevedo, L. M., de Almeida Oliveira, T. & da Mota Santana, J. Vitamin D deficiency aggravates COVID-19: Systematic review and meta-analysis. Crit. Rev. Food Sci. Nutr. https://doi.org/10.1080/10408398.2020.1841090 (2020).",
"year": "2020"
},
{
"DOI": "10.1016/j.metabol.2021.154753",
"author": "A Bassatne",
"doi-asserted-by": "crossref",
"journal-title": "Metabolism",
"key": "2701_CR12",
"unstructured": "Bassatne, A. et al. The link between COVID-19 and VItamin D (VIVID): A systematic review and meta-analysis. Metabolism 119, 154753 (2021).",
"volume": "119",
"year": "2021"
},
{
"DOI": "10.1111/cen.14540",
"author": "Z Wang",
"doi-asserted-by": "publisher",
"journal-title": "Clin. Endocrinol.",
"key": "2701_CR13",
"unstructured": "Wang, Z. et al. Association of vitamin D deficiency with COVID-19 infection severity: Systematic review and meta-analysis. Clin. Endocrinol. https://doi.org/10.1111/cen.14540 (2021).",
"year": "2021"
},
{
"key": "2701_CR14",
"unstructured": "NICE guideline COVID-19 rapid guideline: Vitamin D http://www.nice.org.uk/guidance/ng187 (2020)."
},
{
"author": "JK Stroehlein",
"journal-title": "Cochrane Database Syst. Rev.",
"key": "2701_CR15",
"unstructured": "Stroehlein, J. K. et al. Vitamin D supplementation for the treatment of COVID-19: A living systematic review. Cochrane Database Syst. Rev. 5, CD015043 (2021).",
"volume": "5",
"year": "2021"
},
{
"DOI": "10.1038/s41392-020-00417-y",
"author": "C Loucera",
"doi-asserted-by": "publisher",
"first-page": "290",
"journal-title": "Signal Transduct. Target. Ther.",
"key": "2701_CR16",
"unstructured": "Loucera, C. et al. Drug repurposing for COVID-19 using machine learning and mechanistic models of signal transduction circuits related to SARS-CoV-2 infection. Signal Transduct. Target. Ther. 5, 290. https://doi.org/10.1038/s41392-020-00417-y (2020).",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1186/s13040-021-00234-1",
"author": "K Rian",
"doi-asserted-by": "publisher",
"first-page": "5",
"journal-title": "BioData Min.",
"key": "2701_CR17",
"unstructured": "Rian, K. et al. Mechanistic modeling of the SARS-CoV-2 disease map. BioData Min. 14, 5. https://doi.org/10.1186/s13040-021-00234-1 (2021).",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.1038/s41597-020-0477-8",
"author": "M Ostaszewski",
"doi-asserted-by": "crossref",
"first-page": "136",
"journal-title": "Sci. Data",
"key": "2701_CR18",
"unstructured": "Ostaszewski, M. et al. COVID-19 Disease Map, building a computational repository of SARS-CoV-2 virus-host interaction mechanisms. Sci. Data 7, 136 (2020).",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1056/NEJMp1604635",
"author": "LE Bothwell",
"doi-asserted-by": "crossref",
"first-page": "501",
"journal-title": "N. Engl. J. Med.",
"key": "2701_CR19",
"unstructured": "Bothwell, L. E. & Podolsky, S. H. The emergence of the randomized, controlled trial. N. Engl. J. Med. 375, 501–504 (2016).",
"volume": "375",
"year": "2016"
},
{
"DOI": "10.1001/jama.2018.10136",
"author": "J Corrigan-Curay",
"doi-asserted-by": "publisher",
"first-page": "867",
"journal-title": "J. Am. Med. Assoc.",
"key": "2701_CR20",
"unstructured": "Corrigan-Curay, J., Sacks, L. & Woodcock, J. Real-world evidence and real-world data for evaluating drug safety and effectiveness. J. Am. Med. Assoc. 320, 867–868. https://doi.org/10.1001/jama.2018.10136 (2018).",
"volume": "320",
"year": "2018"
},
{
"key": "2701_CR21",
"unstructured": "US Food and Drug Administration. Use of real-world evidence to support regulatory decision-making for medical devices: Guidance for industry and Food and Drug Administration staff. https://www.fda.gov/downloads/medicaldevices/deviceregulationandguidance/guidancedocuments/ucm513027.pdf (2017)."
},
{
"DOI": "10.1056/NEJMsb1609216",
"author": "RE Sherman",
"doi-asserted-by": "crossref",
"first-page": "2293",
"journal-title": "N. Engl. J. Med.",
"key": "2701_CR22",
"unstructured": "Sherman, R. E. et al. Real-world evidence—What is it and what can it tell us. N. Engl. J. Med. 375, 2293–2297 (2016).",
"volume": "375",
"year": "2016"
},
{
"DOI": "10.1016/j.jcin.2008.01.008",
"author": "EL Hannan",
"doi-asserted-by": "crossref",
"first-page": "211",
"journal-title": "JACC Cardiovasc. Interv.",
"key": "2701_CR23",
"unstructured": "Hannan, E. L. Randomized clinical trials and observational studies: Guidelines for assessing respective strengths and limitations. JACC Cardiovasc. Interv. 1, 211–217 (2008).",
"volume": "1",
"year": "2008"
},
{
"DOI": "10.1007/s00392-016-1025-6",
"author": "MR Cowie",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Clin. Res. Cardiol.",
"key": "2701_CR24",
"unstructured": "Cowie, M. R. et al. Electronic health records to facilitate clinical research. Clin. Res. Cardiol. 106, 1–9 (2017).",
"volume": "106",
"year": "2017"
},
{
"DOI": "10.1016/j.gaceta.2019.03.003",
"author": "D Muñoyerro-Muñiz",
"doi-asserted-by": "crossref",
"first-page": "105",
"journal-title": "Gac. Sanit.",
"key": "2701_CR25",
"unstructured": "Muñoyerro-Muñiz, D. et al. Health record linkage: Andalusian health population database. Gac. Sanit. 34, 105–113 (2019).",
"volume": "34",
"year": "2019"
},
{
"DOI": "10.1002/cpt.1586",
"author": "G Carrigan",
"doi-asserted-by": "crossref",
"first-page": "369",
"journal-title": "Clin. Pharmacol. Ther.",
"key": "2701_CR26",
"unstructured": "Carrigan, G. et al. Using electronic health records to derive control arms for early phase single-arm lung cancer trials: Proof-of-concept in randomized controlled trials. Clin. Pharmacol. Ther. 107, 369–377 (2020).",
"volume": "107",
"year": "2020"
},
{
"DOI": "10.1186/s12916-019-1481-8",
"author": "SV Ramagopalan",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "BMC Med.",
"key": "2701_CR27",
"unstructured": "Ramagopalan, S. V., Simpson, A. & Sammon, C. Can real-world data really replace randomised clinical trials?. BMC Med. 18, 1–2 (2020).",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.1038/ejcn.2010.265",
"author": "I González-Molero",
"doi-asserted-by": "crossref",
"first-page": "321",
"journal-title": "Eur. J. Clin. Nutr.",
"key": "2701_CR28",
"unstructured": "González-Molero, I. et al. Vitamin D deficiency in Spain: A population-based cohort study. Eur. J. Clin. Nutr. 65, 321–328 (2011).",
"volume": "65",
"year": "2011"
},
{
"DOI": "10.1016/j.ijid.2020.12.077",
"author": "N Liu",
"doi-asserted-by": "crossref",
"first-page": "58",
"journal-title": "Int. J. Infect. Dis.",
"key": "2701_CR29",
"unstructured": "Liu, N. et al. Low vitamin D status is associated with coronavirus disease 2019 outcomes: A systematic review and meta-analysis. Int. J. Infect. Dis. 104, 58–64 (2021).",
"volume": "104",
"year": "2021"
},
{
"DOI": "10.1111/apt.15777",
"author": "JM Rhodes",
"doi-asserted-by": "crossref",
"first-page": "1434",
"journal-title": "Aliment. Pharmacol. Ther.",
"key": "2701_CR30",
"unstructured": "Rhodes, J. M., Subramanian, S., Laird, E. & Kenny, R. A. low population mortality from COVID-19 in countries south of latitude 35 degrees North supports vitamin D as a factor determining severity. Aliment. Pharmacol. Ther. 51, 1434 (2020).",
"volume": "51",
"year": "2020"
},
{
"DOI": "10.1007/s40520-020-01570-8",
"author": "PC Ilie",
"doi-asserted-by": "crossref",
"first-page": "1195",
"journal-title": "Aging Clin. Exp. Res.",
"key": "2701_CR31",
"unstructured": "Ilie, P. C., Stefanescu, S. & Smith, L. The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality. Aging Clin. Exp. Res. 32, 1195–1198 (2020).",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.1016/j.medidd.2020.100041",
"author": "PE Marik",
"doi-asserted-by": "crossref",
"journal-title": "Med. Drug Discov.",
"key": "2701_CR32",
"unstructured": "Marik, P. E., Kory, P. & Varon, J. Does vitamin D status impact mortality from SARS-CoV-2 infection?. Med. Drug Discov. 6, 100041 (2020).",
"volume": "6",
"year": "2020"
},
{
"DOI": "10.1002/jbmr.4387",
"author": "JL Pérez-Castrillón",
"doi-asserted-by": "crossref",
"first-page": "1967",
"journal-title": "J. Bone Miner. Res.",
"key": "2701_CR33",
"unstructured": "Pérez-Castrillón, J. L. et al. Calcifediol is superior to cholecalciferol in improving vitamin D status in postmenopausal women: A randomized trial. J. Bone Miner. Res. 36, 1967–1978 (2021).",
"volume": "36",
"year": "2021"
},
{
"author": "ME Castillo",
"journal-title": "J. Steroid Biochem. Mol. Biol.",
"key": "2701_CR34",
"unstructured": "Castillo, M. E. et al. Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study. J. Steroid Biochem. Mol. Biol. 203, 105751 (2020).",
"volume": "203",
"year": "2020"
},
{
"key": "2701_CR35",
"unstructured": "Nogues, X. et al. Calcifediol treatment and COVID-19-related outcomes. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3771318 (2021)."
},
{
"DOI": "10.3390/nu13061760",
"author": "JF Alcala-Diaz",
"doi-asserted-by": "crossref",
"first-page": "1760",
"journal-title": "Nutrients",
"key": "2701_CR36",
"unstructured": "Alcala-Diaz, J. F. et al. Calcifediol treatment and hospital mortality due to COVID-19: A cohort study. Nutrients 13, 1760 (2021).",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1001/jama.2020.26848",
"author": "IH Murai",
"doi-asserted-by": "crossref",
"first-page": "1053",
"journal-title": "J. Am. Med. Assoc.",
"key": "2701_CR37",
"unstructured": "Murai, I. H. et al. Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: A randomized clinical trial. J. Am. Med. Assoc. 325, 1053–1060 (2021).",
"volume": "325",
"year": "2021"
},
{
"DOI": "10.1007/s40618-021-01639",
"author": "J Oristrell",
"doi-asserted-by": "publisher",
"journal-title": "J. Endocrinol. Investig.",
"key": "2701_CR38",
"unstructured": "Oristrell, J. et al. Vitamin D supplementation and COVID-19 risk: A population-based, cohort study. J. Endocrinol. Investig. https://doi.org/10.1007/s40618-021-01639 (2021).",
"year": "2021"
},
{
"DOI": "10.3390/biomedicines9050509",
"author": "J Oristrell",
"doi-asserted-by": "crossref",
"first-page": "509",
"journal-title": "Biomedicines",
"key": "2701_CR39",
"unstructured": "Oristrell, J. et al. Association of calcitriol supplementation with reduced COVID-19 mortality in patients with chronic kidney disease: A population-based study. Biomedicines 9, 509 (2021).",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1210/clinem/dgab439",
"author": "EB Jude",
"doi-asserted-by": "publisher",
"first-page": "e4708",
"journal-title": "J. Clin. Endocrinol. Metab.",
"key": "2701_CR40",
"unstructured": "Jude, E. B., Ling, S. F., Allcock, R., Yeap, B. X. Y. & Pappachan, J. M. Vitamin D deficiency is associated with higher hospitalization risk from COVID-19: A retrospective case-control study. J. Clin. Endocrinol. Metab. 106, e4708–e4715. https://doi.org/10.1210/clinem/dgab439 (2021).",
"volume": "106",
"year": "2021"
},
{
"DOI": "10.1530/EJE-20-0665",
"author": "JP Bilezikian",
"doi-asserted-by": "crossref",
"first-page": "R133",
"journal-title": "Eur. J. Endocrinol.",
"key": "2701_CR41",
"unstructured": "Bilezikian, J. P. et al. Mechanisms in endocrinology: Vitamin D and COVID-19. Eur. J. Endocrinol. 183, R133–R147 (2020).",
"volume": "183",
"year": "2020"
},
{
"author": "JM Quesada-Gomez",
"journal-title": "J. Steroid Biochem. Mol. Biol.",
"key": "2701_CR42",
"unstructured": "Quesada-Gomez, J. M., Entrenas-Castillo, M. & Bouillon, R. Vitamin D receptor stimulation to reduce acute respiratory distress syndrome (ARDS) in patients with coronavirus SARS-CoV-2 infections: Revised Ms SBMB 2020_166. J. Steroid Biochem. Mol. Biol. 202, 105719 (2020).",
"volume": "202",
"year": "2020"
},
{
"DOI": "10.3390/nu12040988",
"author": "WB Grant",
"doi-asserted-by": "crossref",
"first-page": "988",
"journal-title": "Nutrients",
"key": "2701_CR43",
"unstructured": "Grant, W. B. et al. Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths. Nutrients 12, 988 (2020).",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1016/j.steroids.2011.06.009",
"author": "Y Takano",
"doi-asserted-by": "crossref",
"first-page": "1305",
"journal-title": "Steroids",
"key": "2701_CR44",
"unstructured": "Takano, Y., Mitsuhashi, H. & Ueno, K. 1α, 25-Dihydroxyvitamin D3 inhibits neutrophil recruitment in hamster model of acute lung injury. Steroids 76, 1305–1309 (2011).",
"volume": "76",
"year": "2011"
},
{
"DOI": "10.1016/j.bcp.2020.113955",
"author": "S Zheng",
"doi-asserted-by": "crossref",
"journal-title": "Biochem. Pharmacol.",
"key": "2701_CR45",
"unstructured": "Zheng, S. et al. Vitamin D attenuates lung injury via stimulating epithelial repair, reducing epithelial cell apoptosis and inhibits TGF-β induced epithelial to mesenchymal transition. Biochem. Pharmacol. 177, 113955 (2020).",
"volume": "177",
"year": "2020"
},
{
"DOI": "10.1210/me.2013-1146",
"author": "J Kong",
"doi-asserted-by": "crossref",
"first-page": "2116",
"journal-title": "Mol. Endocrinol.",
"key": "2701_CR46",
"unstructured": "Kong, J. et al. VDR attenuates acute lung injury by blocking Ang-2-Tie-2 pathway and renin-angiotensin system. Mol. Endocrinol. 27, 2116–2125 (2013).",
"volume": "27",
"year": "2013"
},
{
"DOI": "10.3892/mmr.2015.4685",
"author": "YY Shi",
"doi-asserted-by": "crossref",
"first-page": "1186",
"journal-title": "Mol. Med. Rep.",
"key": "2701_CR47",
"unstructured": "Shi, Y. Y. et al. Vitamin D/VDR signaling attenuates lipopolysaccharide-induced acute lung injury by maintaining the integrity of the pulmonary epithelial barrier. Mol. Med. Rep. 13, 1186–1194 (2016).",
"volume": "13",
"year": "2016"
},
{
"DOI": "10.1096/fj.15-272872",
"author": "JM Martinez-Moreno",
"doi-asserted-by": "crossref",
"first-page": "1367",
"journal-title": "FASEB J.",
"key": "2701_CR48",
"unstructured": "Martinez-Moreno, J. M. et al. Vitamin D modulates tissue factor and protease-activated receptor 2 expression in vascular smooth muscle cells. FASEB J. 30, 1367–1376 (2016).",
"volume": "30",
"year": "2016"
},
{
"DOI": "10.1530/EC-19-0429",
"author": "M Blondon",
"doi-asserted-by": "crossref",
"first-page": "1447",
"journal-title": "Endocr. Connect.",
"key": "2701_CR49",
"unstructured": "Blondon, M. et al. Thrombin generation and fibrin clot structure after vitamin D supplementation. Endocr. Connect. 8, 1447–1454 (2019).",
"volume": "8",
"year": "2019"
},
{
"DOI": "10.3892/mmr.2017.7546",
"author": "J Xu",
"doi-asserted-by": "crossref",
"first-page": "7432",
"journal-title": "Mol. Med. Rep.",
"key": "2701_CR50",
"unstructured": "Xu, J. et al. Vitamin D alleviates lipopolysaccharide-induced acute lung injury via regulation of the renin-angiotensin system. Mol. Med. Rep. 16, 7432–7438 (2017).",
"volume": "16",
"year": "2017"
},
{
"DOI": "10.1093/ajcn/nqab123",
"author": "N Charoenngam",
"doi-asserted-by": "crossref",
"first-page": "1189",
"journal-title": "Am. J. Clin. Nutr.",
"key": "2701_CR51",
"unstructured": "Charoenngam, N. et al. A pilot-randomized, double-blind crossover trial to evaluate the pharmacokinetics of orally administered 25-hydroxyvitamin D3 and vitamin D3 in healthy adults with differing BMI and in adults with intestinal malabsorption. Am. J. Clin. Nutr. 114, 1189–1199 (2021).",
"volume": "114",
"year": "2021"
},
{
"DOI": "10.1007/s00198-018-4520-y",
"author": "J Quesada-Gomez",
"doi-asserted-by": "crossref",
"first-page": "1697",
"journal-title": "Osteoporos. Int.",
"key": "2701_CR52",
"unstructured": "Quesada-Gomez, J. & Bouillon, R. Is calcifediol better than cholecalciferol for vitamin D supplementation?. Osteoporos. Int. 29, 1697–1711 (2018).",
"volume": "29",
"year": "2018"
},
{
"DOI": "10.1001/jama.2020.17023",
"author": "JA Sterne",
"doi-asserted-by": "crossref",
"first-page": "1330",
"journal-title": "J. Am. Med. Assoc.",
"key": "2701_CR53",
"unstructured": "Sterne, J. A. et al. Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19: A meta-analysis. J. Am. Med. Assoc. 324, 1330–1341 (2020).",
"volume": "324",
"year": "2020"
},
{
"DOI": "10.1016/S1473-3099(21)00019-0",
"author": "B Gutiérrez-Gutiérrez",
"doi-asserted-by": "publisher",
"journal-title": "Lancet Infect. Dis.",
"key": "2701_CR54",
"unstructured": "Gutiérrez-Gutiérrez, B. et al. Identification and validation of clinical phenotypes with prognostic implications in patients admitted to hospital with COVID-19: A multicentre cohort study. Lancet Infect. Dis. https://doi.org/10.1016/S1473-3099(21)00019-0 (2021).",
"year": "2021"
},
{
"author": "WH Ng",
"journal-title": "MBio",
"key": "2701_CR55",
"unstructured": "Ng, W. H. et al. Comorbidities in SARS-CoV-2 patients: A systematic review and meta-analysis. MBio 12, e03647-03620 (2021).",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1007/s00068-017-0786-6",
"author": "T Zakrison",
"doi-asserted-by": "crossref",
"first-page": "385",
"journal-title": "Eur. J. Trauma Emerg. Surg.",
"key": "2701_CR56",
"unstructured": "Zakrison, T., Austin, P. & McCredie, V. A systematic review of propensity score methods in the acute care surgery literature: Avoiding the pitfalls and proposing a set of reporting guidelines. Eur. J. Trauma Emerg. Surg. 44, 385–395 (2018).",
"volume": "44",
"year": "2018"
},
{
"DOI": "10.1093/pan/mpl013",
"author": "DE Ho",
"doi-asserted-by": "crossref",
"first-page": "199",
"journal-title": "Polit. Anal.",
"key": "2701_CR57",
"unstructured": "Ho, D. E., Imai, K., King, G. & Stuart, E. A. Matching as nonparametric preprocessing for reducing model dependence in parametric causal inference. Polit. Anal. 15, 199–236 (2007).",
"volume": "15",
"year": "2007"
},
{
"DOI": "10.1002/bimj.201700330",
"author": "D Hajage",
"doi-asserted-by": "crossref",
"first-page": "1151",
"journal-title": "Biom. J.",
"key": "2701_CR58",
"unstructured": "Hajage, D. et al. Closed-form variance estimator for weighted propensity score estimators with survival outcome. Biom. J. 60, 1151–1163 (2018).",
"volume": "60",
"year": "2018"
},
{
"DOI": "10.1162/003465304323023651",
"author": "GW Imbens",
"doi-asserted-by": "crossref",
"first-page": "4",
"journal-title": "Rev. Econ. Stat.",
"key": "2701_CR59",
"unstructured": "Imbens, G. W. Nonparametric estimation of average treatment effects under exogeneity: A review. Rev. Econ. Stat. 86, 4–29 (2004).",
"volume": "86",
"year": "2004"
},
{
"DOI": "10.1002/sim.7084",
"author": "PC Austin",
"doi-asserted-by": "crossref",
"first-page": "5642",
"journal-title": "Stat. Med.",
"key": "2701_CR60",
"unstructured": "Austin, P. C. Variance estimation when using inverse probability of treatment weighting (IPTW) with survival analysis. Stat. Med. 35, 5642–5655 (2016).",
"volume": "35",
"year": "2016"
},
{
"author": "Y Benjamini",
"first-page": "289",
"journal-title": "J. R. Stat. Soc. Ser. B",
"key": "2701_CR61",
"unstructured": "Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J. R. Stat. Soc. Ser. B 57, 289–300 (1995).",
"volume": "57",
"year": "1995"
},
{
"DOI": "10.1186/s12874-019-0863-0",
"author": "JJ Liao",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "BMC Med. Res. Methodol.",
"key": "2701_CR62",
"unstructured": "Liao, J. J., Liu, G. F. & Wu, W.-C. Dynamic RMST curves for survival analysis in clinical trials. BMC Med. Res. Methodol. 20, 1–10 (2020).",
"volume": "20",
"year": "2020"
},
{
"author": "EA Stuart",
"first-page": "8",
"journal-title": "J. Stat. Softw.",
"key": "2701_CR63",
"unstructured": "Stuart, E. A., King, G., Imai, K. & Ho, D. MatchIt: Nonparametric preprocessing for parametric causal inference. J. Stat. Softw. 42, 8 (2011).",
"volume": "42",
"year": "2011"
},
{
"key": "2701_CR64",
"unstructured": "Hajage, D. hrIPW: Hazard ratio estimation using Cox model weighted by the estimated propensity score. https://CRAN.R-project.org/package=hrIPW (2020)."
},
{
"key": "2701_CR65",
"unstructured": "Uno, H. et al. survRM2: Comparing restricted mean survival time. https://CRAN.R-project.org/package=survRM2 (2020)."
},
{
"key": "2701_CR66",
"unstructured": "Therneau, T. A package for survival analysis in R. https://CRAN.R-project.org/package=survival (2020)."
},
{
"key": "2701_CR67",
"unstructured": "Kassambara, A., Kosinski, M., Biecek, P. & Fabian, S. Package ‘survminer’. https://rpkgs.datanovia.com/survminer/ (2017)."
}
],
"reference-count": 67,
"references-count": 67,
"relation": {},
"score": 1,
"short-container-title": [
"Sci Rep"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Multidisciplinary"
],
"subtitle": [],
"title": [
"Real world evidence of calcifediol or vitamin D prescription and mortality rate of COVID-19 in a retrospective cohort of hospitalized Andalusian patients"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "11"
}
